
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 28 March 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.821509
This article is part of the Research TopicAnastomotic and Intestinal Wound Healing: Recent advances and future directionsView all 11 articles
Introduction: Protective loop-ileostomy is one of the most common interventions in abdominal surgery to provide an alternative intestinal outlet until sufficient healing of a distal anastomosis has occurred. However, closure of a loop-ileostomy is also associated with complications. Thus, knowledge of the optimal time interval between primary and secondary surgery is crucial.
Methods: Data from 409 patients were retrospectively analyzed regarding complications and risk factors in closure-associated morbidity and mortality. A modified Clavien-Dindo classification of surgical complications was used to evaluate the severity of complications.
Results: A total of 96 (23.5%) patients suffered from postoperative complications after the closure of the loop-ileostomy. Early closure within 150 days from enterostomy (n = 229) was associated with less complications (p < 0.001**). Looking at the severity of complications, there were significantly more (p = 0.014*) mild postoperative complications in the late closure group (>150 days). Dysfunctional digestive problems—either (sub-) ileus (p = 0.004*), diarrhea or stool incontinence (p = 0.003*)—were the most frequent complications associated with late closure. Finally, we could validate in a multivariate analysis that “time to closure” (p = 0.002*) is independently associated with the development of complications after closure of a protective loop-ileostomy.
Conclusion: Late closure (>150 days) of a loop-ileostomy is an independent risk factor in post-closure complications in a multivariate analysis. Nevertheless, circumstances of disease and therapy need to be considered when scheduling the closure procedure.
Installation of an artificial bowel output (enterostomy) to circumvent an intestinal obstruction can be traced back to ancient times with first records of a surgical ileostomy, ranging back to 1879 (1). Today, many oncologic and non-oncologic diseases involving intra-abdominal organs demand the installation of an enterostomy during disease owed to complications, such as perforation, obstruction, compression, or infection of the intestine (1–3). Protective (loop-) ileostomy is one of the most common interventions in abdominal surgery to provide—in conjunction with the attached stoma appliance—an alternative intestinal outlet (2).
Procedures of surgical enterostomy are principally reversible, and, especially, a protective loop-ileostomy is generally intended to be only temporary until sufficient healing of a distal anastomosis has occurred (2). However, not only the feasibility of stoma closure but also the timing is a relevant question that is a decisive factor influencing patient-related physical and psychological outcomes (4, 5). Until recently, abdominal surgeons have widely agreed upon a temporizing strategy when confronted with a decision toward or against early closure of a protective loop-ileostomy (6–8). However, current literature suggests that a belated closure of a protective loop-ileostomy—even though lacking a consistent and consensual critical cut-off—might be associated with higher morbidity and mortality, thus, suggesting some prognostic risk factors in post-closure complications (2–5, 9–12). In our hospital, we aim to perform the stoma reversal procedure within 3–6 months.
Because of the inconsistent and yet sparsely conducted research, this study wants to validate those recent observations and aims at confining the optimal time interval to ameliorate adverse outcomes after the closure of protective loop-ileostomy.
In a retrospective analysis, 409 patients with the closure of a protective loop-ileostomy—as the only inclusion criterion—at the University of Regensburg medical center were included. The time of primary surgery covered a period from January 2000 to August 2012. Patient demographics, primary diagnosis, and indication for enterostomy as well as details of the circumstances of enterostomy creation and the primary surgery, and stoma-related complications during and after a hospital stay, as well as information about ileostomy closure and follow-up care, were recorded by means of a hospital-internal questionnaire.
The widely approved Clavien-Dindo classification of surgical complications was applied for the ranking of adverse perioperative outcomes (13, 14). Grade I represents mild complications and comprises any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic, or radiological interventions. The present modification condensed Clavien-Dindo Grades II and III to the new category moderate complications that summarize those unwanted events that indicate any further intervention. Severe complications (Clavien-Dindo Grade IV) contain life-threatening conditions requiring ICU management and/or re-operation. Lethal outcomes correspond to Clavien-Dindo Grade V. Complication rates were operationalized as a proportion of patients with at least one adverse sequelae of the respective population.
Statistical analysis was conducted with IBM SPSS Statistics 20. Data were checked for normal distribution with the Kolmogorov-Smirnov-Test. Fisher's Exact test or Chi-Square test served for comparison of nominal values; risk factors were analyzed with univariate and multivariate logistic regression. When reaching a two-sided α-error level of p < 0.05, statistical significance was assumed.
