- Department of Trauma and Orthopedics, Peking University People’s Hospital, Beijing, China
Background: Proximal humeral migration is common in patients with rotator cuff tears. In this study, we aimed to evaluate the relevance between proximal humeral migration and some rotator cuff tear-related factors.
Methods: A total of 75 patients with unilateral rotator cuff tears were retrospectively included from August 2016 to January 2018 who underwent magnetic resonance imaging and X-ray examinations before enrollment. We introduced the upward migration index (UMI) to stratify the patients into three groups, Group A: 1 < UMI ≤ 1.3; Group B: 1.3 < UMI ≤ 1.4; and Group C: UMI > 1.4. Pearson correlation analysis and logistic regression analysis were used to evaluate the relationship between UMI and age, sex, body mass index, pain, fatty degeneration grade, tear size, and thickness of ruptured tendon. Then, the χ2 test and receiver operator characteristic curve were applied to measure the diagnostic value of UMI.
Results: The average UMI was 1.34 ± 0.07, ranging from 1.16 to 1.48. For the Pearson correlation analysis, there was a negative correlation between UMI and tear size (R = −0.68, p < 0.01), and also, there was a negative correlation between UMI and the visual analogue scale score (R = 0.342, p < 0.01). What is more, there was a negative correlation between UMI and the fatty degeneration grade (R = −0.373, p < 0.01). Ordinal multinomial logistic regression analysis indicated that tear size (β = −1.825, p < 0.001) was the independent predictor of UMI, which was a risk factor for humeral upward migration. The cutoff points of UMI were 1.38 and 1.3 to determine tears and distinguish large tears from small ones.
Conclusions: UMI is a good predictor for humeral upward migration, which is related to the tear size of posterosuperior cuff tears. When the UMI is <1.3, a large tear should be alerted. Combining physical examination and X-ray is helpful for evaluating rotator cuff tears.
Introduction
Proximal humeral migration is common in rotator cuff tear patients, but the detailed mechanism is still unknown (1, 2). The possible reason includes deltoid pulling or spacing missing after rotator cuff tears. Currently, proximal humeral migration mainly depends on the direct measurement of the acromion humeral distance (AHD), which helps shoulder surgeons to evaluate tear severity and make treatment decisions (3). Previous studies have shown that AHD < 7 mm indicated a rotator cuff tear (4, 5). However, the traditional AHD is thought inaccurate in judging humeral migration (6) because the size of the humeral head varies among different genders, ages, heights, weights, and races. So, we introduced the upward migration index (UMI), which was first mentioned in 1996 (7), to evaluate the proximal humeral migration and eliminate the impact of anatomical differences and the magnifying effect of X-rays on subacromial space. Also, we proposed to find out the relationship between the degree of proximal humeral upward migration and other factors, such as tear size and fatty degeneration grade.
Materials and Methods
General Information
This study included patients with unilateral rotator cuff tears from Peking University People’s Hospital from August 2016 to January 2018. All the patients had shoulder pain before treatment. The posterosuperior cuff tears (supraspinatus and infraspinatus) were highly suspected by the physical examination and confirmed by further imaging examination. The inclusion criteria included the following: (1) Magnetic resonance imaging (MRI) of the affected shoulder was performed within half a year before inclusion and confirmed a full-thickness tear of the supraspinatus/infraspinatus with or without tendon retraction. (2) An X-ray examination was performed within half a year before inclusion. (3) The interval between the two examinations should not be longer than 1 month. Additionally, the exclusion criteria were the following: (1) a history of shoulder surgery on the same side; (2) a history of proximal humeral or acromial fractures on the same side; (3) a history of instability or dislocation; (4) tear of subscapularis muscles; and (5) a history of nerve injury on the same limb. Eventually, 75 patients met the criteria, including 38 males and 37 females, with an average age of 64.5 years (range: 35–87 years). The body mass index (BMI) was also recorded. All the patients signed informed consent before enrollment. Fifty-two patients without rotator cuff tears were also included for further comparison.
A standard protocol anteroposterial radiograph was taken of all patients, slightly turned to the image side (20°), and the arm in external rotation with the palm facing forward. The film-focus distance was measured at 115 cm, and a 15° craniocaudal tilt was used to project the undersurface of the acromion perpendicular (8, 9).
