- 1Department of Ultrasound, Shaoxing People's Hospital, Shaoxing, China
- 2Department of Hepatobiliary and Pancreatic Surgery, Shaoxing People's Hospital, Shaoxing, China
- 3Shaoxing Key Laboratory of Minimally Invasive Abdominal Surgery and Precise Treatment of Tumor, Shaoxing, China
Congenital pelvic arteriovenous malformation (AVM) is a rare vascular abnormality whereby arteries and veins are directly connected with malformed vascular plexus. Owing to its low incidence and nonspecific symptoms, the ultrasonographic characteristics of congenital pelvic AVM in males have been infrequently studied. A 30-year-old man visited our hospital complaining of progressive pain in the right lower abdomen and lumbar area since 2 months previously. Abdominal ultrasound (US) was performed at the initial examination and pelvic AVM was diagnosed, which was then confirmed by computed tomographic angiography. After right internal iliac artery embolization, the patient recovered uneventfully and remained asymptomatic during the 12-month follow-up period. Congenital pelvic AVM should thus be included in the differential diagnosis of pelvic cystic masses in males despite its low incidence, with US also being of great diagnostic value. We describe the ultrasonic features of AVM in detail and hope that this study may contribute to the ultrasonic diagnosis of congenital pelvic AVM in males.
Introduction
Pelvic arteriovenous malformation (AVM) is a rare vascular abnormality whereby arteries and veins are connected with a nidus of dysplastic vascular channels, and it is particularly rare in male patients (1). As most pelvic AVMs are secondary to trauma, prior surgery, or tumor, congenital pelvic AVMs in males are even rarer (2–4).
There have been some studies on congenital pelvic AVM in the last few decades despite its low incidence. However, previous studies (Table 1) mainly affirmed the value of computed tomography (CT) and angiography, whereas ultrasound (US) was rarely characterized in detail despite it being the preferred initial examination owing to the advantages of low cost, convenience and easy operation. Moreover, the symptoms of pelvic AVM are nonspecific and include flank, abdominal or pelvic pain, hematuria, hemospermia, impotence, and dysuria (5), leading to difficulties in diagnosis. Therefore, the ultrasonographic characteristics of congenital pelvic AVM in male patients have been infrequently studied by clinicians.
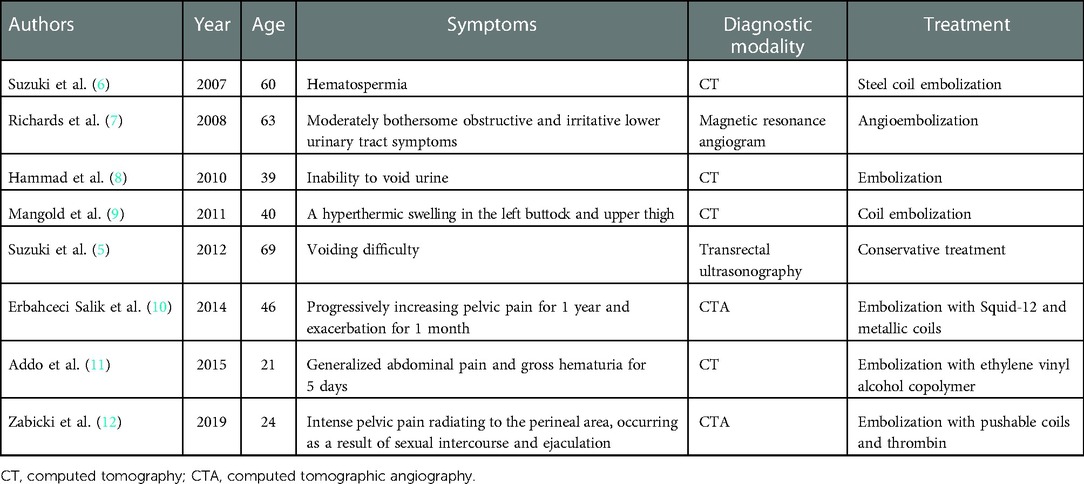
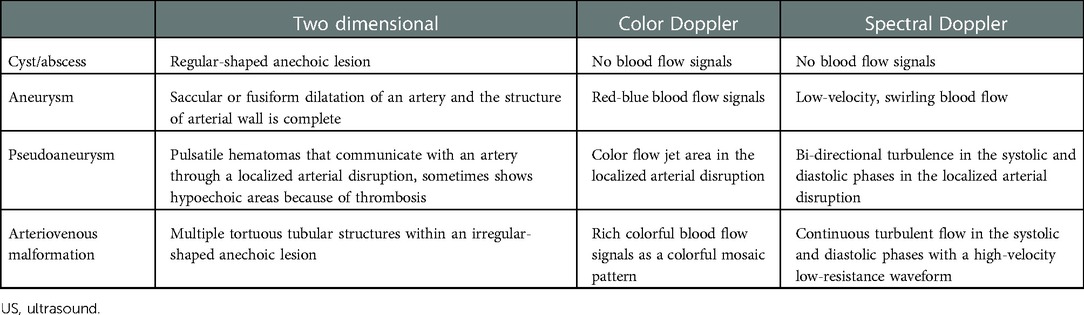
Table 1. Synopsis of the presenting symptoms, diagnostic modalities, and therapeutic strategies of the eight congenital pelvic arteriovenous malformations developed in male patients.
