- 1Department of Orthopaedic Surgery, University of Minnesota School of Medicine, Minneapolis, MN, United States
- 2Center for Movement and Gait Analysis, Children’s Hospital Colorado, Anschutz Medical Campus, Aurora, CO, United States
- 3Department of Orthopaedic Surgery, University of Colorado School of Medicine, Aurora, CO, United States
- 4Department of Pediatrics, Children’s Hospital Colorado, Anschutz Medical Campus, Aurora, CO, United States
- 5Department of Orthopaedics and Rehabilitation, Yale University School of Medicine, New Haven, CT, United States
Purpose: This study aims to compare radiographic outcomes and complication rates of immobilization with an abduction pillow to spica casting for postoperative care after a hip reconstruction with varus derotational proximal femur osteotomy (VDRO) with or without pelvic osteotomy for children with cerebral palsy (CP).
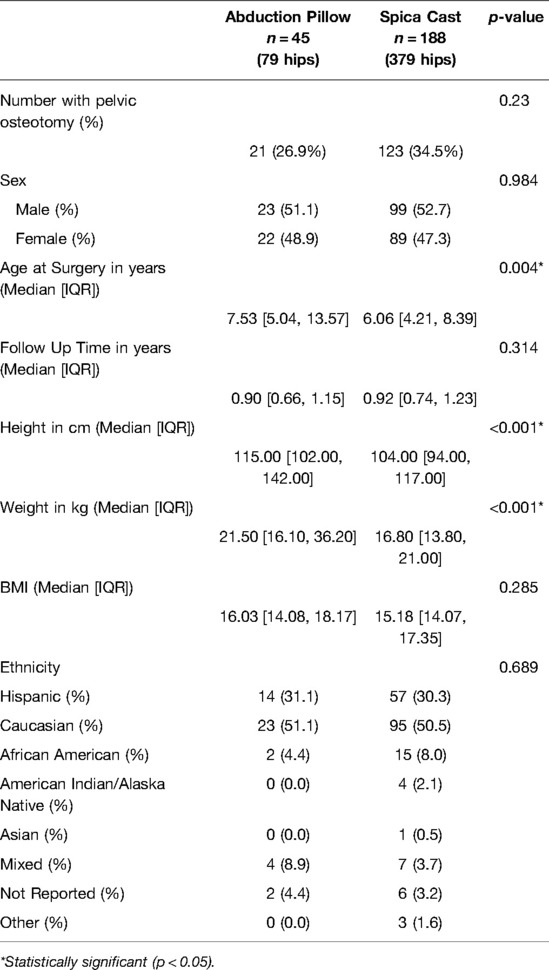
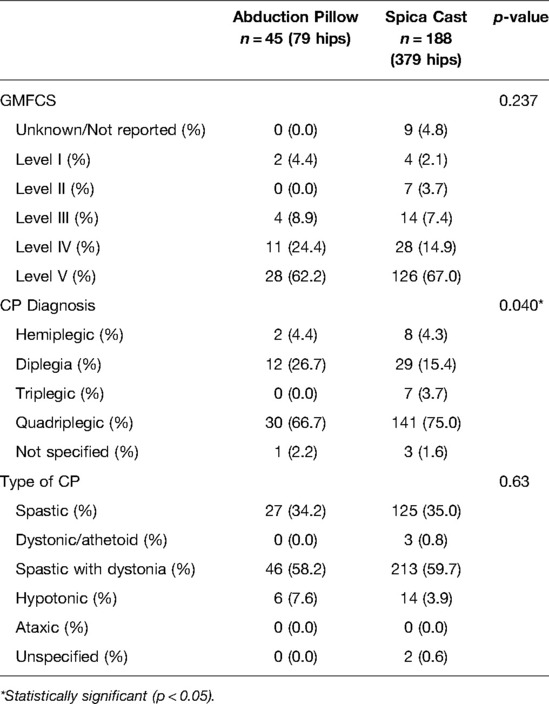
Methods: 233 children (1–18 years old) diagnosed with CP that underwent VDRO with or without pelvic osteotomy were identified, of which 188 patients were immobilized with a spica cast and 45 were immobilized with an abduction pillow, based on surgeon preference. 123 (65%) in the Spica group and 21 (47%) in the pillow group had pelvic osteotomies. Demographic data and complication rates were collected. Radiographic parameters, including anatomic medial proximal femoral angle (aMPFA), acetabular index (AI) and migration percentage (MP), were measured for each patient at the completion of surgery, six weeks post-operatively, and one year post-operatively.
