
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg. , 24 February 2022
Sec. Pediatric Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.835235
This article is part of the Research Topic Current Advances in Pediatric Surgery View all 32 articles
Background: Pediatric rectal prolapse is a common issue in clinical practice. Among various managements, sclerotherapy is an important method to successfully treat pediatric rectal prolapse, especially for the first injection. The knowledge of the first injection of sclerotherapy can be revealed by a systemic review and meta-analysis of randomized clinical trials.
Methods: We performed a systematic search and a meta-analysis for the retrospective clinical studies of sclerotherapy in pediatric rectal prolapse. The comparison between remission and recurrence after the first injection of sclerotherapy was performed to find if the first injection of sclerotherapy can treat rectal prolapse completely. After a restricted selection, 17 studies involving 1,091 pediatric rectal prolapse subjects with sclerotherapy were enrolled in a variety of classifications of injection agents. The focused outcome was to check whether the first injection of sclerotherapy can achieve a remission status. The meta-analysis was performed by Review Manager 5.4.
Results: Among the subjects receiving sclerotherapy, the meta-analysis favors the remission status after receiving the first injection of sclerotherapy. The meta-analysis results showed significant remission tests for the overall effect and significant heterogeneities in odds ratio and the fixed-effects model. The significant therapeutic effects remained, however, even after testing in the relative risk and the random-effects model.
Conclusions: Despite significant heterogeneity and relatively low quality of evidence, the first injection of sclerotherapy may conceivably demonstrate therapeutic effects to help the patients of pediatric rectal prolapse achieve a remission status.
Pediatric rectal prolapse is a significant issue in clinical practice. The weak pelvic musculature might predispose the children to such disease. In addition, the loose attachment of rectal mucosa to the muscularis will contribute to rectal prolapse (1). Most patients of pediatric rectal prolapse belong to the mucosal subtype, which is related to straining due to constipation during the toilet training process in children. Pediatric rectal prolapse in older children might be related to congenital neuromuscular abnormalities, autism or developmental delay, and anorectal malformations (2, 3).
The incidence rate of pediatric rectal prolapse was still not clear (4, 5). Spontaneous resolution would be around 60–90% in pediatric rectal prolapse. Compared to pediatric rectal prolapse, rectal prolapse in adults was rarely spontaneously resolving (2). Despite the high rate of spontaneous resolution, pediatric patients with rectal prolapse will suffer much if the condition will not spontaneously resolve. Therefore it is still necessary to receive the management if there is no spontaneous resolution. Before the ultimate choice of operation (6, 7), sclerotherapy would be an important procedure to relieve the pediatric prolapse (3, 5, 8–11). Therefore, it is important for us to understand the intermediate choice (sclerotherapy) between operation and conservative treatment. In this study, we planned to enroll the related articles of sclerotherapy in pediatric rectal prolapse. We wanted to confirm the remission effects of the first injection of sclerotherapy in pediatric rectal prolapse in the study design of systematic review and meta-analysis. We hypothesized that the first injection of sclerotherapy would favor remission rather than recurrence (no remission after the first injection of sclerotherapy and necessary subsequent injection of sclerotherapy).
We used the following keywords: “rectal” or “rectum” or “prolapse” or “children” or “pediatric” or “sclerotherapy” and “rectal prolapse” to search and to collect the related articles in the PubMed, ScienceDirect, Embase, Web of Science, and Scopus databases. The articles were limited to those published or e-published online before December 2021.
The inclusion criteria of this study were as follows: (1) Sclerotherapy treatment for pediatric patients with rectal prolapse; (2) The studies with sclerotherapy outcome and related clinical profiles; (3) The studies with detailed data of sclerotherapy and pediatric rectal prolapse; (4) These studies were also published in English language in the journals of science citation index database; and (5) Retrospective or prospective study. The exclusion criteria were the following: (1) Some parts of detailed data were unavailable in the content of the articles (unavailable even after inquiring the corresponding authors about the data needed for this meta-analysis); (2) The authors did not respond or could not have access to the dataset, in which case the articles would be excluded as the category without detailed data; (3) The studies that do not belong to patients with rectal prolapse or sclerotherapy; and (4) Review articles.