Against this background, we present a rare case of congenital pelvic AVM diagnosed by abdominal US and discuss the ultrasonic features for diagnosis. This work may contribute to the ultrasonic diagnosis of congenital pelvic AVM in the male population.
Case presentation
A 30-year-old man visited our hospital with a complaint of progressive persistent colic in the right lower abdomen and lumbar area over a period of 2 months, with no fever, nausea, vomiting, frequency/urgency of urination, urodynia, or hematuria. The causative factor was unclear. The patient denied a history of tumor, trauma, or previous surgery. Physical examination was normal with no tenderness or rebound tenderness in the abdomen, and no palpable mass was found. Laboratory investigations (routine blood and biochemical analysis, and tumor markers) were unremarkable. As the initial imaging examination, abdominal US revealed multiple tortuous tubular structures within an irregularly shaped anechoic lesion (62 mm × 56 mm) located on the right side of the bladder. Color Doppler flow imaging (CDFI) displayed rich colorful blood flow signals as a colored mosaic pattern in the same lesion, and spectral Doppler showed continuous turbulent flow in the systolic and diastolic phases with a high-velocity low-resistance waveform (Figure 1). In the context of these imaging features, pelvic AVM was suspected.
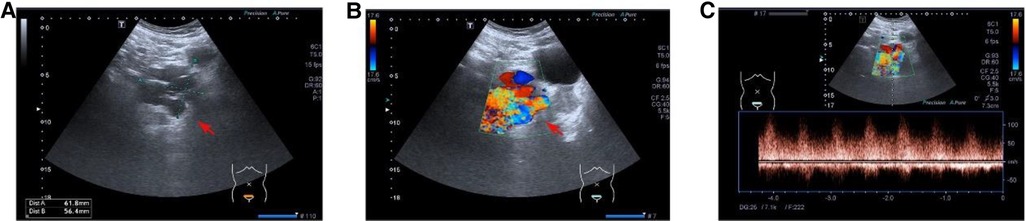
Figure 1. (A) Multiple tortuous tubular structures within an irregularly shaped anechoic lesion were revealed by B-mode ultrasound. (B) Color Doppler flow imaging displayed rich colorful blood flow signals as a colored mosaic pattern. (C) Spectral Doppler showed continuous turbulent flow in the systolic and diastolic phases with a high-velocity low-resistance waveform.
The patient underwent computed tomographic angiography (CTA) after the sonographic diagnosis of pelvic AVM, whereby a large pelvic AVM supplied mainly by the right internal iliac artery was found (Figure 2), thus confirming the final diagnosis of pelvic AVM. He was then admitted for transcatheter embolization. The preoperative laboratory examinations were within normal limits. When arteriography indicated feeding arteries arising from the right internal iliac artery, the right internal iliac artery was embolized by spring coils (Figure 3). The patient recovered uneventfully after embolization. He remained asymptomatic during the follow-up period and was re-examined with abdominal US 19 months after embolization, in which the pelvic AVM decreasing in volume and the systolic blood flow velocity reduction were revealed (Figure 4).
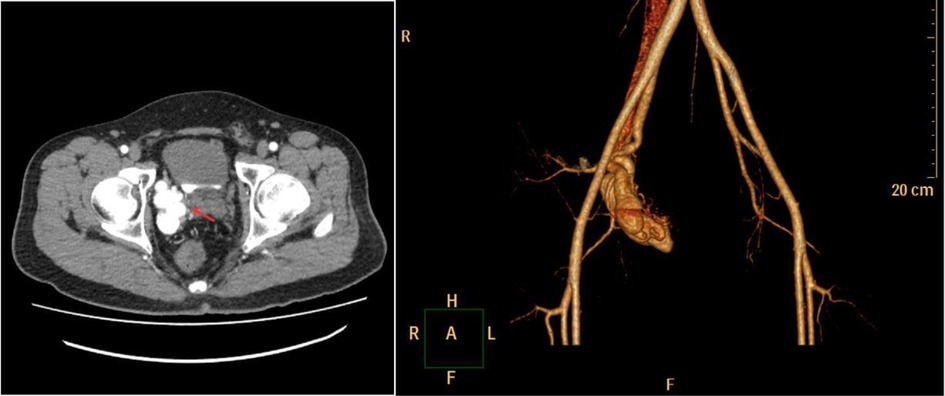
Figure 2. Computed tomographic angiography showed a large pelvic arteriovenous malformation (red arrow) supplied mainly by the right internal iliac artery.

