- Department of Orthopaedics and Traumatology, Faculty of Medicine, National University of Malaysia, Kuala Lumpur, Malaysia
Lower limb surgery is usually performed under general or regional anaesthesia in normal operating room setting. However, when the surgery need to be performed in situations where there are limited resources and equipment, especially during a pandemic outbreak, in battlefields or area of disaster occurrence, the wide-awake local anaesthesia no tourniquet (WALANT) surgery can be utilised. This study aims to assess the efficacy of performing lower limb surgery using WALANT technique. A randomised cross-sectional study was designed to assess the effectiveness of WALANT in lower limb surgery, particularly in terms of duration of anaesthesia, Hamilton Anxiety Rating Scale (HAM-A), pain visual analogue scale (VAS), duration of surgery, amount of estimated blood loss (EBL) and total length of stay (LOS). A total of 91 patients requiring lower limb surgery were recruited, with only 83 patients completed the VAS pain assessment for all time points of the study. Mean age of patients was 52.1 ± 14.9 years. Mean VAS score were 1.19 ± 1.53 and 1.46 ± 1.86, preoperatively and intraoperatively. Mean VAS score were 0.55 ± 1.52, 0.60 ± 1.41, and 1.06 ± 1.69 at 2, 4, and 6 h post-surgery, respectively. Majority (79; 86.8%) of patient has preoperative anxiety score that was <17. Mean surgery duration was 65.28 ± 39.02 min, mean EBL was 91.34 ± 78.94 cc, whereas mean LOS was 3.35 ± 1.16 days. EBL was a weak predictor of postoperative pain. In conclusion, WALANT technique for lower limb surgery is effective and safe.
Introduction
Lower limb surgery is commonly done in general orthopaedic setting following various trauma or morbidities such as motor vehicle accident, assaults, fall, foot deformity and others. It is usually performed under general or regional anaesthesia. Apart from the inherent risks and costs associated with these anaesthetic techniques (1), it is usually difficult to perform these types of surgeries when there are limited resources and equipment available, especially during a pandemic outbreak such as COVID-19 where there is a shift of hospital resources to focus on pandemic management. Therefore, an alternative approach should be explored to improve these limitations. One of the surgical approaches which could improve the healthcare service is the wide-awake local anaesthesia no tourniquet (WALANT) surgery. WALANT refers to a type of surgery which involves surgeon-administered mixture of local anaesthetic for pain control and epinephrine for hemostasis and improved anaesthetic effect. Since no tourniquet, sedation or general anaesthesia are used for the surgery, the patient remains fully awake throughout the entire surgical procedure (2).
WALANT has been used in hand surgeries (3, 4) as well as procedures involving foot and ankle (1, 2). This anaesthetic technique has fewer risks and side effects compared to conventional sedation or general anaesthesia technique. For example, preoperative testing is often unnecessary and no anaesthetic staff or equipment are required. Since there is limited equipment needed, the technique can be used for ambulatory clinic where surgeries can be performed in any places. This is beneficial in certain settings such as in the battlefield and areas where disaster occurs. Besides, surgeon can communicate with the sober and coherent patient throughout perioperative period, providing the patient with greater insight into both the procedure and the recovery process (1).
Despite the benefits, the patient’s comfort and well-being have been the main concern for surgeons given the nature of WALANT surgery. As such, several studies had been done to assess patient experience with WALANT technique and the results were rather encouraging. For example, in a 2014 trial for WALANT in the lower limb surgery setting which involved the forefoot, hind foot and lower leg, the patients were assessed for their level of anxiety, pain and satisfaction intraoperatively. Results from the trial showed that peri- and post-operative pain and anxiety were significantly improved in patients who underwent WALANT surgery compared to the general anaesthesia group (1). Another different survey reported that the patients would choose WALANT technique if another operation was necessary and they would recommend the technique to a friend (5).
Although WALANT surgery is widely used in other countries, it is still uncommon in Malaysia. Since there is no available data published for WALANT lower limb surgery in the country, this study aims to assess the efficacy of performing lower limb surgeries (from knee region and distally) using the WALANT technique. The efficacy of the technique is assessed by studying the effectiveness of WALANT anaesthesia over the surgery, duration of action of the anaesthesia, duration of surgery performed, amount of estimated blood loss (EBL) during the surgery as well as the total length of stay (LOS) at the hospital after the surgery for the patients. This study would be the pioneer project in Malaysia and would contribute further in the emerging WALANT technique, especially in lower limb surgery.