Results: There was not a statistically significant difference in BMI (p = 0.285), gender distribution (p = 0.984), or median follow-up time (p = 0.314) between groups. Rates of complications were consistent among groups with no differences in instances of delayed unions (p = 0.10), subluxations (p = 0.55), infection (p = 0.71), or non-unions (p = 0.10). There was no statistically significant difference in number of patients with an ideal aMPFA, AI, or MP (p = 0.44, p = 0.19, p = 1.00) at one year post-operatively.
Conclusions: Immobilization with an abduction pillow is a safe and effective alternative to hip spica casting following hip reconstruction.
Introduction
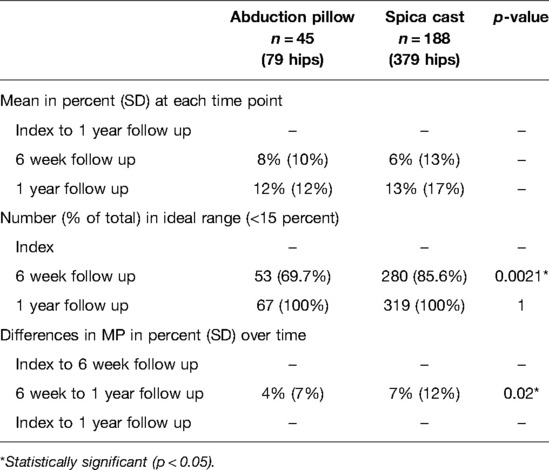
Cerebral palsy (CP) is a heterogeneous neurodevelopmental disorder which frequently results in neuromuscular hip dysplasia (also referred to as neurogenic dislocation of the hip) (1, 2). Commonly observed pathologies include coxa valga, increased femoral anteversion, and posterosuperior acetabular deficiency, which can lead to hip dislocation (3). Numerous guidelines and algorithms for periodic surveillance of the hips in CP patients exist, typically relying on clinical examination and an anteroposterior pelvic radiograph to track progression of these findings. Radiographically, the anatomical medial proximal femoral angle (aMPFA) (Figures 1C, F) can be used to measure the relative coronal plane alignment of the proximal femur (4, 5). The Reimers index/migration percentage (MP) (Figures 1A, D) and acetabular index (AI) (Figures 1B, E) can be measured to evaluate the location of the femoral head within the socket, and degree of acetabular dysplasia respectively (6, 7).
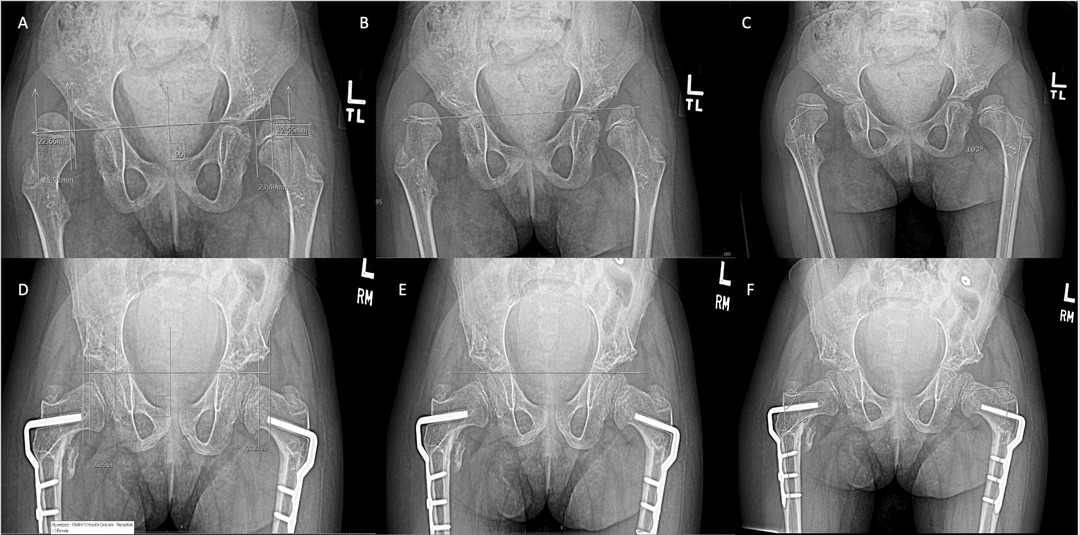
Figure 1. Measurements of a single patient pre- and post-operative of a VDRO for a single patient. (A–C) are pre-operative MP, AI, aMPFA respectively, while (D–F) are post-operative MP, AI, aMPFA respectively.
The risk of hip migration is directly correlated with increasing level Gross Motor Function Classification System (8), thus necessitating the need for more frequent surveillance with increasing severity of involvement (9).
