
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 04 May 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.896536
This article is part of the Research Topic Co-use of medicines in surgery View all 114 articles
Objective: The present study is designed to study the analgesic and sedative effect of different doses of dexmedetomidine combined with butorphanol in continuous analgesia after a cesarean section.
Methods: A total of 60 puerperae undergoing a cesarean section recruited from a single center were divided into three groups according to the postoperative continuous analgesia protocol: control group (100 mL of normal saline containing 10 µg/kg fentanyl and 0.25 mg of palonosetron, 2 mL/h for continuous analgesia for 48 h), DB1 group (100 mL of normal saline containing 1.0 µg/kg dexmedetomidine, 4 mg of butorphanol, 10 µg/kg fentanyl, and 0.25 mg of palonosetron, 2 mL/h for continuous analgesia for 48 h), and DB2 group (100 mL normal saline containing 2.0 µg/kg dexmedetomidine, 4 mg of butorphanol, 10 µg/kg fentanyl, and 0.25 mg of palonosetron, 2 mL/h for continuous analgesia for 48 h). We compared the blood pressure, heart rate, oxygen saturation, VAS score, Ramsay score, and adverse reactions of puerperae among the three groups after surgery.
Results: The baseline data all have no significant difference in the three groups (p > 0.05). Compared with those in the control group, the systolic blood pressure, diastolic blood pressure, heart rate, and VAS score of the puerperae in the DB1 group and DB2 group were significantly decreased at 6, 24, and 48 h (P < 0.05), while the Ramsay scores of the puerperae in DB1 group and DB2 group were significantly increased at 6, 24, and 48 h (p < 0.05). At the same time, the systolic blood pressure, diastolic blood pressure, heart rate, and VAS score of the puerperae in the DB2 group were significantly lower than those in the DB1 group (P < 0.05), while the Ramsay scores of the puerperae in DB2 group were significantly higher than those in the DB1 group (P < 0.05). Also, there is no significant difference in oxygen saturation and adverse reactions of puerperae among the three groups after surgery (p > 0.05).
Conclusion: Dexmedetomidine combined with butorphanol can improve the analgesic and sedative effects in continuous analgesia after a cesarean section, and the analgesic and sedative effects of dexmedetomidine in the high-dose group are better than those in the low-dose group.
Postoperative pain-induced stress can lead to a series of changes in physiology, psychology, and behavior and adversely affect the normal endocrine and immune functions of humans (1, 2). Previous studies have shown that postoperative pain is closely related to the occurrence of postoperative complications, delays postoperative recovery, and affects patient prognosis (3, 4). In addition, severe postoperative pain is considered to be a high-risk factor for long-term chronic pain after surgery (5, 6). After a cesarean section, pain seriously affects the daily activities of the puerperium, and it is not conducive to early postpartum lactation and lactation and hinders the communication between the mother and the baby (7, 8). Therefore, it is of great significance to provide good, safe, and reliable analgesia to puerperae. Adequate postoperative analgesia can not only relieve postoperative fatigue and improve the comfort and satisfaction of puerperae but also help to improve the quality of postoperative recovery of puerperae (7, 8). However, there is currently no standard protocol for postcesarean section analgesia.
Dexmedetomidine is an α2 adrenergic receptor agonist with high selectivity and has sedative, analgesic, antisympathetic, anxiolytic, and stress-reducing effects, while it rarely causes respiratory depression (9–11). Butorphanol, an analgesic, exerts its analgesic effect mainly by agonizing κ receptors and partially antagonizing μ receptors (12). In addition, butorphanol is widely used in postoperative patient-controlled intravenous analgesia (PCIA), but it can cause many side effects when used alone (13). However, clinical studies suggest that dexmedetomidine can enhance the analgesic effect of butorphanol, and its combination can reduce its adverse effects (14, 15). In the present study, we designed to study the analgesic and sedative effect of different doses of dexmedetomidine combined with butorphanol in continuous analgesia after a cesarean section.
This study complied with the principles of the Declaration of Helsinki and was reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Northern College in Hebei Province. In addition, all volunteers who participated in this study were informed about the content of this study and signed an informed consent form.