Methods
Study design
This is a randomised cross-sectional study performed during the period of July 2020 to June 2021 in the General Operation Theatre (GOT), Emergency Department Operation Theatre (EDOT) of Daycare of Hospital Canselor Tuanku Mukhriz (HCTM), Pusat Perubatan Universiti Kebangsaan Malaysia (PPUKM). The study conformed to the Declaration of Helsinki and followed International Conference on Harmonization (ICH) – Good Clinical Practice (GCP) guidelines. Assessment of efficacy on WALANT surgery would be based on all subjects who completed the study.
Patient selection
Patients with lower limb surgeries, from knee and distally, who agreed to use the WALANT method, were included in the study. Patients with peripheral vascular disease (ankle brachial systolic index, ABSI <0.9 and >1.2), poorly controlled diabetes mellitus, ischaemic heart disease, polytrauma, injuries involving femur or above knee level were excluded from the study. Patients with lower limb infections or who had surgeries involving intramedullary devise such as nailing were also excluded. Besides, psychiatry patients like those with anxiety were also excluded from the study. Informed consent was obtained from all the patients before participating in the study.
Preparation and administration of WALANT solution
The WALANT solution consisted of 50 ml of lignocaine (1%) with 1:100,000 epinephrine. It was prepared by using 50 ml of normal saline (0.9%) and 50 ml of lignocaine (2%). 1:100,000 epinephrine was prepared by mixing 100 ml of the prepared solution with 1 ml of 1:1,000 epinephrine.
The toxicity of lignocaine is 7 mg/kg (6). Therefore, the maximum amount of WALANT solution to be administered in a patient had to be calculated based on the patient’s weight. For example, a patient weighs 70 kg can tolerate 490 mg of lignocaine (1%) (70 kg × 7 mg/kg). Since 1 ml of WALANT solution consisted of 10 mg of lignocaine (1%) with 1:100,000 epinephrine, the maximum amount of WALANT solution to be administered in the patient is 49 ml.
10 ml of sodium bicarbonate (8.4%) was added along with the WALANT solution to reduce pain during administration before the lower limb surgery begun. The solution was injected subdermally in perpendicular direction into area of surgery.
Other drugs such as phentolamine, terbutaline or phenoxybenzamine, which can reverse epinephrine vasoconstriction in human digits; and intraipid 20% solution, which can reverse lignocaine toxicity, should be prepared in the emergency trolley in case of any complication occur.
Data collection and analysis
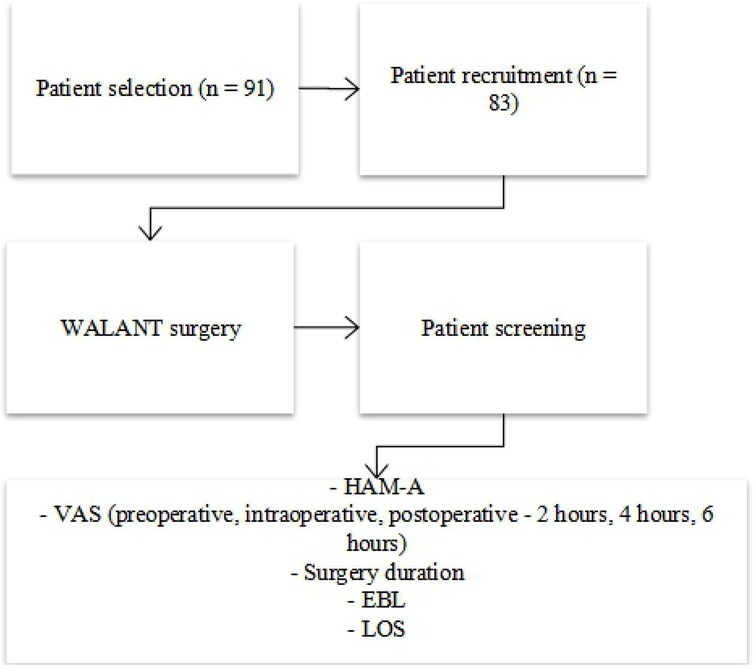
Various data including patients’ demographics, Hamilton Anxiety Rating Scale (HAM-A), pain visual analogue scale (VAS), duration of surgery in minutes, EBL during the surgery in cubic centimeters (cc) and total LOS in hospital (days) were recorded. The data were analysed using the Rasch Measurement Analysis Software version 4.4.5. Level of significance was set at p < 0.05 for every analysis. Figure 1 shows the flow chart of the study.