The study was conducted according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (23). The risk of bias for each study was assessed by the random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting. We extracted the following data from the eligible articles. First, the success rate and patient number of the first injection of sclerotherapy in pediatric patients with rectal prolapse were gathered. Second, the remission rate and patient number under the first injection of sclerotherapy were collected. Third, the recurrence and patient number of the first injection of sclerotherapy in pediatric patients with rectal prolapse were gathered. Fourth, the probable side effects of sclerotherapy in pediatric patients with rectal prolapse was noted.
WZ reviewed the abstracts to screen the articles. WZ and YS performed the extraction of clinical outcome data from the text, tables, and figures of the enrolled articles independently. The enrolled articles had the clinical outcome data in the text, tables, figures, or supplementary material. Then, a collaborative review was performed to resolve any discrepancies. All authors participated to review the final results.
The odds ratio (OR) with 95% CI (a summary statistic) was obtained by the Mantel–Haenszel method for dichotomous variables. Chi-square tests were used to study heterogeneity between the enrolled studies. The derived I2 statistic was used to estimate the statistical heterogeneity of studies included in the meta-analysis. The I2 statistic was used to estimate the percentage of the total variation across studies due to heterogeneity rather than chance. The I2 values of 25, 50, and 75% represented low, medium, and high heterogeneity, respectively. If the heterogeneity is high, the random-effects model will be used for the analysis and the fixed-effects model will be used for studies with low or moderate heterogeneity. Subgroup analyses were not possible due to the lack of patient-level data. All P values were two-sided. All statistical analyses were conducted with Review Manager Version 5.4 (The Cochrane Collaboration, London).
The initial literature search through the dataset found 124 articles and the additional records from other sources were 14 articles. Then, 55 duplicates were removed and the residual 83 articles were screened according to the relevance of abstracts and titles. Of that, 40 articles were discarded after this step. Full-text contents of the remaining 43 articles were assessed for eligibility. Then, 27 articles were excluded due to review articles, not nurse-led studies, not randomized trials, and not perioperative setting. The qualitative analysis of these 16 articles was performed and no articles were excluded. Therefore, only 16 studies were included in this meta-analysis (1, 4, 5, 10–22). The flow diagram was presented according to the PRISMA guideline (Figure 1). The detailed characteristics of the 16 studies were also summarized in Table 1.
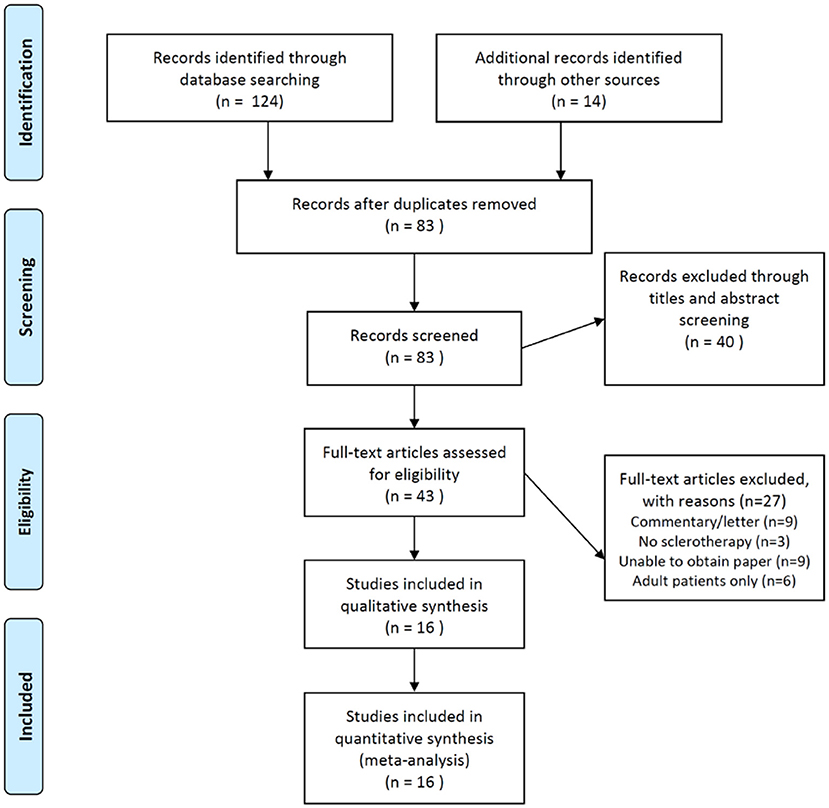
Figure 1. The preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram of the current meta-analysis. The current meta-analysis followed the PRISMA guideline to identify the potentially relevant literature and to screen the identified literature using the abstract and title selection. The full text of screened literature was assessed to find the eligible studies and to include the suitable ones for the final meta-analysis.
