- 1Fuyang People's Hospital, Fuyang, China
- 2Department of Orthopedics, The Second Affifiliated Hospital of Anhui Medical University, Hefei, China
- 3Center for Clinical Medicine, Huatuo Institute of Medical Innovation (HTIMI), Berlin, Germany
- 4Anhui Medical University, Fuyang, China
- 5Anhui Armed Police General Hospital, Hefei, China
Objective: The study aims to explore the feasibility and clinical effect of posterior minimally invasive treatment of cruciate ligament tibial avulsion fracture.
Methods: Posterior knee minimally invasive approach was used to treat avulsion fracture of posterior cruciate ligament (PCL) tibia in 15 males and 11 females. The length of the incision, intraoperative blood loss, operation time, postoperative hospital stay, residual relaxation, and fracture healing time were analyzed to evaluate the curative effect, learning curve, and advantages of the new technology. Neurovascular complications were recorded. During the postoperative follow-up, the International Knee Joint Documentation Committee (IKDC), Lysholm knee joint score, and knee joint range of motion were recorded to evaluate the function.
Results: All 26 patients were followed up for 18–24 months, with an average of 24.42 ± 5.00 months. The incision length was 3–6 cm, with an average of 4.04 ± 0.82 cm. The intraoperative blood loss was about 45–60 ml, with an average of 48.85 ± 5.88 ml. The operation time was 39–64 min, with an average of 52.46 ± 7.64 min. The postoperative hospital stay was 2–5 days, with an average of 2.73 ± 0.87 days. All incisions healed grade I without neurovascular injury. All fractures healed well with an average healing time of 9.46 ± 1.33 weeks (range, 8–12 weeks). The Lysholm score of the affected knee was 89–98 (mean, 94.12 ± 2.49) at 12-month follow-up. The IKDC score was 87–95 with an average of 91.85 ± 2.19, and the knee range of motion was 129–148° with an average of 137.08 ± 5.59°. The residual relaxation was 1–3 mm, with an average of 1.46 ± 0.65 mm.
Conclusion: This minimally invasive method provides sufficient exposure for internal fixation of PCL tibial avulsion fractures without the surgical complications associated with traditional open surgical methods. The process is safe, less invasive, and does not require a long learning curve.
Background
As the most complicated joint of human body, the stability of knee joint depends on the surrounding ligaments to a great extent. Posterior cruciate ligament (PCL) is the necessary ligament to maintain the stability of the knee joint, and it is also the main limiting factor to prevent excessive posterior tibial movement. Its fracture and injury will greatly affect the stability of the knee joint (1).
PCL injury accounts for 3%–44% of acute knee joint injuries and is often accompanied by other ligament injuries (2–4). The avulsion fracture of PCL is a kind of knee joint injury, which can easily lead to instability of knee joint and accelerate the long-term degeneration of knee joint. The avulsion fracture of the tibia is usually caused by high-energy injuries, which are common in motorcycle accidents (5, 6). At this time, the knee joint is in a bent position or in an overextended position. If the upper end of the tibia is subjected to violence from front to back, the tension on the PCL will easily exceed its tolerance limit, which will lead to injuries such as PCL fracture. Due to the anatomical characteristics of PCL tibial attachment points, some of them are located outside the joint cavity. When the avulsion fracture of PCL tibial insertion occurs, the fracture end is often embedded in the joint capsule and surrounding soft tissues, which makes it difficult to reduce the fracture by manipulation. If the torn pieces are not displaced, nonsurgical treatment can be recommended. At present, it is considered that the main treatment for avulsion fracture of displaced PCL tibial insertion is surgical treatment to restore PCL function and knee stability (7, 8), and avulsion fracture of PCL tibial attachment is considered an indication of surgical reduction and internal fixation (9). The main surgical treatments include open reduction and internal fixation (10–13) and arthroscopic reduction and internal fixation (14–16). Although there are many case series published on the management and outcomes of PCL avulsion fractures, no optimal surgical management has been suggested (5, 17). This paper attempts to find a simpler and minimally invasive method to treat PCL tibial avulsion fracture, which does not need to dissect the surrounding soft tissues layer by layer, and at the same time better protect the surrounding muscles and blood vessels and nerves. We intend to use this new minimally invasive approach to fix PCL tibial avulsion fracture, which has been successfully applied to 26 patients. The effectiveness, safety, and advantages of this method are analyzed by using the results measurement method of clinician's specialist evaluation and patient report.
Clinical data
General information
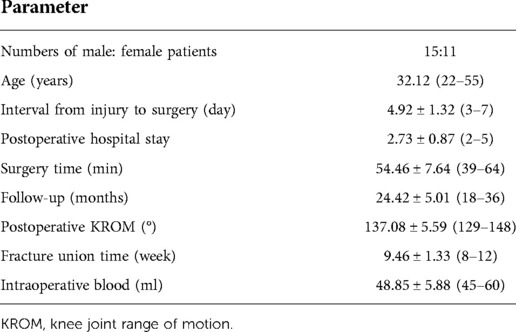
From January 2015 to January 2020, 26 cases of PCL tibial avulsion fracture were studied retrospectively at the orthopaedics departments of both Second Affiliated Hospital of Anhui Medical University and Anhui Armed Police General Hospital, Hefei, China. After all patients were admitted to the hospital, routine biochemical and physical examinations were completed, and their physical condition and surgical tolerance were fully evaluated. Lachman test and back drawer test were positive before operation; and x-ray, computed tomography (CT) scanning + three-dimensional reconstruction, and magnetic resonance imaging (MRI) (Figure 1) examination of the knee joint of the affected limb were improved, so as to facilitate the evaluation of fracture size and the selection of internal fixation devices during operation. The consent of patients and their families was obtained before operation.
