
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 27 April 2022
Sec. Thoracic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.889753
This article is part of the Research Topic Case Reports in Thoracic Surgery: 2021 View all 11 articles
Background: Crigler-Najjar syndrome type 2 (CNS-II) is a rare genetic disease that is associated with a lack of uridine diphosphate-glucuronosyltransferase. Esophageal carcinoma is the sixth most common cause of cancer-related death worldwide, for which surgery is the most effective treatment. Reports on patients with both conditions requiring surgery are limited and The impact of hyperbilirubinemia caused by CNS-II on the perioperative period is unknown. Previous studies have found that patients with Crigler-Najjar syndrome have an increased risk of gallstones and related complications, which also poses corresponding challenges to the treatment. Herein, we present a patient with CNS-II who underwent successful thoracoscopic surgery for esophageal carcinoma.
Case summary: A 65-year-old male presented to our hospital with a choking sensation after eating. A physical examination showed yellowing of the sclera and skin. The patient manifested persistent jaundice since birth and had visited many hospitals, but the cause remained undiagnosed. We performed genetic testing, which confirmed CNS-II. Gastroscopy indicated esophageal carcinoma. A multidisciplinary team discussion was carried out to determine the appropriate treatment and perioperative management for this patient. The results show that surgical resection was the most appropriate approach. Finally, the patient underwent thoracoscopic surgery for esophageal carcinoma without complications.
Conclusion: Esophageal carcinoma in patients with Crigler-Najjar syndrome is a rare case, and perioperative management is key in the treatment process. It is necessary to pay close attention to the changes of the disease to prevent complications.
Crigler-Najjar syndrome type 2 (CNS-II), also called Arias syndrome, is caused by mutations in UGT1A1 and is associated with a deficiency in uridine diphosphate-glucoronosyltransferase (UDP-GT) (1, 2). The disorder is transmitted by autosomal recessive inheritance and is characterized by hyperbilirubinemia (3). Existing studies have shown that patients with Crigler-Najjar syndrome (CN) are at increased risk for gallstones and related complications (4–8), and the early diagnosis of gallstones and cholangitis is challenged due to permanent jaundice. Esophageal carcinoma is an aggressive disease for which surgery is the most effective treatment. However, esophageal carcinoma with simultaneous CNS-II is exceedingly rare, with only a few cases reported thus far. The impact of hyperbilirubinemia on surgical treatment of esophageal cancer is unclear, and its associated complications are unknown. In this paper, we report a patient with CNS-II who underwent successful thoracoscopic surgery for esophageal carcinoma.
A 65-year-old male patient experienced a choking sensation during eating for 2 months.
A 65-year-old male patient was admitted to our hospital because of a choking sensation during eating for 2 months, which was accompanied by retrosternal pain and had no obvious cause.
The patient had a 3-year history of hypertension and took telmisartan for blood pressure control. The patient had manifested yellow discoloration of the skin and sclera since childhood, for which he had visited many hospitals, but his condition did not improve with medication.
The patient’s parents were of a consanguineous marriage and had raised three sons and three daughters. Two sons and one daughter also had yellow discoloration while the others showed no relevant symptoms. The patient’s daughter and grandson have no relevant symptoms. Its pedigree is shown in Figure 1.
The patient was generally in a good condition with no supraclavicular lymph node enlargement. The breath sounds of the lungs were rough without rales or Rhonchi. Heart rate was 102 beats/min, and heart rhythm was regular, showing no pathologic murmur. The abdomen was flat and soft, without tenderness or rebound tenderness. Yellow discoloration of the skin and sclera was observed.