All the data were extracted from the electronic database of Peking University People’s Hospital. Proximal migration was measured using the UMI, where the distance between the center of the humeral head and the undersurface of the acromion (CA) was divided by the radius of the humeral head (R) (Figure 1) (9). All the data were measured by orthopedic surgeons trained in shoulder surgery. Finally, patients were assigned into three groups according to the UMI value, namely, Group A: 1 < UMI ≤ 1.3; Group B: 1.3 < UMI ≤ 1.4; and Group C: UMI > 1.4.
Evaluation of the Shoulder Pain
The visual analogue scale (VAS) was applied for pain assessment. Clinically, the total score is 10, with 0 for no pain, 1–3 for mild pain, 4–6 for moderate pain, 7–9 for severe pain, and 10 for unbearable pain.
Magnetic Resonance Imaging
All patients underwent MRI of the shoulder in oblique coronal, oblique sagittal, and axial planes on a 3.0-T Signa scanner (GE Healthcare, Chicago, USA). The size, location, and degeneration degree of the supraspinatus/infraspinatus were estimated through the different planes of MRI. The tear size was obtained on the T2 oblique coronal and oblique sagittal planes with the maximal defect (10, 11). To measure the thickness of teared tendon thickness, the maximal stump of supraspinatus/infraspinatus on the T2 oblique coronal plane. The extent of muscle degeneration was defined as described by Goutallier et al. (12). Grade 0 indicated normal muscle, grade 1 was some fatty streaks, grade 2 was defined as <50% fatty muscle atrophy, grade 3 was 50% fatty muscle atrophy, and grade 4 indicated >50% fatty muscle atrophy. The Goutallier classification was originally intended to describe the performance of computed tomography and expanded later by Fuchs et al. to describe MRI results (13).
Data Analysis
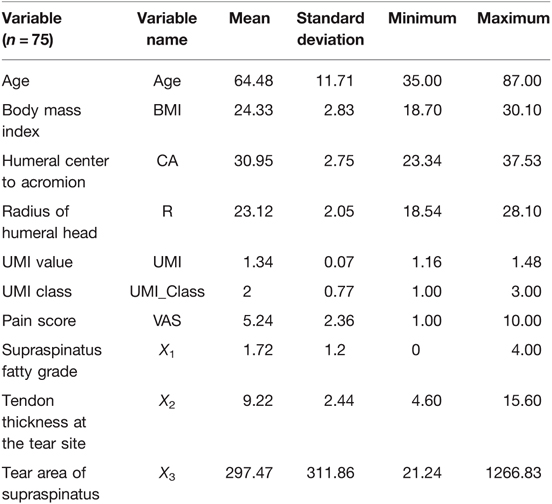
The acronyms are described in Table 1. SPSS Statistics (version 22.0, IBM) was used to analyze data in this study, and the Pearson correlation was used to determine the relationship between the MRI results, other different factors, and UMI grades.
Considering that UMI may be affected by multiple factors, the factors associated with the UMI grade were selected as the independent variables in this study. The UMI grade was regarded as the dependent variable for further ordinal multinomial logistic regression to determine the possible influence and significance.
The receiver operator characteristic (ROC) curves were drawn, with the UMI values defined as the test variables and tear sizes defined as the state variables, to determine the cutoff point of tear sizes. Finally, ROC curves were drawn by combining the UMI values of 52 patients without tears together with the values of patients suffering tears as the test variables and the tear state as the state variables to obtain the cutoff value of the normal UMI grade and so on, which is of great significance for future diagnosis and treatment.
Results
Calculation of Upward Migration Index
According to the method described above, the CA and R values were obtained by the X-ray imaging system. The range of UMI values was 1.16–1.48, with a mean value of 1.34. According to the method defined previously, the patients were divided into three groups. There were 22 patients in group A, 31 patients in group B, and 22 patients in group C.
Scores of Shoulder Pain on the Affected Side of Each Group
The VAS score was obtained from all the 75 patients and ranged from 1 to 10, with an average of 5.24. The mean score of group A was 5.9 (range: 1–10), group B was 5.8 (range: 2–10), and group C was 3.8 (range: 1–3).