This clinical research project was assessed and approved by the local Ethical Committee of the University of Regensburg medical center under reference No. 18-104-899.
In our study population, closure of a protective loop-ileostomy was feasible in 86.8% (data not shown). That means, at the same time, 13.2% of all cases failed to be reversed, and a temporarily intended enterostomy might have become a permanent one (death, n = 39; lost to follow-up, n=16; refused any further surgical intervention, n = 4). For the 409 patients included in our further analyses, the average time from the primary procedure to the closure of the protective loop ileostomy was 1,674 days (median = 136 days). A negative and unwanted post-closure outcome with postoperative complications affected nearly every fourth closure procedure (23.5%). We found that waiting more than 90 days (p = 0.032*) or 120 days (p = 0.012*) was already associated with a significantly higher rate of postoperative complications (data not shown). However, as shown in Figure 1 and Table 1, especially scheduling the closure procedure after 150 days from the initial procedure, made a decisive difference concerning negative outcomes after loop-ileostomy closure (31.7 vs. 17.%; p = 0.001**) compared to an early closure within 150 days. Furthermore, as shown in Figure 2, patients with a late closure procedure also had a significantly longer hospital stay (median, 6 vs. 6.5 days and IQR, 3 vs. 4.75 days; p = 0.0087).
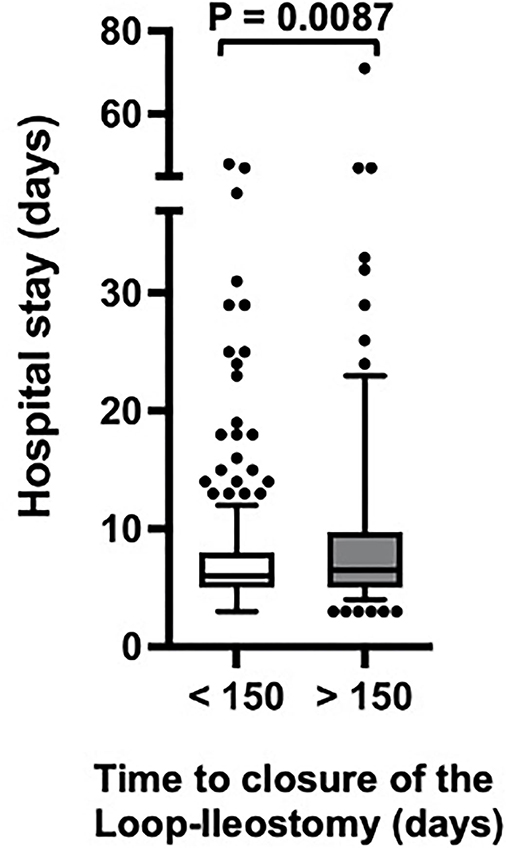
Figure 2. Hospital stay depending on the time of closure of the protective loop-ileostomy. Statistic: non-parametric Mann–Whitney test.
Having established that timing of the closure of a protective loop-ileostomy had a significant impact on the rate of postoperative complications, we further analyzed potential reasons for a belated closure procedure to find any distribution bias between the early (<150 days) and late (>150 days) closure group. As shown in Table 2, the patients who received an early closure (mean = 57.5 years, SD = 14.6 years) were—on average—significantly younger than the patients whose enterostomy was closed after 150 days (mean = 60.3 years, SD = 11. years; p = 0.028*). However, the ratio between young and old patients with enterostomy below or above 60 years of age was equally distributed between both groups (p = 0.122). Furthermore, there was no significant difference in the gender distribution between the early (men: 71.2%; women: 28.8%) and late (men: 73.3%; women: 26.7%) closure groups (p = 0.630).