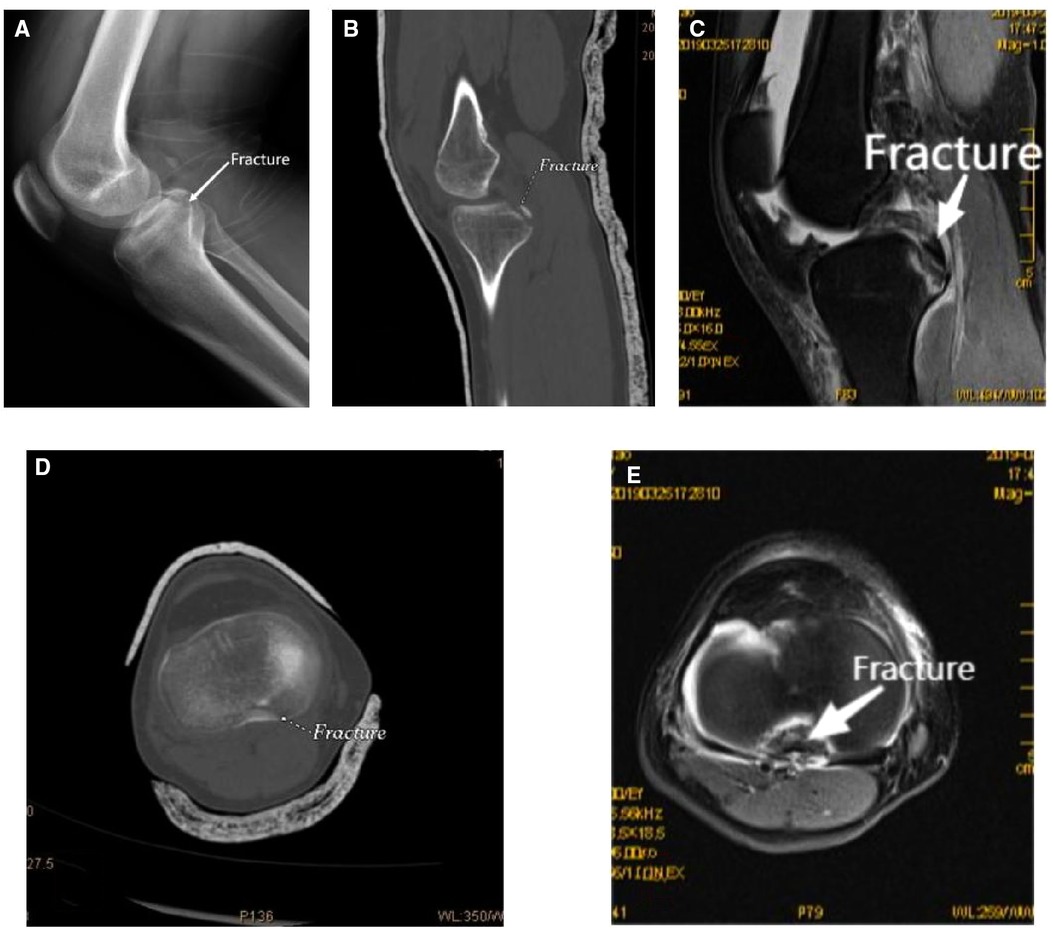
Figure 1. Preoperative x-ray, CT, and MRI of the patient [(B,C) sagittal view; (D,E) transverse view]. CT, computed tomography; MRI, magnetic resonance imaging.
Inclusion criteria
(1) Fresh PCL tibial avulsion fracture (fracture within 3 weeks);
(2) Lachman test and back drawer test were positive before operation;
(3) Meyers–McKeever II and III, and preoperative CT measurements of fracture block size can be fixed by hollow lag screws;
(4) Knee joint function was good before injury;
(5) Follow-up for more than 12 months, complete imaging data; and
(6) The images obtained showed that the mean fracture displacement of PCL was ≥6.7 mm (18).
Exclusion criteria
(1) Patients with anterior cruciate ligament, collateral ligament, and meniscus injury;
(2) Preoperative MRI showed PCL rupture;
(3) Osteoarthritis with previous joint dysfunction, history of knee joint trauma or Kellgren–Lawrence grade ≥2;
(4) Patients with distal femur or proximal tibia fracture; and
(5) Preoperative surgical evaluation, patients with severe heart, respiratory, and other medical diseases who cannot be operated on.
Surgical technique
All of the patients were operated on by three senior orthopedic surgeons of the same team. General anesthesia was used as the anesthesia method. After satisfactory anesthesia, an electric pneumatic tourniquet was tied in the prone position at the root of the thigh of the affected limb. The pressure of the tourniquet was set at 280 mmHg, and the knee joint was flexed from 30° to 45° to fully relax the medial gastrocnemius muscle.
