- 1Department of Orthopedics, Orthopedic Research Institute, West China Hospital, Sichuan University, Chengdu, China
- 2Department of Respiratory and Critical Care Medicine, West China Hospital, Sichuan University, Chengdu, China
Purpose: To compare the clinical outcomes of arthroscopic anterior cruciate ligament (ACL) repair and autograft ACL reconstruction for ACL ruptures.
Methods: PubMed, EMBASE, Scopus, Web of Science and The Cochrane Library were searched for relevant studies from 1 January 1990 to 21 March 2022. Two evaluators independently screened the literature, extracted data and assessed the methodological quality of the enrolled studies. Meta-analysis was conducted using RevMan 5.4 software.
Results: Ten studies with mean follow-up periods from 12 to 36 months were included. For 638 patients with ACL ruptures, arthroscopic ACL repair showed statistically comparable outcomes of failure (p = 0.18), complications (p = 0.29), reoperation other than revision (p = 0.78), Lysholm score (p = 0.78), Tegner score (p = 0.70), and satisfaction (p = 0.45) when compared with autograft ACL reconstruction. A significantly higher rate of hardware removal (p = 0.0008) but greater International Knee Documentation Committee (IKDC) score (p = 0.009) were found in the ACL repair group. The heterogeneity of the side-to-side difference of anterior tibial translation (ΔATT) was high (I2 = 80%). After the sensitivity analysis, the I2 decreased dramatically (I2 = 32%), and the knees with ACL repair showed significantly greater ΔATT (P = 0.04).
Conclusion: For proximal ACL ruptures, arthroscopic ACL repair showed similar clinical outcomes, and even better functional performance when compared to autograft ACL reconstruction. ACL repair has a higher rate of hardware removal, and might be related to greater asymptomatic knee laxity. More high-quality prospective trials are needed to confirm our findings.
Introduction
Primary open repair of the anterior cruciate ligament (ACL) was the standard surgical technique for ACL ruptures until the 1980s, when poor results at longer follow-up were reported (1–4). Thereafter, open ACL repair was gradually replaced by arthroscopic autograft ACL reconstruction for ACL ruptures.
However, autograft ACL reconstruction has several problems, such as anterior knee pain, thigh muscle weakness following harvesting, and an extensive rehabilitation period (5). In the past decade, renewed and increasing interest in ACL repair has arisen and various arthroscopic ACL repair techniques have been introduced, especially for proximal ACL ruptures (6, 7). Among these newly developed surgeries, four ACL repair techniques have been in the spotlight (5): suture anchor repair (SAR) of the ACL, repair with dynamic intraligamentary stabilization (DIS), internal brace ligament augmentation (IBLA) and bridge-enhanced ACL repair (BEAR). Moreover, previous published systematic reviews showed promising results following ACL repair. In 2017, Ahmad et al. (7) analyzed 23 articles related to DIS and concluded that ACL repair might be an effective modality for the treatment of acute proximal ACL tears. In another systematic review, van der List et al. (8) found that different techniques of primary ACL repair were safe with failure rates between 7 and 11%, and good functional outcome scores in 1,101 patients. However, subsequent two systematic reviews (9, 10) reported inconsistent results following ACL repair compared with ACL reconstruction.
On further review of the above literatures (7–10), we found most included studies in these systematic reviews were case series with relatively small sample sizes, and the number of high-quality trials comparing arthroscopic ACL repair with reconstruction was scarce, making it difficult to conduct a meta-analysis comparing arthroscopic ACL repair with autograft ACL reconstruction. Importantly, there are several high-quality comparative clinical trials (11–14) published in recent years reporting that arthroscopic ACL repair yields ideal results comparable to those of ACL reconstruction. Therefore, the purpose of this meta-analysis was to quantitatively compare the clinical outcomes of arthroscopic ACL repair and autograft ACL reconstruction for ACL ruptures. The study is to explore that whether arthroscopic ACL repair can be a viable alternative to ACL reconstruction for patients with ACL ruptures, providing an optional surgery for treating ACL tears in clinical practice.
Methods
Literature Search
This study was conducted in strict accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (15). We searched PubMed, Embase, Scopus, Web of Science, and the Cochrane Library, using the combination of “anterior cruciate ligament”, “ACL”, “repair”, “suture”, “dynamic intraligamentary stabilization”, “internal brace”, “bridge-enhanced”, “autograft” and “reconstruction”. The search was performed by two independent researchers. All possible studies from 1 January 1990 to 21 March 2022, were manually retrieved. In addition, the reference lists of all retrieved articles were reviewed for potentially eligible studies. Any disagreement was debated and resolved with a third researcher.
Inclusion and Exclusion Criteria
Inclusion criteria: (1) the enrolled patients had a confirmed diagnosis of ACL rupture; (2) clinical studies comparing primary arthroscopic ACL repair to autograft ACL reconstruction; (3) a minimum of 12-month follow-up; (4) written in English.
Exclusion criteria: (1) presence of multiligamentous injuries or knee dislocations; (2) presence of concomitant lesions that would alter the rehabilitation; (3) presence of previous knee injuries on either the injured or contralateral knee; (4) long-term follow-up of historical studies; (5) focused on skeletally immature patients; (6) study with smallest cohort or shortest follow-up (different studies that report on the same group of patients); (7) data inadequate or unavailable.
Data Extraction
Two researchers independently extracted data from the included studies. Characteristics of the enrolled studies (authors, year, country, study design, level of evidence, sample size), and patients’ baseline information (age, sex, time from injury to surgery, follow-up period, rupture location, autograft). The following clinical outcomes were extracted and pooled: (1) failure, complications, reoperation other than revision, hardware removal rates; (2) anteroposterior (AP) knee laxity assessed by the mean difference in anterior tibial translation (ΔATT) between the injured and contralateral knees; and (3) patient-reported outcomes including the International Knee Documentation Committee (IKDC) score (16), the Lysholm score (17), the Tegner score (18), and satisfaction.
Quality Assessment
Two authors made their own assessment of the risk of bias of enrolled randomized controlled trials (RCTs) according to the Risk of Bias Tool conferred by the Cochrane Handbook (19), and those of cohort and case–control studies by the Methodological Index for Non-Randomized Studies (MINORS) criteria (20). A third evaluator made the final decision when any disagreements appeared.
Statistical Analysis
Statistical analyses were performed with Manager V.5.4 (The Cochrane Collaboration, Software Update, Oxford, UK). We analyzed the outcomes by calculating the weighted mean difference (WMD) and pooled odds ratio (OR) with corresponding 95% confidence intervals (CIs). A P value <0.05 was considered to be statistically significant. We evaluated and characterized the heterogeneity of each eligible study with Cochrane’s Q statistic and I2 statistics. Statistical heterogeneity between studies was assessed using the I2 value, where less than 50% was considered to be within the acceptable range of heterogeneity and the fixed effect model was applied. Otherwise, the random effect model was adopted. In case of any heterogeneity, the following methods were applied to explain: (1) sensitivity analysis; (2) subgroup analysis. Sensitivity analyses were conducted to confirm the robustness of pooled outcomes by sequentially removing the included studies one-by-one. Subgroup analyses according to RCT design or non-RCT design were conducted for all outcomes. For the primary outcome failure rates, subgroup analyses according to the rupture location and ACL repair technique were performed. Publication bias was not assessed because the number of studies included in each study area was less than 10; therefore, the statistical power was low.
