
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Surg. , 13 April 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.866191
This article is part of the Research Topic Advances in Proctology and Colorectal Surgery View all 45 articles
 Diego Coletta1,2*
Diego Coletta1,2* Cristina De Padua3
Cristina De Padua3 Immacolata Iannone3
Immacolata Iannone3 Antonella Puzzovio3
Antonella Puzzovio3 Paola Antonella Greco2
Paola Antonella Greco2 Alberto Patriti2
Alberto Patriti2 Filippo La Torre1,3
Filippo La Torre1,3Defunctioning ileostomy (DI) is a surgical procedure adopted for fecal diversion in colorectal surgery to prevent the most important complication, i.e., anastomotic leakage (AL). It could be defined as a defect in the intestinal wall integrity at the suture site leading to a communication between the inside and outside compartments such as pelvic abscess close to the anastomosis and recto-vaginal fistula (1). Most surgeons suggest the use of fecal diversion in patients undergoing low anterior resections of rectal tumors followed by ultra-low colorectal or coloanal anastomoses at high risk for anastomotic failure. Although a stoma does not always prevent AL, it may reduce the incidence of sepsis in the event of leakage and decreases the rate of emergency reoperation (2–4). Fecal diversions have been associated with poor quality of life, stoma-related complications from 3 to 33%, and perioperative risk of stoma closure later on or a reversal of stoma not happening because of patients at high risk of complications (5). In the past decade, most techniques have been described as variants of the conventional loop ileostomy or as novel technical notes, changing the site of stoma or using tubes to perform it. With the advent of minimally invasive surgery, new techniques have been developed in an attempt to maintain the concept of less invasiveness for the patients. The aim of our paper is to give a snapshot of the current literature on the available types of DI to prevent AL in colorectal surgery, searching by three different electronic databases, namely Pubmed/Medline, Web of Science (WOS), and EMBASE, using a combination of the following MESH terms: “loop ileostomy,” “cannula ileostomy,” “tube ileostomy,” “defunctioning ileostomy,” “diverting loop ileostomy,” “colorectal surgery,” “anastomotic leak,” and “fecal diversion.” The references of the retrieved articles were screened to find further studies. We chose to not describe “Ghost ileostomy” and “Hidden ileostomy,” because these are not ostomies but considered as alternative procedures to DI, so cannot be included in the group of fecal diversionsa.
The more popular technique used to perform a conventional loop ileostomy is that described for the first time by Turnbull and Weakley (6) around the late 1960s. The intestinal loop is pulled out through an abdominal transparietal circular opening at the level of the right iliac fossa and fixed with four interrupted sutures between the parietal fascia, peritoneum, and seromuscular layer of the bowel, in order to avoid postoperative prolapse. A rod is used to pull out and keep the loop in place to avoid retraction and to exclude the efferent loop from the transit of the bowel content. After the opening of the stoma, interrupted mucocutaneous stitches with absorbable materials are used to complete stoma fixation to the skin. The ileostomy takedown is made with a peristomal skin incision, complete mobilization of the bowel loop, intestinal anastomosis, and abdominal wall reconstruction. In the past decades, many variants of classic techniques have been reported. The changes have consisted of eliminating the use of the rod, trying new material for the rod, suturing the efferent loop, and changing the site of ostomy (7–10) (Figure 1A).
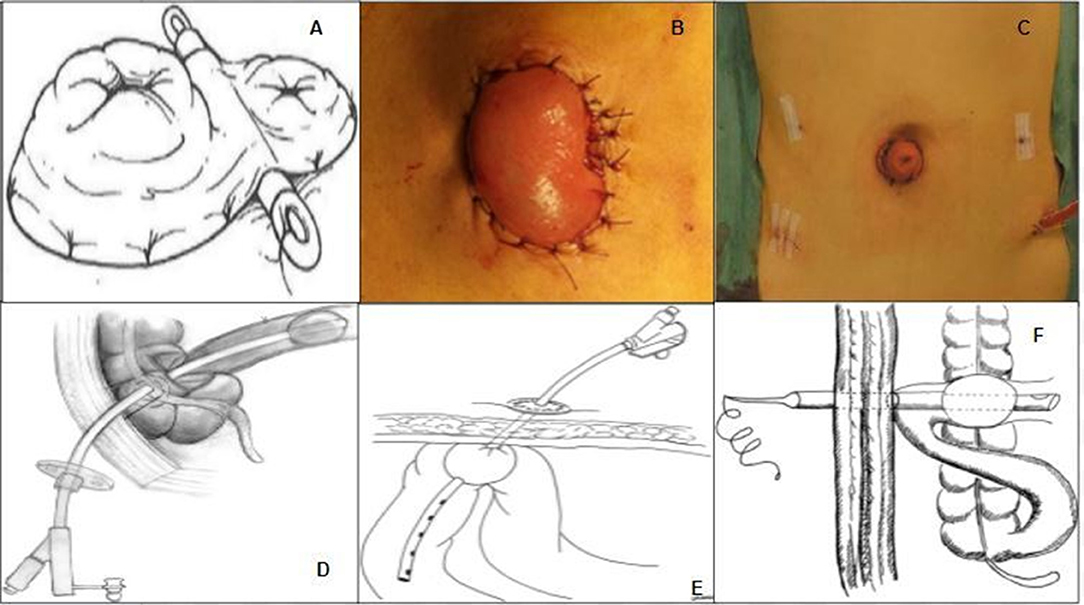
Figure 1. (A) Classic Turnbull loop ileostomy, from Whitehead and Cataldo (11). (B) Skin bridge loop ileostomy, from Ye et al. (12). (C) Umbilical ileostomy, from Eto et al. (13). (D) Transcaecal ileostomy, from Monzòn-Abad et al. (14). (E) Percutaneous ileostomy, from Rondelli et al. (15). (F) Cannula ileostomy from Hua et al. (16).