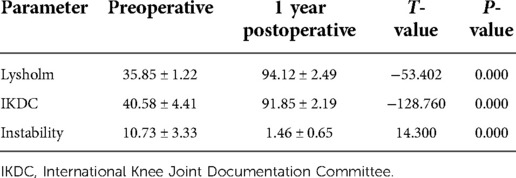
Before the operation, a 3–4 cm surgical mark was made along the medial margin of the gastrocnemius muscle from 1 to 2 cm above the popliteal stria; routine disinfection and towel laying were performed. A 3–4 cm incision was performed from the medial side of the popliteal stria along with the preoperative surgical incision mark. The medial margin of the medial head of the gastrocnemius muscle was determined. The anatomical gap between the medial head of the gastrocnemius muscle and the semitendinosus muscle was bluntly dissected with fingers, and the lateral margin of the medial head of the gastrocnemius muscle was bluntly separated from the semitendinosus muscle. The medial head of the gastrocnemius muscle and the vascular nerve in popliteal fossa were pulled outward with a thyroid hook, and the semimembrane muscle and semitendinosus muscle were pulled medially. At this time, the thick muscle belly could play a role in protecting the vascular nerve structure, and no pressure was directly applied to the vascular nerve during the operation. Therefore, dissection of the protected medial popliteal fossa is relatively safe. Until the posterior congestion and swelling of the joint capsule are exposed, the avulsion fracture fragment could be seen by a longitudinal incision of the joint capsule, and the fracture fragment was lifted along with the PCL. The surgical site was fully washed with normal saline, the surrounding soft tissue embedded in the fracture fragment was cleaned, and the fracture fragment was reduced to the bone bed. 1–2 Kirschner wires were vertically placed at the upper edge of the bone bed, and the direction and depth of the Kirschner wires were visualized to avoid damage to the surrounding articular cartilage. When the direction and position were good, 1–2 hollow lag screws with a diameter of 4.0 mm and partial thread were used for fixation according to the size of the fracture block during the operation. Spacers can be used according to the intraoperative conditions. After the fluoroscopic position and depth of the C-arm machine were good during the operation, the incision was sutured layer by layer after a drainage tube was inserted (Figure 2). An illustration of surgical anatomy of PCL tibial avulsion fracture is shown in Figure 3. The knee joint of the affected limb was fixed at a flexion position of 30°–45° using a functional adjustable knee brace.
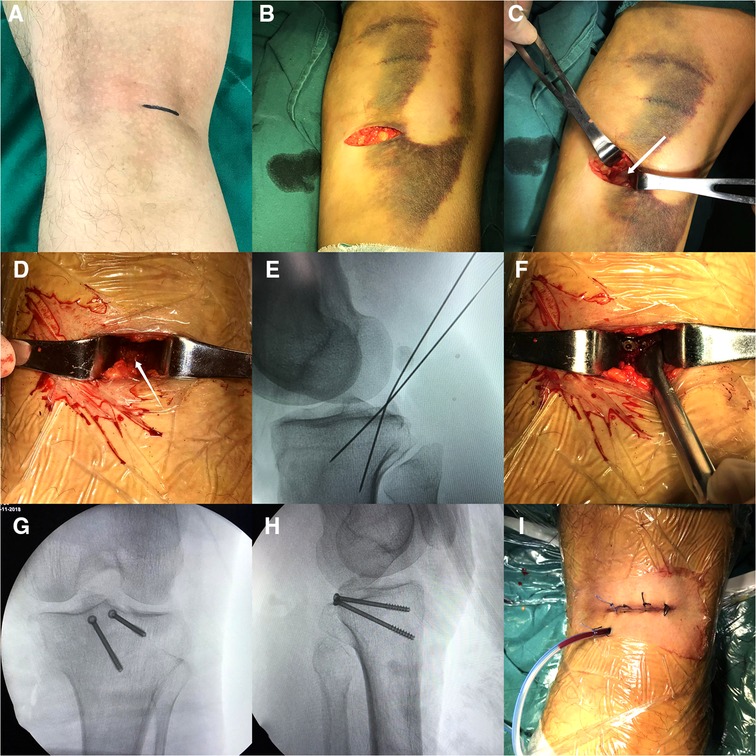
Figure 2. (A–C) A 3–4 cm surgical incision was performed along the preoperative marker, the gastrocnemius muscle's medial head was separated, and the joint capsule was fully exposed by pulling outward. (D–F) The joint capsule was cut open, washed, the fracture block was reduced, and the Kirschner wire was used for temporary fixation. Cannulated lag screws were used for fixation after the fracture was well positioned in fluoroscopic position. (G–I) The intraoperative fluoroscopic anterolateral x-ray film was satisfactory, and the incision was closed layer by layer after rinsing and inserting the drainage tube.
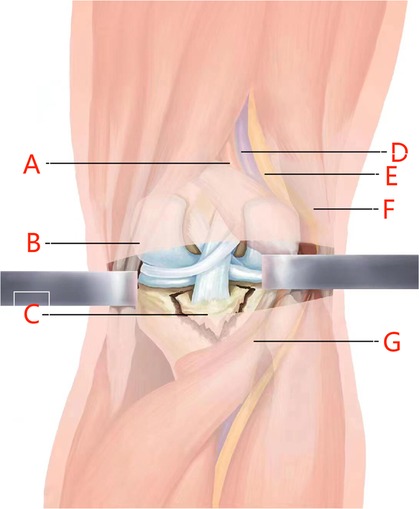
Figure 3. Illustration of surgical anatomy of PCL tibial avulsion fracture. [(A) Popliteal artery; (B) semitendinosus muscle; (C) avulsion fracture of posterior cruciate ligament; (D) popliteal vein; (E) tibial nerve; (F) long head of biceps femoris; (G) medial head of gastrocnemius muscle]. PCL, posterior cruciate ligament.