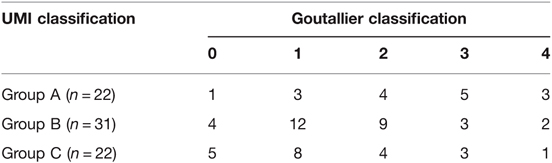
Comparison of Magnetic Resonance Imaging Results of Supraspinatus/Infraspinatus Tear between Different Groups
The size of tear is measured in the oblique sagittal and oblique coronal planes with the largest defect. The mean tear size was 297.47 mm2 (range: 21.24–1266.83 mm2). In group A, the mean tear size was 631.58 mm2 (range: 68–1266.83 mm2). For group B, the mean tear size was 196.23 mm2 (range: 31.68–801 mm2). In group C, the mean tear size was 105.98 mm2 (range: 21.24–348.80 mm2). Because of measurements in millimeters, the variance between different values seemed significantly magnified. So, all the statistical data were converted to the natural logarithmic (ln) and marked as Z3. The tendency of fatty degeneration in supraspinatus/infraspinatus (Goutallier grade 2 or above) was detected in 39 of 75 patients, which concludes 19 cases of grade 2, 13 cases of grade 3, and 7 cases of grade 4. Others included 12 cases of grade 0 and 24 cases of grade 1. The results are listed in Table 2. The mean thickness of the tendon was 9.1 mm (range: 4.6–11.7 mm) in group A, 9.5 mm (range: 5.7–14.7 mm) in group B, and 10.1 mm in group C (range: 6.3–15.6 mm).
Correlation between General Data and the Upward Migration Index of the Humeral Head
Pearson correlation analysis was performed between UMI and other factors in this study, and the results are listed in Table 3. The UMI grade was negatively correlated with the pain score (R = −0.342, p = 0.003). In contrast, the UMI grade had no correlation with age, gender, and BMI, which further proved that the index could minimize the influence of age, gender, height, and some other factors.
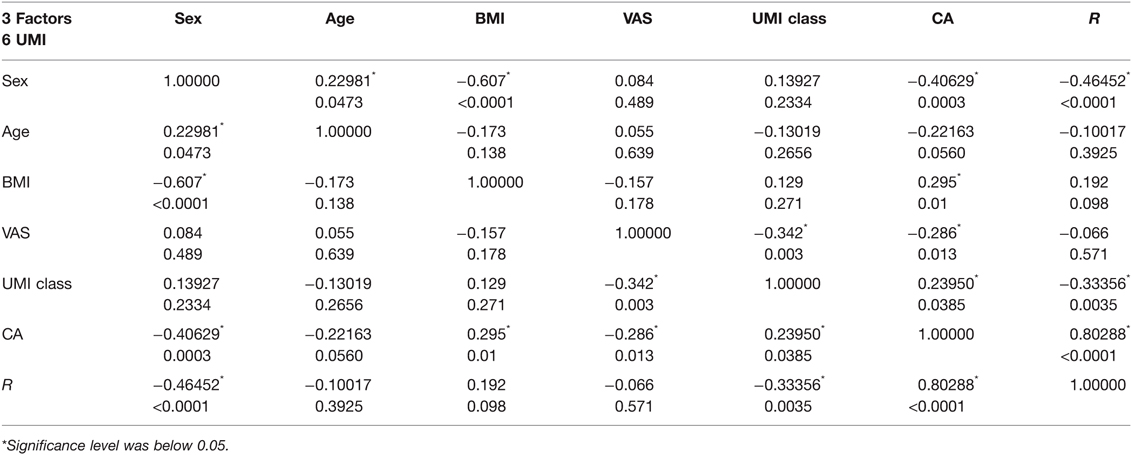
Table 3. Pearson analysis between different factors (the number at the top of each unit is a correlation coefficient, and the value below is a p-value). Gender: male = 1, female = 2.
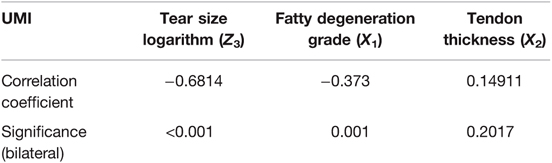
Correlation between Different Magnetic Resonance Imaging Results and Upward Migration Index
The correlation between different MRI results and UMI was presented separately (Table 4). Pearson correlation analysis confirmed a highly negative correlation between the logarithm of the UMI grade and rotator cuff tear area (R = −0.68, p < 0.001). For the UMI grade and fatty degeneration degree of the rotator cuff, the correlation analysis also showed a negative correlation (R = −0.373, p = 0.001). However, there was no correlation between the UMI grade and tendon thickness at the tear side (R = 0.15, p = 0.2017).