From January 2019 to December 2019, 60 puerperae undergoing a cesarean section were recruited in the present study. These puerperae must meet the following standards. Inclusion criteria are as follows: (1) undergoing a cesarean section under combined spinal–epidural anesthesia; (2) The American Society of Anesthesiologists (ASA) grades of grades I to II; (3) first birth, between 20 and 35 years old, with a height of 1.5–1.75 m; and (4) informed and agreed to participsate in this research. Exclusion criteria are as follows: (1) long-term use of nonsteroidal anti-inflammatory drugs, opioids, tranquilizers, and sedatives; (2) mental illness, intellectual disability, or other reasons for the maternal inability to complete the pain and sedation score; (3) preoperative heart rate below 50 bpm with abnormal cardiac conduction and rhythm; (4) neuromuscular endocrine diseases and allergic reactions to α2 adrenergic receptor agonists; (5) having a history of abdominal surgery in the past; and (6) anesthesia fails, the operation time is more than 2 h, the intraoperative blood loss is more than 500 mL, or a second operation is required to treat postpartum hemorrhage.
All participants received combined spinal–epidural anesthesia, with open venous access to infuse ringer sodium lactate (state approval no. H20044239; Shandong Weigao Pharmaceutical Co., Ltd., Shandong, China) and choosing the lumbar 3–4 space as the puncture point. Ephedrine hydrochloride injection (state approval no. H22020730; Tonghua Baishan Pharmaceutical Co., Ltd., Jilin, China) or phenylephrine (state approval no. H31021175; Shanghai Hefeng Pharmaceutical Co., Ltd., Shanhai, China) is given to maintain circulatory stability according to changes in the blood pressure and heart rate.
Sixty patients were divided into three groups according to the postoperative continuous analgesia protocol: control group, DB1 group, and DB2 group. The control group received 100 mL of normal saline containing 10 µg/kg fentanyl and 0.25 mg palonosetron, 2 mL/h for continuous analgesia for 48 h. The DB1 group received 100 mL of normal saline containing 1.0 µg/kg dexmedetomidine, 4 mg butorphanol, 10 µg/kg fentanyl, and 0.25 mg palonosetron, 2 mL/h for continuous analgesia for 48 h. The DB2 group received 100 mL of normal saline containing 2.0 µg/kg dexmedetomidine, 4 mg butorphanol, 10 µg/kg fentanyl, and 0.25 mg palonosetron, 2 mL/h for continuous analgesia for 48 h.
Herein, we used a visual analogue scale (VAS) score to assess pain at 6, 24, and 48 h after the cesarean section. Additionally, VAS scores range from 0 to 10, with higher scores indicating more severe pain. We used the Ramsay score to assess the level of sedation at 6, 24, and 48 h after the cesarean section, and the Ramsay scores range from 1 to 6, with higher scores indicating higher levels of sedation. We collected the clinical data of participants of age, height, weight, gestational week, onset time of operation, fetal delivery time, duration of surgery, and duration of anesthesia. At the same time, the blood pressure, heart rate, oxygen saturation, VAS score, and Ramsay score were also being determined at 1, 6, 24, and 48 h after the cesarean section. In addition, the adverse reactions including malignant vomiting, dizziness, itchy shin, bradycardia, and low blood pressure were also recorded immediately after surgery to 1 week after surgery.
Data in the present study were analyzed by SPSS 19.0 software (SPSS Inc., Chicago, USA). Qualitative data are presented as counts (%), and p-values are calculated using chi-square or Fisher’s exact test as appropriate. The Kolmogorov–Smirnov test was used to check whether quantitative data conformed to a normal distribution; data that conformed to a normal distribution were presented as mean ± standard deviation, and an unpaired Student’s t-test was used to compare differences and calculate p-values. Quantitative data that did not conform to a normal distribution were presented as the median (interquartile range), and the Mann–Whitney U-test was used to compare differences and calculate p-values. p < 0.05 were considered statistically significant.
The baseline data including characteristics including age, height, weight, and gestational week and surgical indicators including the onset time of operation, fetal delivery time, duration of surgery, and duration of anesthesia all have no significant difference in the three groups (p > 0.05) (Table 1).