Postoperative treatment and rehabilitation
Antibiotics were routinely used once within 24 h after operation to prevent infection. A functional adjustable knee brace was used to fix the knee joint of the affected limb at a flexion position of 30°–45°, and a cotton pad was used to prevent posterior displacement of the tibia. After returning to the ward, the patient was encouraged to start ankle pump exercise, quadriceps femoris contraction, and other functional exercises, and straight leg elevation training was performed 1 day after surgery. Passive knee flexion range of motion (0°–60°) was completed within 3 weeks after operation. At 4–6 weeks after surgery, the patient was in active flexion (0°–90°) in the prone position. After 8 weeks, normal knee movement can be restored, and the knee brace of the affected limb can be removed. During the first 4 weeks after surgery, toe contact or partial weight bearing on the leg was allowed, and physical therapy for knee mobility was initiated. Full weight bearing was permitted only after radiographs showed good evidence of bone healing. After 2–3 months, when sufficient strength, knee joint range of motion (KROM), and proprioceptive skills are restored, return to heavy strength or competitive physical activity is limited. The minimally invasive approach group could be exercised as early as the patient could tolerate. A regular monthly x-ray examination was performed to observe whether avulsion fracture of the affected limb reached the clinical healing standard. IKDC score, Lysholm score, and KROM score were recorded for the first time and each time after operation to evaluate the improvement of knee joint function and stability of the affected limb.
Observation index
The Lachman test and posterior drawer test were observed after limb surgery. Patients were followed up at 4 weeks, 6 weeks, 2 months, 3 months, and every month thereafter, during which the affected limb was evaluated using the IKDC form and the Lysholm scale. The range of motion and residual relaxation of the knee were measured. All clinical evaluations were performed by two independent observers who were blinded to the surgical procedure. The IKDC score, Lysholm score, knee range of motion, and residual relaxation of the affected limb at 1 year after operation were analyzed to evaluate the recovery of the affected limb.
Statistical methods
For data analysis, the statistical software Spss23.0 was used. Measurement data with a normal distribution were expressed as mean standard deviation, and the t-test was used to compare the Lysholm score, IKDC score, and residual relaxation between preoperative and postoperative patients. P < 0.05 indicates statistical significance between the two groups, which is used to assess the clinical efficacy of surgery.
Results
All the operations were successfully completed, and the incision was healed at stage I. There were no complications such as incision infection, intra-articular infection, joint fibrosis, deep vein thrombosis, and fracture nonunion. The drawer test after Lachman test was negative, and the knee stability recovered well after operation. All 26 patients were followed up 18–24 months, with an average of 24.42± 5.01 months. The incision length was 3–6 cm, with an average of 4.04 ± 0.82 cm. The intraoperative blood loss was about 45–60 ml, with an average of 48.85 ± 5.88 ml. The operation time was 39–64 min, with an average of 52.46 ± 7.64 min. The postoperative hospital stay was 2–5 days, with an average of 2.73 ± 0.87 days. All fractures healed 8–12 weeks, with an average healing time of 9.46 ± 1.33 weeks (Table 1).
The Lysholm score of the affected knee was 89–98 (mean 94.12 ± 2.49) at 1 year follow-up. The IKDC score was 87–95 with an average of 91.85 ± 2.19, and the KROM was 129°–148° with an average of 137.08 ± 5.59°, which was statistically significant compared with that before surgery (P < 0.05) (Table 2).
Discussion
The aim of this study was to explore a new, minimally invasive, and safe surgical method for tibial PCL avulsion fracture that could fully expose the field of vision in a safer way without requiring large incisions, reduce the dissection and treatment of the surrounding muscle tissue, and avoid damage to the surrounding vascular and nerve systems.
The strength of the PCL is about twice that of the ACL, and it is considered to be the strongest ligament in the knee joint, which plays an important role in the stability of the joint (19). The incidence of PCL rupture is lower than that of other ligaments, which is related to its strong fibrous structure (20). PCL tibial avulsion fracture is a special form of PCL injury that is relatively rare compared with typical PCL tear (17, 21). The treatment of PCL tibial avulsion fracture is mainly divided into conservative treatment and surgical treatment. Zhao et al. believed that nonsurgical treatment can be successfully used for fractures with displacement less than 5 mm (22). Yoon et al. found that conservative treatment could achieve satisfactory results when the displacement of a simple PCL avulsion fracture was less than 6.7 mm (18). Although these conservative treatments have achieved good results, there are many complications in the late stages of the conservative treatment of displaced PCL tibial avulsion fractures, which are easy to lead to knee instability, severe mobility limitation, and knee degeneration. In order to prevent instability and further degenerative changes, early operation should be performed (23–25).