White blood cell count was 7.0 × 109/L, neutrophil percentage was 63.1%, hemoglobin concentration was 125 g/L, alanine transaminase was 9 IU/L, aspartate aminotransferase was 18 IU/L, total bilirubin was 187 µmol/L, direct bilirubin was 19.9 µmol/L, and indirect bilirubin was 167.8 µmol/L. Electrocardiography revealed sinus rhythm. we also take a DNA analysis,Genetic testing showed (Figure 2):
(1) UGT1A8_ex5 c.1447T > G(p.Tyr483Asp)
(2) UGT1A1_ex1 c.211G > A(p.Gly71Arg)
(3) UGT1A4_ex1 c.395T > C(p.Leu132Pro)
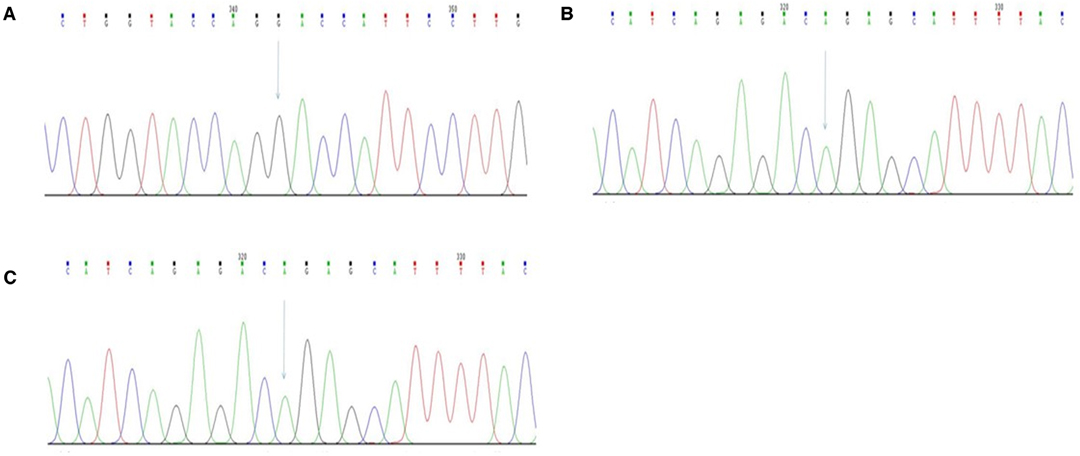
Figure 2. (A) UGT1A8_ex5c.1447T > G(p.Tyr483Asp)NCBI reference sequence: CTGGTACCAG TACCATTCCTTG; (B) UGT1A1_ex1c.211G > A(p.Gly71Arg) NCBI reference sequence: CATCAGAGAC GGAGCATTTTAC; (C) UGT1A4_ex1c.395T > C(p.Leu132Pro) NCBI reference sequence: GTGGAGCTAC TGCATAATGAGG.
It was suggested that the patient has CNS-II. Other laboratory indicators were all within normal limits.
Esophagography showed mucosal damage in the mid-to-lower segment of the esophagus, with a filling defect shadow and irregular small niche with a lesion measuring approximately 8.1 cm in length. Gastric endoscopy showed a cauliflower-like ulcero-proliferative growth in the lower part of the esophagus, which was considered to be esophageal squamous cell carcinoma according to the symptoms of the ulcerating surface covered with white moss, and the depressed central part (Figure 3).
The final diagnosis was esophageal carcinoma and Crigler-Najjar syndrome type 2.
The patient underwent thoracoscopic surgery. Tissue was obtained and sent for pathological examination. The postoperative pathological diagnosis was esophageal squamous cell carcinoma (tumor volume, 7.4 × 5.1 × 1.6 cm). Moderate differentiation was observed with infiltration to the adventitia, and there was no lymph node metastasis (Figure 4).
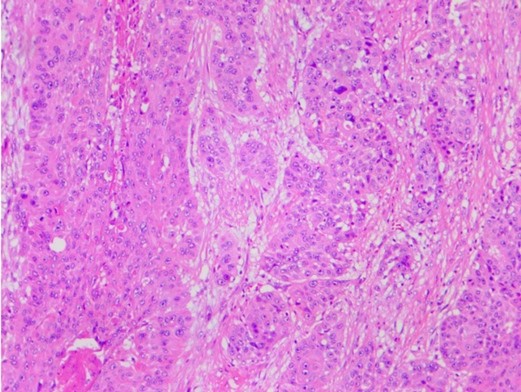
Figure 4. Microscopic findings show squamous carcinoma, (hematoxylin and eosin staining, magnification × 100).
