
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg., 25 March 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.855851
Purpose: To systematically evaluate the benefits of reducing and fixing displaced lesser trochanter (LT) of trochanteric fractures and when this procedure is worth the effect.
Methods: From database establishment through March 2021, four online databases (PubMed, Cochrane, Embase, and Web of Science) were searched for relevant literature that investigated reduction and fixation for displaced LT of trochanteric fractures. The papers were then screened by two reviewers independently and in duplicate according to prior inclusion and exclusion criteria. Demographic data as well as data on fracture types, surgical protocols, and surgical outcomes were recorded, analyzed, and interpreted.
Results: Total 10 clinical studies with 928 patients were included, in which 48 cases had intact LT and 880 cases involved the displaced LT, of which 196 (22.27%) cases underwent reduction and fixation for LT while the rest of 684 (77.73%) cases not. In these studies, complications were evaluated as a more applicable predictive parameter for operation than postoperative hip function.
Conclusion: It was beneficial to reduce and fix the displaced LT when one of the conditions below occurred: displacement distance of LT ≥2 cm, quantity of comminuted LT fragments ≥2, and range of LT fragments in medial wall ≥75%; the fracture line of LT fragments reaching or exceeding the midline of the posterior wall.
As the population aging increasingly, the incidence of hip fractures in senile people is obviously elevated (1). Trochanteric fractures account for a significant proportion of hip fractures, ranging from 45 to 50%, in which 50–60% are classified unstable (2). According to the most used classification systems, Arbeitsgemeinschaft fur Osteosynthesefragen foundation and the Orthopedic Trauma Association (AO/OTA) classification and Evans-Jensen classification, this pattern of fracture may involve four fragments the distal femoral fragment, the femoral neck, the greater trochanter, and the lesser trochanter (LT) (3). It is accepted that orthopedists should try to anatomically reduce and fix the two main fragments and greater trochanter (4, 5). Lesser trochanter, an important structure of the femoral posteromedial wall, plays a pivotal role in stress distribution and reconstruction stability in trochanteric fracture (6). However, the necessity of reducing and fixing LT fragments remains controversial (2–4).
At present, the most commonly used clinically operated protocols for trochanteric fracture include extramedullary fixation devices [e.g., dynamic hip screw (DHS)], intramedullary fixation devices[e.g., proximal femoral nail anti-rotation (PFNA)], and hip arthroplasty (e.g., hemiarthroplasty) (7, 8), but none of them are designed to fix the displaced LT. On the contrary, those orthopedic surgeons who advocate fixing the displaced LT have proposed kinds of fixation devices and skills since last century, including lag screw (9), cerclage wire (Figure 1) (2), double cables (10), candy-package (11), modified candy-package (12), etc.
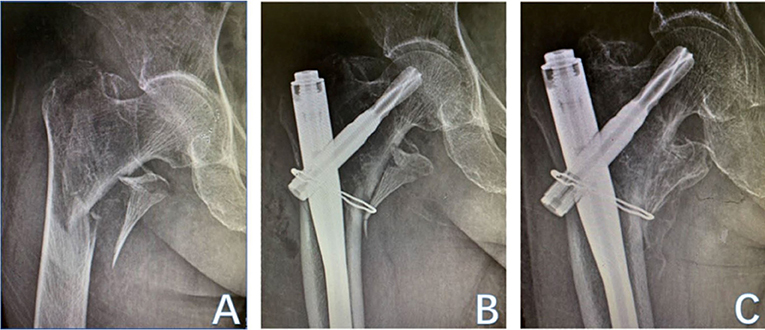
Figure 1. An 81-year-old woman suffered from trochanteric fracture with displaced LT (A). Ten days later, she underwent operation of PFNA and cerclage wire (B). The follow-up after 5 months implied LT union (C).
Besides, most classifications, such as AO/OTA (1990) (13), revised AO/OTA(2018) (14), Evans (15), and Evans/Jensen (16), didn't investigated the stratification exclusive for LT fracturing degree. Recently, a novel classification (Figure 2) for medial wall fragments in trochanteric fractures has been proposed (17). It classified medial fragments into three types based on the degree of posterior cortex involvement: type 1: LT fragment with fracture line not exceeding base of the LT; type 2: a larger LT fragment and posterior cortex involved near the base of LT with fracture line not reaching the midline of the posterior wall; type 3: a much larger LT fragment and large posterior cortex involved with fracture line reaching or exceeding the midline of the posterior wall. To the best of our knowledge, this was the first study that classified the posteromedial cortex (mainly the LT) in trochanteric fracture and investigated its potential predictive role in complications.