At present, the surgical options for PCL tibial avulsion fracture mainly include arthroscopic repair and open reduction and internal fixation. According to certain studies, the clinical efficacy of open approach and arthroscopic fixation of PCL tibial avulsion fractures is comparable (23, 26, 27). Since the use of arthroscopic surgery was first reported in 1995, with the progress of arthroscopic technology, arthroscopic treatment of PCL tibial avulsion fractures has been widely concerned (4, 28, 29). Although arthroscopic technology provides a minimally invasive technique and can be used in the same environment to handle any accompanying advantage of the meniscus, the synovial membrane and the surrounding ligament injury (14, 29–31), on the contrary, in addition to the requirements of technical and logical reasoning, it shows a higher rate of arthrofibrosis, longer operation time, high technical requirements, a long learning curve, the need for a specific device. In contrast to the open technique, it is not possible to see the avulsion fragment directly. In addition, arthroscopic reduction and fixation are more challenging than open surgery (32, 33).
Previous studies have reported a variety of surgical methods for tibial PCL avulsion fractures. Burks and Schaffer first described in 1990 a simplified retrogenicular inverted “L” approach that has become the standard open surgical approach for avulsion fractures of the PCL. The incision of this surgical approach is large and easy to damage the blood vessels and nerves (34). Nicandri et al. describe the “S” shape incision, this is a kind of improved after into the road, intraoperative do not need to remove gastrocnemius. However, this operation requires the separation and ligation of popliteal nerves, blood vessels, and muscles to find the fracture end, which increases the difficulty of the operation and postoperative complications (35).
This study's clinical results are comparable with those of recent studies that used different methods and techniques. The average operation time in this study was 54.46 ± 7.34 min, the average fracture union time was 9.46 ± 1.33 weeks, average Lysholm score was 94.12 ± 2.49, and average IKDC score was 91.85 ± 2.19. All patients' functional knee range of motion was restored, including full extension with a flexion of 137.08 ± 5.59° and an average residual relaxation of 1.46 ± 0.65 mm. Khalifa et al. described 31 cases involving a small set plate and plate fixation via an open “S” approach. Lysholm score was 93.4 ± 3.9. The knee flexion was 120.7°, which allowed for full extension. The incision was large, and there was significant vascular and nerve damage in the popliteal fossa (10). Bi et al. reported 15 cases of three-channel arthroscopic surgery involving autologous tendon transplantation, TightRope, and interference screw fixation. Lysholm's score was 94.25 ± 3.32. The residual relaxation was 1.08 ± 0.86 mm, and IKDC score was 91.13 ± 3.78. This arthroscopic surgery causes little trauma and can repair joint tissue damage. However, the operation is difficult and requires special instruments, which are difficult to obtain in primary care hospitals (36). Among the 36 patients described by Hao et al., 20 were treated with a self-made hook plate posterior medial inverted “L” approach and 16 with an EndoButton under arthroscopy. The inverted “L” approach took 57.80 ± 5.60 min to complete. Fracture union took 11.05 ± 2.21 weeks, Lysholm score was 95.50 ± 3.19, and the knee flexion was 134.80 ± 4.94°. The arthroscopic operation took 67.81 8.69 min, the fracture union time was 11.88 ± 2.25 weeks, Lysholm score was 95.19 ± 2.61, and the knee flexion was 131.44 ± 7.30°. The clinical efficacy of the traditional approach and arthroscopy were compared in this study. There were no significant differences in fracture healing time, Lysholm score, or knee flexion between the two groups at the last follow-up, but the operation time of the traditional approach group was significantly shorter than that of the arthroscopy group, and the difference was statistically significant. In this study, there was no significant difference in fracture healing time, Lysholm score, or knee flexion operation time when compared with the traditional inverted “L” approach. However, in our study, the surgical incision was smaller, the postoperative appearance was more attractive, the damage to the surrounding soft tissues was less severe, and the patients were able to exercise sooner (12). Gavaskar et al. described 22 patients whose surgical methods were similar to those used in this study, including the use of a small incision behind the knee. The difference was that Gavaskar et al. used a C-arm machine for fluoroscopic positioning prior to surgery to improve the accuracy of the incision position. The use of a 2-cm-wide Langenbeck retractor to separate the popliteal vascular and nerve bundles during surgery resulted in better visual field exposure and a shorter operation time (mean, 40 min), which is worth learning. However, the researchers separated the vascular and nerve bundles from the popliteal fossa, which could cause damage (37).
In this study, through a small transverse incision, the natural muscle gap between the medial head of the gastrocnemius muscle and the semitendinosus muscle was separated, and the vascular nerve bundle at the popliteal fossa was pulled to the lateral side together, thus avoiding the injury of the vascular nerve during operation. The operation can be performed under direct vision, which is beneficial to the reduction of the fracture block. In this study, the length of the incision and the degree of satisfaction with the scar after the operation are obviously better than those of a traditional operation. The operation time was not obviously prolonged (10), and the operation time may be further shortened for senior orthopedic surgeons as the operation progresses. Compared with arthroscopy, the operation time was significantly reduced (38). As with other surgical approaches, after operation, IKDC score, Lysholm score, knee joint mobility, and residual relaxation were significantly improved (31, 39).