At 1, 6, 24, and 48 h after the cesarean section, the systolic blood pressure (Table 2), diastolic blood pressure (Table 3), and heart rate (Table 4) of puerperae in the DB1 group and DB2 group are all significantly lower than those in the control group (p < 0.05), and the systolic blood pressure, diastolic blood pressure, and heart rate of pirpera in the DB2 group are all significantly lower than those in the DB1 group (p < 0.05). However, there is no significant difference among these three groups in oxygen saturation of puerpera (p > 0.05) (Table 5).
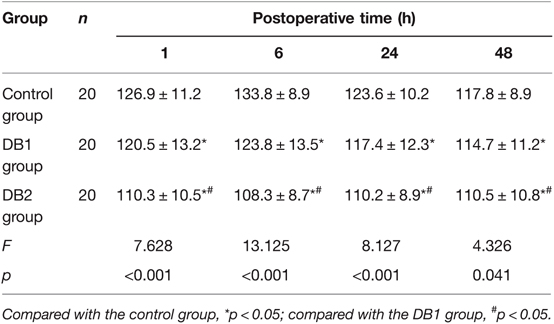
Table 2. Comparison of systolic blood pressure of puerperae at different times after surgery among three groups (mean ± SD, mmHg).
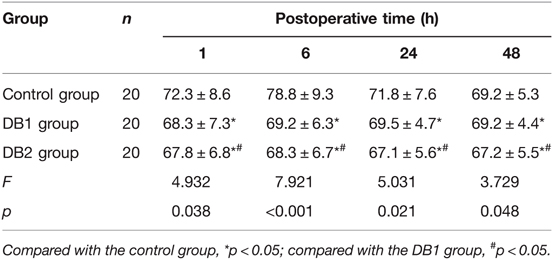
Table 3. Comparison of diastolic blood pressure of puerperae at different times after surgery among three groups (mean ± SD, mmHg).
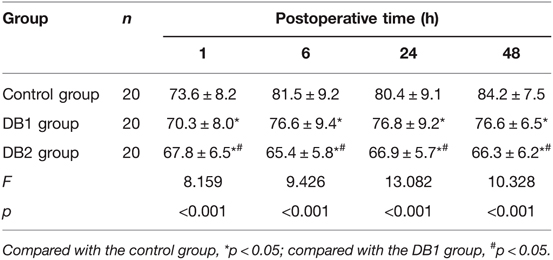
Table 4. Comparison of the heart rate of puerperae at different times after surgery among three groups (mean ± SD, n/min).
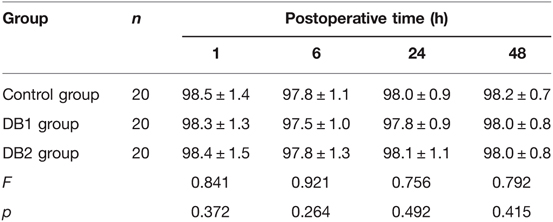
Table 5. Comparison of oxygen saturation of puerperae at different times after surgery among three groups (mean ± SD, %).
The VAS scores of puerperae at 6, 24, and 48 h after the cesarean section in the DB1 group and DB2 group are all significantly lower than those in the control group (P < 0.05), and the VAS scores of puerperae at 6, 24, and 48 h after the cesarean section in the DB2 group are significantly lower than those in the DB1 group (P < 0.05) (Table 6).
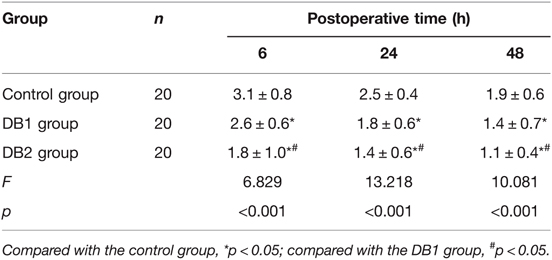
Table 6. Comparison of VAS scores of puerperae at different times after surgery among three groups (mean ± SD, score).
The Ramsay scores of puerperae at 6, 24, and 48 h after the cesarean section in the DB1 group and DB2 group are all significantly higher than those in the control group (p < 0.05), and the Ramsay scores of puerperae at 6, 24, and 48 h after the cesarean section in the DB2 group are significantly higher than those in the DB1 group (p < 0.05) (Table 7).