With a high LT detachment ratio of over 50% in trochanteric fractures (3, 18), many reports tried to demonstrate whether it was worth the effort to reduce and fix the displaced LT. However, they couldn't reach a consensus. Some reports (2, 8, 19) implicated that LT fixation could regain higher primary stability, resulting in lower implants failure rates, but the incidental price may increase, such as longer operation time, increased intra-operative blood loss, and iatrogenic injury of the surrounding nerves/vessels. Therefore, they concluded that reduction and fixation for LT should be individually weighed upon the patients' mobility demands and health status. In the meanwhile, several studies (3, 20, 21) demonstrated that reducing and fixing LT or not would get similar outcomes. On the contrary, some studies (4, 17, 22) verified that severely displaced LT might increase the postoperative complications, from which they recommended that this kind of LT should be reduced and fixed. Moreover, it is noticed that orthopaedists paid more attention to the postoperative injury of surrounding vessels (23–27) especially potentially life and limb-threatening pseudoaneurysm (28–37), caused by displaced LT. Therefore, the question “does the reduction and fixation for LT fragment in trochanteric fracture treatment worth the effect?” is hardly to be answered.
The current systematic review was performed using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) as the guidelines. From database establishment through November 2021, four online databases (PubMed, Cochrane, Embase, and Web of Science) had been searched that investigated reduction and fixation of LT in trochanteric fractures, with no language restriction (non-English literature was translated if necessary). The broad search included the following terms “lesser trochanter,” “trochanteric fracture,” “reduce,” “fix,” and “wire.” Moreover, the reference lists of the identified studies were hand-searched and gray literature sources, such as Open-Gray, were searched as additional search methods.
Inclusion criteria were as follows: (1) investigating human trochanteric femur fractures; (2) existing LT fragment; (3) reporting postoperative outcomes associated with fixed or unfixed LT fragments; and (4) randomized controlled trials (RCT), cohort studies, case-control studies, and case series.
Exclusion criteria were as follows: (1) femoral neck fracture involved; (2) pathologic fracture of LT (tumor metastasis); (3) LT avulsion fractures in adolescents with high-energy violence; and (4) no full-text available.
The initial outcome involved a total of 471 studies after searching four databases and other sources. The abstract and full text of this literature were screened by two reviewers (Yang and Mao) independently and in duplicate according to prior inclusion and exclusion criteria. Any screening discrepancies would be reassessed by the third senior reviewer (Dong) till they reached an agreement.
Data of all included studies were collected and recorded in an Excel spreadsheet (Version 2019; Microsoft Corp) by two reviewers (Yang and Mao), which included the information of the authors, published date, study design, sample size, mean age, mean follow-up, surgical protocols, and outcomes.
The methodological quality of all included studies was evaluated using Methodological Index for the Non-Randomized Studies (MINORS) instrument, the Newcastle-Ottawa Scale (NOS) instrument, and the Cochrane Risk of Bias (ROB) tool. MINORS are used to evaluate the non-comparative, comparative, and non-randomized studies with maximum scores of 16, 24, and 24, respectively (38). NOS is specially designed to assess the quality of case-control study and cohort study both with the maximum scores of 9 (39). Besides, the ROB tool is appropriate for the quality assessment of RCTs with the ROB figure (40).
The inter-reviewer agreements on abstract screening, full-text screening, and grading scores of the studies quality were evaluated using the kappa statistic. In the meanwhile, statistical analysis was performed using STATA (Stata Corp. LLC; College Station; Stata/MP 16.0 for Windows). It should be noted that owing to the inadequate reports, methodological difference, and various outcome indicators of included research, quantitative synthesis/meta-analysis was limited to be performed. Therefore, we performed the descriptive analysis for all included studies, and numeric data and categorical data were expressed as Mean ± SD and numbers with percentages, respectively. Statistics significance was calculated by Student's t-test, one-way ANOVA, and the Fisher exact test with a significance level of 0.05.
The primary retrieve for online databases resulted in 471 studies, of which 10 were full-text studies that met the inclusion and exclusion criteria (Figure 3). The reviewers reached substantial agreement and the interreviewer reliability at the abstract (κ = 0.893 [95% CI, 0.889–0.897]), full-text (κ = 1.000), and the quality evaluation of studies (κ = 0.841 [95% CI, 0.801–0.881]) was available.