Figure 3. (A) Arteriography demonstrated pelvic arteriovenous malformation and feeding arteries arising from the right internal iliac artery. (B) Arteriography postembolization.
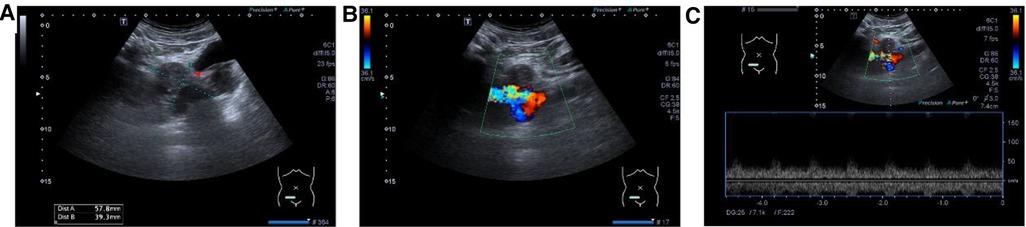
Figure 4. (A) Part of the irregularly shaped anechoic lesions became hypoechoic (red arrow) in the B-mode ultrasound. (B) Color Doppler flow imaging showed the colored mosaic pattern decreased in volume. (C) Spectral Doppler showed the systolic blood flow velocity is reduced after embolization.
Discussion
Pelvic congenital AVMs in males are relatively rare. In 2002, Game et al. (2) reported 2 cases of pelvic congenital AVMs in male patients and reviewed 15 previously published cases, after which only 8 more cases (listed in Table 1) have been reported to date. Here, we present a rare case report of a male congenital pelvic AVM diagnosed by abdominal US with a detailed description of the US findings, hoping this work may contribute to the ultrasonic diagnosis of congenital pelvic AVMs.
The malformed vascular plexus formed by the remnant capillary network constitute the structures between the arterial and venous systems. AVM may occur in any part of the body but mainly in the brain, neck, lung, and kidney. Pelvic AVMs are relatively rare, especially in males. The presenting symptoms of pelvic AVM are nonspecific and can be either subtle or dramatic and may even be fatal (13). Both the low incidence and low specificity of the symptoms make the early clinical diagnosis difficult. Although palpating a pulsatile mass and hearing loud or harsh noises on physical examination is a significant indication of pelvic AVM (2), not all masses may be palpable, and rectal examination is not routine. In addition, AVM might not be diagnosed during routine examination (14), contributing to a diagnostic dilemma.
Despite the fact that abdominal US is usually the initial routine imaging examination, according to previous literature reports, the diagnostic value of US remains questionable with regard to male congenital pelvic AVM. Game et al. (2) considered that US could only show a nonspecific hypoechogenic area and was not able to differentiate an AVM from a cyst or an abscess. Aslan et al. (14) suggested that the US characteristics of AVM are nonspecific but could alert the sonographer to the possibility of a vascular abnormality. Although previous literature has reported congenital AVM diagnosed by transrectal US in which a pulsating mass was palpable on rectal examination, the US features of AVM were not described in detail (5). Moreover, in most previous articles, US only detected the lesions while being unable to make the diagnosis of AVM (6, 12).
In contrast to previous literature, we believe that, with the application of Doppler, US is also a potential tool of solid diagnostic value for congenital pelvic AVM in males. Mittal et al. (15) considered that US and Doppler imaging could be used to diagnose vascular anomalies. In the present case, we found multiple tortuous tubular structures within an irregularly shaped anechoic lesion on gray-scale ultrasonography. To help differentiate this from a cyst or abscess, CDFI was also performed, whereby rich colorful blood flow signals were revealed in the same lesion; by contrast, cysts or abscess cavities lack the presence of vascularity and color flow. Aneurysms and pseudoaneurysms share some characteristics with AVM on US because they are all hypervascularized, but they also have their own unique features (as listed in Table 2) and can be differentiated by US.