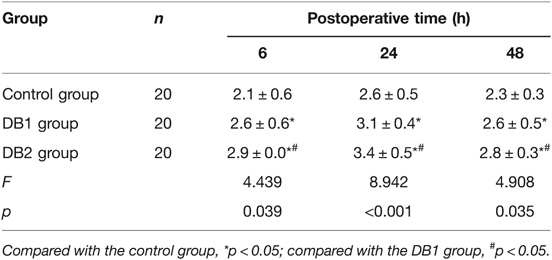
Table 7. Comparison of Ramsay scores of puerperae at different times after surgery among three groups (mean ± SD, score).
There is no significant difference among the control group, DB1 group, and DB2 group in the adverse reactions at 48 h after surgery (p > 0.05) (Table 8).
In this study, we found that continuous intravenous infusion of dexmedetomidine along with butorphanol in PCIA after a cesarean section could lead not only to pain reduction and enhanced analgesic effect (according to VAS) but also improved sedative effects, while it did not affect the adverse reaction. At the same time, we also found that high-dose dexmedetomidine was more effective for analgesia and sedation than low-dose dexmedetomidine.
The use of opioids alone for sedation after a cesarean section has many disadvantages. On the one hand, the analgesic effect is insufficient (16). On the other hand, the application of high-dose opioid analgesics significantly increased the incidence of postoperative nausea, vomiting, and respiratory depression (17). In addition, the safety of many analgesics excreted in breast milk in newborns is uncertain (16, 17). Dexmedetomidine is a nonopioid drug with both peripheral and central analgesic effects, and it is a selective α2 adrenoceptor agonist, which can reduce sympathetic nerve activity, the release of catecholamines, and the harmful stimulation caused by surgery and has a certain protective effect on important organs. Results from a randomized and placebo-controlled study have shown that the combination of sufentanil and dexmedetomidine for PCA after a cesarean section can reduce sufentanil consumption and improve parturients’ satisfaction compared with sufentanil PCA alone (18). In addition, a recent study indicated that adding dexmedetomidine to the postoperative analgesia regimen for a cesarean section could enhance postoperative analgesia and improve satisfaction (19). In previous studies (20–22), the doses of dexmedetomidine for sustained analgesia after a cesarean section included 0.08, 0.5, and 3 µg/kg/h, so we administered 1.0 and 2.0 µg/kg/h dexmedetomidine to determine the dose-dependent effect and optimal dose of analgesic management with PCIA in the present study.
Furthermore, cesarean section-induced pain is not only from incision but also from uterine contraction during uterine involution, and there is no evidence suggesting that opioids are effective for uterine contraction pain (16). Butorphanol exerts an analgesic effect through the dual action of opioid receptor agonism-antagonism, and its single application has a definite effect on the treatment of severe and moderate pain (12, 13). More importantly, butorphanol can also relieve visceral pain, which can make up for the lack of opioid analgesics in postoperative analgesia for mothers (23, 24). In this study, we found that maternal addition of butorphanol for analgesia was effective in reducing uterine cramping pain, suggesting that butorphanol can relieve visceral pain in postcesarean section analgesia. Postoperative pain is the main factor leading to postoperative sleep deprivation, and patients with severe sleep deprivation are prone to postoperative hyperalgesia (25, 26). In addition, butorphanol has many advantages for PCIA after a cesarean section because of its unique pharmacological properties. First, the analgesic mechanism of butorphanol is mainly achieved by activating κ receptors, and the activation of κ receptors enables it to exert a more potent analgesic effect in the treatment of visceral pain (23, 24). Second, the milk secretion rate of butorphanol is low, and the drug concentration in maternal milk at therapeutic doses is extremely low, so there is almost no obvious adverse effect on the newborn (27).