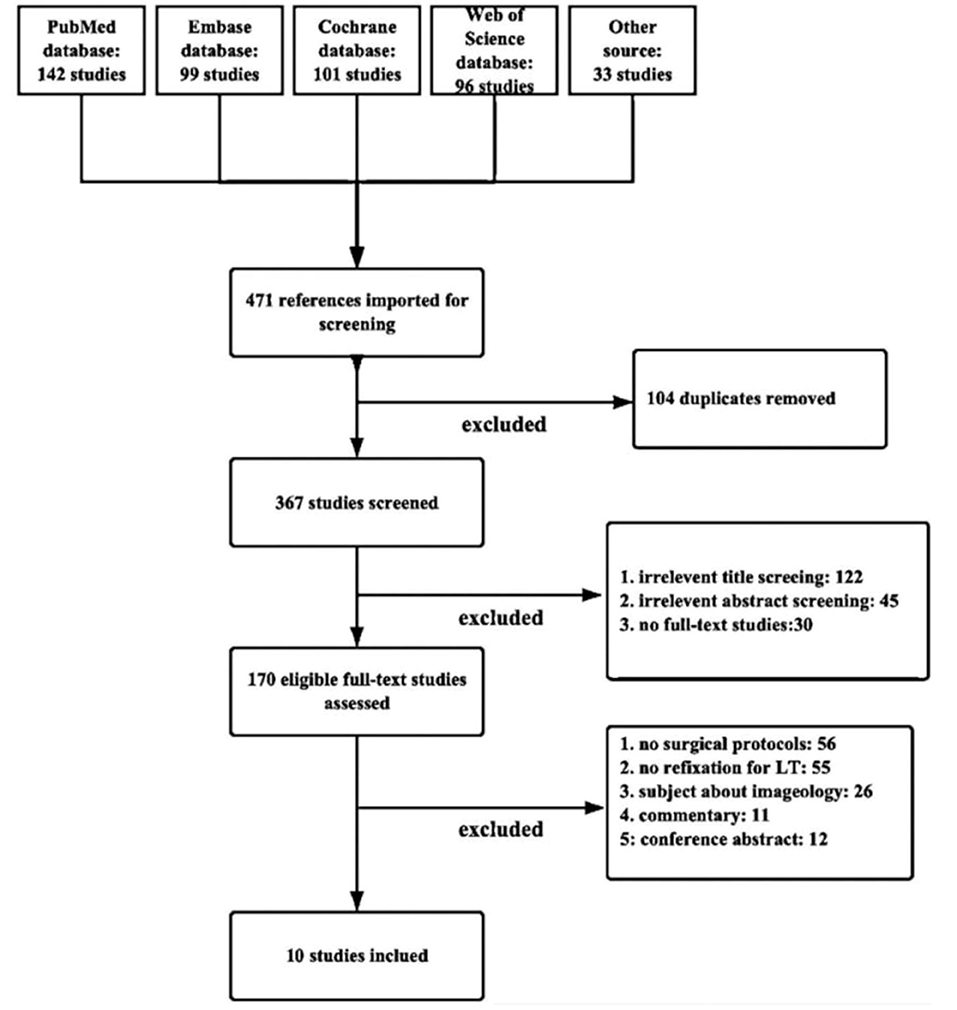
Figure 3. PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) flow diagram demonstrating the systematic review of the literature for studies investigating fixation necessity of displaced lesser trochanter in trochanteric fractures.
The included 10 studies (Table 1) consisted of two retrospective case series (Level 4), one prospective case series (Level 4), six retrospective comparative studies (Level 2), and one RCT (Level 1). The three cases series were evaluated by MINORS checklist with mean scores of 10.67 (range, 10–12), implicating a fair quality of evidence. The six retrospective comparative studies were assessed by NOS with mean stars of 7.83 (range, 6–9), demonstrating a high quality of evidence. In the meanwhile, using the ROB tool, evidence quality of the lone RCT was verified as a moderate risk of bias (Figure 4).
In each of the comparative studies, statistical differences of demographic data (such as gender ratio, age distribution ratio, and follow-up ratio) between/among groups were calculated, which ensured baseline groups equivalence.
Based on the limited studies involving the topic, only 10 reports were identified in the current study (Table 1). These studies described a total of 928 patients, from which 48 (5.17%) cases had intact LT while 880 (94.83%) cases involved the displaced LT, of which 196 (22.27%) cases underwent fixation of LT while the rest of 684 (77.73%) cases not. Moreover, these 928 patients with a mean age of 70.36 years (range, 23–94 years) comprised 389 men and 539 women. Besides, the mean follow-up was 20.15 months (range, 6.5–57 months) with eight studies reporting a minimum follow-up of 1 year except for the shorter follow-up of 6.5 months (3) and 9 months (9) in two reports. Besides, nine studies had an attrition ≤ 25.00% while one study (5) had a large attrition of 33.07%. Due to variations of reported outcomes among included studies, including eight studies reporting postoperative hip function, two (5, 41) reporting surgical costs, two (3, 19) reporting hip flexion strength, three (12, 41, 42) reporting change of neck-shaft angle (NSA), and four (5, 9, 12, 22) reporting complication incidence.