This is the most recent variant of the classic loop ileostomy technique, consisting of using a skin flap as a rod (17). The skin is incised, creating a rectangular skin bridge about 3 cm long and 1 cm wide, and the subcutaneous fat is divided. This flap is passed through an avascular window opened in the mesentery at the apex of the chosen ileal loop and then secured with separate stitches of 2/0 absorbable suture to the distal edge of the opening, determining the exclusion of the efferent loop of the stoma. The afferent and the efferent loops are fixed to the skin with a 3/0 absorbable suture to prevent retraction and dislocation. Some recent papers (12, 18) demonstrate that the skin bridge loop ileostomy may significantly reduce the early postoperative stoma-related complications, the frequency of exchanged ostomy bags, and patient medical costs after hospital discharge if compared with a conventional loop ileostomy. The ostomy closure follows the same techniques of conventional loop ileostomy (Figure 1B).
Used for the first time in pediatric patients with Hirschsprung's disease or imperforate anus (10), this technique has increased in use together with the rise of laparoscopic surgery in order to maintain the concept of minimal invasiveness of the surgical procedures. The loop of the ileum designated for the ileostomy was brought out without tension through the umbilical port site with a vertical skin incision just below the umbilicus. It is important to widen the fascial incision to allow for a 5 cm gap as for the conventional ileostomy, and the intestinal serosa and fascia were fixed. Three points of the serosal muscular layer were sutured on the caudal side and on both lateral sides to prevent retraction. The intestinal tract was opened, and the umbilicus is fixed to the incision end of the stoma to assist in the elevation of the intestinal tract. Ostomy reversal is performed through a full mobilization of the stoma including the umbilicus, followed by the anastomosis. Finally, the skin is fixed to the muscle layer subcutaneously with two needles to form a new umbilicus (19–25) (Figure 1C).
Simpson and Srivastava (26) described this technique of ileal diversion in 1975 to allow a complete colonic lavage and ileal decompression in elective colonic surgery. A Foley catheter (26, 27) or a gastrostomy tube (14) is inserted through the cecum in the ileocecal valve and then the balloon is inflated. The catheter and the cecum are fastened with a single or double purse-string suture to the parietal peritoneum and abdominal wall. Ostomy closure is performed by a gradual deflation of the balloon started at postoperative day 5 (27) or at postoperative day 7 (14), and when is complete, the catheter is removed (Figure 1D).
After the performance of colorectal anastomosis, a modified 18 or 20 Fr jejunostomy tube is placed into the distal ileum about 40 cm proximal to the ileocecal valve by ensuring that the distal part of the tube was in the afferent loop to optimize the drainage (15). The jejunostomy balloon was inflated with 7–10 ml of normal saline then the catheter is fixed in the ileal loop with a purse-string and was brought out through the abdominal wall in the right inferior quadrant also by using a port incision in laparoscopic and robotic surgery. Between the 8th and the 11th postoperative days, a CT scan with a trans-anal enema of hydrosoluble iodate contrast is performed to assess the integrity of the anastomosis, and the catheter can be removed by deflating progressively the balloon. Finally, the abdominal orifice is kept open and connected to a urostomy bag (Figure 1E).