Results
Literature Search
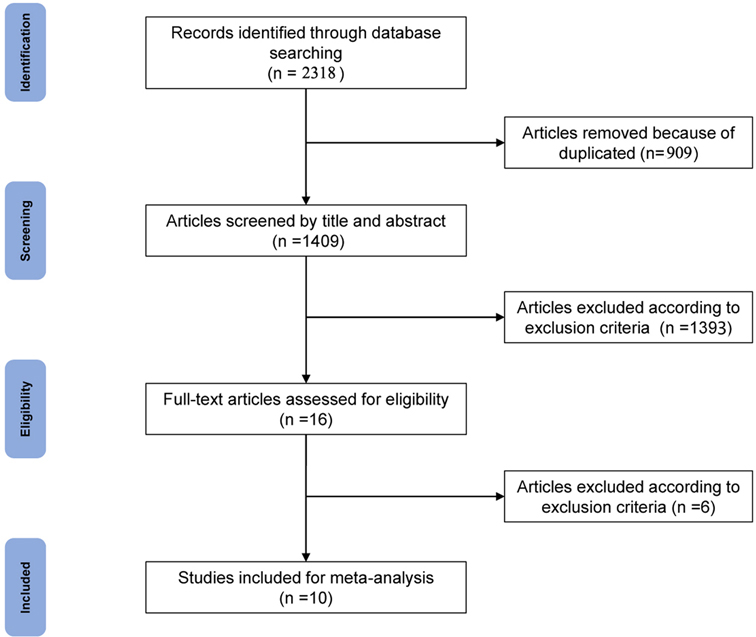
Two independent researchers searched PubMed, Embase, Scopus, Web of Science and the Cochrane Library according to the identified keywords, and a total of 2,318 articles were retrieved. After 909 duplicates were removed, the titles and abstracts of 1,409 remaining articles were screened, and 1,393 articles were removed according to the inclusion and exclusion criteria. The remaining full texts of 16 articles were screened independently by two researchers. The study by Gagliardi et al. (21) was excluded because this cohort enrolled skeletally immature patients (7–18 years old). The study by Jonkergouw et al. (22) was excluded because it compared outcomes following ACL repair with or without additional internal bracing. The study by Sporsheim et al. (23) was excluded because it was a 30-year follow-up of a history study, in which the contemporary arthroscopic ACL repair technique was not performed. The study by van der List et al. (24) was excluded because the follow-up period was less than 12 months. The study by Connolly et al. (25) excluded only reported postoperative pain and narcotic prescriptions at the first visit. Two studies (26, 27) by Murray et al. focused on the same group of patients, and the study with shorter follow-up (27) was excluded. Finally, 10 articles (11–14, 26, 28–32) were included in the meta-analysis, including 4 RCTs (11–14), 1 prospective cohort study (26), 3 retrospective cohort studies (28, 29, 31), and 2 case–control studies (30, 32) (Figure 1).
Quality Assessment
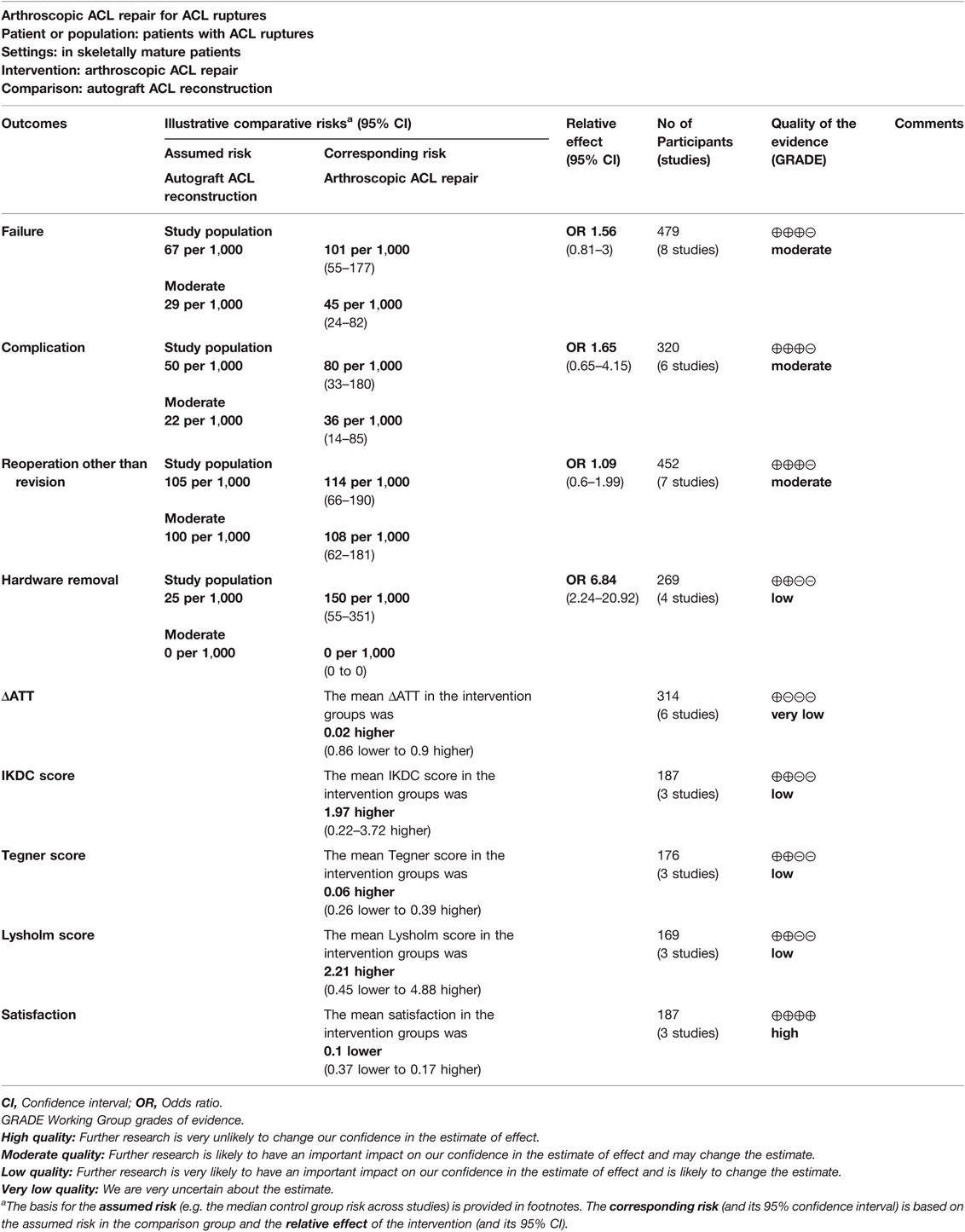
The quality of the included RCTs was assessed using Review Manager software, and they are summarized and visualized in Figure 2. The quality of the included cohort and case–control studies was evaluated by MINORS criteria, which are shown in Table 1.