Based on anteroposterior X-ray films in all included studies, three studies set up the concrete cut-off of displacement distance of LT (DDLT, measurement method depicted in Figure 5), including 5 mm (12), 10 mm (22), and 20 mm (3) (Table 1). Besides, two other studies set up the concrete quantity and sizes of displaced LT. One was that three groups were built up based on the new classification for a medial wall in trochanteric fractures (17); the other study was that all patients were divided into five groups according to the quantity of LT fragment (<2, =2, and >2) and range of LT fragment in the femoral posteromedial wall (<75, ≥75%) (42).

Figure 5. Distance a and b are defined as the lengths from the highest fracture site to the corresponding site at the lesser trochanter and the lowest fracture site to the corresponding site at the lesser trochanter, respectively. And the displacement distance of lesser trochanter is defined as the average of the distance a and distance b.
As for the surgical protocols for trochanteric fractures with displaced LT in 880 patients, 196 (22.27%) patients' displaced LT were reduced and fixed while the rest (77.73%) were not. And 196 fixation devices consisted of 19 (9.69%) lag screws and 177 (90.31%) wires, of which 22 (12.43%) wires were bundled up as modified candy-package while bundling techniques of the rest of 155 (87.57%) wires were not mentioned. Besides, among 196 patients with displaced LT fixed, 58 (29.59%) cases underwent IM with wiring, 119 (60.71%) DHS with wiring, and 19 (9.69%) DHS with a lag screw.
Among the included studies, eight studies reported postoperative hip function with Harris hip score (HHS) (43) or Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) (44), three reported femur NSA, two reported hip flexion strength, and one reported femoral neck shortening (FNS). It is obvious that HHS/WOMAC is the most concerned outcome indicator for orthopedic surgeons. Puram et al. (20) believed that HHS was such a representative because it reflected both function and symptoms of the hip, including pain, deformity, limp, shortening, and range of motion. According to HHS checklist (100 points), ≥90, excellent; 80–89, good; 70–79, fair; <70, poor (Table 2).
Out of eight studies that made a statistical analysis about HHS/WOMAC, five studies (5, 12, 19, 20, 22) demonstrated no statistical significance between/among groups, two studies (3, 9) verified that both fixation and non-fixation of displaced LT got “excellent” marks. One study (41) substantiated that fixation of displaced LT would get a higher mark (p = 0.049). It should be noticed that no statistical significance in HHS was observed between DHS with wiring (20) vs. IM nail with wiring (22) (p = 0.444) (Table 3).
The NSA is a meaningful method to assess the collapse degree of the femoral head after fracture, which is 127 degree (range, 110–140 degrees) in adults (45). Besides, recently orthopedists prefer to use the term “telescoping” to quantify the degree of FNS after fracture, of which the value is negatively correlated with the stability of the hip joint (42). Thus, orthopedic surgeons try to reduce and fix the fracture fragments to their original anatomical position in case of substantial changes of NSA and FNS leading to instability of the femur-implant structure, even implant failure. However, the surgical protocol of DHS with wiring (20, 41) had less but not significant influence on postoperative NSA changes (p > 0.05) compared to that of non-fixation for LT. Nevertheless, one study (42) demonstrated that larger (≥75% area of the posteromedial wall) and much more comminuted (≥2) LT fragments could result in statistically significant changes of NSA (p < 0.025) and FNS (p < 0.01).
As for the hip flexion strength, Aprato et al. (46) believed that displaced LT implication could significantly reduce hip flexion strength compared to that of the trochanteric fractures without displaced LT in 90 degree position, neutral position, and Figure 4 position (p = 0.008, p = 0.034, p = 0.034, respectively). Although Schenkel et al. (3) demonstrated that on comparison with the uninjured hip side, non-fixation for LT had no significant influence on hip flexion strength in 0 and 30 degrees position (both p > 0.05).
Various complications associated with displaced LT were reported in 10 studies including implant failure, severe thigh pain, loss of reduction, and hip varus deformity. However, only six studies reported complications and out of which two studies (17, 22) demonstrated that much bigger displaced LT (type 3 or its displacement distance ≥1 cm) fragments had significant differences in complication incidence to that of the inferiors (p = 0.001, p = 0.043, respectively). Besides, implant failure is seriously necessary for the revision operation. Only one study (17) reported that this severe complication was defined: (1) subsequent fracture, (2) fracture nonunion, (3) cut-out, (4) implant or screw breakage, (5) progressive fracture displacement, and (6) lateral protrusion of the blade or screw. In the meanwhile, they also demonstrated that LT of type 3 (one type in the newly reported classification of the medial wall in trochanteric fractures mentioned above) had a significant incidence of implant failure to that of other types (p = 0.001). What's more, it was investigated that large (≥1 cm) displaced LT without fixation could result in significantly unbearable thigh pain (p = 0.023) (22) (Table 4).