Results
Patient demographics
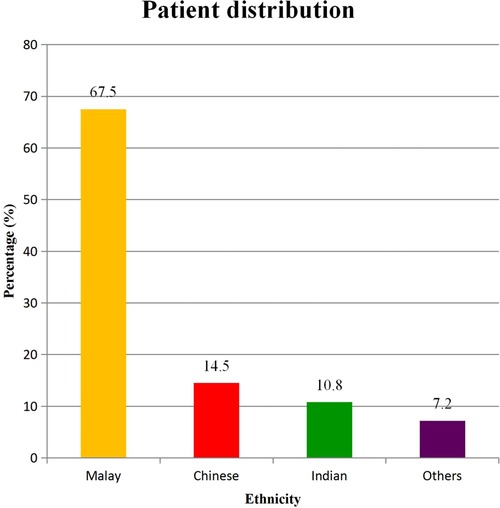
A total of 91 (34 males and 57 females) patients requiring lower limb surgery were recruited in this study. Only 83 (32 males and 51 females) patients completed the VAS pain assessment for all time points of the study with a mean age of 52.1 ± 14.9 years (Figure 1). Race distribution for these patients were 56 (67.5%) Malay, 12 (14.5%) Chinese, 9 (10.8%) Indian, and 6 (7.2%) other races (Figure 2).
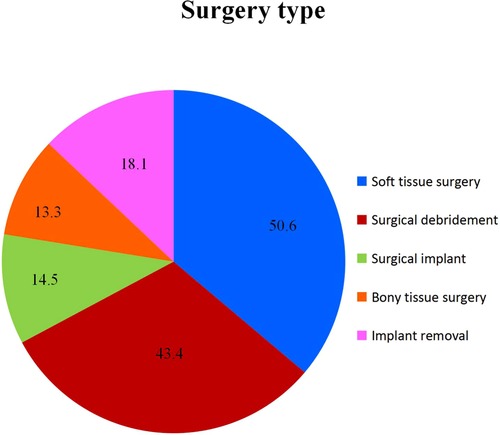
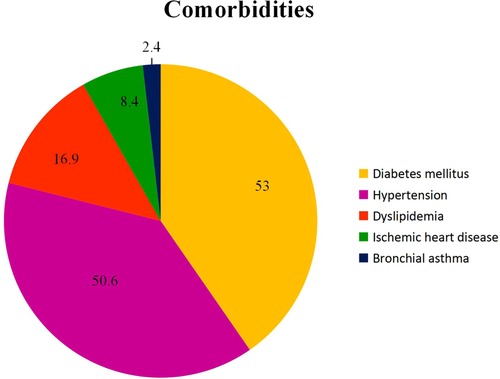
Out of the total 83 patients, 14.5% (12) patients required surgical implant, 43.4% (36) patients required surgical debridement of the wound, 50.6% (42) patients required soft tissue surgery, 13.3% (11) patients required bony tissue procedure and 18.1% (15) patients required removal of implant (Figure 3). In terms of comorbidities, 50.6% (42) patients had hypertension, 53.0% (44) patients had diabetes mellitus, 16.9% (14) patients had dyslipidemia, 8.4% (7) had ischemic heart disease, and 2.4% (2) had bronchial asthma (Figure 4). Additionally, the mean fasting blood sugar (FBS) and ABSI among the patients were known to be 7.5 ± 2.2 and 1.1 ± 0.2, respectively.
Pain assessment Pre-, intra- and post-surgery
Pain level was assessed before, during, and after WALANT surgery with VAS. The mean VAS score pre-surgery was 1.19 ± 1.53. Reasonably, pain was greater during surgery but remains at low level with the intra-surgery VAS score of 1.46 ± 1.86. The observed low level of pain was maintained after surgery with VAS score of 0.55 ± 1.52, 0.60 ± 1.41, and 1.06 ± 1.69 at 2, 4, and 6 h post-surgery, respectively. No statistically significant difference between the time points were observed.