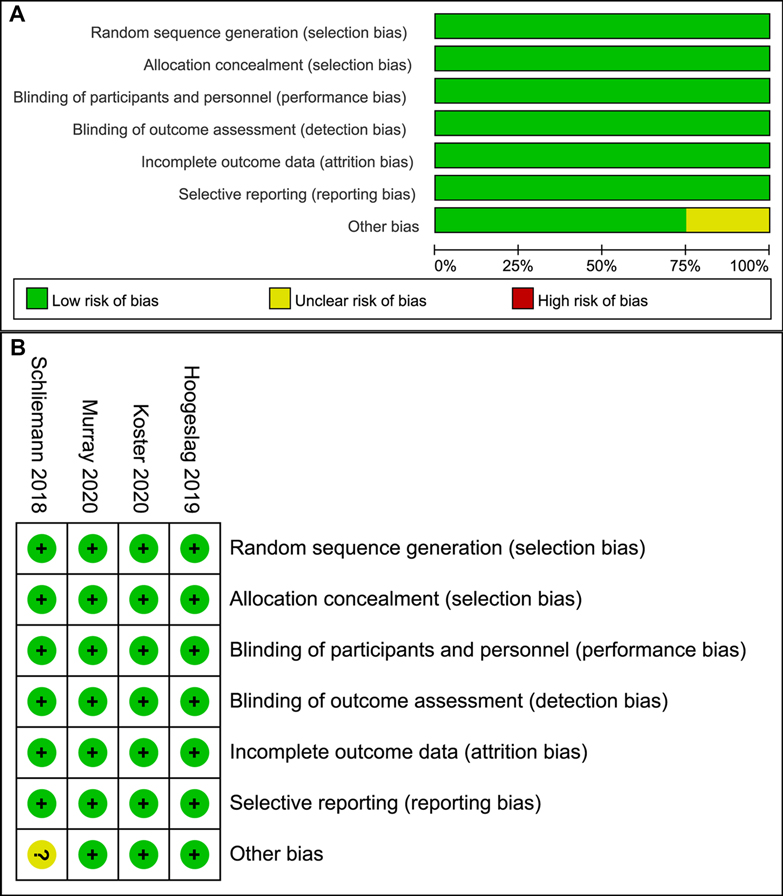
Figure 2. Risk of bias graph (A) Graph of the risk of bias for the included RCTs; (B) graph of the risk of bias summary for the included RCTs.
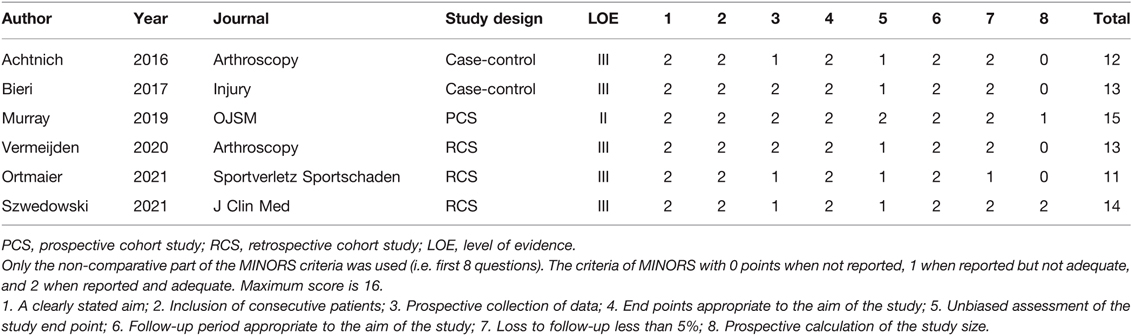
Table 1. Quality assessment of the non-RCT studies using the Methodological Index for Non-Randomized Studies (MINORS) criteria.
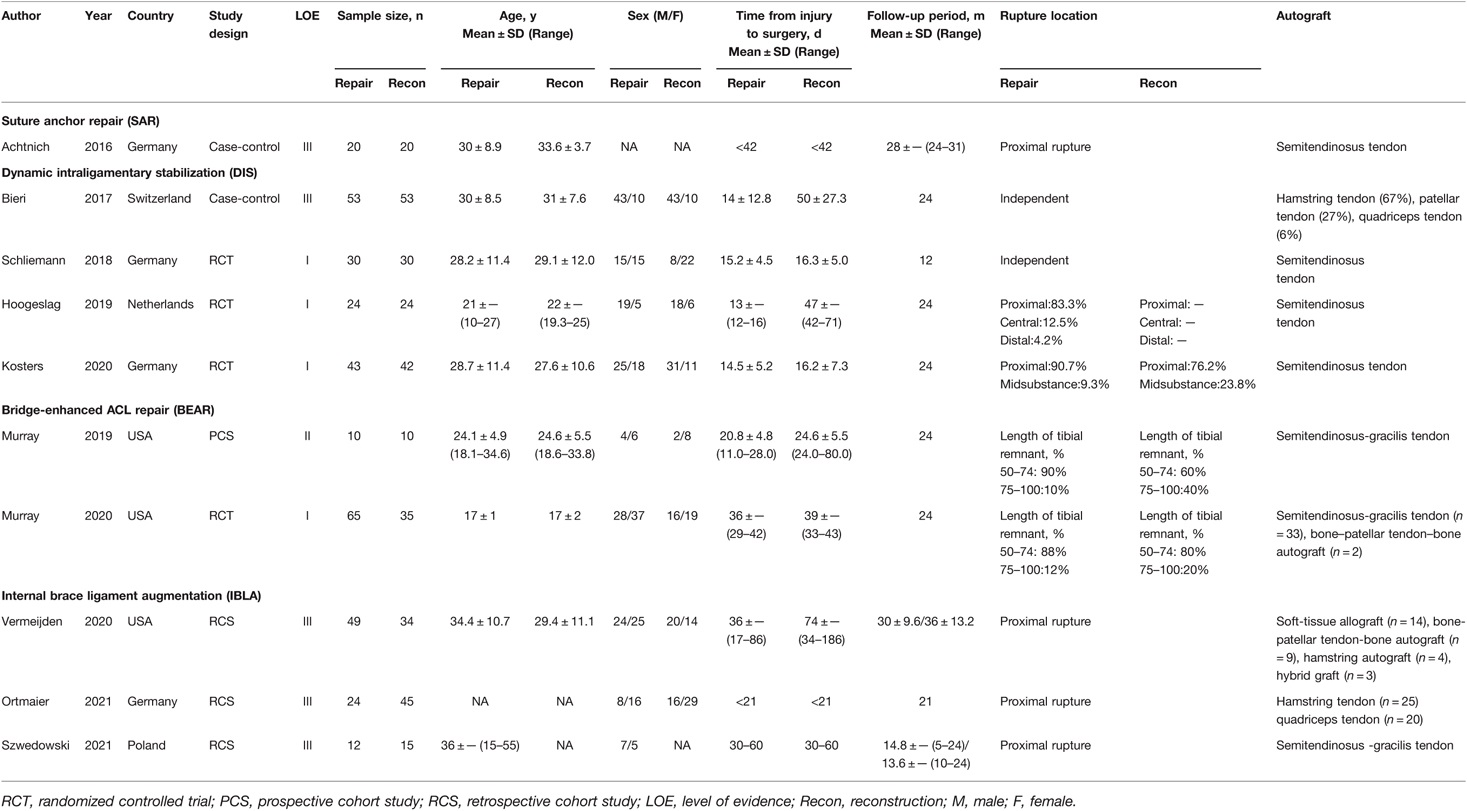
Baseline Data
Detailed baseline information for all included articles is summarized in Table 2, with a total of 638 patients assigned to the two groups (ACL repair/ACL reconstruction = 330/308). The mean age of patients ranged from 17 to 36 years old, and the percentage of male patients was from 30 to 81%. The mean time from injury to surgery ranged from 13 to 74 days, and the follow period ranged from 12 to 36 months. Two studies (14, 30) enrolled patients independent of the ACL rupture location, while other studies (11–13, 26, 28, 29, 31, 32) mainly included patients with ACL proximal rupture. As for the selection of autograft for ACL reconstruction, most studies (11–14, 26, 28, 32) used semitendinosus tendon, while the other studies (29–31) used hamstring tendon, patellar tendon, or quadriceps tendon. For the ACL repair techniques, primary SAR of the ACL was performed in 1 study (32), using one suture anchor to reattach the ACL remnant back to the femoral footprint. A total of 4 studies (11, 12, 14, 30) reported outcomes following primary ACL suture repair with DIS. After the remaining threads in the ACL stump were tensioned and the tibial stump was repositioned to the femoral footprint, an intraligamentary braid with cortical button fixation on the femoral side and an additional elastic link (a spring-in-screw mechanism) on the tibial side was introduced. A total of 2 studies (13, 26) by Murray et al. focused on patients treated with BEAR, involving suture repair of the ligament combined with a BEAR scaffold saturated with 5–10 ml autologous blood to bridge the gap between the ends of the torn ligament. In the other 3 studies (28, 29, 31), after completion of ACL suture repair, IBLA was achieved by adding FiberTape to the ACL substance, and fixed with a suture anchor perpendicular to the tibial cortex.