Reconstructive hip surgery has been shown to be an effective means of treating symptomatic or unacceptably aligned hips (10, 11). This typically consists of a varus derotation osteotomy of the proximal femur (VDRO) to correct coxa valga and excess anteversion, and/or pelvic osteotomy for correction of acetabular dysplasia (12). While in the absence of pelvic osteotomies one may not expect there be improvement in AI, there is evidence that a VDRO alone may instigate bony remodeling of the acetabulum (3, 12, 13).
Absolute indications for VDRO include an MP greater than 50% or new hip dislocations with a break in Shenton’s line. Relative indications include a rapid increase in MP, MP greater than 40% with hip pain, difficulty with perineal hygiene, gait dysfunction and seating intolerance (10, 14, 15). An absolute indication for addition of a pelvic osteotomy is an acetabular index (AI) greater than 30 degrees with associated instability (16), with relative indications for an AI greater than 30 degrees, a level 5 GMFCS, or if the patient is older than 6 years of age (10, 12, 17, 18).
Historically, post-operative immobilization has most commonly included hip spica casting (Figure 2A) (11, 15, 19). Theoretical advantages of casting include stability of the bony reconstruction prior to bony union, maintenance of articular alignment, and protection of incisions, and as such some surgeons utilize them in patients with poor bone quality or if there is concern for the fixation achieved intraoperatively (17, 19–21). There are known postoperative complications when using hip spica casts, including skin sores, hygiene difficulties, need for specialized car seats, wheelchair challenges, prolonged anesthesia time, and psychosocial impacts on both the patient and their family (22). Casting may be unnecessary due to the stability of contemporary internal fixation hardware used for proximal femur osteotomies, as well as the stability of commonly used pelvic osteotomy techniques (23).
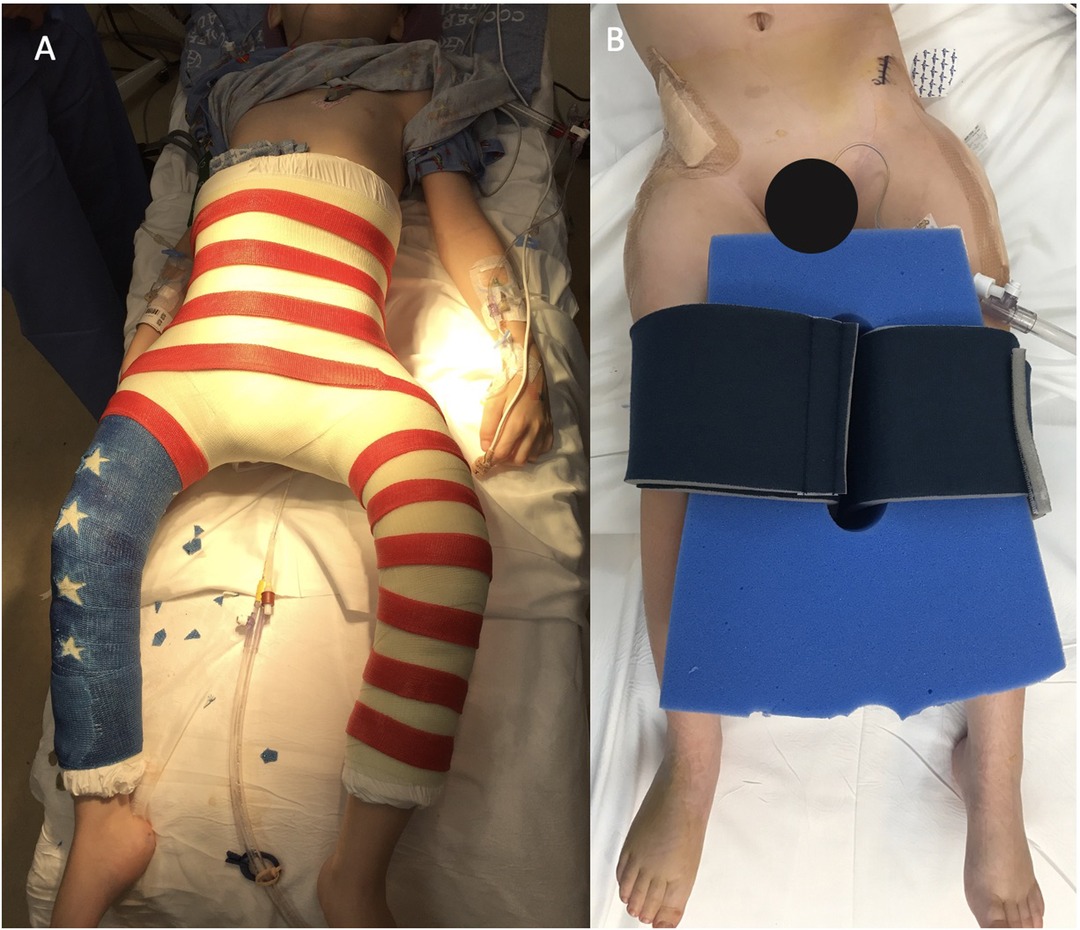
Figure 2. Immobilization after a Varus Derotational Osteotomy. (A) shows an example of a spica cast. (B) shows an example of an abduction wedge pillow.
