- Department of Urology, The Second Affiliated Hospital of Dalian Medical University, Dalian, Liaoning, China
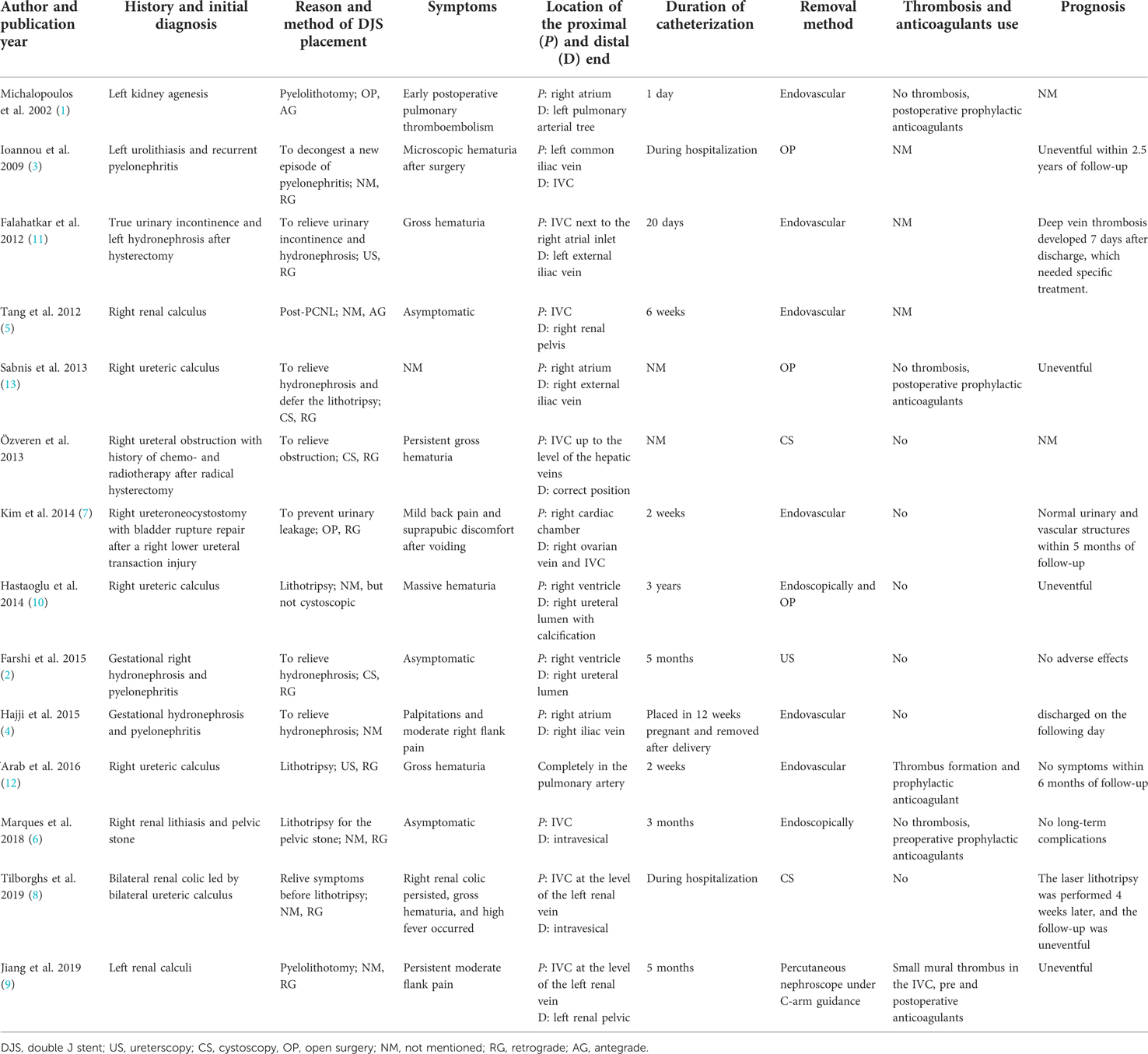
Double J stent (DJS) malposition in the vascular system is a rare and severe complication. We present two cases in our department who went through DJS malposition in the inferior vena cava and our experience in treatment, and we reviewed the previous case reports to further summarize its underlying reasons and prevention and treatment methods.
Introduction
Double J stent (DJS) placement is a common operation in the urology department to relieve or prevent ureteral obstruction and stricture. Although there are some common complications, such as hematuria, bladder irritation, flank, and suprapubic pain, or serious complications, such as vesicoureteral reflux, DJS migration, and DJS encrustation, it is generally a safe and effective procedure. In rare conditions, however, there are also cases where DJSs are misplaced or migrated to an abnormal position. We present two cases of DJS malposition in the inferior vena cava (IVC) and successful treatment in our center.