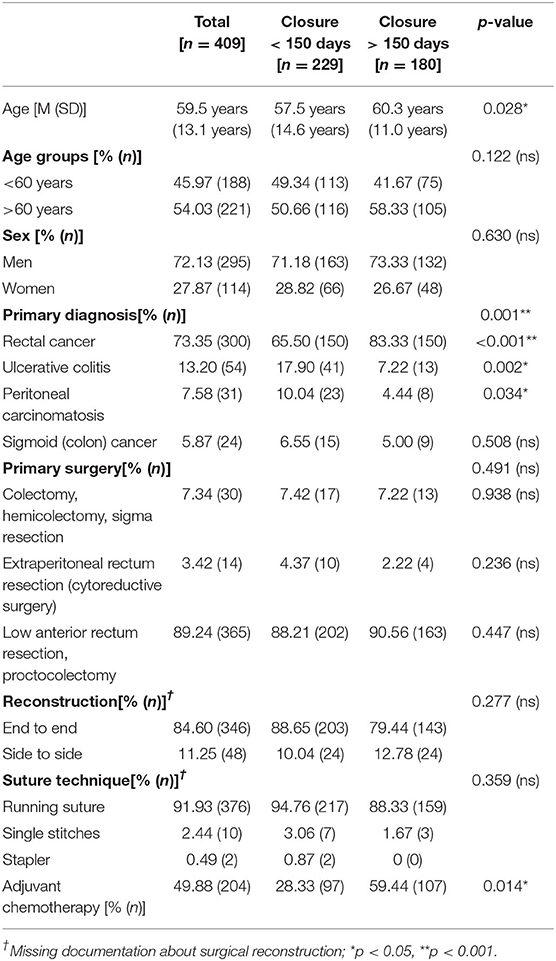
Table 2. Distribution of risk factors in the overall population and within the subgroups of early and late closure.
Regarding the primary diagnosis, the patients with rectal cancer significantly more often (83.3%) underwent a late closure after 150 days from primary surgery compared to the patients with other diagnoses (p < 0.001**), while the closure of protective loop-ileostomy in the patients with ulcerative colitis (17.9%; p = 0.002*) or peritoneal carcinomatosis (10%; p = 0.034*) was significantly more frequently conducted early within 150 days after enterostomy. Only the patients with (sigmoid) colon cancer were equally distributed between the groups of early and late closure (p = 0.508).
The corresponding primary surgical interventions, however, did not significantly differ in the distribution between early or late closure (p = 0.491)—neither for (hemi-) colectomy and sigma resection (p = 0.938), nor for extraperitoneal rectum resection (p = 0.236) or low anterior rectum resection and proctocolectomy (p = 0.447). Furthermore, neither the reconstruction technique (end to end or side to side), nor the suture technique was significantly different between the two groups. However, the patients in the late closure group frequently received significantly adjuvant chemotherapy before the closure procedure was performed (p = 0.0141).
Next, we analyzed the severity of post-closure complications based on a slightly modified Clavien-Dindo classification. As shown in Table 1, digestive dysfunctions occurred significantly more often in the patients with a late closure (>150 days): (sub-) ileus (4.8 vs. 12.8%; p = 0.004*) or diarrhea and stool incontinence (5.7 vs. 14.4%; p = 0.003*) affected the patients with a belated closure more often. Other unwanted outcomes, such as formation of fistulas or abscesses (1.7 vs. 4.4%; p = 0.109), injury of other intra-abdominal organs (1.3 vs.0.0%; p = 0.123), insufficient wound healing (3.9 vs. 4.4%; p = 0.796) or development of an abdominal wall hernia (0.9 vs.0.6%; p = 0.708), were found with a similar contribution between both groups. Moreover, the severity of the post-closure complications was associated with the timing of the closure procedure. Early stoma closure within 150 days from primary surgery was associated with significantly less mild (7.9 vs. 15.6%; p = 0.014*) complications. The categories of moderate (4.8 vs. 8.9%; p = 0.099) or severe complications (4.4 vs. 7.2%; p = 0.213), however, resembled similar distribution between both groups without lethal complications.
In a final step, we wanted to link certain associated factors with post-closure complications. We found “time to clo” (p < 0.001**) and “sex” (p = 0.045*) as significant risk factors in the development of post-closure complications in a univariate logistic regression analysis as demonstrated in Table 3. Late closure of the protective loop-ileostomy after 150 days was associated with up to 12 times elevated risk for complications compared to early closure within 150 days from primary surgery (OR: 0.443; CI, 95%: 0.078–0.706) and the risk for men tripled that of women (OR: 0.566; CI, 95%: 0.324–0.988). Finally, we could substantiate that the timing of the closure is still a significant risk factor (p = 0.002*), even when controlled for gender, in a multivariate logistic regression analysis as shown in Table 4.