Postoperative care strategies are highly variable between surgeons and institutions, with large differences in immobilization strategies, and this lack of consensus is in part due to the lack of substantial evidence directly comparing different methods of immobilization. Described alternatives have included long leg splints with abduction wedge, abduction wedge alone, Petrie cast, long leg splints alone, night splint foam, short leg casts with derotation bar and knee immobilizers, hip abduction orthosis, or no immobilization at all (19). The most common method outside spica casting at our institution is an abduction pillow, a commonly utilized method according to a recent survey by Miller et al. (19) (Figure 2B). Length of immobilization was 6 weeks in spica cast, and 6 weeks in abduction pillow.
This study characterizes the radiographic outcomes and postoperative complication profile between two methods of post-operative immobilization utilized at our institution after hip reconstruction for patients with CP. We theorize that radiographic outcomes and rates of postoperative complication in patients treated with abduction pillows are not significantly different than hip spica casts. Abduction pillows may obviate the challenges that hip spica casts pose to care teams, patients and their parents in the post-operative period.
Materials and Methods
Subjects
After approval from our institution’s ethical review board, a retrospective cohort study was created, in which patient consent was not required. We examined a consecutive cohort of children 1–18 years of age with CP that underwent unilateral or bilateral VDRO with or without pelvic osteotomy (San Diego osteotomy) at a single institution between 1999 and 2017. Patients undergoing single event multi-level surgery (SEMLS) were not included. Only patients that had clearly documented immobilization with a hip spica cast or abduction pillow post-operatively were included. Patients were excluded if they did not have one year of follow-up, or if they had a concomitant diagnosis that might significantly change their course of recovery (e.g., collagen-vascular disorder). 436 hip reconstructions in 233 patients were included in the analysis. 188 patients (357 hips) were immobilized in a hip spica cast post-operatively, while 45 patients (79 hips) were immobilized with an abduction pillow with or without knee immobilizers. For the purposes of comparing radiographic outcomes, number of hips operated on was used, while post-operative complications are compared on an individual patient basis.
Outcome Variables
Demographic data and complications were reviewed for the post-operative period. All immobilization was maintained for at least 6 weeks post-operatively, with eventual weaning by 3 months post-operatively. AP pelvis radiographs, as well as intra-operative fluoroscopic images, were used for radiographic assessment. aMPFA was measured at index using intraoperative fluoroscopy. AI, MP, and aMPFA were measured at six weeks post-operatively and one year post-operatively. AI and MP could not be accurately assessed via index fluoroscopy as they require an image with both hips in view.
Statistical Methods
Descriptive statistics including mean and standard deviation were used to characterize continuous variables. Paired t-tests were used to evaluate demographic differences between the immobilization groups. Ideal radiographic measurements were defined as follows: aMPFA = 80–88°, AI = 20–26°, MP less than 15% (2), the number of patients meeting these parameters in each group was documented for each measured time point. Fisher’s exact test was used to evaluate difference between the two groups. Change in each radiographic parameter over follow-up time was also analyzed and compared between the two groups.
Results
Demographic data and disease characteristics are summarized in Tables 1 and 2, demonstrating the overall similarity of the two groups. All patients underwent at least a VDRO. 21 (26.9% of patients treated with abduction pillow underwent pelvic osteotomy in addition to VDRO, compared to 123 (34.5%) treated with spica cast (p = 0.23). There were no differences between the spica cast and the abduction pillow group for sex distribution, ethnicity, BMI, follow up time. The abduction pillow group was significantly older, taller, and heavier on average. There was no significant difference in GMFCS classification or CP type between the two groups. There was a difference in CP diagnosis with more quadriplegic and triplegic involvement in the casting group.