Case presentation
Case 1
In 2006, a 54-year-old woman complained about right flank pain for 2 days, accompanied by a fever, as high as 39.1°C, for 1 day. Three months ago, she had undergone extracorporeal shockwave lithotripsy (SWL) for right kidney calculi, and scanty gravel was discharged. The physical examination showed obvious percussion pain in her right flank region. Blood and urine routines were normal. Ultrasound and plain CT revealed the diameter of the right renal pelvis was 4.5 cm and a ureteral calculus of 0.8 × 0.9 cm in the lower right ureter, about 3 cm away from the ureteral orifice. The patient’s temperature turned normal soon after antibiotic application. Therefore, ureteroscopic pneumatic lithotripsy was performed under epidural anesthesia without further contrast imaging such as retrograde pyelogram or on-table fluroscopy and ultrasound. The guidewire was reserved, and a double-opening F5 DJS was tried to be placed retrograde, but it was stuck at the ureteral orifice (Figure 1A). Instead, a DJS with a blind proximal coil was placed retrograde under a cystoscope, with a guidewire against its end (Figure 1B). There were no obvious postoperative complications such as hematuria, abdominal pain, fever, and the like. Unfortunately, no postoperative fluoroscopy and ultrasound were performed.

Figure 1. Pattern diagram of the properties of guidewire and double J stents (DJSs). (A) Inner diameter of the DJS is too large so the guidewire cannot fit the stent perfectly, which leads to DJS stuck at the ureteral orifice (arrow). (B) Another kind of a DJS with a blind proximal coil, which needs to be placed with a guidewire against its end. (C) DJS has a blunt-end design (arrow), and the inner diameter matches well with the guidewire, which can make the insertion safer and more accurate.
Two months later, the patient was advised to remove the DJS. As a long time had passed, the radiological data could not be obtained. According to the descriptions of the medical record system, routine laboratory tests including urinalysis were normal; fluoroscopy exhibited that the DJS was abnormally close to the spine, and plain CT revealed that the proximal end of the DJS was located in the IVC and the distal end penetrated and was attached to the distal ureter. After surgeons failed to find the distal end of the DJS in the bladder and collecting system in cystoscopy and ureteroscopy, an exploratory operation was performed using an extraperitoneal approach through an oblique incision of the right lower rectus abdominis muscle. The lower ureter, IVC, and external iliac vein were exposed, then the DJS was touched in the internal iliac vein. The distal end was located under the serosa of the distal ureter. The DJS was retracted completely without uncontrollable bleeding and thrombosis inside the stent. During a 1-year follow-up, the patient did not complain of any specific signs of hemorrhage, infection, or thrombotic complications, including fever, abnormal pain, anemia, and dyspnea. The semiannual ultrasound was clean.
Case 2
In 2019, a 75-year-old woman with a history of postoperative recurrence of endometrial carcinoma was admitted to our hospital for chemotherapy. The physical examination showed mild percussion pain in her right flank region. Blood and urine routines were normal. A PET-CT showed the invaded right ureter, bladder, and adjacent intestine and the dilated right hydronephrosis ureter. After consulting with our urologist, a retrograde cystoscopic DJS placement was determined to be performed directly without further contrast imaging. Obvious resistance emerged when the hydrophilic guidewire went up about 10 cm. With an increased thrust, the guidewire went up smoothly after a sense of breakthrough; then, a DJS was placed along the guidewire without obvious postoperative complications. No on-table fluoroscopy or ultrasound was performed during the whole procedure.
After the procedure, the patient developed a fever, reaching 38.4°C. A blood routine showed mild elevated WBC, and urinalysis showed slight microscopic haematuria. An ultrasound revealed that her right hydronephrosis was the same as before, and there was no stent echo in her renal pelvis. An x-ray image hinted at a DJS malposition (Figure 2). A plain CT scan showed that the proximal end of the stent was located in the IVC at the level of upper renal polar (Figure 3). Approximately a week after the placement, the location of the distal coil was found to be intravesical under the cystoscope, and the DJS was slowly and integrally removed with retrieval forceps. After that, a percutaneous nephrostomy and catheterization were performed. The patient’s vital signs were stable all the time, and no hemorrhage symptoms such as tachycardia, unstable blood pressure, or abdominal pain occurred. After 8 months of follow-up, the patient is still on regular chemotherapy with normal renal function. The same as Case 1, the patient did not complain of specific signs; also, regular blood tests and ultrasound showed no abnormality.