Only two studies (5, 41) reported the differences in blood loss and operative time due to different fracture types and surgical protocols between subgroups. It was reported that both using PFNA treatments, the operative time, and blood loss were significantly elevated in trochanteric fractures with displaced LT than that of those with intact LT (both, p < 0.05) (5). Moreover, between LT fixed group and not fixed group the former was demonstrated that would significantly augment the two costs (both, p < 0.05) (41).
To the best of our knowledge, a review of LT is rare and the current systematic review on this subject is the first. In the current study, the primary finding was that during 2013–2020's orthopedic surgeons preferred not to deal with the displaced LT (636 cases of LT non-fixation in 880 cases involving displaced LT, 72.7%). But if they did deal, they preferred to choose the protocols of DHS with wires (60.71%) than IM nail with wires (29.59%), and DHS with lag screw (9.69%).
Moreover, we analyzed some significant elements and surgical protocols that future orthopedic surgeons should notice in operations for trochanteric fractures with kinds of displaced LT. In 10 included studies, HHS was the most used and reported clinical instrument to assess patients' postoperative hip function in multiple aspects, as the primary outcome indicator in the current study as well. After evaluating the correlation between HHS and surgical protocols, it was not surprised that whether to fix displaced LT or not, no statistical significance in HHS was observed, and both resulted in excellent/good HHS marks (p > 0.05), which was consistent with the conventional operation selection trend that most orthopedists preferred not to reduce or fix LT fragment. However, one study reported statistical significance in HHS between subgroups (p = 0.049) (41), and we analyzed this might result from restrictive fracture types of distribution and bias. Moreover, we observed that protocols of DHS/IM nail and wires/lag screw all got excellent/good HHS marks and no significant differences among these methods were found. In the meanwhile, we observed that when the quantity of comminuted LT fragments was ≥2 and the range of LT fragments in the posteromedial wall was ≥75%, the differences of complications associated indicators, femoral NSA change, and FNS, reached statistical significance (p < 0.01, p < 0.025, respectively). Besides, one biomechanical study (8) demonstrated that specific protocol, such as PFNA with LT fixation, could significantly reduce FNS. Therefore, we analyzed that severely comminuted LT might exert a negative role in stability of the femur-implant structure, and protocol of PFNA with wiring LT would have more benefits. But specific surgical protocol should be further individually ascertained after assessing bony quality and fracture types of various patients. After exclusion of possible influence due to uneven distribution of fracture types and complex hip strength compensatory mechanism, we analyzed hip flexion strength, a complication associated indicator as well, was not significantly affected by displaced LT nor the various surgical protocols, which was consistent with HHS (Table 5).
Complication was the other vital parameter to weigh the feasibility of carrying out a reduction and fixation procedure for displaced LT during operation, as the secondary outcome indicator in the current study as well. We analyzed that the incidence of complication was significantly elevated when the displaced LT featured as DDLT ≥2 cm or type 3, especially the implant failure in the latter situation.
Previous studies had demonstrated that in unstable trochanteric fractures reduction and fixation for small and large LT fragments could increase the mechanical stability by 17 and 57%, respectively (6). It also had been substantiated that large LT, as well as its extent calcar, exerted a vital influence on redistributing stress in the proximal femur by increasing load in the anterolateral wall and decreasing the load in the posteromedial wall (4). Besides, fixation for displaced LT could exert a buttress effect on the posteromedial cortex to get initial stability, which could allow patients early ambulation (47). It is widely identified by clinical physicians that large posteromedial bone fragments with large value of displacement distance need to be surgically fixed, but no consensus is reached for the concrete degree of this “large”(4, 17, 22). We observed that four included studies had implied how large of displaced LT should be noticed: DDLT ≥ 10 mm (3), ≥ 20 mm (22), a quantity of comminuted LT fragments ≥2 with a range of displaced LT in posteromedial wall ≥75% (42), and type 3 (17). Moreover, Zhang et al. (4) divided the LT fragments into three types: dislocated but intact LT, LT maintaining a continuation with greater trochanter and quantity of comminuted LT fragments >3. From which, they recommended reduction and fixation for the former two types, but the last type was not for difficulties in present techniques or increased intraoperative risks. Owing to the inadequate reports of primary and secondary outcome indicators in included studies, overall statistical analysis was hard to perform. Therefore, we proposed a novel classification about cut-offs of DDLT and the sizes of displaced LT to assess when prefer to get displaced LT fixed: (a1) DDLT <1 cm, preferring not to reduce or fix displaced LT, (a2) 1 cm ≤ DDLT < 2 cm, demanding further individual judgment, (a3) DDLT ≥ 2 cm, preferring to reduce and fix displaced LT; (b1) quantity of comminuted LT fragments <2 or range of LT fragments in medial wall <75%, preferring not to reduce or fix displaced LT, (b2) quantity of comminuted LT fragments ≥2 and range of LT fragments in medial wall ≥75%, preferring to reduce and fix displaced LT; (c1) fracture line of LT fragments not reaching the midline of the posterior wall, preferring not to reduce or fix displaced LT, (c2) fracture line of LT fragments reaching or exceeding the midline of the posterior wall, preferring to reduce and fix displaced LT.