Radiographic Outcomes
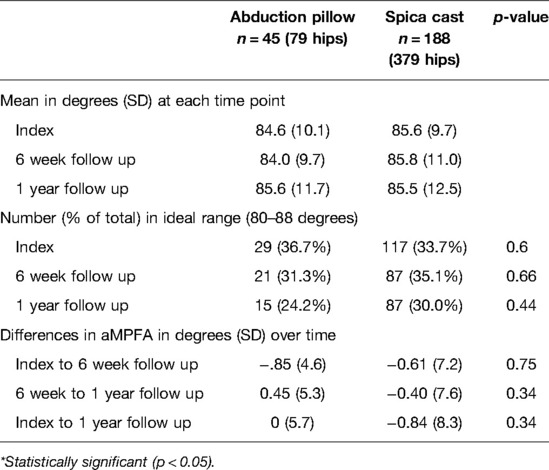
aMPFA (Table 3)
Mean measurements were similar throughout the course of follow up in both groups (Table 3). There was no statistically significant difference in number of hips with ideal measurements at any time point, and no difference in angular change over the year of follow up.
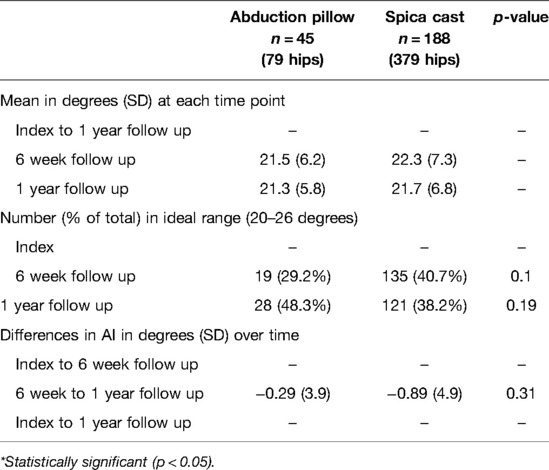
AI (Table 4)
Mean measurements were also similar throughout the course of follow up, and there was never a statistically significant difference in number of hips with ideal measurements (Table 4). There was a higher percentage of hips treated with spica cast with improved AI at index, however this difference was not significant and decreased over the year of follow up. There was no difference in change in AI over the course of follow up between the two groups.
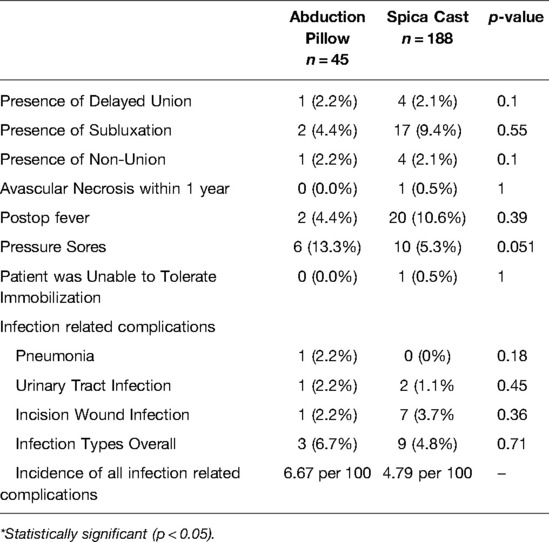
MP (Table 5)
MP was also similar at all time points between the two groups (Table 5). There was a statistically significant difference at 6 week follow up in the number of patients with ideal measurements (p = 0.0021), however in both groups by the 1 year follow up 100% ideal measurements were obtained. There was a statistically significant change in MP over time between the two groups with a change of 4% in the pillow group and 7% in the spica group (p = 0.02).
Postoperative Complications
Documented postoperative complications are detailed in Table 6. There were no significant differences between the two groups in rates of any complication.
Discussion
While hip spica casts were classically considered the standard for immobilization following hip reconstructive surgery in children with CP, there is evidence that satisfactory outcomes can be obtained with alternative methods of postoperative immobilization (19, 24, 25). Spica casts have been actively avoided by families and care teams familiar with them because they are cumbersome and associated with other challenges during care (26). Albrektson et al. compared the two methods in a retrospective review of 21 patients with CP or other genetic syndromes undergoing hip surgery and concluded that spica casts should be used in patients with osteopenia or instability in the early post-operative period (21). Truong et al. demonstrated similar pain and complication profiles in children treated in spica casts versus short leg casts linked with a bar (27). Modern internal fixation has proven reliable in maintaining the alignment and compression of osteotomies during healing. The stability of pelvic osteotomy techniques, when used, has also allowed many surgeons to view spica casting as optional. Miller et al. recently showed that there is a tremendous lack of consensus in postoperative immobilization for CP hip reconstruction (19). This study sought to directly compare outcomes of hip reconstruction at a single institution in children that were immobilized with spica casts versus abduction pillows and better elucidate the complication rate of these methods.