Dexmedetomidine acts on the α2 adrenoceptor agonist in the nucleus locus coeruleus, reduces the release of norepinephrine, simulates natural sleep, and produces sedative, hypnotic, and anxiolytic effects (28, 29). In the present study, we found that dexmedetomidine combined with butorphanol can improve the sedative effects (according to the Ramsay score) in continuous analgesia after a cesarean section, and the analgesic and sedative effects of dexmedetomidine in the high-dose group are better than those in the low-dose group, which is consistent with the findings of Zhang et al. (30). Zhang et al. found that dexmedetomidine was more effective than sufentanil for maternal labor sedation, and the analgesic and sedative effects of dexmedetomidine in the high-dose group were better than those in the low-dose group (30).
Postoperative pain can induce adverse events, such as cardiovascular disease, respiratory depression, digestive and urinary system dysfunction, and neuroendocrine disorders, which bring great discomfort to patients and seriously affect the postoperative recovery of patients (31, 32). At the same time, although the use of unreasonable postoperative analgesics can effectively control pain, it can also cause adverse reactions, such as malignant vomiting, dizziness, itchy skin, bradycardia, and low blood pressure (33, 34). Therefore, to date, there is still no accepted and optimal analgesic regimen for postoperative pain. In our study, we found that the addition of dexmedetomidine combined with butorphanol to the basic postoperative analgesia regimen enhanced the analgesic effect without increasing the adverse reactions in patients, which suggested that dexmedetomidine combined with butorphanol is not only effective in postoperative analgesia and sedation but also safe in puerperae after a cesarean section.
There were several limitations to our study. First, we only studied the effect of dexmedetomidine combined with butorphanol on mothers and did not study the content of dexmedetomidine and butorphanol in maternal milk and whether they affected neonates. Second, the sample size included in this study is small, so the results may be biased to a certain extent. The results of this study need to be further verified by a systematic study with large sample size. At last, we only analyzed two doses of dexmedetomidine, and more doses of dexmedetomidine need to be studied to further explore the optimal dose for clinical application.
Dexmedetomidine combined with butorphanol can improve the analgesic and sedative effects in continuous analgesia after a cesarean section, and the analgesic and sedative effects of dexmedetomidine in the high-dose group are better than those in the low-dose group.
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding author/s..
The studies involving human participants were reviewed and approved by the ethics committee of our hospital. The patients/participants provided their written informed consent to participate in this study.
HL and YW are mainly responsible for the writing of the article. FL is mainly responsible for research design. YW is mainly responsible for data analysis. WR and LY are responsible for the guidance of the entire research. The corresponding author is Hui Liu, and she is responsible for ensuring that the descriptions are accurate and agreed upon by all authors. All authors contributed to the article and approved the submitted version.
This study was supported by the Zhangjiakou Key Research and Development Projects (1921060D).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Gelman D, Gelmanas A, Urbanaitė D, Tamošiunas R, Sadauskas S, Bilskiene D, et al. Role of multimodal analgesia in the evolving enhanced recovery after surgery pathways. Medicina. (2018) 54(2):20. doi: 10.3390/medicina54020020