The endotracheal tube can be used to perform fecal diversion after the colorectal anastomosis; some authors named this technique “cannula” ileostomy (16) and some others “tube” ileostomy (28, 29). A double row of concentric purse-string sutures is placed onto the ileum wall with absorbable sutures and the tracheal cannula is inserted into the distal ileum through a small incision within the inner purse-string, after which the inner and then the external purse-string sutures are tied. Thereafter, normal saline is injected into the balloon and the tube is pulled out through the abdominal wall. The loop is secured to the same location at the parietal peritoneum, near the tube end with seromuscular stitches. The cannula is then pulled tight, and sutures at the fixation site are tightly knotted. The procedure ends with or without a reversible single row of staples across the whole width of the terminal ileum about 10 cm distal to the site of tube insertion. The tube is removed 2 days after the anal function of the patient resumes, during which the tube is blocked with the deflated balloon to ensure that the passage of bowel content continues after its removal between the 20th and the 75th postoperative days.
Chowdri et al. (30) described the same procedure but using a 26 Fr three-way self-retaining Foley catheter, and they also named it “tube ileostomy.” In the postoperative period, the management of ostomy requires a regular check of the free flow of contents by washing the tube with normal saline. The tube is deflated between the 5th and 7th postoperative days, clamped after the second week, and finally removed after the third week of surgery to obtain a controlled fistula (Figure 1F).
Table 1 shows the characteristics of the main included studies.
Defunctioning ileostomy is a surgical procedure adopted for the fecal diversion in colorectal surgery to prevent AL. The perfect technique to perform an ileostomy does not exist and any one of the available procedures could be best suited for the patient. All the techniques described could be adopted in open or minimally invasive surgery by using the laparoscopic port incisions adapted as needed, except for the umbilical ileostomy that can be performed only in laparoscopic surgery for obvious intrinsic technical reasons. We aimed to give a snapshot of the current literature on the available types of DI in colorectal surgery. The most important characteristic of a fecal diversion is to be really “defunctioning” as much as possible, without stoma-related complications and with only some or no discomfort for the patients. Moreover, a temporary ileostomy should be easy to take down spontaneously if possible, as described for some techniques (15, 16). In our study, we described the different available techniques that could not have been compared, but some have been compared to the conventional Turnbull loop ileostomy (8, 12, 18) in terms of stoma-related complications and ostomy management. Carannante et al. (18) compared the conventional technique with a plastic rod to the skin bridge one, showing an improvement of stomal infection, dermatitis, and ulcers in the second group. Besides, the average number of exchanged stoma wafers per week resulted in more than half with statistical significance. No studies investigated eventual differences in the ostomy take-down outcomes that seem to be the same for both techniques. Eto et al. (23, 31) compared the conventional ileostomy and umbilical ileostomy after the laparoscopic anterior resection for rectal cancer. The studies demonstrated a lower wound infection rate in the group of conventional loop ileostomy with better surgical outcomes, but a significantly lower incidence of incisional hernia and relative risk for its development in the umbilical ileostomy group. The temporary percutaneous ileostomy seems to be a valid alternative to the classic loop ileostomy after low anterior resection and extraperitoneal anastomosis, offering a more comfortable and complete fecal diversion with fewer stoma-related and surgical complications if compared with a conventional DI (32). The real novelty is that this ostomy does not require surgery for its closure. The comparison between tube/cannula ileostomy and conventional loop ileostomy has shown no statistical difference in terms of anastomotic dehiscence, stomal complications, and pain. The main differences are the longer hospital stay for the traditional loop ileostomy group and the need for a second surgery for its closure (28, 33). In daily practice, no one technique leads to superior performance than another, and no evidence supports to advise the use of one routinely; the confidence and the expertise of the surgeons in performing a DI and the characteristics of patients play a key role in the choice of the technique to adopt. Further prospective studies with multiple arms of investigation are needed to compare the different techniques of DI to prevent AL in colorectal surgery.
The perfect technique to perform a DI does not exist; different techniques can be performed and every patient should receive the proper tailored one. The surgeon should know every one of these available choices and use them as the arrows in the quiver of an archer when needed.
DC and FLT have designed the study. DC, II, and CD have performed the literature search and extracted data. DC has written the manuscript and is responsible for the financial support. FLT, APu, APa, and PAG have critically revised the manuscript. All authors contributed to the article and approved the submitted version.