This review included 436 VDROs in 233 patients at a single institution, with similar demographic data between the two immobilization groups. There was no difference in the distribution of GMFCS level, with GMFCS V being most common. There were more children that underwent concomitant pelvic osteotomies in the casting group, but this was not a significant difference. The group of patients immobilized in a cast were significantly younger, shorter, and weighed less than the spica cast group. This is likely due to the decreased feasibility of caring for a child in a spica cast with increasing patient size.
The method of post-operative immobilization did not significantly affect radiographic parameters at one year. There was no difference in femoral correction (aMPFA) or acetabular correction (AI) between the two groups throughout the follow-up period. MP was more likely to be in the ideal range at 6 weeks in hips immobilized with casts, but this difference was not significant between the groups at 1 year. It was found that the MP changed less over time in the abduction pillow compared to the spica cast group. This may be due to the overall younger age and increased number of pelvic osteotomies in the spica group, creating a cohort with more remodeling potential in the hip (28, 29). Hip reduction has been shown to reliably improve over time following hip reconstruction (2, 12, 13). Every hip in this series had a MP less than 15% at one year, thus this initial difference in the depth of hip reduction did not affect the overall success of reconstruction.
There was no difference in any complication between the two groups. Skeletal complications such as delayed union, nonunion, and surgical site infection were not significantly different, with only one case of avascular necrosis identified by one year in the cohort. Medical complications were also similar between both groups. A common belief is that spica casts can result in skin sores, and this was observed in 5% of patients immobilized in this manner. However, 13% of patients immobilized with abduction pillows had documented pressure sores as well, either at bony prominences (e.g., sacrum) or from the immobilizing device itself (e.g., strap of pillow over the knee). It is important for clinicians and families to be aware that neither method of immobilization is benign—careful attention to skin integrity is mandatory while the devices are in place, and our facility has developed a protocol to prevent these pressure sores with the abduction pillow.
Our retrospective study has some limitations. There were unequal numbers in each treatment group, reflecting the change in practice that occurred during the study period. This non-randomized study allowed surgeons to choose immobilization method based on preference, which introduces selection bias in assigning the method used and also fails to control for confounders (e.g., osteopenia). Both groups were very similar and represent an accurate snapshot of the broad distribution of children with CP that undergo hip reconstruction. As discussed, the spica group was younger and smaller, likely reflecting surgeon preference of avoiding casts in larger, older patients less likely to tolerate them. There is no established protocol regarding this at our institution. Patient positioning for pelvic radiographs is sometimes difficult at 6 weeks due to patient discomfort, especially from joint stiffness if they were just removed from a cast. This could result in inaccurate measurements at that time point, but there was ultimately a lack of statistical difference at 1 year in any of our measurements. Some patients were excluded due to other diagnoses that may have altered treatment plans, such as collagen or genetic disorders and other bone dysplasias. The surgeon and family should discuss how to immobilize these patients with whichever method is safest based on their individual needs. This study did not examine compliance with the wedge pillow, as it is theoretically removable. A major goal of employing a pillow instead of a cast is to decrease the burden on the family. This study lacks a qualitative measure of treatment-related quality of life that could better enable surgeons to understand the perspective of the families they treat, which could ultimately contribute to the choice of immobilization. This paper also did not address patients specifically undergoing multi-level surgery, in which other immobilization in the lower limbs may preclude utilization of a pillow. In these situations surgeon’s may consider using a pillow in conjunction with casts versus an alternative method. Reconstruction frequently alleviates contractures about the hip, but caution should be considered if there is any residual asymmetry (e.g., windswept deformity).
Conclusion
The use of a spica casts after hip reconstruction in CP presents many challenges to the patient, family, and clinician. This study sought to compare outcomes of hip reconstruction after which children were immobilized with spica casts or hip abduction pillows. There were no differences in osteotomy alignment or healing, and ultimate hip reduction was excellent regardless of which method was used. Skin complications were observed in both groups. This would suggest it is reasonable to utilize a patient focused shared decision making conversation as part of the process in determining what type of immobilization would be best. Future research is needed to determine if the elimination of spica casting does truly lessen the treatment burden on families while still ensuring safe immobilization.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Colorado Multiple Institutional Review Board. Written informed consent from the participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author Contributions
Study Designed by authors DBF, JTR. Data acquisition performed by authors ALV, DBF, AST, AAS. Data analysis and interpretation performed by LJS, ALV, AAS, AST. All authors contributed to the article and approved the submitted version.
Acknowledgements
The authors wish to thank the CP team at Children's Hospital Colorado lead by Dr. Frank Chang, and the faculty/staff of CGMA and the J. T. Tai & Company Foundation for providing space and personnel to perform this research project.