Three months after surgery, the patient revisited our hospital for review. He had recovered well with no related complications, suggesting that the efficacy of surgical treatment was satisfied for this patient with esophageal cancer and CNS-II.
Crigler-Najjar syndrome (CN), which was first described in 1952, is caused by lack of UDP-GT. It can be divided into two categories: type 1 and type 2. Patients with severe jaundice and no response to phenobarbital are classified as Crigler-Najjar syndrome type 1 which type 2 (9).
Crigler-Najjar syndrome type 2 is the less severe form of the disease, with the deficiency in UDP-GT being <30%. UDP-GT is a membrane protein binding on the endoplasmic reticulum, which catalyzes the transfer of the D-Glucuronic acid of UDP – D-Glucuronic acid to other molecules. So it plays play a key part in the Metabolism of bilirubin and promotes the water solubility of acceptors, which promotes the bilirubin excreted from the body by the bile and urine. CNS-II is mostly observed in infants or later in childhood, with bilirubin levels in the region of 102.6–342 mmol/L (10). These patients seldom develop central nervous system involvement complicated by kernicterus. Generally, there are no other notable biochemical parameters, except serum bilirubin. These patients usually survive into adulthood. If the condition becomes serious, it can be treated with phenobarbital to control bilirubin at an appropriate level (11).
Through genetic testing, the patient found three mutated genes, namely UGT1A8, UGT1A1 and UGT1A4. UGT1A8 is a homozygous missense mutation, which has been reported to be detected in Gilbert syndrome and hyperbilirubinemia (12, 13). In vitro functional experiments showed that the mutant protein produced by the mutation had very low scavenging activity against total bilirubin glucuronic acid (13). ClinVar database recorded the mutation as a pathogenic or suspected pathogenic mutation (14). The genetic testing company used SIFT and Polyphen-2 to predict the function of the protein, and the results were both harmful, so the mutation was considered as pathogenic. UGT1A1 is a common variant in Gilbert syndrome and Crigler-Najjar syndrome in the East Asian population (15). In vitro studies have shown that the mutation leads to decreased enzyme activity and is associated with elevated serum bilirubin levels in infants (16). UGT1A1 gene related to CNS-II, Gilbert syndrome (GS), Crigler-Najjar syndrome type 1 (CNS-1) were inherited by autosomal recessive inheritance. As for UGT1A4, ClinVar database has not included this locus, and it is an unknown mutation of clinical significance according to software analysis.
The incidence of CN is approximately at 0.6 patients per million. It is extremely rare for patients with esophageal carcinoma and CNS-II. To the best of our knowledge, this is the first case ever reported. the influence of CN on the occurrence of esophageal cancer is not very well understood, the association CN and early esophageal cancer seen in this case may be incidental. So, there is no experience in this case.
Pre-operative multidisciplinary discussion was held. We all agree that it is important for patients not to suffer starvation for a long period time, which may increase the level of bilirubin. Postoperative vomiting should be avoided by maintaining basal glucose infusion. Ondansetron appears to be efficacious in preventing severe vomiting, but furosemide, salicylates, ampicillin, sulfonamide, and ceftriaxone should be avoided (17). The efficacy of jaundice drugs in the patient was poor, but the jaundice could be reduced. Hepatic encephalopathy may also occur as a postsurgical complication. If necessary, plasma exchange should be performed. Should considerable pruritus occur, phenobarbitals can be used. postoperative parenteral nutrition was administered cautiously to avoid exacerbating jaundice. Should jaundice worsen, bilirubin adsorption is recommended. chemotherapy had a great impact on this patient’s liver function, and radiotherapy alone was not adequately effective in treating esophageal cancer, so surgery was the best choice. In terms of surgical options, we chose minimally invasive surgery, which has a similar overall survival rate, lower complications and better tolerance compared with open surgery (18).