Failure, Complications, Reoperation Other than Revision, and Hardware Removal Rates
Failures were defined as postoperative recurrent instability of the ipsilateral knee joint regardless of the need for revision surgery. A total of 9 studies (11–14, 26, 28, 30, 32) reported failures after surgery, the result of which was 27/255 in the ACL repair group and 15/224 in the ACL reconstruction group (OR, 1.56; 95% CI, 0.81–3.00; I2 = 0%; P = 0.18) (Figure 3A).
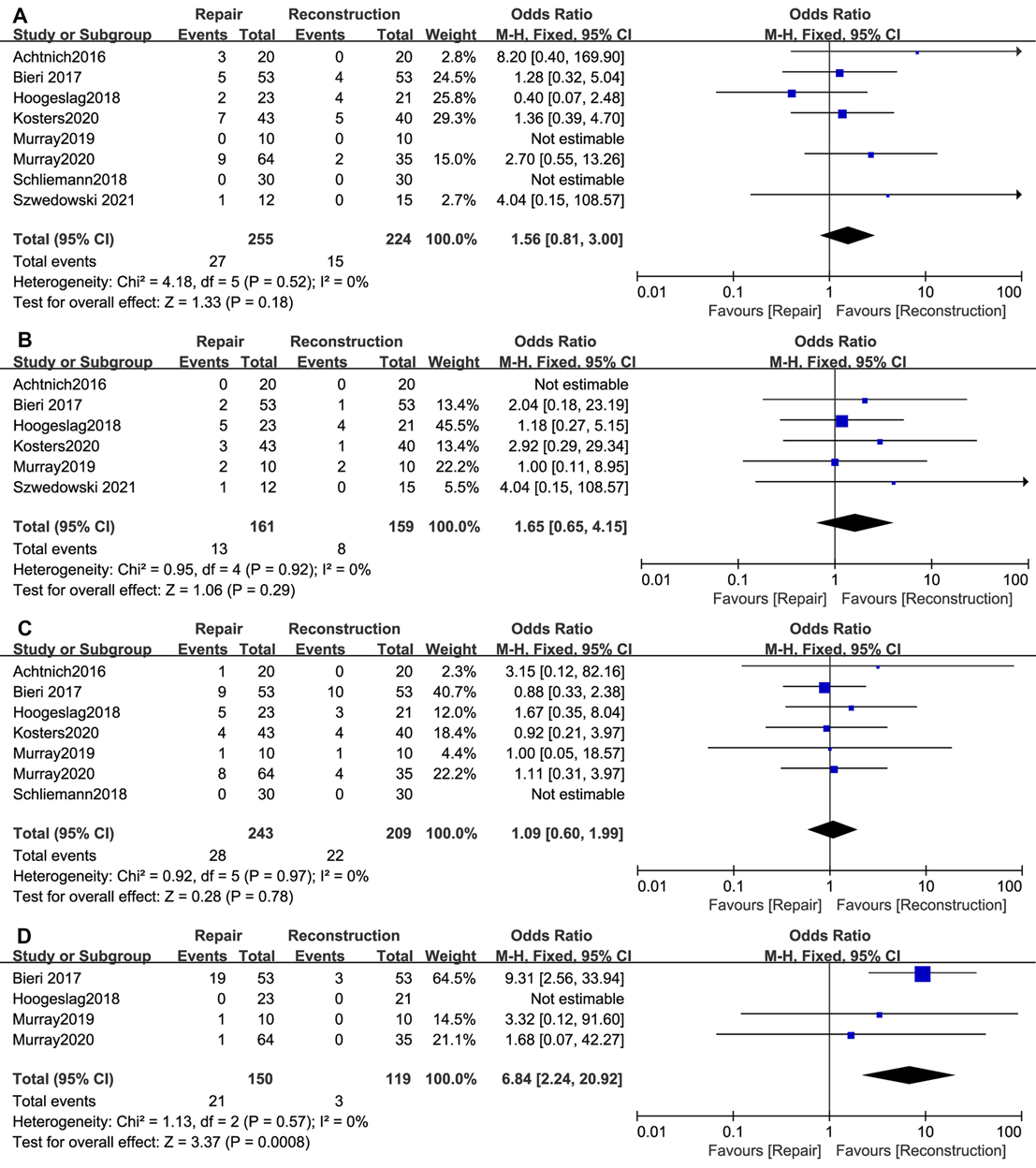
Figure 3. Meta-analysis of the rates of (A) Failure; (B) Complications; (C) Reoperation rather than revision; (D) Hardware removal.
A total of 6 studies (11, 12, 26, 28, 30, 32) reported postoperative complications, including superficial or deep infection, deep venous thrombosis (DVT), and pain at the tibial screw without the need for removal. There were 13/161 patients in the ACL repair group and 8/159 in the ACL reconstruction group (OR, 1.65; 95% CI, 0.65–4.15; I2 = 0%; P = 0.29) (Figure 3B).
Reoperations other than revision were defined as additional surgical interventions for ipsilateral knee disorders other than ACL retears, such as menisci lesions, synovitis, and arthrofibrosis. Reoperations were reported in 7 studies (11, 13, 14, 26, 30–32), and the result was 28/243 in the ACL repair group and 22/209 in the ACL reconstruction group (OR, 1.09; 95% CI, 0.60–1.99; I2 = 0%; P = 0.78) (Figure 3C).
Hardware removal rates were reported in 4 studies (11, 13, 26, 30), the result of which was 21/150 (19 in the DIS group, 2 in the BEAR group) in the ACL repair group and 3/119 (3 in the DIS group) in the ACL reconstruction group (OR, 6.84; 95% CI, 2.24–20.92; I2 = 0%; P = 0.0008) (Figure 3D).