Conflict of Interest
Dr. Frumberg reports personal fees from Orthofix, personal fees from OrthoPediatrics, personal fees from Ultragenyx, outside the submitted work. Dr. Rhodes reports personal fees from OrthoPediatrics, and a research grant from Smith & Nephew both outside the submitted work. All other authors declare that they have no personal or financial relationships that could create a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rosenbloom L. Definition and classification of cerebral palsy. definition, classification, and the clinician. Dev Med Child Neurol Suppl. (2007) 109:43. doi: 10.1111/j.1469-8749.2007.tb12629.x
2. Shore B, Spence D, Graham H. The role for hip surveillance in children with cerebral palsy. Curr Rev Musculoskelet Med. (2012) 5(2):126–34. doi: 10.1007/s12178-012-9120-4
3. Huh K, Rethlefsen SA, Wren TA, Kay RM. Surgical management of hip subluxation and dislocation in children with cerebral palsy: isolated VDRO or combined surgery? J Pediatr Orthop. (2011) 31(8):858–63. doi: 10.1097/BPO.0b013e31822e0261
4. Kocabiyik A, Misir A, Kizkapan TB, Yildiz KI, Kaygusuz MA, Alpay Y, et al. Changes in hip, knee, and ankle coronal alignments after total hip arthroplasty with transverse femoral shortening osteotomy for unilateral crowe type IV developmental dysplasia of the hip. J Arthroplasty. (2017) 32(11):3449–56. doi: 10.1016/j.arth.2017.05.044
5. Paley D, Pfeil J. Principles of deformity correction around the knee. Orthopade. (2000) 29(1):18–38. doi: 10.1007/s001320050004
6. Reimers J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl. (1980) 184:1–100. doi: 10.3109/ort.1980.51.suppl-184.01
7. Shore BJ, Shrader MW, Narayanan U, Miller F, Graham HK, Mulpuri K. Hip surveillance for children with cerebral palsy: a survey of the POSNA membership. J Pediatr Orthop. (2017) 37(7):e409–14. doi: 10.1097/BPO.0000000000001050
8. Soo B, Howard JJ, Boyd RN, Reid SM, Lanigan A, Wolfe R, et al. Hip displacement in cerebral palsy. J Bone Joint Surg Am. (2006) 88(1):121–9.16391257
9. American Academy for Cerebral Palsy and Developmental Medicine. Hip Surveillance in Cerebral Palsy. https://www.aacpdm.org/publications/care-pathways/hip-surveillance [Accessed January 23, 2022] (2017).
10. Hagglund G, Alriksson-Schmidt A, Lauge-Pedersen H, Rodby-Bousquet E, Wagner P, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Joint J. (2014) 96-b(11):1546–52. doi: 10.1302/0301-620X.96B11.34385
11. Bouwhuis CB, van der Heijden-Maessen HC, Boldingh EJ, Bos CF, Lankhorst GJ. Effectiveness of preventive and corrective surgical intervention on hip disorders in severe cerebral palsy: a systematic review. Disabil Rehabil. (2015) 37(2):97–105. doi: 10.3109/09638288.2014.908961.24731007
12. Chang FM, May A, Faulk LW, Flynn K, Miller NH, Rhodes JT, et al. Outcomes of isolated varus derotational osteotomy in children with cerebral palsy hip dysplasia and predictors of resubluxation. J Pediatr Orthop. (2018) 38(5):274–8. doi: 10.1097/BPO.0000000000000809
13. Chang FM, Ma J, Pan Z, Ingram JD, Novais EN. Acetabular remodeling after a varus derotational osteotomy in children with cerebral palsy. J Pediatr Orthop. (2016) 36(2):198–204. doi: 10.1097/BPO.0000000000000418
14. Eilert RE, MacEwen GD. Varus derotational osteotomy of the femur in cerebral palsy. Clin Orthop Relat Res. (1977) (125):168–72. PMID: 880760
15. Shrader MW, Wimberly L, Thompson R. Hip surveillance in children with cerebral palsy. J Am Acad Orthop Surg. (2019) 27(20):760–8. doi: 10.5435/JAAOS-D-18-00184
16. Pope DF, Bueff HU, DeLuca PA. Pelvic osteotomies for subluxation of the hip in cerebral palsy. J Pediatr Orthop. (1994) 14(6):724–30. doi: 10.1097/01241398-199414060-00007