Figure 2. X-ray screening of a double J stent (DJS) malposition. The location of the DJS was abnormally closed to the spine.
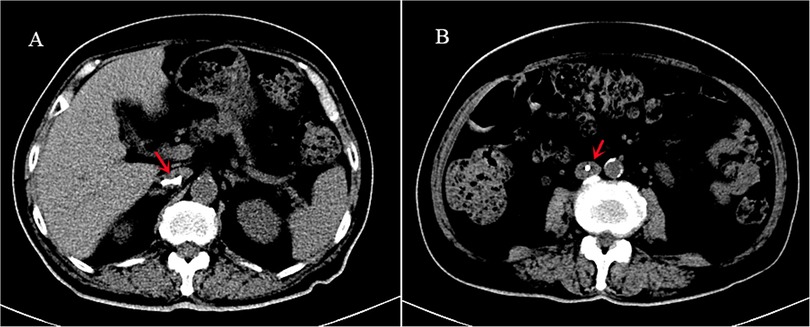
Figure 3. Computed tomography revealing the double J stent malposition (arrow). The proximal coil was at the level of upper renal polar.
Discussion
Michalopoulos et al. (1) first described a DJS intravascular migration case in 2002. There are complications including flank pain, severe gross hematuria, infection, thrombosis, and so on. In the worst situation, the DJS may migrate to the cardiac and pulmonary vascular system following the blood cycle, rendering acute pulmonary embolism, tricuspid regurgitation, and endocarditis (1–4). To common sense, patients should tend to develop hematuria due to the connection between the vascular and urinary systems established by the DJS. However, surprisingly, many reports, including our cases, only disclosed microscopic or even no hematuria (2, 3, 5, 6) (Table 1). This situation is considered due to an obstructive clot inside the DJS (5). In addition, abnormal persistent flank, back pain, and high fever also hint at the existence of DJS malposition (4, 7–9) (Table 1). According to Tang’s (5) view, the intrapelvic pressure is naturally higher than that of the IVC (5–12 cm H2O), especially when there is obstructive hydronephrosis (even more than 22 cm H2O). Therefore, urine is more likely to reflux to blood rather than the opposite, which may lead to infection. In our cases, neither of them complained about abnormal pain and haematuria; only mild fever occurred in Case 2, which proved that the complication could be so covert. In addition, fever due to vesicoureteral reflux is easily seen after DJS placement. Our report reminds urologists of the possibility of urine reflux into the circulatory system directly.
In both of our cases, the DJSs were located in the IVC eventually. The reported locations of intravascular malposition of the DJS include the external iliac vein (3), IVC (6), ovarian vein (7), right ventricle (2, 10), right atrium (4), and pulmonary artery (1). For most situations, the malposition of DJS occurs on the right side (71.4% vs. 28.6%) (Table 1), the same as our facts that both cases occurred on the right side. The stent might break into the IVC through the right iliac vein or directly from the ureter; however, there were also cases that went through left disease (Figure 4) (9, 11). All postoperative x-ray examinations screened DJS malposition, which was aberrantly close to the spine. Our cases further proved this specific imagiological feature.
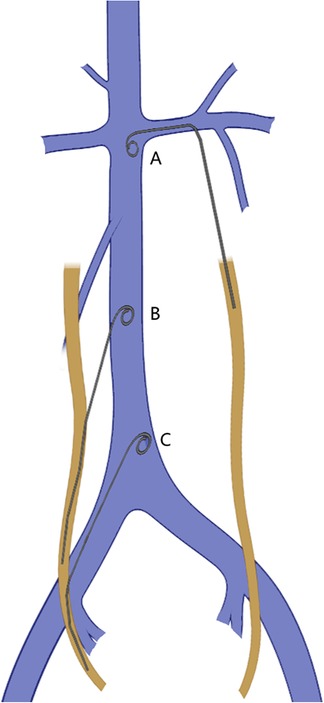
Figure 4. Common pathways for double J stents (DJSs) to enter the inferior vena cava (IVC). (A) through the left renal vein; (B) directly breaking into the IVC through the right ureter; (C) migration to the IVC via the right iliac vein.