Ordinal Multinomial Logistic Regression Analysis
According to the previous analysis, the pain score, tear area, and fatty degeneration were correlated with the UMI grade. Further, ordinal multinomial logistic regression analysis was performed by taking the VAS score, fatty infiltration degree, and tear area of supraspinatus/infraspinatus (logarithmic value) as independent variables and the UMI grade as the dependent variable (Table 5). The goodness-of-fit test verified the validity of the model with χ2 = 65.6 (p < 0.001). Table 5 shows that the odds ratio value was 6.2 (p < 0.001), so the larger the tear of the rotator cuff, the lower the grade of UMI, and the more severely the proximal humerus migrates.
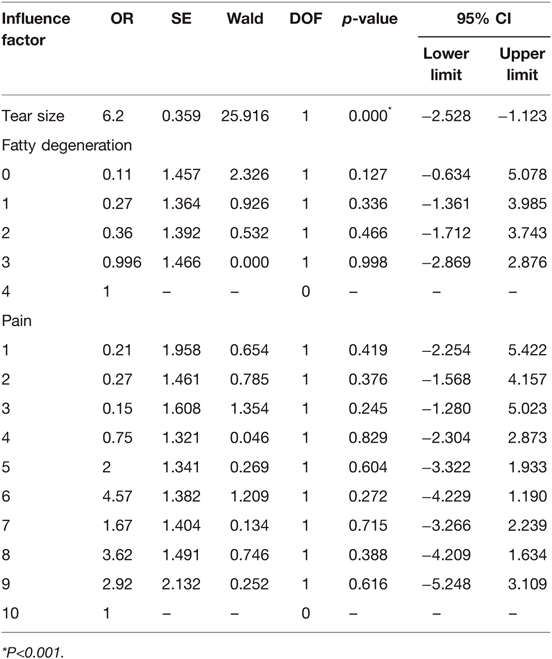
Table 5. Ordinal multinomial logistic regression analysis of factors affecting proximal humeral migration.
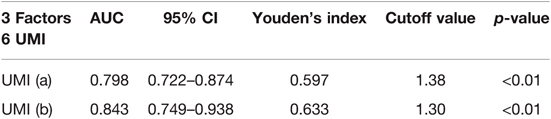
Evaluation of the Value of Upward Migration Index for Predicting Rotator Cuff Tear by the Receiver Operator Characteristic Curve
The UMI values of 52 patients without rotator cuff tears, together with the 75 patients with rotator cuff tears, were used as test variables, and the presence or absence of rotator cuff tear as state variables to draw ROC curves (Figure 2A). By analyzing the sensitivity and specificity at different cutoff points, the points with the largest Youden index were selected as the diagnostic criteria to determine the rotator cuff tear. Hence, the cutoff value was 1.38, as described in Table 6.
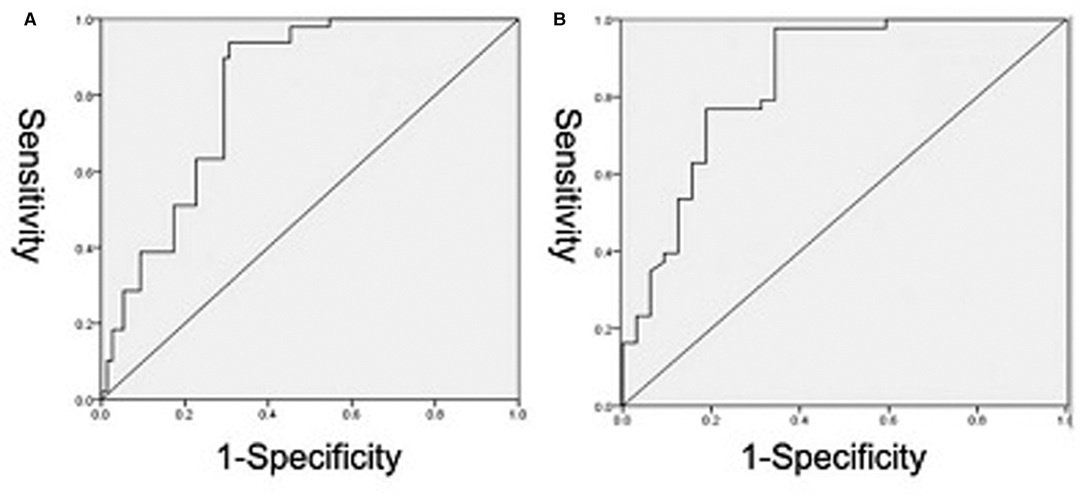
Figure 2. ROC curve to determine the cutoff value of UMI for discriminating tear (A) and tear size (B). The reference line is indicated in green. The values of area under the curve were 0.798 and 0.843, respectively.