DC received financial aid for the drawing up of the present article from the Ph.D. Course in Advanced Surgical Technologies of the Sapienza University of Rome.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rahbari NN, Weitz J, Hohenberger W, et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery. (2010) 147:339–51. doi: 10.1016/j.surg.2009.10.012
2. Hüser N, Michalski CW, Erkan M, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg. (2008) 248:52–60. doi: 10.1097/SLA.0b013e318176bf65
3. Smith JD, Paty PB, Guillem JG, Temple LK, Weiser MR, Nash GM. Anastomotic leak is not associated with oncologic outcome in patients undergoing low anterior resection for rectal cancer. Ann Surg. (2012) 256:1034–8. doi: 10.1097/SLA.0b013e318257d2c1
4. Lin JK, Yueh TC, Chang SC, Lin CC, Lan YT, Wang HS, et al. The influence of fecal diversion and anastomotic leakage on survival after resection of rectal cancer. J Gastrointest Surg. (2011) 15:2251–61. doi: 10.1007/s11605-011-1721-5
5. Anaraki F, Vafaie M, Behboo R, Maghsoodi N, Esmaeilpour S, Safaee A. Quality of life outcomes in patients living with stoma. Indian J Palliat Care. (2012) 18:176–80. doi: 10.4103/0973-1075.105687
6. Turnbull RB Jr, Weakley FL. Ileostomy technics and indications for surgery. Rev Surg. (1966) 23:310–4
7. Flati G, Talarico C, Carboni M. An improved technique for temporary diverting ileostomy. Surg Today. (2000) 30:104-5. doi: 10.1007/PL00010038
8. Dziki Ł, Mik M, Trzciński R, Buczyński J, Darnikowska J, Spychalski M, et al. Evaluation of the early results of a loop stoma with a plastic rod in comparison to a loop stoma made with a skin bridge. Polski Przeglad chirurgiczny. (2014) 87:31–4. doi: 10.1515/pjs-2015-0014
9. Milner CS, Sutton C, Hemingway D. The skin bridge loop colostomy. Tech Coloproctol. (2006) 10:137 doi: 10.1007/s10151-006-0267-0
10. Fitzgerald PG, Lau G Y, Cameron GS. Use of the umbilical site for temporary ostomy: review of 47 cases. J Pediatr Surg. (1989) 24:973. doi: 10.1016/S0022-3468(89)80194-0
11. Whitehead A, Cataldo PA. Technical Considerations in Stoma Creation Clin. Colon Rectal Surg. (2017) 30:162–71. doi: 10.1055/s-0037-1598156
12. Ye H, Huang S, Yu J, Zhou Q, Xi C, Cao L et al. Comparison of the clinical outcomes of skin bridge loop ileostomy and traditional loop ileostomy in patients with low rectal cancer. Sci Rep. (2021) 11:9101. doi: 10.1038/s41598-021-88674-x
13. Eto K, Omura N, Haruki K, Uno Y, Ohkuma M, Nakajima S, et al. Transumbilical defunctioning ileostomy: A new approach for patients at risks of anastomotic leakage after laparoscopic low anterior resection. Anticancer Res. (2013) 33:5011–5.
14. Monzón-Abad A, Gracia-Roche C, Martínez-Germán A, Barranco-Domínguez I, Sánchez-Fuentes N. A preliminary study of transcaecal ileostomy as an alternative to defunctioning ostomies. Colorectal Dis. (2014) 16:130–3. doi: 10.1111/codi.12489
15. Rondelli F, Mariani L, Boni M, Federici MT, Cappotto FP, Mariani E. Preliminary report of a new technique for temporary faecal diversion after extraperitoneal colorectal anastomosis. Colorectal Dis. (2010) 12:1159–61. doi: 10.1111/j.1463-1318.2010.02294.x
16. Hua H, Xu J, Chen W, Zhou X, Wang J, Sheng Q, Lin J. Defunctioning cannula ileostomy after lower anterior resection of rectal cancer. Dis Colon Rectum. (2014) 57:1267–74. doi: 10.1097/DCR.0000000000000217
17. Pace U, Rega D, Scala D, Montesarchio L, Delrio P Skin bridge loop ileostomy: technical details. Tech Coloproctol. (2014) 18:855–6. doi: 10.1007/s10151-014-1142-z
18. Carannante F, Mascianà G, Lauricella S, Caricato M, Capolupo GT. Skin bridge loop stoma: outcome in 45 patients in comparison with stoma made on a plastic rod. Int J Colorectal Dis. (2019) 34:2195–7. doi: 10.1007/s00384-019-03415-x
19. Hada M, Hayashi K, Sawada K, Oshima M, Kato Y, Oyama K, et al. Anticipation of umbistoma in laparoscopic anterior rectal resection: Ileostomy and ostomy closure. J Anus Rectum Colon. (2018) 2:77–82. doi: 10.23922/jarc.2017-037