Systematic assessment of included studies revealed several limitations that more than half of them reported inadequate main outcome indicators, thus meta-analysis and overall statistical analysis were limited to perform. Moreover, the topic “postoperative outcome” of patients with trochanteric fractures generally was not affected by displaced LT alone. More elements, like fracture line involving femoral lateral wall, osteoporosis, anatomical reduction, and surgical devices selection, etc., were previously demonstrated that played pivotal roles in postoperative outcomes (4), which means that these confounding parameters with inadequately reporting might delay proper evaluation of efficacy frequency and severity of adverse events. Therefore, these limitations should be further systematically investigated in the future studies.
In the current study, we suggested that it was beneficial to reduce and fix the displaced LT when one of conditions below occurred: DDLT ≥2 cm; quantity of comminuted LT fragments ≥2 and range of LT fragments in medial wall ≥75%; and fracture line of LT fragments reaching or exceeding the midline of the posterior wall. Besides, we didn't find any significant difference in postoperative outcomes between the two protocols PFNA with LT wires and DHS with LT wires.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Y-HD and A-LY had the idea for the article. A-LY and WM performed the literature search, data analysis, and the first draft. Y-HD, J-GW, Y-QH, H-FN, and H-LL critically revised and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
This study was funded by the Highlevel Talent Special Fund of the Minhang District of Shanghai (File No. 5-1), which is received for open access publication fees.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank Dr. Lin-Li Li for the article formatting and submitting, his guidance, which greatly assisted in the final phase of the study.
DDLT, displacement distance of LT; NSA, neck-shaft angle; FNS, femoral neck shortening; LTFQ, quantity of comminuted lesser trochanter fragments; LTFR, range of lesser trochanter fragment in medial wall; VAS, visual analog scale.
1. Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. (2017) 377:2053–62. doi: 10.1056/NEJMcp1611090
2. Wu HF, Chang CH, Wang GJ, Lai KA, Chen CH. Biomechanical investigation of dynamic hip screw and wire fixation on an unstable intertrochanteric fracture. Biomed Eng Online. (2019) 18:49. doi: 10.1186/s12938-019-0663-0
3. Schenkel M, Kaniewska M, Bühler T, Anderson S, Eid K. No difference in flexion power despite iliopsoas fatty degeneration in healed hip fractures with large lesser trochanter displacement. Eur J Orthop Surg Traumatol. (2018) 28:1313–9. doi: 10.1007/s00590-018-2200-4
4. Zhang Y, Sun Y, Liao S, Chang S. Three-dimensional mapping of medial wall in unstable pertrochanteric fractures. Biomed Res Int. (2020) 2020:8428407. doi: 10.1155/2020/8428407
5. Liu X, Liu Y, Pan S, Cao H, Yu D. Does integrity of the lesser trochanter influence the surgical outcome of intertrochanteric fracture in elderly patients? BMC Musculoskelet Disord. (2015) 16:47. doi: 10.1186/s12891-015-0492-7
6. Apel DM, Patwardhan A, Pinzur MS, Dobozi WR. Axial loading studies of unstable intertrochanteric fractures of the femur. Clin Orthop Relat Res. (1989) 246:156–64. doi: 10.1097/00003086-198909000-00025
7. Ehlinger M, Favreau H, Eichler D, Adam P, Bonnomet F. Early mechanical complications following fixation of proximal femur fractures: From prevention to treatment. Orthop Traumatol Surg Res. (2020) 106:S79–87. doi: 10.1016/j.otsr.2019.02.027
8. Ehrnthaller C, Olivier AC, Gebhard F, Dürselen L. The role of lesser trochanter fragment in unstable pertrochanteric A2 proximal femur fractures - is refixation of the lesser trochanter worth the effort? Clin Biomech. (2017) 42:31–7. doi: 10.1016/j.clinbiomech.2016.12.013
9. Ye F, Zhang LJ, Li YZ, Zheng XD, Wang X, Yang YB, et al. [Design of the reduction fixator and its clinical application in treating fracture of lesser trochanter of femur]. Zhongguo Gu Shang. (2015) 28:726–9.