The I2 was 95% CI, which revealed high heterogeneity. Therefore, the random-effects model was applied. The test for the overall effect was Z = 5.07 (p < 0.00001) and the meta-analysis results favored remission after the first injection of sclerotherapy in pediatric patients of rectal prolapse (Figure 2). However, the range of 95% CI of several studies included “1” (5, 15, 20). One study revealed the tendency to favor recurrence (13).
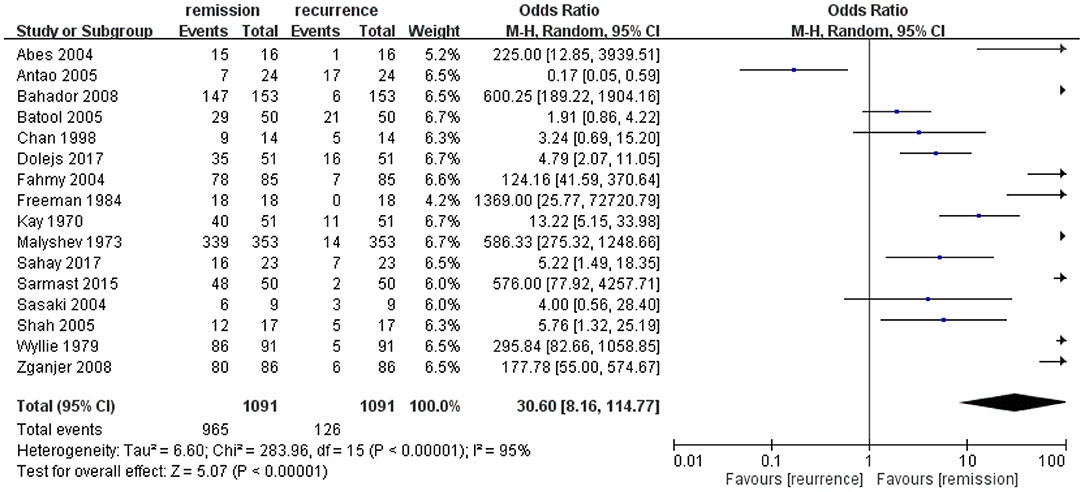
Figure 2. The odds ratio of remission vs. recurrence for the first injection of sclerotherapy in the enrolled studies of pediatric rectal prolapse. The first injection of sclerotherapy showed a favorable result toward remission rather than recurrence. The heterogeneity was high and the result was statistically significant.
In the current meta-analysis, the results showed that the first injection of sclerotherapy might have a higher OR to help the pediatric patients with rectal prolapse achieve a remission status. However, the high heterogeneity and the 95% CI of several studies that included an OR of 1 might bias our findings. In a previously published review (24), they focused on the success rate of a single injection (77%), overall complication rate (14%), and the significant difference between different sclerosing agents (no significant differences). Based on their findings, our meta-analysis enrolled all kinds of sclerosing agents in the first injection of sclerotherapy, which should not have a bias from the different sclerosing agents. Our study also supported that there was a high OR of remission after the first injection of sclerotherapy on the pediatric rectal prolapse. Our results suggested that the first injection of sclerotherapy should play a crucial role in the treatment of pediatric patients with rectal prolapse.
In clinical practice, the management for pediatric rectal prolapse has yet to reach a consensus. There are over 100 surgical procedures in the field of rectal prolapse (25). The majority of infants and children can be spontaneously resolved without an aggressive management. Some patients can resolve after conservative management, such as medical treatment for constipation. However, a subgroup of patients might need aggressive intervention due to persistent symptoms or the lack of spontaneous resolve (2). Therefore, when the clinicians make a clinical judgment, that is, whether they want to take a more aggressive management, sclerotherapy might be an intermediate choice between conservative treatment and surgery.