17. Shore BJ, Zurakowski D, Dufreny C, Powell D, Matheney TH, Snyder BD. Proximal femoral varus derotation osteotomy in children with cerebral palsy: the effect of age, gross motor function classification system level, and surgeon volume on surgical success. J Bone Joint Surg Am. (2015) 97(24):2024–31. doi: 10.2106/JBJS.O.00505
18. Shore BJ, Powell D, Miller PE, Matheney TH, Snyder BD. Acetabular and femoral remodeling after varus derotational osteotomy in cerebral palsy: the effect of age and gross motor function classification level. J Pediatr Orthop B. (2016) 25(4):322–30. doi: 10.1097/BPB.0000000000000322
19. Miller SD, Juricic M, Fajardo N, So J, Shore B, Narayanan UG, et al. Variability in postoperative immobilization and rehabilitation following reconstructive hip surgery in nonambulatory children with cerebral palsy. J Pediatr Orthop. (2021) 41(7):e563–9. doi: 10.1097/BPO.0000000000001850
20. Noonan KJ, Walker TL, Kayes KJ, Feinberg J. Varus derotation osteotomy for the treatment of hip subluxation and dislocation in cerebral palsy: statistical analysis in 73 hips. J Pediatr Orthop B. (2001) 10(4):279–86. PMID: 11727369
21. Albrektson J, Kay RM, Tolo VT, Skaggs DL. Abduction pillow immobilization following hip surgery: a welcome alternative for selected patients. J Child Orthop. (2007) 1(5):299–305. doi: 10.1007/s11832-007-0054-0
22. Stasikelis PJ, Lee DD, Sullivan CM. Complications of osteotomies in severe cerebral palsy. J Pediatr Orthop. (1999) 19(2):207–10. doi: 10.1097/01241398-199903000-00014
23. Mubarak SJ, Valencia FG, Wenger DR. One-stage correction of the spastic dislocated hip. use of pericapsular acetabuloplasty to improve coverage. J Bone Joint Surg Am. (1992) 74(9):1347–57. doi: 10.2106/00004623-199274090-00008
24. Hoffer MM, Stein GA, Koffman M, Prietto M. Femoral varus-derotation osteotomy in spastic cerebral palsy. J Bone Joint Surg Am. (1985) 67(8):1229–35. doi: 10.2106/00004623-198567080-00014
25. Norman-Taylor FH. Spicaless hip surgery for cerebral palsy. Orthop Proc. (2015) 97-B(Supp 9):13–13. https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992X.97BSUPP_9.BSCOS2015-013
26. Miller F, Girardi H, Lipton G, Ponzio R, Klaumann M, Dabney KW. Reconstruction of the dysplastic spastic hip with peri-ilial pelvic and femoral osteotomy followed by immediate mobilization. J Pediatr Orthop. (1997) 17(5):592–602. doi: 10.1097/01241398-199709000-00005
27. Truong U, Sylvanus T, Koester TM, Barney CC, Georgiadis AG, Carpenter J, et al. A comparison of hip spica casting to short leg casts and bar after hip reconstruction in cerebral palsy. Cureus. (2020) 12(5):e8028. doi: 10.7759/cureus.8028
28. Dohin B. The spastic hip in children and adolescents. Orthop Traumatol Surg Res. (2019) 105(1S):S133–41. doi: 10.1016/j.otsr.2018.03.018
Keywords: abduction pillow, spica cast, immobilization, hip reconstruction, cerebral palsy
Citation: Vasconcellos AL, Tagawa AS, Rhodes JT, Silveira LJ, Skinner AA and Frumberg DB (2022) Postoperative Immobilization After Hip Reconstruction in Cerebral Palsy: No Difference Between Hip Spica and Abduction Pillow. Front. Surg. 9:863287. doi: 10.3389/fsurg.2022.863287
Received: 27 January 2022; Accepted: 12 May 2022;
Published: 6 June 2022.
Edited by:
Angelo Gabriele Aulisa, Bambino Gesù Children’s Hospital (IRCCS), ItalyReviewed by:
Dmitry Popkov, Russian Ilizarov Scientific Center for Restorative Traumatology and Orthopaedics, RussiaFrank Braatz, University Medical Center Göttingen, Germany
Copyright © 2022 Vasconcellos, Tagawa, Rhodes, Silveira, Skinner and Frumberg. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: David B. Frumberg RGF2aWQuRnJ1bWJlcmdAWWFsZS5lZHU=
Specialty section: This article was submitted to Pediatric Orthopedics, a section of the journal Frontiers in Surgery
 Alexander L. Vasconcellos
Alexander L. Vasconcellos Alex S. Tagawa
Alex S. Tagawa Jason T. Rhodes
Jason T. Rhodes Lori J. Silveira
Lori J. Silveira Austin A. Skinner2
Austin A. Skinner2