AP Knee Laxity
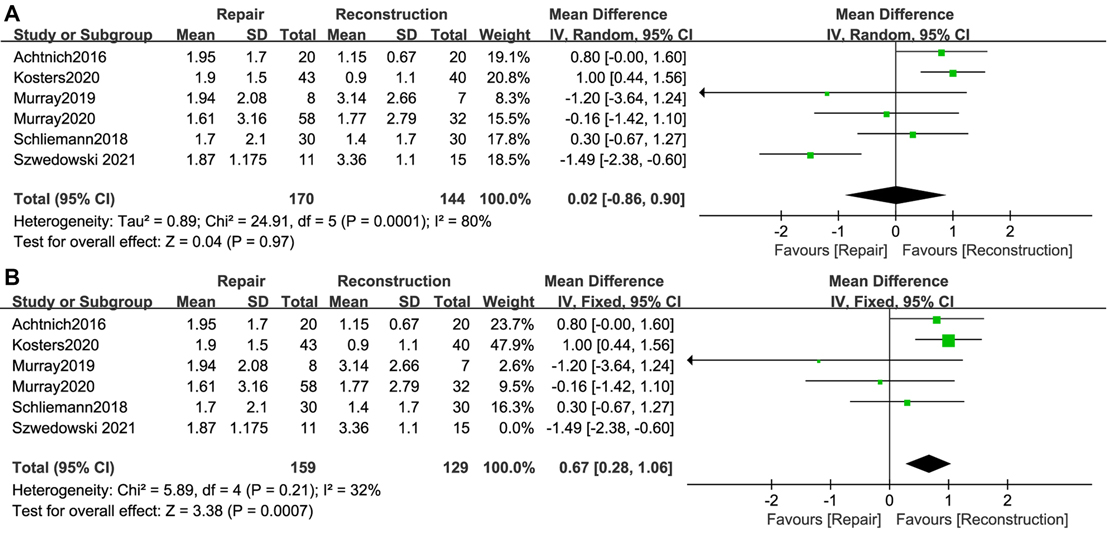
A total of 6 studies (12–14, 26, 28, 32) reported ΔATT when stress was exerted on the knees, with a total of 170 cases in the ACL repair group and 144 cases in the ACL reconstruction group. The difference in postoperative ΔATT between the two groups was not statistically significant (WMD, 0.02; 95% CI, −0.86–0.90; I2 = 80%; P = 0.97) (Figure 4A). Because the I2 was relatively high, sensitivity analyses were performed by sequentially removing the included studies. After removing the study (28) by Szwedowski et al., the I2 decreased dramatically, and knees with ACL repair showed significantly greater ΔATT (WMD, 0.56; 95% CI, 0.04–1.08; I2 = 32%; P = 0.04) (Figure 4B).
Patient-Reported Outcomes
The IKDC score was mentioned in 5 studies (11–14, 26), with 167 cases in the ACL repair group and 132 cases in the ACL reconstruction group. ACL repair showed an advantage in terms of the postoperative IKDC score over ACL reconstruction (WMD, 2.23; 95% CI, 0.57–3.89; I2 = 0%; P = 0.009) (Figure 5A).
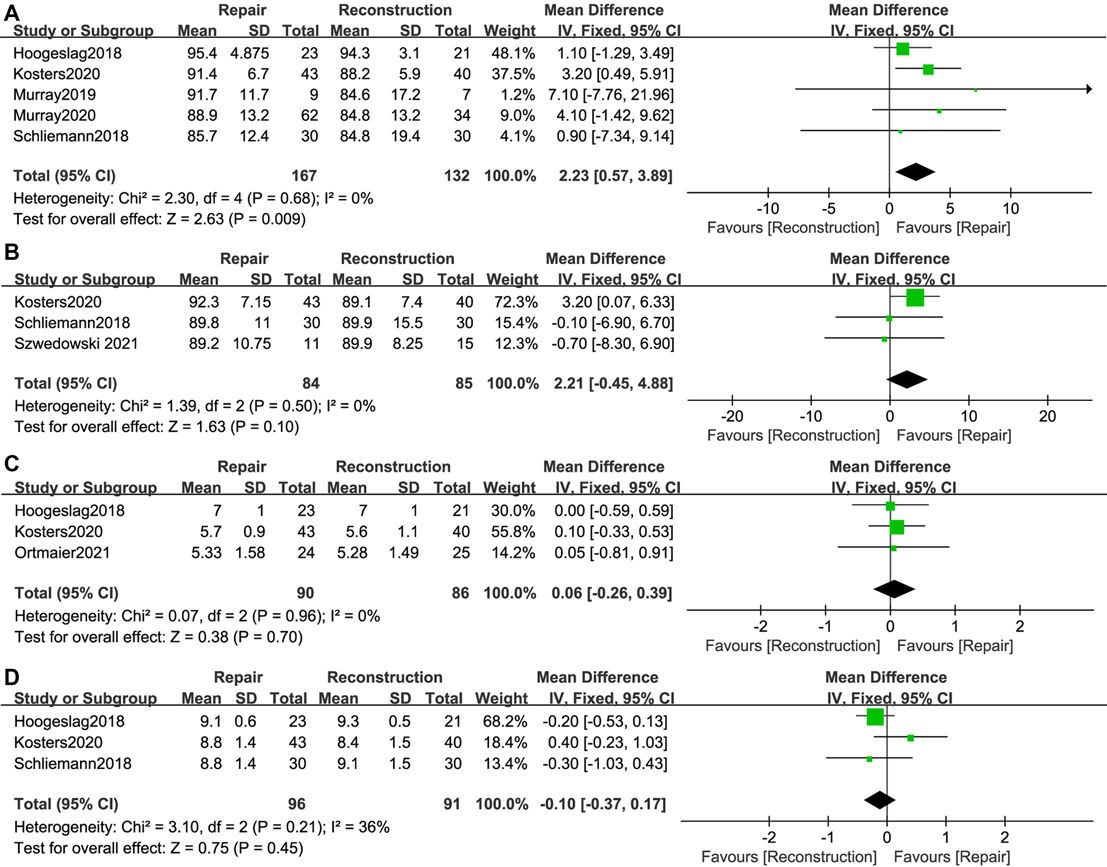
Figure 5. Meta-analysis of patient-reported outcomes (A) IKDC score; (B) Lysholm score; (C) Tegner score; (D) Satisfaction.
The Lysholm score was reported in 3 studies (12, 14, 28), involving 84 patients in the ACL repair group and 85 patients in the ACL reconstruction group. There was no significant difference in the postoperative Lysholm score between the two groups (WMD, 2.21; 95% CI, −0.45–4.88; I2 = 0%; P = 0.10) (Figure 5B).
Tegner score was reported in 3 studies (11, 12, 31). There were 90 cases in the ACL repair group and 86 cases in the ACL reconstruction group. Compared to ACL reconstruction, ACL repair provided comparable improvements in the postoperative Tegner score (WMD, 0.06; 95% CI, −0.26–0.39; I2 = 0%; P = 0.70) (Figure 5C).
A total of 3 studies (11, 12, 14) reported satisfaction (range, 0–10; 0 representing unsatisfied and 10 representing very satisfied) after surgery. With 96 patients in the ACL repair group and 91 patients in the ACL reconstruction group, no significant difference regarding patient satisfaction after surgery was found between the two groups (WMD, −0.10; 95% CI, −0.37–0.17; I2 = 36%; P = 0.45) (Figure 5D).