However, due to the high probability of spontaneous resolution (60–90%) of pediatric rectal prolapse (2), we can observe that it is difficult to enroll a high number of patients for the sclerotherapy, except the studies of Bahador et al. (14) and Malyshev et al. (17). Therefore, the meta-analysis results might be influenced by the two relatively big studies in patient numbers. In addition, the lack of standardization of sclerosing agents, the number, and the location of injections also contributed to the difficulty to standardize the treatment procedures of sclerotherapy. The proportion of patients who would experience a resolution of rectal prolapse with non-operative management remains unknown, even with a recent meta-analysis with such data (24). Another review article showed that the success rate of sclerotherapy in pediatric rectal prolapse was 79.5% (25), which was similar to the meta-analytic data of Hintz et al. (24). However, the review article just used a systematic review strategy to conclude the success rate of sclerotherapy. Therefore, we still need more data to confirm the remission effects of the first injection of sclerotherapy in pediatric rectal prolapse.
There were several limitations in the current study. First, the high heterogeneity and the relatively poor quality of data might bias our findings. Even if the random-effect model can adjust such bias, the influences for our study results were still significant. Second, the lack of demographic data for the “real subgroup” of sclerotherapy in most enrolled studies might limit our ability to analyze the subgroup differences. The lack of demographic data was because we focused on sclerotherapy for pediatric rectal prolapse. However, not all enrolled studies would provide the demographic data “purely” for “sclerotherapy for rectal prolapse,” which is the reason for the lack of some demographic data in Table 1. Third, the lack of a detailed information on subgroups was also an obstacle in performing the subgroup analysis. Fourth, the different kinds of sclerosing agents were included in the current study, which might bias our interpretations. However, the meta-analysis of Hintz et al. suggested that there was no significant difference in the treatment effects between different sclerosing agents (24). Fifth, all the enrolled studies had a retrospective design, which would also influence our meta-analysis results. The references we searched also revealed that the published studies were all retrospective, probably due to the characteristics of the clinical practice of pediatric rectal prolapse, and it might be difficult to enroll such patients in a design of randomized clinical trials or double-blinded trials. Further studies of randomized trials might be warranted to confirm the treatment and remission effects of the first injection of sclerotherapy.
Despite significant heterogeneity and a relatively low quality of evidence, the first injection of sclerotherapy might demonstrate the therapeutic effects to help the patients of pediatric rectal prolapse achieve remission status. However, more randomized trials with more standardization of sclerotherapy procedures will be warranted in the future to confirm the remission effects of the first injection of sclerotherapy in pediatric rectal prolapse.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
WZ reviewed the abstracts to screen the articles. WZ and YS performed the extraction of clinical outcome data from text, tables, and figures of the enrolled articles independently. MZ checked the manuscript and gave instructions. LL provided the idea of the study design and gave instructions. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
2. Saadai P, Trappey AF, Langer JL. Surgical management of rectal prolapse in infants and children. Eur J Pediatr Surg. (2020) 30:401–5. doi: 10.1055/s-0040-1716725
3. Corman ML. Rectal prolapse in children. Dis Colon Rectum. (1985) 28:535–9. doi: 10.1007/BF02554107
4. Dolejs SC, Sheplock J, Vandewalle RJ, Landman MP, Rescorla FJ. Sclerotherapy for the management of rectal prolapse in children. J Pediatr Surg. (2017). doi: 10.1016/j.jpedsurg.2017.10.015