When the UMI of the 75 patients with rotator cuff tears worked as the test variable and the tear size classified as 200 mm2 as the state variables, the ROC curve was drawn (Figure 2B). Similarly, the point with the largest Youden index was selected as the diagnostic criterion to determine the rotator cuff tear size; the cutoff value was 1.3 (Table 6).
Discussion
Superior rotator cuff tears can lead to superior humeral migration and subacromial impingement (14). The dynamic changes of the glenohumeral joint occur in the progressive stage of a rotator cuff tear and indicate a poor prognosis (15). However, the natural process and related factors involved in these changes have not been clarified yet. The current judgment of proximal humeral migration mainly depends on the direct measurement of AHD. An arthroscopic study found that the average distance between the humeral head and acromion was 10.5 mm. When the rotator cuff torn, the average distance was reduced to 8.2 mm (16). AHD < 7 mm predicted a larger rotator cuff tear and a dramatic decrease in the success rate of surgical repair (4, 17). Therefore, 7 mm is a widely accepted criterion. However, because of the anatomical differences and X-ray magnification on subacromial spaces, the measurement of AHD directly by an X-ray examination is thought inaccurate. UMI was introduced to evaluate humeral upward migration more reliably and accurately by eliminating the influence of positional and anatomical differences and other factors. By the single-factor correlation analysis, many variables, especially CA and R, were related to age, sex, and BMI, while UMI had no correlation with gender, age, BMI, etc. Therefore, the novel index, UMI = CA/R, was introduced in this study to effectively eliminate the confounding impact of the above factors, which provided a new judging reference for the proximal humeral migration in the future.
The main purpose of this study is to explore the factors resulting in the upward migration of the proximal humerus and analyze their contributions. First, Pearson correlation analyses were carried out, respectively, between the influencing factors and UMI, demonstrating that the tear size of the supraspinatus/infraspinatus muscle, fatty degeneration grade, and VAS score were correlated with the UMI grade. Namely, the larger the tears or more severe the fatty degeneration, the greater the migration of the proximal humerus. To further verify the conclusions, the VAS score, the logarithm of tear size, and the fatty degeneration grade were selected as independent variables and the UMI grade as the dependent variable for ordinal multinomial logistic regression analysis. It suggested that the tear size was an independent factor among all factors; namely, a larger tear size indicated a lower grade of UMI and more severe migration of the proximal humerus. Additionally, when the UMI value was <1.3, more than 90% of patients were found to have a large full-thickness tear (over 200 mm2). However, there were exceptions in this study: a few patients with UMI values >1.3 also displayed large tears, indicating that although the reduced UMI value could reflect the integrity of supraspinatus/infraspinatus, it should not be the only criterion for judging tear severity and treatment options.
In the past decades, many studies emphasized the significant role of early diagnosis and treatment in the improvement of the cuff repair effect (18, 19). Ultrasound and MRI provide a highly specific and accurate diagnosis of the rotator cuff tear, which makes them the main imaging examination. However, in clinical practice, an X-ray is always the first examination in the case of acute shoulder pain because of its convenience and intuitive feature of the bony structure. Hence, the preliminary judgment from the early X-ray is critical for the diagnosis and further treatment. Our study indicated a significant correlation between the UMI and tear size, which partially verified the MRI examination results. Therefore, in the primary outpatient and emergency diagnosis, the reduced UMI value in an X-ray with positive physical examination signs can preliminarily determine the degree of rotator cuff tear. Moreover, when the UMI value is <1.3, a wide range of tear should be highly suspected, which works as an important reference for the early and accurate diagnosis. However, many other factors are also involved in the final choice of treatment and prognosis, such as age, muscle strength, gender, and functional needs, which require surgeons to combine multiple factors to make a judgment, such as the medical history and physical and other examinations.