2. Wang J, Yin Y, Zhu Y, Xu P, Sun Z, Miao C, et al. Thoracic epidural anaesthesia and analgesia ameliorates surgery-induced stress response and postoperative pain in patients undergoing radical oesophagectomy. J Int Med Res. (2019) 47(12):6160–70. doi: 10.1177/0300060519866943
3. Kehlet H. Postoperative pain, analgesia, and recovery-bedfellows that cannot be ignored. Pain. (2018) 159(Suppl 1):S11–6. doi: 10.1097/j.pain.0000000000001243
4. Zieliński J, Morawska-Kochman M, Zatoński T. Pain assessment and management in children in the postoperative period: a review of the most commonly used postoperative pain assessment tools, new diagnostic methods and the latest guidelines for postoperative pain therapy in children. Adv Clin Exp Med. (2020) 29(3):365–74. doi: 10.17219/acem/112600
5. Chapman CR, Vierck CJ. The transition of acute postoperative pain to chronic pain: an integrative overview of research on mechanisms. J Pain. (2017) 18(4):359.e1–9.e38. doi: 10.1016/j.jpain.2016.11.004
6. Glare P, Aubrey KR, Myles PS. Transition from acute to chronic pain after surgery. Lancet. (2019) 393(10180):1537–46. doi: 10.1016/S0140-6736(19)30352-6
7. Roofthooft E, Joshi GP, Rawal N, Van de Velde M. PROSPECT working group of the European Society of Regional Anaesthesia and Pain Therapy and supported by the Obstetric Anaesthetists’ Association. PROSPECT guideline for elective caesarean section: updated systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. (2021) 76(5):665–80. doi: 10.1111/anae.15339
8. Kintu A, Abdulla S, Lubikire A, Nabukenya MT, Igaga E, Bulamba F, et al. Postoperative pain after cesarean section: assessment and management in a tertiary hospital in a low-income country. BMC Health Serv Res. (2019) 19(1):68. doi: 10.1186/s12913-019-3911-x
9. Carr ZJ, Cios TJ, Potter KF, Swick JT. Does dexmedetomidine ameliorate postoperative cognitive dysfunction? A brief review of the recent literature. Curr Neurol Neurosci Rep. (2018) 18(10):64. doi: 10.1007/s11910-018-0873-z
10. Keating GM. Dexmedetomidine: a review of its use for sedation in the intensive care setting. Drugs. (2015) 75(10):1119–30. doi: 10.1007/s40265-015-0419-5
11. Tasbihgou SR, Barends CRM, Absalom AR. The role of dexmedetomidine in neurosurgery. Best Pract Res Clin Anaesthesiol. (2021) 35(2):221–9. doi: 10.1016/j.bpa.2020.10.002
12. Ji J, Lin W, Vrudhula A, Xi J, Yeliseev A, Grothusen JR, et al. Molecular interaction between butorphanol andκ-opioid receptor. Anesth Analg. (2020) 131(3):935–42. doi: 10.1213/ANE.0000000000005017
13. Zhu Z, Zhang W. Efficacy and safety of butorphanol use in patient-controlled analgesia: a meta-analysis. Evid Based Complement Alternat Med. (2021) 2021:5530441.
14. Ding X, Luo Y, Shi L, Liu C, Yan Z. Butorphanol in combination with dexmedetomidine provides efficient pain management in adult burn patients. Burns. (2021) 47(7):1594–601. doi: 10.1016/j.burns.2020.12.025
15. Ahsan MZ, Khan FU, Zhao MJ, Wang YX. Synergistic interaction between butorphanol and dexmedetomidine in antinociception. Eur J Pharm Sci. (2020) 149:105322. doi: 10.1016/j.ejps.2020.105322
16. Beardsley PM, Zhang Y. Synthetic opioids. Handb Exp Pharmacol. (2018) 252:353–81. doi: 10.1007/164_2018_149
17. Nedeljkovic SS, Kett A, Vallejo MC, Horn JL, Carvalho B, Bao X, et al. Transversus abdominis plane block with liposomal bupivacaine for pain after cesarean delivery in a multicenter, randomized, double-blind, controlled trial. Anesth Analg. (2020) 131(6):1830–39. doi: 10.1213/ANE.0000000000005075
18. Nie Y, Liu Y, Luo Q, Huang S. Effect of dexmedetomidine combined with sufentanil for post-caesarean section intravenous analgesia: a randomised, placebo-controlled study. Eur J Anaesthesiol. (2014) 31(4):197–203. doi: 10.1097/EJA.0000000000000011
19. Imani F, Rahimzadeh P, Faiz HR, Nowruzina S, Shakeri A, Ghahremani M. Comparison of the post-caesarean analgesic effect of adding dexmedetomidine to paracetamol and ketorolac: a randomized clinical trial. Anesth Pain Med. (2018) 8(5):e85311.