Surgery went smoothly, and due to concern for the potential impact on liver function, enteral nutrition rather than parenteral nutrition was adopted. During postoperative hospitalization, certain indicators, including liver function, total bilirubin, direct bilirubin, and indirect bilirubin, were similar to those before surgery (Figure 5). The patient was able to drink and eat one week after surgery, and he reported no obvious discomfort. He was discharged two weeks after surgery, without much change in various indicators compared with before surgery. Three months later, the patient revisited our hospital for review and had recovered well, with no related complications. This suggests that the efficacy of surgery was satisfied in this patient with esophageal carcinoma and CNS-II.
CNS-II is a relatively benign disease. The management of the disease involves a variety of methods, including lifelong diet adjustment counseling, ensuring adequate hydration, avoiding triggers such as stress, and lifelong phenobarbital treatment. Genetic counseling, especially about blood relationship, is an important part of management and regular follow-up. For the part of esophageal cancer, the patient has successfully received surgical treatment, and according to the postoperative pathological results, the operation has reached R0 resection, and no lymph node metastasis has been found. It is pT1BN0M0 stage IB, does not need postoperative radiotherapy and chemotherapy, and needs regular follow-up and nutritional support treatment.
Patients with Crigler-Najjar syndrome are at increased risk of various complications due to the presence of persistent hyperbilirubinemia, and the risk of surgical resection may be high, but for diseases that require surgical treatment, surgical treatment can still be performed under close perioperative monitoring and appropriate management.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
DM, FC, XC wrote the original manuscript and and contributed to literature review; YC contributed to editing the report. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Liaqat A, Shahid A, Attiq H, Ameer A, Imran M. Crigler-Najjar syndrome Type II diagnosed in a patient with jaundice since birth. J Coll Physicians Surg Pak. (2018) 28:806–8.
2. Radlović N. Hereditary hyperbilirubinemias. Srp Arh Celok Lek. (2014) 142:257–60. doi: 10.2298/SARH1404257R
3. Strassburg CP. Hyperbilirubinemia syndromes (Gilbert-Meulengracht, Crigler-Najjar, Dubin-Johnson, and Rotor syndrome). Best Pract Res Clin Gastroenterol. (2010) 24:555–71. doi: 10.1016/j.bpg.2010.07.007
4. Powell LW, Hemingway E, Billing BH, Sherlock S. Idiopathic unconjugated hyperbilirubinemia (Gilbert’s syndrome). A study of 42 families. N Engl J Med. (1967) 277:1108–12. doi: 10.1056/NEJM196711232772102
5. Foulk WT, Butt HR, Owen CA, Whitcomb FF, Mason HL. Constitutional hepatic dysfunction (Gilbert’s disease): its natural history and related syndromes. Medicine (Baltimore). (1959) 38:25–46. doi: 10.1097/00005792-195902000-00002
6. Kagita A, Adachi Y, Kambe A, Kamisako T, Yamamoto T. Type II crigler-Najjar syndrome with intrahepatic cholestasis. J Gastroenterol. (1994) 29:214–7. doi: 10.1007/BF02358686
7. Strauss KA, Robinson DL, Vreman HJ, Puffenberger EG, Hart G, Morton DH. Management of hyperbilirubinemia and prevention of kernicterus in 20 patients with Crigler-Najjar disease. Eur J Pediatr. (2006) 165:306–19. doi: 10.1007/s00431-005-0055-2