Subgroup Analyses
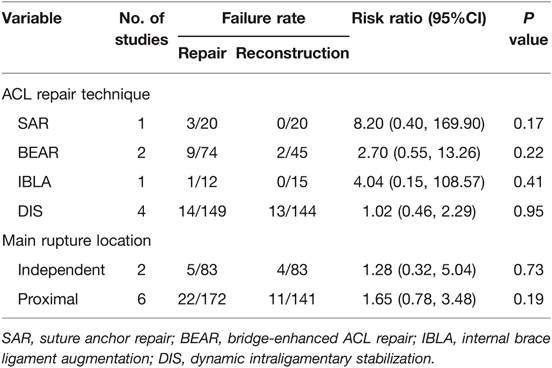
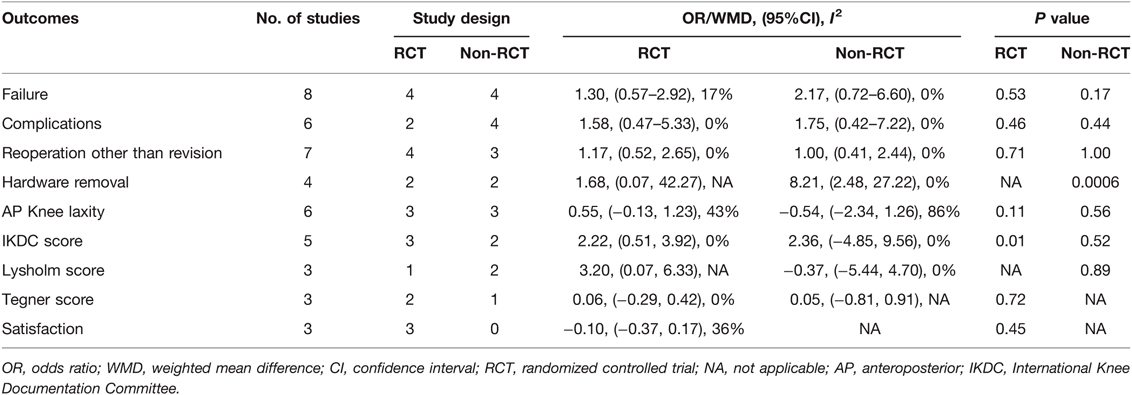
Subgroup analyses for the primary outcome failure rates according to the rupture location and ACL repair technique were performed. No significant differences between different repair techniques and rupture locations were observed (Table 3). Subgroup analyses according to RCT design or non-RCT design were also conducted for all outcomes including failure, complications, reoperation other than revision, hardware removal rates, AP Knee laxity and patient-reported outcomes, but no significant differences or changes of outcomes were found according to the designs (Table 4). All the important outcomes are listed in Table 5.
Discussion
This is the first meta-analysis to compare primary arthroscopic ACL repair to gold standard autograft ACL reconstruction. Different from previous results, this study revealed that, with a mean follow-up period from 12 to 36 months, patients who underwent arthroscopic ACL repair had statistically comparable outcomes of failure, complications, reoperation other than revision, Lysholm score, Tegner score, and satisfaction when compared with autograft ACL reconstruction. In addition, arthroscopic ACL repair showed subtle advantages in terms of the IKDC score but a higher rate of hardware removal and possibly greater ΔATT than ACL reconstruction.
ACL reconstruction has become the gold standard surgical treatment for ACL ruptures since the late 20th century. However, Van der List et al. (33) reviewed the evolutionary history of ACL surgical treatment modalities, and proposed that the paradigm shifting away from primary ACL repair was partly due to “unfortunate timing”. Immature arthroscopic technology, a long period of immobilization after surgery (34, 35), and an unbefitting choice of patients (1) contributed to poor outcomes following open ACL repair. In 1991, Sherman et al. (1) reported an important finding that patients with proximal tears and good tissue quality tended to have significantly better clinical results than those with other types of tears. In 1993, Genelin et al. (36) performed open repair for patients with proximal ACL tears, and observed excellent outcomes at mid-term follow-up. Several studies (37–39) had already reported similar favorable outcomes in the early 1980s. A systematic review by Van der List et al. (40) found that open primary ACL repair yielded excellent outcomes in patients with proximal tears. These results suggested that primary arthroscopic ACL repair might play a role in treating proximal ACL tears. Previous systematic reviews (6, 7, 9, 10) revealed that ACL reconstruction led to better survivorship and improvement in postoperative function than arthroscopic ACL repair, but the use of internal bracing, biological augmentation, and dynamic stabilization had the potential to increase the success rate of repair. With some newly published studies enrolled, this is the first review to report that arthroscopic ACL repair is not inferior to autograft ACL reconstruction, and even has some advantages over reconstruction.
In theory, primary arthroscopic ACL repair techniques have some advantages over autograft ACL reconstruction. For example, proprioception should be maintained (41), less invasive, early range of motion (ROM) regain (24), native kinematics should be restored (42), donor site morbidity should be avoided, and osteoarthritis should be prevented (43). In addition, standard ACL reconstruction can be easily performed if primary ACL repair fails, while revision surgery for failed ACL reconstruction is much more complex. Studies included in our meta-analysis showed outcomes in favor of these advantages. Vermeijden et al. (29) observed that patients who underwent ACL repair had less awareness of their operated knees than those who underwent reconstruction at the 2- to 5- year follow-up, especially in patients older than 30 years, male patients and patients with a body mass index larger than 25. Schliemann et al. (14) reported that there were no significant differences between the two groups for knee kinematic and kinetic parameters at any time of the 6-month follow-up, but those in the DIS group had better early activity at weeks 2 and 3 after surgery. Ortmaier et al. (31) concluded that patients with IBLA had the same return-to-sports activity level as patients with classic ACL reconstruction at short-term follow-up. However, whether these advantages can be maintained at longer follow-up is unclear, and needs to be verified by further studies.
In this meta-analysis, potential disadvantages of ACL repair were also observed. ACL repair showed a significantly higher rate of hardware removal, mainly due to more requests for implant removal in patients with DIS repair. In the DIS procedure, the monobloc spring- screw is much bulkier than that used in ACL reconstruction, because it has to withstand a high tensile load. Although it is unnecessary to remove the spring- screw when ACL heals, Henle et al. (44) reported that nearly half of patients asked to remove it without any clinical need, while this procedure is uncommonly performed after ACL reconstruction (45, 46). This might be a disadvantage of DIS, but the hardware removal procedure is a minimally invasive operation under local anesthesia, yielding almost no negative effects on the recovery process.
Another potential disadvantage of ACL repair is AP knee laxity. Inconsistent results were reported in the included studies. The overall pooled outcome suggested no significant difference between ACL repair and reconstruction, but the heterogeneity was considered to be high (I2 = 80%). This heterogeneity might be caused by the differences in study design and ACL repair techniques. After removing the study by Szwedowski et al. (28), the I2 decreased to 32%, and ACL repair showed significantly larger ΔATT than reconstruction. These results indicated that arthroscopic ACL repair might be related to greater AP knee laxity than reconstruction, but this asymptomatic laxity can only be observed when stress is exerted on the knees. Further studies should pay attention to long-term postoperative AP knee laxity in the two groups.
To further explore potential factors that would influence failure rates, we performed subgroup analyses. The rupture location and ACL repair technique are essential. Among the 10 included studies, 8 studies (11–13, 26, 28, 29, 31, 32) mainly enrolled patients with proximal ruptures, and the other 2 studies (14, 30) enrolled patients regardless of the rupture location. For ACL repair techniques, 1 study (32) used SAR, 2 studies (13, 26) used BEAR, 3 studies (28, 29, 31) used IBLA, and 4 studies (11, 12, 14, 30) used DIS. After subgroup analyses according to the rupture location and repair technique, no significant differences between different rupture locations and repair techniques were observed. However, these results should be interpreted with caution because the number of studies that enrolled patients regardless of the rupture location was only 2, and the number of studies using SAR and BEAR was also limited.