Underlying reasons
We comprehensively analyze the underlying reasons, mainly related to the perforation of the ureter led by myriad factors (1): (1) Ureteral factors—Various kinds of damage to the ureter, such as calculus, chronic inflammation, malignant tumor, and pelvic surgery, may not only escalate its fragility but also cause ureteral stricture, which increases the resistance of DJS placement (8, 11). (2) The properties of guidewires and stents—If there is a mismatch between the guidewire and the stent, like the inner diameter of the DJS is too thick, it will not fit the guidewire perfectly, which will make it not amenable to insert and increase the risk of ureteral penetration. In addition, a blunt-end design can help to prevent penetration (Figure 1C). (3) Iatrogenic factors—Injury during lithotripsy and violent operation will lead to ureteral perforation. Following the standard steps of DJS placement is also of much importance, or the patient may develop unprecedented complications. In addition, an inappropriate pre- and intraoperative decision is also an important reason. A poor ureter condition is a common cause of failure in DJS placement, which requires a judicious termination of operation and then performing a nephrostomy instead. In addition, abrupt increases in intraabdominal pressure are also considered to be a factor in promoting the DJS shift (1). It should be noted that intraoperative fluoroscopy can timely reveal the DJS malposition.
In our cases, both the calculus in Case 1 and tumor infiltration in Case 2 could make the ureter more fragile and narrow. In addition, the DJS in Case 1 was not a blunt-end design and did not match the guidewire properly, which added much difficulty to the procedure. Moreover, there was obvious resistance before penetration. The absence of related knowledge and reckless operation against the resistance were notably important reasons in our cases.
Prevention
To avoid this serious complication, physicians ought to evaluate the difficulty of insertion and the risk of ureteral perforation before surgery. Preoperative urography can provide a simple impression of ureteral conditions; however, to the best of our knowledge, the DJS can be placed successfully even if the urography presents a very narrow ureteral lumen. Ureteroscopic operation is recommended, especially when the resistance is abnormal during placement under a cystoscope, to reduce the risk caused by unidentified ureteral perforation. Unfortunately, there are reports of the DJS migrating to the IVC under ureteroscopic surgery, which was explained by the poor surgical view field (12, 13). Intraoperative C-arm fluoroscopy is optional to be performed if available and necessary. Postoperative x-ray is recommended, with which clinicians can carefully confirm the position of the stent. When an x-ray is not suitable, such as for pregnant women, an ultrasound as an alternative can safely confirm whether the guidewire and DJS are correctly located in the renal pelvis and bladder (2).
Treatment
Regarding the treatment for DJS malposition, whether secondary thrombosis exerts a significant influence on decision-making needs to be confirmed. Therefore, contrast CT scanning should be performed when this complication is confirmed, which we did not notice and was risky. Tilborghs et al. (8) summarized that pharmacomechanical thrombolysis is indicated when vital signs are stable, there is no retroperitoneal hemorrhage or active bleeding focus, and adhesions are not present. Otherwise, urgent surgical thrombectomy should be considered. Before and after the surgical removal of the DJS, adequate prophylactic anticoagulation was recommended and adopted by many centers (1, 6, 9, 12, 13), although there is no consensus at present. In our cases, no prophylactic anticoagulant was prescribed, and patients did not present signs of thrombosis complications during follow-up. Considering the adverse effect of anticoagulants, we believe that the administration should be based on an individualized evaluation.
The removal method mainly depends on the position of the distal coil, the patient's general condition, and the available infrastructure (6). Removing an intravesical DJS endoscopically is feasible when there is no thrombosis and retroperitoneal hemorrhage. Previous reports (2, 6, 8) and our experience present that it is still a minimally invasive and safe choice when the surgical and anesthesia teams are fully prepared to cope with severe internal bleeding that may occur at any time. Tilborghs et al. (8) performed an immediate postoperative inferior venocavagraphy, which showed limited contrast leakage from the perforation site. On the opposite, emergency intervention or open surgery should be performed when the DJS completely enters the vascular system and cannot be found endoscopically. Open cardiothoracic surgery with cardiopulmonary bypass is crucial and the first choice, especially when patients have unstable vital signs and severe complications. Before surgery, it should be noticed that excessive encrustation is likely to form around the DJS. Extracorporeal shock wave lithotripsy or holmium laser can eliminate encrustation, which may fix the stent and make removing it difficult (10).
The advantages of our reports are that we provided two rare cases of DJS malposition in the IVC and tried to review every published report. Then, we summarized the underlying causes, prevention, and treatment methods, which we considered helpful to clinical practice. However, there are also a few limitations: We could only get information about Case 1 by retrieving the medical record because a long time has passed, so we could not provide any radiological evidence. Some references are outdated because DJS malposition is a rare complication and lacks authoritative guidelines.