8. Fernandes SR, Moura CM, Rodrigues B, Correia LA, Cortez-Pinto H, Velosa J. Acute cholangitis in an old patient with Crigler-Najjar syndrome type II - a case report. BMC Gastroenterol. (2016) 16:33. doi: 10.1186/s12876-016-0449-9
9. Rodrigues C, Vieira E, Santos R, de Carvalho J, Santos-Silva A, Costa E, et al. Impact of UGT1A1 gene variants on total bilirubin levels in Gilbert syndrome patients and in healthy subjects. Blood Cells Mol Dis. (2012) 48:166–72. doi: 10.1016/j.bcmd.2012.01.004
10. Canu G, Minucci A, Zuppi C, Capoluongo E. Gilbert and Crigler Najjar syndromes: an update of the UDP-glucuronosyltransferase 1A1 (UGT1A1) gene mutation database. Blood Cells Mol Dis. (2013) 50:273–80. doi: 10.1016/j.bcmd.2013.01.003
11. Gailite L, Rots D, Pukite I, Cernevska G, Kreile M. Case report: multiple UGT1A1 gene variants in a patient with Crigler-Najjar syndrome. BMC Pediatr. (2018) 18:317. doi: 10.1186/s12887-018-1285-6
12. Maruo Y, Nishizawa K, Sato H, Sawa H, Shimada M. Prolonged unconjugated hyperbilirubinemia associated with breast milk and mutations of the bilirubin uridine diphosphate- glucuronosyltransferase gene. Pediatrics. (2000) 106(5):E59. doi: 10.1542/peds.106.5.e59
13. Udomuksorn W, Elliot DJ, Lewis BC, Mackenzie PI, Yoovathaworn K, Miners JO. Influence of mutations associated with Gilbert and Crigler-Najjar type II syndromes on the glucuronidation kinetics of bilirubin and other UDP-glucuronosyltransferase 1A substrates. Pharmacogenet Genomics. (2007) 17(12):1017–29. doi: 10.1097/FPC.0b013e328256b1b6
14. Lin R, Wang X, Wang Y, Zhang F, Wang Y, Fu W, et al. Association of polymorphisms in four bilirubin metabolism genes with serum bilirubin in three Asian populations. Hum Mutat. (2009) 30(4):609–15. doi: 10.1002/humu.20895
15. Teng HC, Huang MJ, Tang KS, Yang SS, Tseng CS, Huang CS. Combined UGT1A1 and UGT1A7 variant alleles are associated with increased risk of Gilbert’s syndrome in Taiwanese adults. Clin Genet. (2007) 72(4):321–8. doi: 10.1111/j.1399-0004.2007.00873.x
16. Yamamoto A, Nishio H, Waku S, Yokoyama N, Yonetani M, Uetani Y, et al. Gly71Arg mutation of the bilirubin UDP-glucuronosyltransferase 1A1 gene is associated with neonatal hyperbilirubinemia in the Japanese population. Kobe J Med Sci. (2002) 48(3-4):73–7.
17. Bicak M, Akelma H, Salik F, Kaya S. Combined spinal and TAP blocks for laparoscopic cholecystectomy for a patient with Crigler-Najjar Type 2: a case report. Niger J Clin Pract. (2020) 23:1772–5. doi: 10.4103/njcp.njcp_19_20
Keywords: Esophageal carcinoma, Crigler-Najjar syndrome type 2, case report, esophageal squamous cell carcinoma, surgery, perioperative management
Citation: Ma D, Chen F, Chen X and Chen Y (2022) Perioperative Management of Patient with Esophageal Carcinoma and Crigler-Najjar Syndrome Type 2: A Case Report. Front. Surg. 9:889753. doi: 10.3389/fsurg.2022.889753
Received: 4 March 2022; Accepted: 8 April 2022;
Published: 27 April 2022.
Edited by:
Nuria Maria Novoa, University of Salamanca Health Care Complex, Salamanca, SpainReviewed by:
Madara Kreile, Riga Stradin¸š University, LatviaCopyright © 2022 Ma, Chen, chen and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Chen chenyu5835@126.com
†These authors have contributed equally to this work
Speciality section: This article was submitted to Thoracic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.