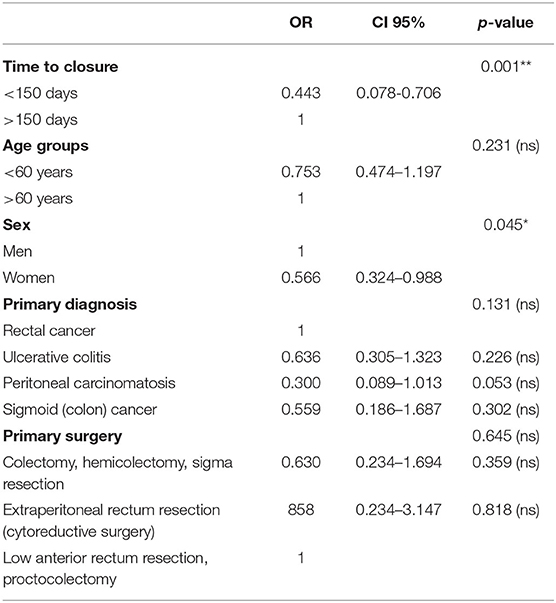
Table 3. Univariate analysis of risk factors in complications after closure of the protective loop-ileostomy.
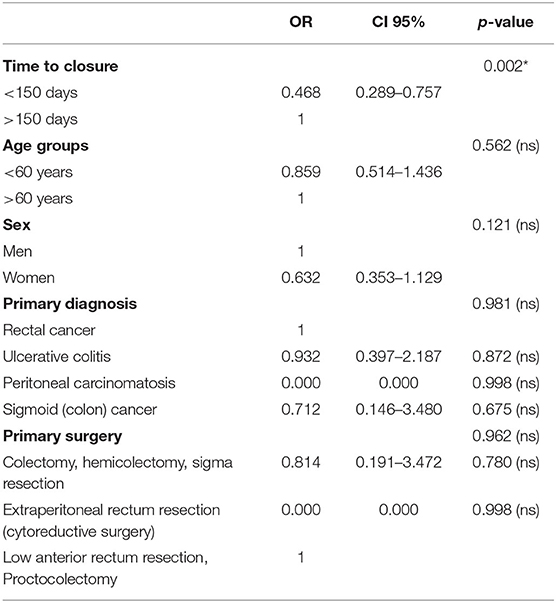
Table 4. Multivariate analysis of risk factors in complications after closure of the protective loop-ileostomy.
The best timing of the closure of a protective loop-ileostomy is yet a quite inconclusive issue with many considerations being insufficiently addressed. Finding the “sweet spot” is further aggravated, because either a hasty or a delayed closure is accompanied by a tremendous risk of post-closure complications (5, 6, 15), amounting to 23.5% in total in the present study. Here, the number of adverse outcomes after protective loop-ileostomy closure was strongly associated with the time interval between primary surgery and closure of the enterostomy. When bowel continuity was restored within 150 days, complications occurred in 17%. Waiting more than 150 days for the closure procedure was associated with complications in almost every third case (31.7%).
The time between installation and closure of a protective loop-ileostomy is often substantially longer than initially planned. Completion of adjuvant chemotherapy is usually the leading argument against the closure of an enterostomy (7, 8). But waiting too long might result in medical, surgical, and psychological impairments (2, 3): Electrolyte derangements, dehydration, and malnutrition such as parastomal skin irritations can be found frequently in patients with a protective loop-ileostomy, and problems such as parastomal herniation, obstruction, or ileus may require surgical intervention (1, 16). Besides, an artificial bowel output disturbs activities of daily living, often leading to a diminution of health-related quality of life, and it changes the self-concept, which, in turn, could lower the patient's self-esteem (17, 18).
As we could demonstrate, dysfunctional complications such as either (sub-) ileus or diarrhea and stool incontinence might not only occur due to a prolonged loop-ileostomy but also as a result of a belated closure. Even though the severity of post-closure complications was relatively low and did not differ between groups in the categories of moderate and severe negative outcomes, mild complications were found significantly more frequent in patients with a late closure of a protective loop-ileostomy. Our data are in line with reports from Abdalla and Scarpinata (19) as well as Hughes et al. (20), who accounted for the negative impact of a delayed closure more than 6 months after index surgery on the rate of post-closure complications in a small cohort, whereas Zhen et al. (21) could not substantiate the inferiority of a late closure operation. The authors observed a comparable number of adverse outcomes for patients with a closure beyond 6 months from primary surgery, but this study group actually received more adjuvant chemotherapy cycles and might, thus, even have a better prognosis than patients with an early closure. Li and Ozuner (22) investigated a time interval of more or <3 months between enterostomy and stoma closure. Findings revealed no relevant intergroup differences.