The treatment options of congenital pelvic AVM in males depend on the severity of presenting symptoms, and asymptomatic or mildly symptomatic lesions are considered not to require therapy (2). A variety of therapies, including ligation of the afferent arteries, excision of the lesion, and embolization, have been used to treat AVM in male patients. However, a surgical approach has been reported to be usually unsuccessful and complicated by hemorrhage, adjacent organ damage, and recurrence (16, 17). In contrast, a lower rate of morbidity, mortality, and invasiveness makes embolization the preferred treatment (18). The goal of embolization is the elimination of the AVM nidus (12). Various embolic materials have been used to treat AVM lesions, including metallic coils, absolute ethanol, ethylene vinyl alcohol copolymers, and rapidly polymerizing acrylic adhesives (18–20). Improved catheters, the use of superselective techniques, and liquid embolic agents have been reported to be effective in treating AVMs, which may provide the best long-term result (18, 21, 22). The patient in our study complained of progressive pain in the right lower abdomen and lumbar area, which eventually became unbearable and could not be relieved by rest. Because he has not yet completed his childbearing and strongly desired fertility despite the risk of recurrence, we used coil embolization of the right internal iliac artery, which only relieved the symptoms but not eliminated the AVM nidus. Therefore, a tight follow-up is essential, and the patient may need further treatment after his childbearing.
Conclusions
We presented the case of a male congenital pelvic AVM first diagnosed by abdominal US. Furthermore, we described the ultrasonic features of AVM in detail and established some key points of differential diagnosis by US in pelvic cystic masses, rarely mentioned in previous literature. For pelvic cystic masses found on two-dimensional US, color Doppler and spectral Doppler are necessary for further differential diagnosis. Furthermore, congenital pelvic AVM should be included in the differential diagnosis of pelvic cystic masses in males despite its low incidence.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Shaoxing People's Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YH collected the images and wrote the manuscript. HQ collected the clinical data and was responsible for follow-up work. XL contributed to revising the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The work was sponsored by Shaoxing Medical Key Discipline (2019SZD05). The funders had no influence on the analysis or publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AVM, arteriovenous malformation; US, ultrasound; CT, computed tomography; CDFI, color Doppler flow imaging; CTA, computed tomographic angiography.
References
1. Lam K, Pillai A, Reddick M. Peripheral arteriovenous malformations: classification and endovascular treatment. Appl Radiol. (2017) 46:15–22. doi: 10.37549/AR2379
2. Game X, Berlizot P, Hassan T, Joffre F, Chokairi S, Houlgatte A, et al. Congenital pelvic arteriovenous malformation in male patients: a rare cause of urological symptoms and role of embolization. Eur Urol. (2002) 42:407–12. doi: 10.1016/S0302-2838(02)00355-X
3. Tufano A, Minelli R, Rossi E, Brillantino C, Di Serafino M, Zeccolini M, et al. Inferior epigastric artery pseudoaneurysm secondary to port placement during a robot-assisted laparoscopic radical cystectomy. J Ultrasound. (2021) 24:535–8. doi: 10.1007/s40477-020-00442-1
4. Tufano A, Asero V, Proietti F, Flammia RS, Franco G, Leonardo C. Arteriovenous fistula after robotic partial nephrectomy: case report and narrative review. Radiol Case Rep. (2022) 17:2550–3. doi: 10.1016/j.radcr.2022.04.038
5. Suzuki K, Tanaka N, Ebine T, Momma T. Pelvic congenital arteriovenous malformation diagnosed by transrectal ultrasonography: a case report. Can Urol Assoc J. (2012) 6:E61. doi: 10.5489/cuaj.10190
6. Suzuki K, Nishimi D, Morioka H, Takanami M. Hematospermia associated with congenital arteriovenous malformation of internal iliac vessels. Int J Urol. (2007) 14:370–2. doi: 10.1111/j.1442-2042.2007.01576.x
7. Richards AJ, Hatrick A, Eden CG. Large pelvic arteriovenous malformation complicating laparoscopic radical prostatectomy. Urology. (2008) 72:1359–61. doi: 10.1016/j.urology.2008.01.001