Pre-surgical anxiety scale, duration of surgery, blood loss and length of stay at hospital
Other surgical outcome parameters measured to evaluate the effectiveness of WALANT surgery include preoperative anxiety, duration of surgery, blood loss, and LOS at hospital. Majority of 91.6% (76) of the patients scored less than 17 on the HAM-A scale depicting an overall low anxiety before the WALANT surgery. The mean time for the WALANT surgery from the incision to the wound closure was 65.28 ± 39.02 min. The mean estimated blood loss following WALANT surgery was 91.34 ± 78.94 cc. Finally, the mean LOS following WALANT surgery was 3.35 ± 1.16 days.
Predictors of post-surgical pain
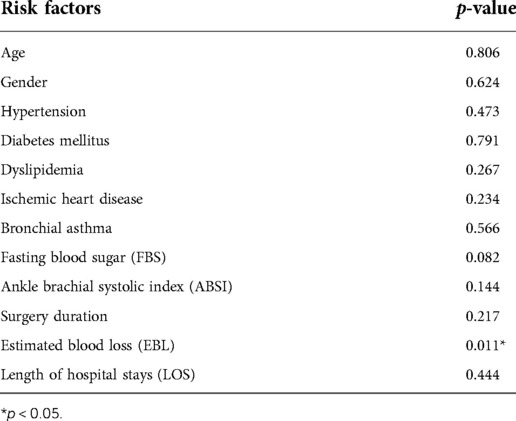
Linear regression analysis was performed to determine the independent predictors associated with pain after 6 h of WALANT surgery. Table 1 describes the association of each risk factor to the surgical pain outcome. Estimated blood loss was found to be correlated with the surgical pain outcome (p < 0.05). However, the multivariate regression analysis revealed that blood loss is not a strong predictor of surgical pain.
Discussion
Wide local anasthesia no torniquet technique has been extensively incorporated in upper limb surgery with a number of studies being published especially in the last decade. Compared to that, the usage of WALANT in lower limb operation requires more studies particularly in Malaysia. The surge of COVID-19 infection seems to be timely for the evaluation of WALANT effectiveness in lower limb surgeries due to the shift of resources towards pandemic management.
In various hand surgeries that applied WALANT technique (6–8), it was found that WALANT provides numerous practical benefits as compared to conventional anaesthesia techniques. It is with confidence stemming from the success of these surgeries that this study is conducted to look for equivalent advantages in lower limb operations.
In this study, the results showed a higher intra-surgery pain VAS score of 1.46 ± 1.86 than that of pre-surgery (1.19 ± 1.53). These scores, however, contradict with a previous WALANT study on foot and ankle surgery by MacNeill and Mayich, which reported a lower intra-surgery pain score of 0.75 ± 0.85 compared to preoperative score of 5.00 ± 3.11 (1). But, the pain scores remained stable and low before, during and even several hours after the surgery, as opposed to those recorded in MacNeill and Mayich, which was considerably higher before (5.00 ± 3.11) and after (5.21 ± 2.90) the surgery (1). The stable scores were in line with another WALANT study involving forefoot surgery by Wright et al., which also reported fairly stable scores ranging from 1.65 ± 1.99 (preoperative), 0.17 ± 0.32 (intraoperative) to 0.45 ± 1.10 (postoperative) (2).
Several studies have shown low anxiety in patients undergoing different types of lower limb surgeries. For example, Bilgetekin et al. reported a median VAS anxiety (VAS-A) score of 1 for the use of WALANT foot and ankle surgery resulting from medial malleolus fracture, lateral malleolus fracture, Achilles tendon rupture, proximal phalangeal fracture, Lisfranc injury, syndesmotic injury, deltoid ligament injury and fifth metatarsal fracture (7). Another study reported significantly lower anxiety for patients who received WALANT forefoot surgery (3.20 ± 3.02) compared to patients who received general anaesthesia treatment (2.98 ± 3.21). For the group that received WALANT treatment, the anxiety score decreased considerably from pre-surgery period (3.20 ± 3.02) to post-surgery period (0.08 ± 0.34) (2). Consistent with previous studies, results from this study also reported an overall low anxiety (<17 on HAM-A scale) in the patients before WALANT surgery.