Closure of a protective loop-ileostomy has to be acknowledged as an independent intervention unaffected by primary indication or surgery and with an often-underestimated risk for post-closure morbidity and mortality (15, 23–25). Although a vast spectrum of gastrointestinal diseases demanding an enterostomy and corresponding diverse enteric resections was included in the analysis, no negative impact of those substantial factors could be proved as relevant for the closure operation in our study. However, rectal cancer and the usual correspondingly low anterior rectum resection seem to negatively influence the post-closure outcome when waiting more than 150 days until the closure of protective loop-ileostomy. Yet, another bias must be critically considered: The closure of a protective loop-ileostomy in patients with rectal cancer is significantly more often postponed and, hence, has proportionately more cases with closure after 150 days from enterostomy.
So far, it was a silent agreement that a closure procedure should not be performed 60–90 days after installation of an enterostomy. This consensus was based on a clinical experience of patient recovery and owed to the circumstance that intra-abdominal adhesions are more manageable after about 2 months from primary surgery, and inflammation, as well as edema of the loop-ileostoma, has usually been resolved. (4, 6) Nevertheless, recent reports have even intended to curtail the time to enterostomy closure to a minimum of only a few weeks (4, 26–30). Farang et al. (29) found that early closure of loop-ileostomy within 2 weeks of index surgery of distal colorectal resection was feasible with outcomes comparable to delayed closure. Robertson et al. (30) came to the same conclusion but pointed out that further investigations are warranted with a special focus on sensitive selection strategies to identify those patients that might profit from this non-standard fast-track approach (27).
However, there are also limitations to our study that need to be considered when interpreting the results. The included number of patients (n = 409) is relatively small, especially when calculating the outcomes for subgroups. A retrospective analysis of clinical data, per se, has some limitations since the assessment of outcomes relies on others for accurate record-keeping, and because the retrospective aspect may introduce selection bias. Furthermore, the data were collected only in a single center and in a health care system with no influence of insufficient resources. This needs to be considered when our data are compared to other settings, where the closure of a protective ileostomy might be delayed due to insufficient health care resources or high costs for the patients.
In our study population, closure of a protective loop-ileostomy was feasible in 86.8% (data not shown). That means, at the same time, 13.2% of all cases failed to be reversed, and a temporarily intended enterostomy became a permanent one. Literature designates relevant risk factors that include advanced age, anastomotic leakage, metastasis, and adjuvant radiochemotherapy (4, 5, 7, 31–34). Consequently, a circumspect consideration of those predictors for non-closure, in conjunction with an overall benefit/risk analysis, is required to achieve the best outcome for each patient when deciding upon a temporary or a permanent stoma in advance of enterostomy (35, 36). Predictive tools like the nomogram, developed by Abe et al. (37), might help to identify patients with a high risk of stoma non-reversal.