Conclusion
DJS placement is a common procedure in the urological department, but it should be noted that there is a possibility of ureteral perforation and even DJS malposition in the vascular system.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
QW is responsible for collecting data and writing the article. CS and YZ are responsible for reviewing the article and proofreading English. BY and LW are responsible for the revision of the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors appreciate Dr. Yang’s teaching as a decent and responsible tutor.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Michalopoulos AS, Tzoufi MJ, Theodorakis G, Mentzelopoulos SD. Acute postoperative pulmonary thromboembolism as a result of intravascular migration of a pigtail ureteral stent. Anesth Analg. (2002) 95(5):1185–8. doi: 10.1097/00000539-200211000-00011
2. Farshi AR, Roshandel MR. Intracardiac migration of ureteral double-J stent: a case report and review. Can Urol Assoc J. (2015) 9(9-10):E661–64. doi: 10.5489/cuaj.2884
3. Ioannou CV, Velegrakis J, Kostas T, Georgakarakos E, Touloupakis E, Anezinis P, et al. Caval migration of a ureteral J-stent after simultaneous ureter and iliac vein perforation during its placement for obstructive pyelonephritis. Int Angiol. (2009) 28(5):421–4. PMID: 19935599
4. Hajji M, Bennani MS, Bekkali S, Jroundi L. Intracaval migration of ureteral stent. J Belg Soc Radiol. (2015) 99(1):28–30. doi: 10.5334/jbr-btr.842
5. Tang Z, Li D, Xiao L, Wan Y, Luo K, Huang L, et al. Re: intracaval migration: an uncommon complication of ureteral double-J stent placement. (From: Falahatkar S, Hemmati H, Gholamjani Moghaddam K. J Endourol (2012) 26:119–121). J Endourol. (2012) 26(8):1100–1; author reply 02. doi: 10.1089/end.2012.0038
6. Marques V, Parada B, Rolo F, Figueiredo A. Intracaval misplacement of a double-J ureteral stent. BMJ Case Rep. (2018) 2018:bcr2017221713. doi: 10.1136/bcr-2017-221713
7. Kim TN, Lee CH, Kong DH, Shin DK, Lee JZ. Misplacement or migration? Extremely rare case of cardiac migration of a ureteral J stent. Korean J Urol. (2014) 55(5):360–62. doi: 10.4111/kju.2014.55.5.360
8. Tilborghs S, Vaganée D, De Wachter S, Hoekx L. Intravascular double J stent migration: a case report, review, and management algorithm. Urol Ann. (2019) 11(1):93–7. doi: 10.4103/UA.UA_52_18
9. Jiang C, Fu S, Chen J, Chen Y, Chen D, Mishra P, et al. Migration of a double J stent into the inferior vena cava: a case report. Medicine (Baltimore). (2019) 98(20):e15668–e68. doi: 10.1097/MD.0000000000015668
10. Hastaoglu IO, Tokoz H, Kavlak E, Bilgen F. Double J ureteral stent displaced through the right ventricle. Interact Cardiovasc Thorac Surg. (2014) 18(6):853–4. doi: 10.1093/icvts/ivu037
11. Falahatkar S, Hemmati H, Gholamjani Moghaddam K. Intracaval migration: an uncommon complication of ureteral double-J stent placement. J Endourol. (2012) 26(2):119–21. doi: 10.1089/end.2011.0469
12. Arab D, Ardestani Zadeh A, Eskandarian R, Asaadi M, Ghods K. An extremely rare complication of ureteral pigtail stent placement: a case report. Nephrourol Mon. (2016) 8(3):e36527–e27. doi: 10.5812/numonthly.36527
Keywords: double j stent, malposition, intravascular migration, complication, treatment
Citation: Wang Q, Shen C, Zhang Y, Wen L and Yang B (2022) Double J stent malposition in the inferior vena cava: Two case reports and a literature review. Front. Surg. 9:910572. doi: 10.3389/fsurg.2022.910572
Received: 1 April 2022; Accepted: 30 September 2022;
Published: 21 October 2022.
Edited by:
Sajid Sultan, Sindh Institute of Urology and Transplantation, PakistanReviewed by:
Bashir Ahmed Qureshi, Sindh Institute of Urology and Transplantation, PakistanSadaf Aba Umer Kodwavwala, Sindh Institute of Urology and Transplantation, Pakistan
© 2022 Wang, Shen, Zhang, Wen and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Yang ZHltbnliQGhvdG1haWwuY29t
†These authors contributed to the work equally and should be regarded as co-first authors
‡ORCID Qihua Wang orcid.org/0000-0001-9868-8277 Chen Shen orcid.org/0000-0002-3396-7141 Bo Yang orcid.org/0000-0002-9449-1167
Specialty Section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
 Qihua Wang
Qihua Wang Chen Shen
Chen Shen Yue Zhang
Yue Zhang Bo Yang
Bo Yang