An open reduction and internal fixation surgery of ankle fractures using WALANT technique reported a mean operation time of 59.72 ± 7.19 min (8), which is approximately the same as the duration recorded in this current study (65.28 ± 39.02 min). Another similar study involving ankle operation reported a shorter mean surgery duration of 36.6 ± 7 min (7). The shorter operation time may be due to the simplicity of the ankle surgical procedures performed as opposed to the more complicated procedures performed in this study, including soft tissue surgery, surgical debridement of wound, surgical implantation and removal of implant.
The mean EBL recorded in the current study was 91.34 ± 78.94 cc, which is higher compared to the average amount of blood loss recorded (29.40 ± 7.38 ml) in an ankle fracture fixation surgery using the same WALANT technique (8). This is probably due to the majority of patients (50.6%) in this study underwent soft tissue surgery, which may lead to more blood loss compared to procedures involving ankle fracture fixation. Although the mean amount of blood loss recorded in this study is rather high, it is significantly lower when compared to other lower limb surgery using conventional anaesthesia techniques. For example, transtibial amputation using tourniquet was reported to have caused a median intraoperative blood loss of 200 ml (interquartile range = 100–300 ml) and a median total blood loss of 737 ml (interquartile range = 331–1218) from Day 0 to Day 4 after the surgery (9). Even a less complicated surgery like total knee replacement would cause a mean total blood loss of about 1.0–1.5 liter when general anaesthesia with tourniquet is used (10).
The mean LOS following WALANT surgery recorded in this study was 3.35 ± 1.16 days. This value is longer compared to other studies using the similar WALANT technique. For instance, a study indicated that patients who underwent ankle fracture surgery only spent an average LOS of 8.3 ± 6.1 h at the hospital on the day of surgery before they were discharged (7). Another similar study involving forefoot surgery reported a shorter LOS (3.60 ± 1.23 h) at the hospital (2). This, again, may be due to the simplicity of the surgeries performed in the two studies, unlike those complicated ones performed in the current study that may require longer time for the wounds to heal. Nonetheless, the mean LOS for the current study is considerably shorter in comparison with lower extremity amputation using conventional anaesthesia, which may lead to months of hospitalization because of serious postoperative complications.
Meanwhile, the association of independent predictors with postoperative pain was determined through linear regression analysis. Results published by multiple studies indicated that age, gender, comorbidities such as diabetes mellitus (11, 12) and duration of surgery (13) are risk factors for higher incidence of post-surgical pain. However, results from this study showed that age, gender, surgery duration and comorbidities including hypertension, diabetes mellitus, dyslipidemia, ischemic heart disease and bronchial asthma did not correlate with post-surgical pain. Blood sugar level (14) and ABSI (15) were found to be associated with several postoperative complications such as poor wound healing and post-surgical cardiovascular events. But, linear regression analysis did not show any relation between the two variables and postoperative pain. Next, longer hospital stay is often associated with a higher incidence of postoperative complications including pain and delayed wound healing, especially in lower extremity amputation. However, in this study, the p-value from linear regression analysis showed no correlation between LOS and post-surgical pain. Although EBL was the only variable found to be correlated with post-surgical pain, it was not a strong predictor as indicated through multivariate regression analysis. Therefore, it cannot be used as a reliable predictor of postoperative pain in patients undergoing lower limb surgery.
The experiment yields an overall satisfying result in regards to the safety and effectiveness of WALANT technique application in lower limb surgery, as demonstrated by previous studies (16–18). The low and stable pain VAS score, especially hours after the surgery, proves the effectiveness of WALANT anaesthesia solution in pain management during and after the lower limb surgery. Besides, the overall low anxiety score before WALANT surgery also shows that the patients are generally quite tolerant of this type of wide-awake surgery. This enables WALANT surgery to be practised more widely in different lower limb surgical procedures.
Furthermore, the short duration of surgery, low amount of blood loss and LOS in hospital enable WALANT surgery to be carried out in places where there are limited healthcare resources and equipment. Short duration of surgery is an important criterion for the application of WALANT technique in battlefields or area of disaster occurence, where certain surgery needed to perform over a short period of time with limited resources in order to save lives. Next, low amount of blood loss during operation means no or limited blood transfusion is required. This is favourable when surgeries are performed outside of operating rooms without appropriate equipment or resources. Finally, short LOS poses another added advantage for WALANT surgery, especially during times of limited intensive care unit or operating room resources when there is a pandemic like COVID-19. More beds and ventilators can therefore be allocated to patients who are truly in need.