8. Hammad FT, Shawish F, Kazim E. Congenital pelvic arteriovenous malformation presenting with urinary retention: a case report. Med Princ Pract. (2011) 20:294–6. doi: 10.1159/000323837
9. Mangold S, Ketelsen D, Syha R, Balletshofer B, Kalender G, Kramer U, et al. Endovascular treatment of a real inferior gluteal artery aneurysm associated with a pelvic arteriovenous malformation. Cardiovasc Intervent Radiol. (2011) 34:1102–5. doi: 10.1007/s00270-011-0131-0
10. Erbahceci Salik A, Islim F, Akgul A, Cil BE. Concomitant transarterial and transvenous embolization of a pelvic arteriovenous malformation using a new liquid embolic agent, squid-12 and detachable coils. Case Rep Vasc Med. (2014) 2014:972870. doi: 10.1155/2014/972870
11. Addo EA, Emtage J, Massis K, Hernandez DJ. A congenital high flow arteriovenous malformation of the bladder presenting with polypoid cystitis and ureteral obstruction. Urol Case Rep. (2015) 3:181–4. doi: 10.1016/j.eucr.2015.07.004
12. Zabicki B, Holstad MJV, Limphaibool N, Juszkat R. Endovascular therapy of arteriovenous malformation in a male patient with severe post-coital pelvic pain. Pol J Radiol. (2019) 84:e258–61. doi: 10.5114/pjr.2019.86893
13. Guida M, Maffucci D, Iannuzzi G, Giordano M, Luciano G, Di Benedetto L, et al. Successful pregnancy after uterine artery embolization for uterine arterovenous malformation: a rare case report. Int J Womens Health. (2018) 10:745–50. doi: 10.2147/IJWH.S182131
14. Aslan H, Acar DK, Ekiz A, Kaya B, Sezer S, Ismayilzade R, et al. Sonographic features and management options of uterine arteriovenous malformation. A case report. Med Ultrason. (2015) 17:561–3. doi: 10.11152/mu.2013.2066.174.sgh
15. Mittal A, Anand R, Gauba R, Choudhury SR, Abbey P. A step-by-step sonographic approach to vascular anomalies in the pediatric population: a pictorial essay. Indian J Radiol Imaging. (2021) 31:157–71. doi: 10.1055/s-0041-1729486
16. Pritchard DA, Maloney JD, Bernatz PE, Symmonds RE, Stanson AW. Surgical treatment of congenital pelvic arteriovenous malformation. Mayo Clin Proc. (1978) 53:607–11.682689
17. Palmaz JC, Newton TH, Reuter SR, Bookstein JJ. Particulate intraarterial embolization in pelvic arteriovenous malformations. AJR Am J Roentgenol. (1981) 137:117–22. doi: 10.2214/ajr.137.1.117
18. Do YS, Kim Y-W, Park KB, Kim D-I, Park HS, Cho SK, et al. Endovascular treatment combined with emboloscleorotherapy for pelvic arteriovenous malformations. J Vasc Surg. (2012) 55:465–71. doi: 10.1016/j.jvs.2011.08.051
19. Jacobowitz GR, Rosen RJ, Rockman CB, Nalbandian M, Hofstee DJ, Fioole B, et al. Transcatheter embolization of complex pelvic vascular malformations: results and long-term follow-up. J Vasc Surg. (2001) 33:51–5. doi: 10.1067/mva.2001.111738
20. Castaneda F, Goodwin SC, Swischuk JL, Wong GCH, Bonilla SM, Wang MJ, et al. Treatment of pelvic arteriovenous malformations with ethylene vinyl alcohol copolymer (onyx). J Vasc Interv Radiol. (2002) 13:513–6. doi: 10.1016/S1051-0443(07)61532-2
21. Bae S, Do YS, Shin SW, Park KB, Kim D-I, Kim YW, et al. Ethanol embolotherapy of pelvic arteriovenous malformations: an initial experience. Korean J Radiol. (2008) 9:148–54. doi: 10.3348/kjr.2008.9.2.148
Keywords: congenital arteriovenous malformation, male, pelvis, urology, case report, ultrasound
Citation: Huang Y, Liu X and Qian H (2023) A male congenital pelvic arteriovenous malformation diagnosed by abdominal ultrasound: A case report and literature review. Front. Surg. 9:907234. doi: 10.3389/fsurg.2022.907234
Received: 29 March 2022; Accepted: 9 December 2022;
Published: 9 January 2023.
Edited by:
Stavros K. Kakkos, University of Patras, GreeceReviewed by:
Tej Mehta, Johns Hopkins Medicine, United StatesReza Shahriarirad, Shiraz University of Medical Sciences, Iran
Peng Teng, Zhejiang University, China
Wayne Yakes, The Yakes Vascular Malformation Center, United States
Antonio Tufano, Sapienza University of Rome, Italy
© 2023 Huang, Liu and Qian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongwei Qian cWh3c3hzcm15eUAxNjMuY29t Xiatian Liu bHh0MjAxNUAxMjYuY29t
Specialty Section: This article was submitted to Vascular Surgery, a section of the journal Frontiers in Surgery
 Yanhua Huang1
Yanhua Huang1 Xiatian Liu
Xiatian Liu Hongwei Qian
Hongwei Qian