This study is not without limitation. First, although we enrolled more comparative studies than any other previous systematic review, the number of RCTs was only 4, and the majority of included studies were cohort and case–control studies. Second, due to a short history of arthroscopic ACL repair, the mean follow-up period of the included studies was not long enough (12–36 months). Third, the ACL repair techniques are varied, and differences in detailed surgical methods and the type of graft for ACL reconstruction were inevitable. However, the biomechanical effect of ACL reconstructions could be considered to be approximately equivalent. Fourth, we failed to conduct a meta-analysis of radiological results after surgery. Although good radiological results were observed, only 2 studies reported ACL healing examined by MRI and 1 study reported signs of osteoarthritis detected by X-rays at the 2-year follow up. Last, rehabilitation courses after surgery varied among studies, which could have influenced postoperative outcomes.
Conclusion
Compared to the autograft ACL reconstruction, arthroscopic ACL repair showed similar clinical outcomes, and even better functional performance in treating proximal ACL ruptures. ACL repair has a higher rate of hardware removal, and might be related to greater asymptomatic knee laxity. Arthroscopic ACL repair might be a viable option for patients with proximal ACL ruptures. However, limited by the amount of high-quality evidence (only 4 RCTs), we cannot draw a definite conclusion. More high-quality prospective trials comparing these two techniques are needed to confirm our findings.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
JZ and XT conceived the idea; LP and TL: screened the literature, extracted data, assessed the methodological quality of the enrolled studies and performed the data analyses; TL and YL: prepared the tables and figures; all authors contributed to the writing and revisions. All authors contributed to the article and approved the submitted version.
Funding
This study was supported in part by grants from National Natural Science Foundation of China (82072514; Xin Tang) and Science & Technology Department of Sichuan Province (2021YFS0238; Xin Tang).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I. The long-term followup of primary anterior cruciate ligament repair. Defining a rationale for augmentation. Am J Sports Med. (1991) 19(3):243–55. doi: 10.1177/036354659101900307
2. Engebretsen L, Benum P, Fasting O, Mølster A, Strand T. A prospective, randomized study of three surgical techniques for treatment of acute ruptures of the anterior cruciate ligament. Am J Sports Med. (1990) 18(6):585–90. doi: 10.1177/036354659001800605
3. Odensten M, Lysholm J, Gillquist J. Suture of fresh ruptures of the anterior cruciate ligament: a 5-year follow-up. Acta Orthop Scand. (1984) 55(3):270–2. doi: 10.3109/17453678408992354
4. Feagin JA Jr, Curl WW. Isolated tear of the anterior cruciate ligament: 5-year follow-up study. Am J Sports Med. (1976) 4(3):95–100. doi: 10.1177/036354657600400301
5. Heusdens CHW. ACL repair: a game changer or will history repeat itself? A critical appraisal. J Clin Med. (2021) 10(5):912. doi: 10.3390/jcm10050912
6. van Eck CF, Limpisvasti O, ElAttrache NS. Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. Am J Sports Med. (2018) 46(9):2291–8. doi: 10.1177/0363546517717956
7. Ahmad SS, Schreiner AJ, Hirschmann MT, Schröter S, Döbele S, Ahrend MD, et al. Dynamic intraligamentary stabilization for ACL repair: a systematic review. Knee Surg Sports Traumatol Arthrosc. (2019) 27(1):13–20. doi: 10.1007/s00167-018-5301-z
8. van der List JP, Vermeijden HD, Sierevelt IN, DiFelice GS, van Noort A, Kerkhoffs G. Arthroscopic primary repair of proximal anterior cruciate ligament tears seems safe but higher level of evidence is needed: a systematic review and meta-analysis of recent literature. Knee Surg Sports Traumatol Arthrosc. (2020) 28(6):1946–57. doi: 10.1007/s00167-019-05697-8
9. Nwachukwu BU, Patel BH, Lu Y, Allen AA, Williams RJ 3rd., Anterior cruciate ligament repair outcomes: an updated systematic review of recent literature. Arthroscopy. (2019) 35(7):2233–47. doi: 10.1016/j.arthro.2019.04.005
10. Hoogeslag RAG, Brouwer RW, de Vries AJ, Boer BC, Huis In ‘t Veld R. Efficacy of nonaugmented, static augmented, and dynamic augmented suture repair of the ruptured anterior cruciate ligament: a systematic review of the literature. Am J Sports Med. (2020) 48(14):3626–37. doi: 10.1177/0363546520904690
11. Hoogeslag RAG, Brouwer RW, Boer BC, de Vries AJ, Huis In ‘t Veld R. Acute anterior cruciate ligament rupture: repair or reconstruction? Two-year results of a randomized controlled clinical trial. Am J Sports Med. (2019) 47(3):567–77. doi: 10.1177/0363546519825878
12. Kösters C, Glasbrenner J, Spickermann L, Kittl C, Domnick C, Herbort M, et al. Repair with dynamic intraligamentary stabilization versus primary reconstruction of acute anterior cruciate ligament tears: 2-year results from a prospective randomized study. Am J Sports Med. (2020) 48(5):1108–16. doi: 10.1177/0363546520905863
13. Murray MM, Fleming BC, Badger GJ, Freiberger C, Henderson R, Barnett S, et al. Bridge-enhanced anterior cruciate ligament repair is not inferior to autograft anterior cruciate ligament reconstruction at 2 years: results of a prospective randomized clinical trial. Am J Sports Med. (2020) 48(6):1305–15. doi: 10.1177/0363546520913532
14. Schliemann B, Glasbrenner J, Rosenbaum D, Lammers K, Herbort M, Domnick C, et al. Changes in gait pattern and early functional results after ACL repair are comparable to those of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. (2018) 26(2):374–80. doi: 10.1007/s00167-017-4618-3
15. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clin Res). (2009) 339:b2700. doi: 10.1136/bmj.b2700
16. Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R, et al. Reliability and validity of the international knee documentation committee (IKDC) subjective knee form. Joint Bone Spine. (2007) 74(6):594–9. doi: 10.1016/j.jbspin.2007.01.036
17. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. (1982) 10(3):150–4. doi: 10.1177/036354658201000306
18. Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. (2009) 37(5):890–7. doi: 10.1177/0363546508330143
19. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clin Res). (2011) 343:d5928. doi: 10.1136/bmj.d5928
20. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. (2003) 73(9):712–6. doi: 10.1046/j.1445-2197.2003.02748.x
21. Gagliardi AG, Carry PM, Parikh HB, Traver JL, Howell DR, Albright JC. ACL repair with suture ligament augmentation is associated with a high failure rate among adolescent patients. Am J Sports Med. (2019) 47(3):560–6. doi: 10.1177/0363546518825255