Nonetheless, this study has several limitations. One of which is small sample size. Only 39 patients completed the VAS pain assessment for all time points despite a total of 81 patients recruited in this study. According to the sample size and item calibration or person measure stability of Rasch Model, a minimum of 50 subjects are needed to achieve a 99% confidence interval (CI) in an experiment (19). Hence, it is recommended for the experiment to be conducted on a larger sample size so that a 99% of CI can be achieved on each parameter, thus validating the data. Perhaps, with the increase of sample size and data, predictors of post-surgical pain can be determined. The next limitation is lack of pain and anxiety assessment. Pain assessment should be done during anaesthesia injection and over the period of days after the surgery to allow investigation of the efficacy of WALANT technique over a longer period of time. Anxiety assessment should also be conducted intra- and post-operatively to better monitor the emotional changes in patients.
Conclusion
WALANT technique for lower limb surgery is as effective as for upper limb surgery, as indicated by low and stable pain VAS score, low preoperative anxiety score on HAM-A, short surgery duration, low amount of estimated blood loss and short LOS at hospital. Age, gender, comorbidities (hypertension, diabetes mellitus, dyslipidemia, ischemic heart disease and bronchial asthma), FBS, ABSI, surgery duration and LOS are not predictors of post-surgical pain while EBL is a weak predictor. Further studies with larger sample size and more parameters included should be conducted to evaluate the safety and efficacy of WALANT technique application in lower limb surgery.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Faculty Medicine of Universiti Kebangsaan Malaysia. The patients/participants provided their written informed consent to participate in this study.
Author contributions
Study design: MYB, NSS, NLM and NAA. Drafting of study protocol: MYB, NSS, NLM and NAA. Statistical analysis and interpretation of results: MYB, NSS, NLM and NAA. Drafting of the initial manuscript: MYB, NSS, NLM, NAA, AF. Revision and editing of the manuscript: MYB, NSS, NLM, NAA and AF. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. MacNeill AL, Mayich DJ. Wide-awake foot and ankle surgery: a retrospective analysis. Foot Ankle Surg. (2017) 23:307–10. doi: 10.1016/j.fas.2016.09.004
2. Wright J, MacNeill AL, Mayich DJ. A prospective comparison of wide-awake local anesthesia and general anesthesia for forefoot surgery. Foot Ankle Surg. (2017) 25:211–4. doi: 10.1016/j.fas.2017.10.015
3. Lalonde DH, Martin AL. Wide-awake flexor tendon repair and early tendon mobilization in zones 1 and 2. Hand Clin. (2013) 29:207–13. doi: 10.1016/j.hcl.2013.02.009
4. Higgins A, Lalonde DH, Bell M, McKee D, Lalonde JF. Avoiding flexor tendon repair rupture with intraoperative total active movement examination. Plast Reconstr Surg. (2010) 126:941–5. doi: 10.1097/PRS.0b013e3181e60489
5. Teo I, Lam W, Muthayya P, Steele K, Alexander S, Miller G. Patients’ perspective of wide-awake hand surgery - 100 consecutive cases. J Hand Surg Eur. (2013) 38:992–9. doi: 10.1177/1753193412475241
6. Feldman G, Orbach H, Rinat B, Rozen N, Rubin G. Internal fixation of metacarpal fractures using wide awake local anesthesia and no tourniquet. Hand Surg Rehabil. (2020) 39(3):214–7. doi: 10.1016/j.hansur.2020.01.003
7. Orbach H, Rozen N, Rubin G. Open reduction and internal fixation of intra-articular distal radius fractures under wide-awake local anesthesia with no tourniquet. J Int Med Res. (2018) 46(10):4269–76. doi: 10.1177/0300060518793036