10. Schopper C, Faschingbauer M, Moeller RT, Gebhard F, Duerselen L, Seitz A. Modified candy-package technique vs. cerclage technique for refixation of the lesser trochanteric fragment in pertrochanteric femoral fractures. A biomechanical comparison of 10 specimen. Injury. (2020) 51:1763–8. doi: 10.1016/j.injury.2020.06.008
11. Lee JM, Lee JH, Lee CW, Kim HM. New wiring method for lesser trochanter fixation in unstable intertrochanteric fractures – technical note. J Korean Fract Soc. (2005):18:209–12. doi: 10.12671/jkfs.2005.18.2.209
12. Kim GM, Nam KW, Seo KB, Lim C, Kim J, Park YG. Wiring technique for lesser trochanter fixation in proximal IM nailing of unstable intertrochanteric fractures: a modified candy-package wiring technique. Injury. (2017) 48:406–13. doi: 10.1016/j.injury.2016.11.016
13. Müller ME, Koch P, Schatzker J. The Comprehensive Classification of Fractures of Long Bones. New York, NY: Springer (1990).
14. Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma. (2018) 32(Suppl 1):S1–70. doi: 10.1097/BOT.0000000000001063
15. Evans EM. The treatment of trochanteric fractures of the femur. J Bone Joint Surg Br. (1949) 31b:190–203. doi: 10.1302/0301-620X.31B2.190
16. Jensen JS. Classification of trochanteric fractures. Acta Orthop Scand. (1980) 51:803–10. doi: 10.3109/17453678008990877
17. Li P, Lv Y, Zhou F, Tian Y, Ji H, Zhang Z, et al. Medial wall fragment involving large posterior cortex in pertrochanteric femur fractures: a notable preoperative risk factor for implant failure. Injury. (2020) 51:683–7. doi: 10.1016/j.injury.2020.01.019
18. Montoli C, Pasquali C, Paiusco E, Pellecchia V, Vulcano E. Lesser trochanter migration following intramedullary fixation of an intertrochanteric femur fracture. Case Rep Orthop. (2016) 2016:9348032. doi: 10.1155/2016/9348032
19. Aprato A, Lo Baido R, Crosio A, Matteotti R, Grosso E, Massè A. Lesser trochanteric avulsion in trochanteric fracture: do we need to fix it in young patients? J Orthop Traumatol. (2013) 14:S3. doi: 10.1007/s10195-013-0257-8
20. Puram C, Pradhan C, Patil A, Sodhai V, Sancheti P, Shyam A. Outcomes of dynamic hip screw augmented with trochanteric wiring for treatment of unstable type A2 intertrochanteric femur fractures. Injury. (2017) 48(Suppl. 2):S72–7. doi: 10.1016/S0020-1383(17)30498-9
21. Sharma G, Gn KK, Khatri K, Singh R, Gamanagatti S, Sharma V. Morphology of the posteromedial fragment in pertrochanteric fractures: a three-dimensional computed tomography analysis. Injury. (2017) 48:419–31. doi: 10.1016/j.injury.2016.11.010
22. Sun Q, Ge W, Hu H, Li G, Wu J, Lu G, et al. The influence of position of the displaced lesser trochanter on clinical outcome of unstable trochanteric femur fractures in the elderly. Biomed Res Int. (2018) 2018:5013646. doi: 10.1155/2018/5013646
23. Mayurasakorn C, Phiphobmongkol V, Sridermma W, Bavonratanavech S. Profunda femoris artery injury caused by lesser trochanter fragment in intertrochanteric fracture: a case report. Trauma Case Reports. (2018) 13:14–7. doi: 10.1016/j.tcr.2017.10.006
24. Lee PYF, Rao PVR, Golding DM, Brock J. Delayed profunda femoris artery bleeding after intramedullary nailing of an unstable intertrochanteric fracture: a case report. JBJS Case Connect. (2017) 7:e60. doi: 10.2106/JBJS.CC.16.00217
25. Regus S, Lang W. Arterial injury and pseudoaneurysm formation after lesser trochanter fracture. Int J Surg Case Rep. (2015) 14:4–6. doi: 10.1016/j.ijscr.2015.06.033
26. Tomčovčík L, Kováč P, Dano J, Cuha R. Late laceration of the superficial femoral artery by an intertrochanteric fracture fragment. HIP Int. (2011) 21:273–5. doi: 10.5301/hip.2011.6512
27. Mauerhan DR, Maurer RC, Effeney D. Profunda femoris arterial laceration secondary to intertrochanteric hip fracture fragments: a case report. Clin Orthop Relat Res. (1981) 161:215–9. doi: 10.1097/00003086-198111000-00026
28. Acosta HF, Solé Florensa P, Marín Nasarre J. Pseudo-aneurysm of the deep femoral artery secondary to displacement of the lesser trochanter in a pertrochanteric fracture of the femur. Case Report Revista Colombiana de Ortopedia y Traumatologia. (2020) 34:82–4. doi: 10.1016/j.rccot.2020.04.001