22. Jonkergouw A, van der List JP, DiFelice GS. Arthroscopic primary repair of proximal anterior cruciate ligament tears: outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg Sports Traumatol Arthrosc. (2019) 27(1):21–8. doi: 10.1007/s00167-018-5338-z
23. Sporsheim AN, Gifstad T, Lundemo TO, Engebretsen L, Strand T, Mølster A, et al. Autologous BPTB ACL reconstruction results in lower failure rates than ACL repair with and without synthetic augmentation at 30 years of follow-up: a prospective randomized study. J Bone Joint Surg Am Vol. (2019) 101(23):2074–81. doi: 10.2106/JBJS.19.00098
24. van der List JP, DiFelice GS. Range of motion and complications following primary repair versus reconstruction of the anterior cruciate ligament. Knee. (2017) 24(4):798–807. doi: 10.1016/j.knee.2017.04.007
25. Connolly PT, Zittel KW, Panish BJ, Rigor PD, Argintar EH. A comparison of postoperative pain between anterior cruciate ligament reconstruction and repair. European J Orthop Surg Traumatol. (2021) 31(7):1403–9. doi: 10.1007/s00590-020-02859-0
26. Murray MM, Kalish LA, Fleming BC, Flutie B, Freiberger C, Henderson RN, et al. Bridge-enhanced anterior cruciate ligament repair: two-year results of a first-in-human study. Orthop J Sports Med. (2019) 7(3):2325967118824356. doi: 10.1177/2325967118824356
27. Murray MM, Flutie BM, Kalish LA, Ecklund K, Fleming BC, Proffen BL, et al. The bridge-enhanced anterior cruciate ligament repair (BEAR) procedure: an early feasibility cohort study. Orthop J Sports Med. (2016) 4(11):2325967116672176. doi: 10.1177/2325967116672176
28. Szwedowski D, Paczesny Ł, Zabrzyński J, Gagat M, Domżalski M, Huri G, et al. The Comparison of clinical result between primary repair of the anterior cruciate ligament with additional internal bracing and anatomic single bundle reconstruction-A retrospective study. J Clin Med. (2021) 10(17):3948. doi: 10.3390/jcm10173948
29. Vermeijden HD, van der List JP, O’Brien R, DiFelice GS. Patients forget about their operated knee more following arthroscopic primary repair of the anterior cruciate ligament than following reconstruction. Arthroscopy. (2020) 36(3):797–804. doi: 10.1016/j.arthro.2019.09.041
30. Bieri KS, Scholz SM, Kohl S, Aghayev E, Staub LP. Dynamic intraligamentary stabilization versus conventional ACL reconstruction: a matched study on return to work. Injury. (2017) 48(6):1243–8. doi: 10.1016/j.injury.2017.03.004
31. Ortmaier R, Fink C, Schobersberger W, Kindermann H, Leister I, Runer A, et al. Return to sports after anterior cruciate ligament injury: a matched-pair analysis of repair with internal brace and reconstruction using hamstring or quadriceps tendons. Sportverletz Sportschaden. (2021) 35(1):36–44. doi: 10.1055/a-1019-0949
32. Achtnich A, Herbst E, Forkel P, Metzlaff S, Sprenker F, Imhoff AB, et al. Acute proximal anterior cruciate ligament tears: outcomes after arthroscopic suture anchor repair versus anatomic single-bundle reconstruction. Arthroscopy. (2016) 32(12):2562–9. doi: 10.1016/j.arthro.2016.04.031
33. van der List JP, DiFelice GS. Primary repair of the anterior cruciate ligament: a paradigm shift. Surgeon. (2017) 15(3):161–8. doi: 10.1016/j.surge.2016.09.006
34. Enneking WF, Horowitz M. The intra-articular effects of immobilization on the human knee. J Bone Joint Surg Am. (1972) 54(5):973–85. doi: 10.2106/00004623-197254050-00003
35. Millett PJ, Wickiewicz TL, Warren RF. Motion loss after ligament injuries to the knee. part I: causes. Am J Sports Med. (2001) 29(5):664–75. doi: 10.1177/03635465010290052401
36. Genelin F, Trost A, Primavesi C, Knoll P. Late results following proximal reinsertion of isolated ruptured ACL ligaments. Knee Surg Sports Traumatol Arthrosc. (1993) 1(1):17–9. doi: 10.1007/BF01552153
37. Strand T, Engesaeter LB, Mølster AO, Raugstad TS, Stangeland L, Stray O, et al. Knee function following suture of fresh tear of the anterior cruciate ligament. Acta Orthop Scand. (1984) 55(2):181–4. doi: 10.3109/17453678408992333
38. Marshall JL, Warren RF, Wickiewicz TL. Primary surgical treatment of anterior cruciate ligament lesions. Am J Sports Med. (1982) 10(2):103–7. doi: 10.1177/036354658201000208
39. Weaver JK, Derkash RS, Freeman JR, Kirk RE, Oden RR, Matyas J. Primary knee ligament repair–revisited. Clin Orthop Relat Res. (1985) 199:185–91. doi: 10.1097/00003086-198510000-00026
40. van der List JP, DiFelice GS. Role of tear location on outcomes of open primary repair of the anterior cruciate ligament: a systematic review of historical studies. Knee. (2017) 24(5):898–908. doi: 10.1016/j.knee.2017.05.009
41. Halinen J, Lindahl J, Hirvensalo E, Santavirta S. Operative and nonoperative treatments of medial collateral ligament rupture with early anterior cruciate ligament reconstruction: a prospective randomized study. Am J Sports Med. (2006) 34(7):1134–40. doi: 10.1177/0363546505284889
42. Fleming BC, Carey JL, Spindler KP, Murray MM. Can suture repair of ACL transection restore normal anteroposterior laxity of the knee? An ex vivo study. J Orthop Res. (2008) 26(11):1500–5. doi: 10.1002/jor.20690
43. Murray MM, Fleming BC. Use of a bioactive scaffold to stimulate anterior cruciate ligament healing also minimizes posttraumatic osteoarthritis after surgery. Am J Sports Med. (2013) 41(8):1762–70. doi: 10.1177/0363546513483446
44. Henle P, Röder C, Perler G, Heitkemper S, Eggli S. Dynamic Intraligamentary Stabilization (DIS) for treatment of acute anterior cruciate ligament ruptures: case series experience of the first three years. BMC Musculoskelet Disord. (2015) 16:27. doi: 10.1186/s12891-015-0484-7
45. Laxdal G, Kartus J, Ejerhed L, Sernert N, Magnusson L, Faxén E, et al. Outcome and risk factors after anterior cruciate ligament reconstruction: a follow-up study of 948 patients. Arthroscopy. (2005) 21(8):958–64. doi: 10.1016/j.arthro.2005.05.007
Keywords: ACL (anterior cruciate ligament), arthroscopic ACL repair, autograft ACL reconstruction, meta-analysis, arthroscope
Citation: Pang L, Li P, Li T, Li Y, Zhu J and Tang X (2022) Arthroscopic Anterior Cruciate Ligament Repair Versus Autograft Anterior Cruciate Ligament Reconstruction: A Meta-Analysis of Comparative Studies. Front. Surg. 9:887522. doi: 10.3389/fsurg.2022.887522
Received: 1 March 2022; Accepted: 5 April 2022;
Published: 20 April 2022.
Edited by:
Paphon Sa-ngasoongsong, Ramathibodi Hospital, Mahidol University, ThailandReviewed by:
Jatupon Kongtharvonskul, Mahidol University, ThailandChaiyanun Vijittrakarnrung, Ramathibodi Hospital, Mahidol University, Thailand
Copyright Copyright © 2022 Pang, Li, Li, Li, Zhu, and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Zhu zhu-jing2008@163.com Xin Tang tangxin9388@163.com
†These authors have contributed equally to this work and share first authorship
Speciality section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Long Pang1†
Long Pang1† Xin Tang
Xin Tang