With regard to the factors affecting the upward migration of proximal humerus, Keener et al. studied the effect of tear size and pain on the dynamics of the glenohumeral joint (20). They found that in addition to size, pain was also associated with the upward migration of the proximal humerus. However, Yamaguchi et al. found that symptomatic and asymptomatic patients with rotator cuff tears both displayed an upward migration of the proximal humerus (18). Hence, the effect of pain is still controversial. For the relationship between fatty degeneration and proximal humeral displacement, Nové-Josserand et al. found that the subacromion space was narrower in the fatty degeneration cases (21). However, normal subacromial space was found in some patients with grade 2 or grade 3 fatty degeneration in our study. Although univariate analysis showed that the fatty degeneration grade and VAS score were correlated with the UMI grade, the correlation was weaker than previously reported. Further ordinal multinomial logistic regression analysis confirmed that the two factors could not affect UMI. The specific reason for this difference from previous research is still unclear, which requires further multicenter clinical trials to verify in the future.
Our results suggest that there is no correlation between the tendon thickness at the tear site and the UMI. This may result from the tendon retraction after a rotator cuff tear and the tissue adhesion around the tear site, which result in uneven thickness. Since the tendon itself has a certain elasticity, the measurement value may be uncertain to some extent. Thus, the UMI on radiographs is a good indicator in the clinical diagnosis of supraspinatus/infraspinatus injury. According to the ROC curve, UMI < 1.38 implicated a normal tear, while a large tear was highly suspected when UMI < 1.3.
There are some limitations to this study. First, this study mainly focused on full-thickness tears, and the changes of partial tears were not included, which should be further studied in the future. Eventually, the conclusion in this study is still theoretical and needs further biomechanical experiments and clinical verification in the future.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Peking University People's Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors contributed to the study conception and design. Material preparation was performed by JC and YZ, data collection was performed by MM, and data analysis was performed by PZ. The first draft of the manuscript was written by BJ and YZ; all authors commented on previous versions of the manuscript. Data collection was performed by MM and JJ. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Key Laboratory of Trauma and Neural Regeneration (Peking University).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Akhtar A, Richards J, Monga P. The biomechanics of the rotator cuff in health and disease - a narrative review. J Clin Orthop Trauma. (2021) 18:150–6. doi: 10.1016/j.jcot.2021.04.019
2. Bezer M, Yildirim Y, Akgun U, Erol B, Guven O. Superior excursion of the humeral head: a diagnostic tool in rotator cuff tear surgery. J Shoulder Elbow Surg. (2005) 14:375–9. doi: 10.1016/j.jse.2004.12.001
3. Jeon YD, Yoon JY, Jeong HJ, Nam GW, Heo K, Kim JU, et al. Significance of the acromiohumeral distance on stress radiography for predicting healing and function after arthroscopic repair of massive rotator cuff tears. J Shoulder Elbow Surg. (2021) 30:e471–81. doi: 10.1016/j.jse.2020.10.029
4. Kaur R, Dahuja A, Garg S, Bansal K, Garg RS, Singh P. Correlation of acromial morphology in association with rotator cuff tear: a retrospective study. Pol J Radiol. (2019) 84:e459–63. doi: 10.5114/pjr.2019.90277
5. Norwood LA, Barrack R, Jacobson KE. Clinical presentation of complete tears of the rotator cuff. J Bone Joint Surg Am. (1989) 71:499–505. doi: 10.2106/00004623-198971040-00004
6. Bernhardt GA, Glehr M, Zacherl M, Wurnig C, Gruber G. Observer variability in the assessment of the acromiohumeral interval using anteroposterior shoulder radiographs. Eur J Orthop Surg Traumatol. (2013) 23:185–90. doi: 10.1007/s00590-012-0942-y
7. Hirooka A, Wakitani S, Yoneda M, Ochi T. Shoulder destruction in rheumatoid arthritis. Classification and prognostic signs in 83 patients followed 5–23 years. Acta Orthop Scand. (1996) 67:258–63. doi: 10.3109/17453679608994684
8. Lehtinen JT, Belt EA, Lyback CO, Kauppi MJ, Kaarela K, Kautiainen HJ, et al. Subacromial space in the rheumatoid shoulder: a radiographic 15-year follow-up study of 148 shoulders. J Shoulder Elbow Surg. (2000) 9:183–7. doi: 10.1067/mse.2000.105446
9. van de Sande MA, Rozing PM. Proximal migration can be measured accurately on standardized anteroposterior shoulder radiographs. Clin Orthop Relat Res. (2006) 443:260–5. doi: 10.1097/01.blo.0000196043.34789.73
10. Ishitani E, Harada N, Sonoda Y, Okada F, Yara T, Katsuki I. Tendon stump type on magnetic resonance imaging is a predictive factor for retear after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. (2019) 28:1647–53. doi: 10.1016/j.jse.2019.05.012
11. Jeong JY, Min SK, Park KM, Park YB, Han KJ, Yoo JC. Location of rotator cuff tear initiation: a magnetic resonance imaging study of 191 shoulders. Am J Sports Med. (2018) 46:649–55. doi: 10.1177/0363546517748925
12. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. (1994):78–83.
13. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. (1999) 8:599–605. doi: 10.1016/S1058-2746(99)90097-6
14. Cetinkaya M, Ataoglu MB, Ozer M, Ayanoglu T, Oner AY, Kanatli U. Do subscapularis tears really result in superior humeral migration? Acta Orthop Traumatol Turc. (2018) 52:109–14. doi: 10.1016/j.aott.2018.01.007
15. Mulla DM, Hodder JN, Maly MR, Lyons JL, Keir PJ. Glenohumeral stabilizing roles of the scapulohumeral muscles: implications of muscle geometry. J Biomech. (2020) 100:109589. doi: 10.1016/j.jbiomech.2019.109589
16. Cotty P, Proust F, Bertrand P, Fouquet B, Rosset P, Alison D, et al. [Rupture of the rotator cuff. Quantification of indirect signs in standard radiology and the Leclercq maneuver]. J Radiol. (1988) 69:633–8.
17. Walch G, Mar Chal E, Maupas J, Liotard JP. [Surgical treatment of rotator cuff rupture. Prognostic factors]. Rev Chir Orthop Reparatrice Appar Mot. (1992) 78:379–88.
18. Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. (2004) 86-a:708–16. doi: 10.2106/00004623-200404000-00007
19. Yamaguchi K, Sher JS, Andersen WK, Garretson R, Uribe JW, Hechtman K, et al. Glenohumeral motion in patients with rotator cuff tears: a comparison of asymptomatic and symptomatic shoulders. J Shoulder Elbow Surg. (2000) 9:6–11. doi: 10.1016/S1058-2746(00)90002-8
20. Keener JD, Wei AS, Kim HM, Steger-May K, Yamaguchi K. Proximal humeral migration in shoulders with symptomatic and asymptomatic rotator cuff tears. J Bone Joint Surg Am. (2009) 91:1405–13. doi: 10.2106/JBJS.H.00854
Keywords: rotator cuff tear, proximal humeral migration, upward migration index, predictor, acromion humeral distance
Citation: Zhang Y, Chen J, Ma M, Ju J, Jiang B and Zhang P (2022) Relevance between Proximal Humeral Migration and Rotator Cuff Tears. Front. Surg. 9:903538. doi: 10.3389/fsurg.2022.903538
Received: 24 March 2022; Accepted: 11 April 2022;
Published: 5 May 2022.
Edited by:
Yang Lv, Peking University Third Hospital, ChinaReviewed by:
Yu Mei, Peking University Third Hospital, ChinaJunlin Zhou, Beijing Chaoyang Hospital, Capital Medical University, China
Copyright © 2022 Zhang, Chen, Ma, Ju, Jiang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baoguo Jiang amlhbmdiYW9ndW9AdmlwLnNpbmEuY29t Peixun Zhang emhhbmdwZWl4dW5AMTI2LmNvbQ==
†These authors have contributed equally to this work and share first authorship
Speciality section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Yichong Zhang
Yichong Zhang Jianhai Chen†
Jianhai Chen†