In the treatment of PCL tibial avulsion fracture by minimally invasive small incision behind the knee, the following experiences are obtained in combination with literature and clinical practice: (1) for the displaced PCL tibial avulsion fracture, the operation should be performed as soon as possible, the limb swelling is light, the hierarchy is clear, and the reduction is easy. (2) The surgical incision should be 3–4 cm, which is too small for exposure, easy to cause tissue damage when pulling, and difficult to adjust the direction when inserting guide wire. (3) It is difficult to detect the meniscus, anterior cruciate ligament, and other structural injuries in this incision, so x-ray, CT, MRI, and other related examinations should be completed before operation. (4) Hollow screws were used for fixation, and three-dimensional CT reconstruction was performed as far as possible to determine the size and displacement direction of the avulsion bone block. Postoperatively, adjustable chuck knee brace was used for fixation. (5) When separating deep soft tissue, blunt separation with fingers was used to avoid injury to the popliteal vascular and nerve bundles, and the level and deep structure of separation could be sensed at the same time. (6) When inserting the guide wire, the operation should be strictly standardized, and the protective coat should be used to prevent tissue involvement and damage to the blood vessels and nerves; the direction of screw placement should be perpendicular to the fracture surface, so as to make the pressure between bone blocks. (7) The bone should be anatomically repositioned, and the PCL should be anatomically repositioned to prevent ligament relaxation. (8) Screw into the need to grasp the strength, enough; if the bone is broken, the tooth gasket can be used to transform the crushed bone into a whole for processing and increase the fixed holding force.
There are numerous flaws in this study, including a short patient follow-up period and a lack of clinical data on the long-term prognosis of this treatment regimen. The research sample is small, and the evidence level of the present study is too low to provide specific clinical treatment guidance. The lack of a control group makes it difficult to explain the technique's benefits and drawbacks; this incision makes it difficult to complete the exploration and repair of other knee structures. Because the size of the fracture fragment was not taken into account during fixation, some smaller bone pieces were unable to be fixed with cannulated lag screws. Smaller fracture pieces can be repaired and reduced using anchors (40), sutures (41, 42), steel wires (11), and specific plates (12, 43).
In addition, the procedure can be difficult for obese or muscular patients because the technique requires the surgeon to open the gastrocnemius muscle to expose the fractured end. If exposure is difficult, the incision may need to be widened or the traditional procedure changed.
Conclusion
This study describes a technique that can be used to complete the internal fixation of tibial PCL avulsions. It uses a minimally invasive approach to the knee joint's posteromedial interval that does not involve separation of the popliteal nerve or blood vessels. In addition, the technique can be applied in source-constrained or smaller hospitals that are not equipped with arthroscopy technology.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee and the review board of the Second Affiliated Hospital of Anhui Medical University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HG is responsible for writing the thesis. HG and YZ are responsible for the main operation. WC and HF put forward surgical ideas. WC and XS are responsible for collecting and processing data. LG polish the paper. LC put forward a lot of suggestions for the later article modification, the deficiencies of the surgical methods and the places to be improved. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Hefei independent innovation policy “Borrow-transfersupplement” project (J2020Y07), Functional limb salvage of diabetic foot (2020byzd347), Masquelet technique combined with transverse bone transfer technique for the treatment of refractory Wagner III and IV diabetic foot (FY2021-027) and tibial periosteum lateral extension for Wagner III and IV diabetic foot in a multidisciplinary collaborative mode (2022xkj225). The funders had no role in the study design, data collection and analysis, in the decision to publish, or in the preparation of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.885669/full#supplementary-material.
References
1. Schuttler KF, Ziring E, Ruchholtz S, Efe T. Posterior cruciate ligament injuries. Unfallchirurg. (2017) 120:55–68. doi: 10.1007/s00113-016-0292-z
2. Fontbote CA, Sell TC, Laudner KG, Haemmerle M, Allen CR, Margheritini F, et al. Neuromuscular and biomechanical adaptations of patients with isolated deficiency of the posterior cruciate ligament. Am J Sport Med. (2005) 33:982–9. doi: 10.1177/0363546504271966