20. Liu S, Peng P, Hu Y, Liu C, Cao X, Yang C, et al. The effectiveness and safety of intravenous dexmedetomidine of different concentrations combined with butorphanol for post-caesarean section analgesia: a randomized controlled trial. Drug Des Devel Ther. (2021) 15:689–98. doi: 10.2147/DDDT.S287512
21. Jiang W, Wang Q, Xu M, Li Y, Yang R, Song X, et al. Assessment of different loading doses of dexmedetomidine hydrochloride in preventing adverse reaction after combined spinal–epidural anaesthesia. Exp Ther Med. (2017) 13(6):2946–50. doi: 10.3892/etm.2017.4335
22. Chen Z, Tang R, Zhang R, Jiang Y, Liu Y. Effects of dexmedetomidine administered for postoperative analgesia on sleep quality in patients undergoing abdominal hysterectomy. J Clin Anesth. (2017) 36:118–22. doi: 10.1016/j.jclinane.2016.10.022
23. Ide S, Minami M, Ishihara K, Uhl GR, Satoh M, Sora I, et al. Abolished thermal and mechanical antinociception but retained visceral chemical antinociception induced by butorphanol in mu-opioid receptor knockout mice. Neuropharmacology. (2008) 54(8):1182–8. doi: 10.1016/j.neuropharm.2008.03.008
24. Sanchez LC, Elfenbein JR, Robertson SA. Effect of acepromazine, butorphanol, or N-butylscopolammonium bromide on visceral and somatic nociception and duodenal motility in conscious horses. Am J Vet Res. (2008) 69(5):579–85. doi: 10.2460/ajvr.69.5.579
25. Waxman JA, Shenouda KG, Lin HS. Assessment and management of postoperative pain associated with sleep apnea surgery. Otolaryngol Clin North Am. (2020) 53(5):765–77. doi: 10.1016/j.otc.2020.05.006
26. Su X, Wang DX. Improve postoperative sleep: what can we do? Curr Opin Anaesthesiol. (2018) 31(1):83–8. doi: 10.1097/ACO.0000000000000538
27. Maduska AL, Hajghassemali M. A double-blind comparison of butorphanol and meperidie in labour: maternal pain relief and effect on the newborn. Can Anaesth Soc J. (1978) 25(5):398–404. doi: 10.1007/BF03006569
28. Fontaine GV, Der Nigoghossian C, Hamilton LA. Melatonin, ramelteon, suvorexant, and dexmedetomidine to promote sleep and prevent delirium in critically ill patients: a narrative review with practical applications. Crit Care Nurs Q. (2020) 43(2):232–50. doi: 10.1097/CNQ.0000000000000304
29. Huang X, Lin D, Sun Y, Wu A, Wei C. Effect of dexmedetomidine on postoperative sleep quality: a systematic review. Drug Des Devel Ther. (2021) 15:2161–70. doi: 10.2147/DDDT.S304162
30. Zhang T, Yu Y, Zhang W, Zhu J. Comparison of dexmedetomidine and sufentanil as adjuvants to local anesthetic for epidural labor analgesia: a randomized controlled trial. Drug Des Devel Ther. (2019) 13:1171–5. doi: 10.2147/DDDT.S197431
31. Hernández-Avalos I, Valverde A, Ibancovichi-Camarillo JA, Sánchez-Aparicio P, Recillas-Morales S, Osorio-Avalos J, et al. Clinical evaluation of postoperative analgesia, cardiorespiratory parameters and changes in liver and renal function tests of paracetamol compared to meloxicam and carprofen in dogs undergoing ovariohysterectomy. PLoS One. (2020) 15(2):e0223697. doi: 10.1371/journal.pone.0223697
32. Lopes A, Seligman Menezes M, Antonio Moreira de Barros G. Chronic postoperative pain: ubiquitous and scarcely appraised: narrative review. Braz J Anesthesiol. (2021) 71(6):649–55.
33. Barnett T, Denke L. Managing postoperative pain with opioid-sparing therapies. Nursing. (2020) 50(12):60–3. doi: 10.1097/01.NURSE.0000694772.54730.b8
Keywords: dexmedetomidine, butorphanol, sedative, analgesic, cesarean section
Citation: Liu H, Wang Y, Li F, Ren W and Yuan L (2022) Analgesic and Sedative Effects of Different Doses of Dexmedetomidine Combined with Butorphanol in Continuous Analgesia after a Cesarean Section. Front. Surg. 9:896536. doi: 10.3389/fsurg.2022.896536
Received: 15 March 2022; Accepted: 7 April 2022;
Published: 4 May 2022.
Edited by:
Songwen Tan, Central South University, ChinaReviewed by:
Li Genlin, The First Affiliated Hospital, University of South China, ChinaCopyright © 2022 Liu, Wang, Li, Ren and Yuan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Liu TGl1MjI2NDA4NkAxNjMuY29t
Speciality section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.