20. Ishiguro S, Komatsu S, Ando K, Osawa T, Yasui K, Arikawa T, et al. Feasibility of umbilical loop ileostomy in overweight and obese patients with rectal cancer during laparoscopic surgery: Preliminary results. Asian J Endosc Surg. (2017) 10:79–82. doi: 10.1111/ases.12316
21. Mushaya CD, Chandra R, Sansom W, Keck J. Temporary diverting ileostomy via the umbilicus: a small case series. Int Surg. (2015) 100:436–43. doi: 10.9738/INTSURG-D-14-00168.1
22. d'Alessandro A, Kari N, Alameh A, Pasquier N, Tarhini A, Vinson Bonnet B, et al. Preliminary experience with umbilical stoma in transumbilical single-port colorectal surgery. Tech Coloproctol. (2018) 22:301–4. doi: 10.1007/s10151-018-1767-4
23. Eto K, Kosuge M, Ohkuma M, Haruki K, Neki K, Mitsumori N, et al. Comparison of transumbilical and conventional defunctioning ileostomy in laparoscopic anterior resections for rectal cancer. Anticancer Res. (2016) 36:4139–44
24. Miyo M, Takemasa I, Hata T, Mizushima T, Doki Y, Mori M, et al. Safety and Feasibility of Umbilical Diverting Loop Ileostomy for Patients with Rectal Tumor. World J Surg. (2017) 41:3205–11. doi: 10.1007/s00268-017-4128-y
25. Seow-En I, Daud MABM, Seow-Choen F. The umbilicus as a site for defunctioning ileostomies. Tech Coloproctol. (2011) 15:213–4. doi: 10.1007/s10151-010-0659-z
26. Simpson A, Srivastava VK. Temporary transcaecal ileal diversion in prevention of anastomotic leak in planned colonic surgery (an alternative to proximal colostomy). Br J Surg. (1975) 62:243–5. doi: 10.1002/bjs.1800620319
27. Winslet MC, Cooke P, Obeid ML. Transcaecal ileal diversion in the management of the ‘at risk' distal colonic anastomosis. Int J Colorect Dis. (1993) 8:57–9. doi: 10.1007/BF00299326
28. Zhou X, Lin C, Chen W, Lin J, Xu J. Completely diverted tube ileostomy compared with loop ileostomy for protection of low colorectal anastomosis: a pilot study. Colorectal Dis. (2014) 16:O327–31. doi: 10.1111/codi.12604
29. Sheng QS, Hua HJ, Cheng XB, Wang WB, Chen WB, Xu JH, et al. A modified spontaneously closed defunctioning tube ileostomy after anterior resection of the rectum for rectal cancer with a low colorectal anastomosis. Indian J Surg. (2016) 78:125–9. doi: 10.1007/s12262-015-1332-6
30. Chowdri NA, Wani MA, Parray FQ, Mir SH, Wani RA. Tube ileostomy as an alternative to conventional ileostomy for fecal diversion. World J Colorectal Surg. (2010) 2:Article 11.
31. Eto K, Kosuge M, Ohkuma M, Ito D, Takeda Y, Yatabe S, et al. Umbilical defunctioning ileostomy for rectal cancer results in reduced risk for incisional hernia. Anticancer Res. (2020) 40:3445–51. doi: 10.21873/anticanres.14330
32. Rondelli F, Balzarotti R, Bugiantella W, Mariani L, Pugliese R, Mariani E. Temporary percutaneous ileostomy versus conventional loop ileostomy in mechanical extraperitoneal colorectal anastomosis: a retrospective study. Eur J Surg Oncol. (2010) 38:1065–70. doi: 10.1016/j.ejso.2012.07.110
Keywords: defunctioning ileostomy, tube ileostomy, cannula ileostomy, loop ileostomy, colorectal surgery, anastomotic leak, fecal diversion
Citation: Coletta D, De Padua C, Iannone I, Puzzovio A, Greco PA, Patriti A and La Torre F (2022) Defunctioning Ileostomy to Prevent the Anastomotic Leakage in Colorectal Surgery. The State of the Art of the Different Available Types. Front. Surg. 9:866191. doi: 10.3389/fsurg.2022.866191
Received: 30 January 2022; Accepted: 08 March 2022;
Published: 13 April 2022.
Edited by:
Gaetano Gallo, University of Catanzaro, ItalyReviewed by:
Giuseppe Currò, University of Catanzaro, ItalyCopyright © 2022 Coletta, De Padua, Iannone, Puzzovio, Greco, Patriti and La Torre. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diego Coletta, ZGllZ29jb2xldHRhMUBnbWFpbC5jb20=; orcid.org/0000-0002-9116-0733
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.