5. Chan WK, Kay SM, Laberge JM, Gallucci JG, Bensoussan AL, Yazbeck S. Injection sclerotherapy in the treatment of rectal prolapse in infants and children. J Pediatr Surg. (1998) 33:255–8. doi: 10.1016/S0022-3468(98)90441-9
6. Puri B. Rectal prolapse in children: laparoscopic suture rectopexy is a suitable alternative. J Indian Assoc Pediatr Surg. (2010) 15:47–9. doi: 10.4103/0971-9261.70634
7. Laituri CA, Garey CL, Fraser JD, Aguayo P, Ostlie DJ, St Peter SD, et al. 15-Year experience in the treatment of rectal prolapse in children. J Pediatr Surg. (2010) 45:1607–9. doi: 10.1016/j.jpedsurg.2010.01.012
8. Chew SS, Marshall L, Kalish L, Tham J, Grieve DA, Douglas PR, et al. Short-term and long-term results of combined sclerotherapy and rubber band ligation of hemorrhoids and mucosal prolapse. Dis Colon Rectum. (2003) 46:1232–7. doi: 10.1007/s10350-004-6720-0
9. Qvist N, Rasmussen L, Klaaborg KE, Hansen LP, Pedersen SA. Rectal prolapse in infancy: conservative versus operative treatment. J Pediatr Surg. (1986) 21:887–8. doi: 10.1016/S0022-3468(86)80015-X
10. Wyllie GG. The injection treatment of rectal prolapse. J Pediatr Surg. (1979) 14:62–4. doi: 10.1016/S0022-3468(79)80578-3
11. Kay NR, Zachary RB. The treatment of rectal prolapse in children with injections of 30 per cent saline solutions. J Pediatr Surg. (1970) 5:334–7. doi: 10.1016/0022-3468(70)90190-9
12. Abes M, Sarihan H. Injection sclerotherapy of rectal prolapse in children with 15 percent saline solution. Eur J Pediatr Surg. (2004) 14:100–2. doi: 10.1055/s-2004-815855
13. Antao B, Bradley V, Roberts JP, Shawis R. Management of rectal prolapse in children. Dis Colon Rectum. (2005) 48:1620–5. doi: 10.1007/s10350-005-0074-0
14. Bahador A, Foroutan HR, Hosseini SM, Davani SZ. Effect of submucosal alcohol injection on prolonged rectal prolapse in infants and children. J Indian Assoc Pediatr Surg. (2008) 13:11–3. doi: 10.4103/0971-9261.42566
15. Batool T, Akhtar J, Ahmed S. Management of idiopathic rectal prolapse in children. J Coll Physicians Surg Pak. (2005) 15:628–30.
16. Fahmy MA, Ezzelarab S. Outcome of submucosal injection of different sclerosing materials for rectal prolapse in children. Pediatr Surg Int. (2004) 20:353–6. doi: 10.1007/s00383-004-1197-4
17. Malyshev YI, Gulin VA. Our experience with the treatment of rectal prolapse in infants and children. Am J Proctol. (1973) 24:470–2.
18. Sahay R, Murthi G, Lindley R. Outcomes following sclerotherapy for mucosal rectal prolapse with oily phenol injection: single-centre review. Pediatr Surg Int. (2017) 33:363–5. doi: 10.1007/s00383-016-4035-6
19. Sarmast MH, Askarpour S, Peyvasteh M, Javaherizadeh H, Mooghehi-Nezhad M. Rectal prolapse in children: a study of 71 cases. Przeglad gastroenterologiczny. (2015) 10:105–7. doi: 10.5114/pg.2015.49003
20. Sasaki Y, Iwai N, Kimura O, Hibi M. The treatment of rectal prolapse in children with phenol in almond oil injection. Eur J Pediatr Surg. (2004) 14:414–7. doi: 10.1055/s-2004-821151
21. Shah A, Parikh D, Jawaheer G, Gornall P. Persistent rectal prolapse in children: sclerotherapy and surgical management. Pediatr Surg Int. (2005) 21:270–3. doi: 10.1007/s00383-005-1384-y
22. Zganjer M, Cizmic A, Cigit I, Zupancic B, Bumci I, Popovic L, et al. Treatment of rectal prolapse in children with cow milk injection sclerotherapy: 30-year experience. World J Gastroenterol. (2008) 14:737–40. doi: 10.3748/wjg.14.737
23. Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg. (2011) 39:91–2. doi: 10.1016/j.jcms.2010.11.001
24. Hintz GC, Zou VZ, Baird R. Sclerotherapy for rectal prolapse in children: a systematic review and meta-analysis. J Pediatr Surg. (2019) 54:1083–8. doi: 10.1016/j.jpedsurg.2019.01.033
Keywords: pediatric, rectal prolapse, sclerotherapy, first injection, remission, meta-analysis
Citation: Zhou W, Shi Y, Zhang M and Li L (2022) The Remission Effects of First Injection of Sclerotherapy for Pediatric Rectal Prolapse: A Systematic Review and Meta-Analysis. Front. Surg. 9:835235. doi: 10.3389/fsurg.2022.835235
Received: 14 December 2021; Accepted: 18 January 2022;
Published: 24 February 2022.
Edited by:
Gunadi, Gadjah Mada University, IndonesiaReviewed by:
Simmi K. Ratan, University of Delhi, IndiaCopyright © 2022 Zhou, Shi, Zhang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Li, bGlsaTAzNjZAc2luYS5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.