8. Fulchignoni C, Bonetti MA, Rovere G, Ziranu A, Maccauro G, Pataia E. Wide awake surgery for flexor tendon primary repair: a literature review. Orthop Rev. (2020) 12(Suppl 1):61–3. doi: 10.4081/or.2020.8668
9. Lalonde D, Eaton C, Amadio P, Jupiter J. Wide-awake hand and wrist surgery: a new horizon in outpatient surgery. Instr Course Lect. (2015) 64:249–59.25745911
10. Bilgetekin YG, Kuzucu Y, Öztürk A, Yüksel S, Atilla HA, Ersan Ö. The use of the wide-awake local anesthesia no tourniquet technique in foot and ankle injuries. Foot Ankle Surg. (2010) 27:535–8. doi: 10.1016/j.fas.2020.07.002
11. Wied C, Tengberg PT, Holm G, Kallemose T, Foss NB, Troelsen A, et al. Tourniquets do not increase the total blood loss or reamputation risk in transtibial amputations. World J Orthop. (2017) 8:62–7. doi: 10.5312/wjo.v8.i1.62
12. Magill P, Cunningham EL, Hill JC, Beverland DE. Identifying the period of greatest blood loss after lower limb arthroplasty. Arthroplast Today. (2018) 4:499–504. doi: 10.1016/j.artd.2018.09.002
13. Kurichi JE, Vogel WB, Kwong PL, Xie D, Bates BE, Stineman MG. Factors associated with total inpatient costs and length of stay during surgical hospitalization among veterans who underwent lower extremity amputation. Am J Phys Med Rehabil. (2013) 92:203–14. doi: 10.1097/PHM.0b013e31827446eb
14. Hernández C, Díaz-Heredia J, Berraquero ML, Crespo P, Loza E, Ruiz Ibán MÁ. Pre-operative predictive factors of post-operative pain in patients with hip or knee arthroplasty: a systematic review. Reumatol Clínica (Engl Ed). (2015) 11:361–80. doi: 10.1016/j.reumae.2014.12.011
15. Lewis GN, Rice DA, McNair PJ, Kluger M. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth. (2015) 114:551–61. doi: 10.1093/bja/aeu441
16. Peters ML, Sommer M, De Rijke JM, Kessels F, Heineman E, Patijn J, et al. Somatic and psychologic predictors of long-term unfavorable outcome after surgical intervention. Ann Surg. (2007) 245:487–94. doi: 10.1097/01.sla.0000245495.79781.65
17. Ye Y, Pan B, Gu M, et al. Fluctuation of fasting blood glucose in patients who underwent primary or revision total joint arthroplasty: a retrospective review. J Orthop Surg Res. (2020) 15:508. doi: 10.1186/s13018-020-02029-2
18. Ko SH, Bandyk DF. Interpretation and significance of ankle-brachial systolic pressure index. Semin Vasc Surg. (2013) 26:86–94. doi: 10.1053/j.semvascsurg.2014.01.002
Keywords: WALANT, local anaesthesia, ambulatory surgery, pain, satisfaction
Citation: Bajuri MY, Saidfudin NS, Mazli N, Azriq N and Azemi AF (2022) Safety of wide-awake local anesthesia with no tourniquet (WALANT) in for lower limb surgery: A potential alternative in times of emergency. Front. Surg. 9:848422. doi: 10.3389/fsurg.2022.848422
Received: 4 January 2022; Accepted: 12 August 2022;
Published: 9 September 2022.
Edited by:
I-Shiang Tzeng, National Taipei University, TaiwanReviewed by:
Guy Rubin, Ha'Emek Medical Center, IsraelGiuseppe Rovere, Agostino Gemelli University Polyclinic (IRCCS), Italy
© 2022 Bajuri, Saidfudin, Mazli, Azriq and Azemi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohd Yazid Bajuri ZXplZHMwMDdAeWFob28uY29tLm15
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Abbreviations WALANT, wide-awake local anesthesia with no tourniquet; HAM-A, hamilton anxiety rating scale; VAS, visual analogue scale; EBL, amount of estimated blood loss; LOS, length of stay; GOT, general operation theatre; EDOT, emergency department operation theatre; HCTM, hospital canselor tuanku mukhriz; PPUKM, pusat perubatan universiti kebangsaan malaysia; ICH, international conference on harmonization; GCP, good clinical practice; ABSI, ankle brachial systolic index; cc, cubic centimeters; FBS, fasting blood sugar
 Mohd Yazid Bajuri
Mohd Yazid Bajuri Nur Sai’dah Saidfudin
Nur Sai’dah Saidfudin Norliyana Mazli
Norliyana Mazli Nik Alif Azriq
Nik Alif Azriq