29. Nossa JM, Márquez D, Rodriguez S, Muñoz JM, Alzate R, Ospina J, et al. Pseudoaneurysm of the deep femoral artery, an unusual complication in intertrochanteric hip fracture: a case study. Curr Orthop Pract. (2019) 30:577–81. doi: 10.1097/BCO.0000000000000808
30. Arbeloa-Gutierrez L, Arenas-Miquelez A, Muñoa L, Gordillo A, Eslava E, Insausti I, et al. Lateral circumflex femoral artery false aneurysm as a complication of intertrochanteric hip fracture with displaced lesser trochanter. Journal of Surgical Case Reports. (2019) 2019:rjz184. doi: 10.1093/jscr/rjz184
31. Piolanti N, Giuntoli M, Nucci AM, Battistini P, Lisanti M, Andreani L. Profunda femoris artery pseudoaneurysm after intramedullary fixation for a pertrochanteric hip fracture. J Orthop Case Rep. (2017) 7:74–7. doi: 10.13107/jocr.2250-0685.758
32. de Raaff CA, van Nieuwenhuizen RC, van Dorp TA. Pseudoaneurysm after pertrochanteric femur fracture: a case report. Skeletal Radiol. (2016) 45:575–8. doi: 10.1007/s00256-015-2315-1
33. Sharma G, Singh R, Sharma V, Farooque K, Kumar A. Acute femoral artery pseudoaneurysm due to lesser trochanter fragment: an unusual complication of an intertrochanteric fracture. Chin J Traumatol. (2013) 16:301–3. doi: 10.3760/cma.j.issn.1008-1275.2013.05.011
34. Lohmann H, Esenwein S, Geier B, Vogel T, Kleinert H. False aneurysm of the deep femoral artery due to pertrochanteric fracture of the hip with displaced fragment of the lesser trochanter. Zeitschrift für Orthopädie und Unfallchirurgie. (2009) 147:23–5. doi: 10.1055/s-2008-1039115
35. Kizilates U, Nagesser SK, Krebbers YM, Sonneveld DJ. False aneurysm of the deep femoral artery as a complication of intertrochanteric fracture of the hip: options of open and endovascular repairs. Perspect Vasc Surg Endovasc Ther. (2009) 21:245–8. doi: 10.1177/1531003510365088
36. Ebong WW. False aneurysm of the profunda femoris artery following internal fixation of an intertrochanteric femoral fracture. Injury. (1978) 9:249–51. doi: 10.1016/0020-1383(78)90017-7
37. Fordyce A. False aneurysm of the profunda femoris artery following nail and plate fixation of an intertrochanteric fracture. Report of a case. J Bone Joint Surg Br. (1968) 50:141–3. doi: 10.1302/0301-620X.50B1.141
38. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. (2003) 73:712–6. doi: 10.1046/j.1445-2197.2003.02748.x
39. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
40. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
41. Guo X, Zhang Y, Xiao J, Xie H, Yu J. Design and clinical application of lesser trochanteric reduction fixation system. Zhongguo xiu fu chong jian wai ke za zhi. (2015) 29:133–7.
42. Ren H, Ao R, Wu L, Jian Z, Jiang X, Yu B. Effect of lesser trochanter posteromedial wall defect on the stability of femoral intertrochanteric fracture using 3D simulation. J Orthop Surg Res. (2020) 15:242. doi: 10.1186/s13018-020-01763-x
43. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. (1969) 51:737–55. doi: 10.2106/00004623-196951040-00012
44. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. (1988) 15:1833–40.
45. Iwamoto M, Basmajian JV, Strom CH. A method for determining femoral neck-shaft and anteversion angles. Arch Phys Med Rehabil. (1972) 53:253–60.
46. Aprato A, Lo Baido R, Crosio A, Matteotti R, Grosso E, Massè A. Does lesser trochanter implication affect hip flexion strength in proximal femur fracture? Eur J Trauma Emerg Surg. (2015) 41:523–9. doi: 10.1007/s00068-014-0476-6
Keywords: trochanteric fracture, lesser trochanter, reduce, fix, hip function, complication
Citation: Yang A-L, Mao W, Wu J-G, He Y-Q, Ni H-F, Li H-L and Dong Y-H (2022) When to Reduce and Fix Displaced Lesser Trochanter in Treatment of Trochanteric Fracture: A Systematic Review. Front. Surg. 9:855851. doi: 10.3389/fsurg.2022.855851
Received: 16 January 2022; Accepted: 21 February 2022;
Published: 25 March 2022.
Edited by:
Yang Lv, Peking University Third Hospital, ChinaReviewed by:
Junlin Zhou, Capital Medical University, ChinaCopyright © 2022 Yang, Mao, Wu, He, Ni, Li and Dong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: You-Hai Dong, eW91aGFpZG9uZzE5NjRAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.