3. Barros MA, Cervone GL, Costa AL. Surgical treatment of avulsion fractures at the tibial insertion of the posterior cruciate ligament: functional result. Rev Bras Ortop. (2015) 50:631–7. doi: 10.1016/j.rboe.2015.09.005
4. Tao T, Yang W, Tao X, Li Y, Zhang K, Jiang Y, et al. Arthroscopic direct anterior-to-posterior suture suspension fixation for the treatment of posterior cruciate ligament tibial avulsion fracture. Orthop Surg. (2022) 14:2031–41. doi: 10.1111/os.13401
5. Hooper PR, Silko C, Malcolm TL, Farrow LD. Management of posterior cruciate ligament tibial avulsion injuries: a systematic review. Am J Sport Med. (2018) 46:734–42. doi: 10.1177/0363546517701911
6. Bali K, Prabhakar S, Saini U, Dhillon MS. Open reduction and internal fixation of isolated PCL fossa avulsion fractures. Knee Surg Sport Traumatol Arthrosc. (2012) 20:315–21. doi: 10.1007/s00167-011-1618-6
7. Jang KM, Lee SH. Delayed surgical treatment for tibial avulsion fracture of the posterior cruciate ligament in children. Knee Surg Sport Traumatol Arthrosc. (2016) 24:754–9. doi: 10.1007/s00167-015-3929-5
8. Guimaraes TM, Helito P, Angelini FJ, Demange MK, Pecora JR, Helito CP. Delayed treatment of a posterior cruciate ligament tibial insertion avulsion fracture in a child with open physis: a case report with a 4-year follow-up. J Pediatr Orthop B. (2017) 26:477–81. doi: 10.1097/BPB.0000000000000432
9. Keyhani S, Soleymanha M, Salari A. Treatment of posterior cruciate ligament tibial avulsion: a new modified open direct lateral posterior approach. J Knee Surg. (2022) 35:862–7. doi: 10.1055/s-0040-1721093
10. Khalifa AA, Elsherif ME, Elsherif E, Refai O. Posterior cruciate ligament tibial insertion avulsion, management by open reduction and internal fixation using plate and screws through a direct posterior approach. Injury. (2021) 52:594–601. doi: 10.1016/j.injury.2020.09.058
11. Li L, Tian W. Displaced avulsion fractures of the posterior cruciate ligament: treated by stellate steel plate fixation. Indian J Orthop. (2015) 49:171–5. doi: 10.4103/0019-5413.152454
12. Liu H, Liu J, Wu Y, Ma Y, Gu S, Mi J, et al. Outcomes of tibial avulsion fracture of the posterior cruciate ligament treated with a homemade hook plate. Injury. (2021) 52:1934–8. doi: 10.1016/j.injury.2021.04.042
13. Qi H, Lu Y, Li M, Ren C, Xu Y, Ma T, et al. Open reduction and internal fixation of the tibial avulsion fracture of the posterior cruciate ligament: which is better, a hollow lag screw combined with a gasket or a homemade hook plate? Bmc Musculoskel Dis. (2022) 23:143. doi: 10.1186/s12891-022-05096-0
14. Kan H, Nakagawa S, Hino M, Komaki S, Arai Y, Inoue H, et al. Arthroscopic fixation technique for avulsion fracture of the posterior cruciate ligament from the tibia. Arthrosc Tech. (2020) 9:e1819–24. doi: 10.1016/j.eats.2020.08.006
15. Tang J, Zhao J. Arthroscopic suture-to-loop fixation of posterior cruciate ligament tibial avulsion fracture. Arthrosc Tech. (2021) 10:e1595–602. doi: 10.1016/j.eats.2021.02.029
16. Yoon JR, Park CD, Lee DH. Arthroscopic suture bridge fixation technique with multiple crossover ties for posterior cruciate ligament tibial avulsion fracture. Knee Surg Sport Traumatol Arthrosc. (2018) 26:912–8. doi: 10.1007/s00167-016-4339-z
17. Katsman A, Strauss EJ, Campbell KA, Alaia MJ. Posterior cruciate ligament avulsion fractures. Curr Rev Musculoskelet Med. (2018) 11:503–9. doi: 10.1007/s12178-018-9491-2
18. Yoon KH, Kim SG, Park JY. The amount of displacement can determine non-operative treatment in posterior cruciate ligament avulsion fracture. Knee Surg Sport Traumatol Arthrosc. (2021) 29:1269–75. doi: 10.1007/s00167-020-06175-2
19. Fanelli GC. Knee dislocation and multiple ligament injuries of the knee. Sports Med Arthrosc. (2018) 26:150–2. doi: 10.1097/JSA.0000000000000220
20. Hesse E, Bastian L, Zeichen J, Pertschy S, Bosch U, Krettek C. Femoral avulsion fracture of the posterior cruciate ligament in association with a rupture of the popliteal artery in a 9-year-old boy: a case report. Knee Surg Sport Traumatol Arthrosc. (2006) 14:335–9. doi: 10.1007/s00167-005-0677-y
21. Sonin AH, Fitzgerald SW, Friedman H, Hoff FL, Hendrix RW, Rogers LF. Posterior cruciate ligament injury: MR imaging diagnosis and patterns of injury. Radiology. (1994) 190:455–8. doi: 10.1148/radiology.190.2.8284399
22. Zhao J, He Y, Wang J. Arthroscopic treatment of acute tibial avulsion fracture of the posterior cruciate ligament with suture fixation technique through Y-shaped bone tunnels. Arthroscopy. (2006) 22:172–81. doi: 10.1016/j.arthro.2005.10.020
23. Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Posterior cruciate ligament: current concepts review. Arch Bone Jt Surg. (2018) 6:8–18. doi: 10.1177/3259671221114820
24. Huang W, Gong X, Rahul M, Priyanka S, Wang C, Liang X, et al. Anterior arthroscopic-assisted fixation of posterior cruciate ligament avulsion fractures. Eur J Med Res. (2015) 20:88. doi: 10.1186/s40001-015-0177-6
25. Montgomery SR, Johnson JS, McAllister DR, Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. (2013) 6:115–23. doi: 10.1007/s12178-013-9162-2
26. Song JG, Nha KW, Lee SW. Open posterior approach versus arthroscopic suture fixation for displaced posterior cruciate ligament avulsion fractures: systematic review. Knee Surg Relat Res. (2018) 30:275–83. doi: 10.5792/ksrr.17.073
27. Sundararajan SR, Joseph JB, Ramakanth R, Jha AK, Rajasekaran S. Arthroscopic reduction and internal fixation (ARIF) versus open reduction internal fixation (ORIF) to elucidate the difference for tibial side PCL avulsion fixation: a randomized controlled trial (RCT). Knee Surg Sport Traumatol Arthrosc. (2021) 29:1251–7. doi: 10.1007/s00167-020-06144-9
28. Kim SJ, Shin SJ, Choi NH, Cho SK. Arthroscopically assisted treatment of avulsion fractures of the posterior cruciate ligament from the tibia. J Bone Joint Surg Am. (2001) 83:698–708. doi: 10.2106/00004623-200105000-00008
29. Wu L, Xu H, Li B, Xu B. Improved arthroscopic high-strength suture fixation for the treatment of posterior cruciate ligament avulsion fracture. J Orthop Surg. (2022) 30:10225536221101701. doi: 10.1177/10225536221101701
30. Zhao D, Zhong J, Zhao B, Li Y, Shen D, Gui S, et al. Clinical outcomes of acute displaced posterior cruciate ligament tibial avulsion fracture: a retrospective comparative study between the arthroscopic suture and EndoButton fixation techniques. Orthop Traumatol Surg Res. (2021) 107:102798. doi: 10.1016/j.otsr.2020.102798
31. Rhee SJ, Jang JH, Choi YY, Suh JT. Arthroscopic reduction of posterior cruciate ligament tibial avulsion fracture using two cross-linked pull-out sutures: a surgical technique and case series. Injury. (2019) 50:804–10. doi: 10.1016/j.injury.2018.11.022
32. Abdallah AA, Arafa MS. Treatment of posterior cruciate ligament tibial avulsion by a minimally-invasive open posterior approach. Injury. (2017) 48:1644–9. doi: 10.1016/j.injury.2017.05.032
33. Reverte-Vinaixa MM, Nunez JH, Muneton D, Joshi N, Castellet E, Minguell J. Outcomes of posterior cruciate ligament tibial avulsion treated with staple fixation: stress TELOS x-ray evaluation. Eur J Orthop Surg Traumatol. (2019) 29:883–91. doi: 10.1007/s00590-019-02371-0
34. Burks RT, Schaffer JJ. A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res. (1990):216–9. doi: 10.1097/00003086-199005000-00031
35. Nicandri GT, Klineberg EO, Wahl CJ, Mills WJ. Treatment of posterior cruciate ligament tibial avulsion fractures through a modified open posterior approach: operative technique and 12- to 48-month outcomes. J Orthop Trauma. (2008) 22:317–24. doi: 10.1097/BOT.0b013e31817279d1
36. Bi M, Zhao C, Chen J, Hong Z, Wang Z, Gan K, et al. Arthroscopic suture fixation with autograft augmentation reconstruction for delayed tibial avulsion fractures of the posterior cruciate ligament. Orthop J Sports Med. (2020) 8:2325967120944047. doi: 10.1177/2325967120944047
37. Gavaskar AS, Karthik B, Gopalan H, Srinivasan P, Tummala NC. A novel MIS technique for posterior cruciate ligament avulsion fractures. Knee. (2017) 24:890–6. doi: 10.1016/j.knee.2017.03.014
38. Chen LB, Wang H, Tie K, Mohammed A, Qi YJ. Arthroscopic fixation of an avulsion fracture of the tibia involving the posterior cruciate ligament: a modified technique in a series of 22 cases. Bone Joint J. (2015) 97-B:1220–5. doi: 10.1302/0301-620X.97B9.35765
39. Hermanowicz K, Goralczyk A, Danowska K, Galazka D, LaPrade RF, Malinowski K. All-Arthroscopic posterior cruciate ligament distal reattachment with extracortical fixation. Arthrosc Tech. (2019) 8:e1425–30. doi: 10.1016/j.eats.2019.07.019
40. Forkel P, Imhoff AB, Achtnich A, Willinger L. All-arthroscopic fixation of tibial posterior cruciate ligament avulsion fractures with a suture-button technique. Oper Orthop Traumatol. (2020) 32:236–47. doi: 10.1007/s00064-019-00626-x
41. Willinger L, Imhoff AB, Schmitt A, Forkel P. Fixation of bony avulsions of the posterior cruciate ligament by a suture-bridge technique. Oper Orthop Traumatol. (2019) 31:3–11. doi: 10.1007/s00064-018-0582-4
42. Zhu W, Lu W, Cui J, Peng L, Ou Y, Li H, et al. Treatment of tibia avulsion fracture of posterior cruciate ligament with high-strength suture fixation under arthroscopy. Eur J Trauma Emerg Surg. (2017) 43:137–43. doi: 10.1007/s00068-015-0606-9
Keywords: minimally invasive, posterior cruciate ligament, avulsion fracture, clinical effects, technique
Citation: Guo H, Zhao Y, Gao L, Wang C, Shang X, Fan H, Cheng W and Liu C (2023) Treatment of avulsion fracture of posterior cruciate ligament tibial insertion by minimally invasive approach in posterior medial knee. Front. Surg. 9:885669. doi: 10.3389/fsurg.2022.885669
Received: 28 February 2022; Accepted: 2 November 2022;
Published: 6 January 2023.
Edited by:
Paphon Sa-ngasoongsong, Mahidol University, ThailandReviewed by:
Lin Zheng, Zhejiang University, ChinaFreeman Miller, Alfred I. duPont Hospital for Children, United States
© 2023 Guo, Zhao, Gao, Wang, Shang, Fan, Cheng and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wendan Cheng c3VueWNjY0AxMjYuY29t Chang Liu MzIyMTMyNDFAcXEuY29t
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Huihui Guo
Huihui Guo Yao Zhao
Yao Zhao Liang Gao
Liang Gao Chen Wang
Chen Wang Xianbo Shang
Xianbo Shang Haitao Fan4
Haitao Fan4 Wendan Cheng
Wendan Cheng