Protective loop-ileostomy is one of the most common interventions in abdominal surgery. Late closure (>150 days) of a protective loop-ileostomy is associated with a significantly higher rate of postoperative complications. Dysfunctional digestive problems, such as ileus, diarrhea, or stool incontinence, were the most frequent complications associated with late closure. Hence, early restitution of enteric continuity might be considered under a careful selection of patients, a thorough pre-operative assessment, and an evaluation of feasibility.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethical Committee of the University of Regensburg medical center under the reference number 18-104-899. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
MH and JW: conception and design of the study. PK, ME, and SO: data acquisition. PK, ME, SO, MH, and JW: analysis and interpretation of the data. JW: drafting of the manuscript. HS, MH, and JW: revision of the manuscript. All authors had access to the study data and critically reviewed and approved the final version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Martin ST, Vogel JD. Intestinal stomas. Adv Surg. (2012) 46:19–49. doi: 10.1016/j.yasu.2012.04.005
2. Ambe PC, Kurz NR, Nitschke C, Odeh SF, Moslein G, Zirngibl H. Intestinal ostomy. Dtsch Arztebl Int. (2018) 115:182–7. doi: 10.3238/arztebl.2018.0182
3. Shabbir J, Britton DC. Stoma complications: a literatureoverview. Color Dis. (2010) 12:958–64. doi: 10.1111/j.1463-1318.2009.02006.x
4. Sherman KL, Wexner SD. Considerations in stoma reversal. Clin Colon Rectal Surg. (2017) 30:172–7. doi: 10.1055/s-0037-1598157
5. Gessler B, Haglind E, Angenete E. Loop ileostomies in colorectal cancer patients–morbidity and risk factors for nonreversal. J Surg Res. (2012) 178:708–14. doi: 10.1016/j.jss.2012.08.018
6. Perez RO, Habr-Gama A, Seid VE, Proscurshim I, Sousa A, Kiss D, et al. Loop ileostomy morbidity: timing of closure matters. Dis Colon Rectum. (2006) 49:1539–45. doi: 10.1007/s10350-006-0645-8
7. Sier MF, van Gelder L, Ubbink DT, Bemelman WA, Oostenbroek RJ. Factors affecting timing of closureand non-reversal of temporaryileostomies. Int J Colorectal Dis. (2015) 30:1185–92. doi: 10.1007/s00384-015-2253-3
8. Bakx R, Busch ORC, Bemelman WA, Veldink GJ, Slors JFM, van Lanschot JJB. Morbidity of temporary loop ileostomies. Dig Surg. (2004) 21:277–81. doi: 10.1159/000080201
9. Jimenez-Rodriguez RM, Segura-Sampedro JJ, Rivero-Belenchon I, Diaz Pavon J, Garcia Cabrera A, Vazquez Monchul J, et al. Is the interval from surgery to ileostomy closure a risk factor for low anterior resection syndrome? Colorectal Dis. (2017) 19:485–90. doi: 10.1111/codi.13524
10. Saito Y, Takakura Y, Hinoi T, Egi H, Tashiro H, Ohdan H. Body mass index as a predictor of postoperative complications in loop ileostomy closure after rectal resection in Japanese patients. Hiroshima J Med Sci. (2014) 63:33–8.
11. Man VCM, Choi HK, Law WL, Foo DCC. Morbidities after closure of ileostomy: analysis of risk factors. Int J Colorectal Dis. (2016) 31:51–7. doi: 10.1007/s00384-015-2327-2
12. Pokorny H, Herkner H, Jakesz R, Herbst F. Mortality and complications after stoma closure. Arch Surg. (2005) 140:956–60; discussion 960. doi: 10.1001/archsurg.140.10.956
13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. (2004) 240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae
14. Clavien PA, Barkun J, de Oliveira ML, Vauthey J, Dindo D, Schulick R, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. (2009) 250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2
15. Sharma A, Deeb A-P, Rickles AS, Iannuzzi JC, Monson JRT, Fleming FJ. Closure of defunctioning loop ileostomy is associated with considerable morbidity. Colorectal Dis. (2013) 15:458–62. doi: 10.1111/codi.12029
16. Caricato M, Ausania F, Ripetti V, Bartolozzi F, Campoli G, Coppola R. Retrospective analysis of long-term defunctioning stoma complications after colorectal surgery. Color Dis. (2007) 9:559–61. doi: 10.1111/j.1463-1318.2006.01187.x
17. Tsunoda A, Tsunoda Y, Narita K, Watanabe M, Nakao K, Kusano M. Quality of life after low anterior resection and temporary loop ileostomy. Dis Colon Rectum. (2008) 51:218–22. doi: 10.1007/s10350-007-9101-7
18. O'Leary DP, Fide CJ, Foy C, Lucarotti ME. Quality of life after low anterior resection with total mesorectal excision and temporary loop ileostomy for rectal carcinoma. Br J Surg. (2001) 88:1216–20. doi: 10.1046/j.0007-1323.2001.01862.x
19. Abdalla S, Scarpinata R. Early and late closure of loop ileostomies: a retrospective comparative outcomes analysis. Ostomy Wound Manage. (2018) 64:30–5. doi: 10.25270/owm.2018.12.3035
20. Hughes DL, Cornish J, Morris C. Functional outcome following rectal surgery-predisposing factors for low anterior resection syndrome. Int J Colorectal Dis. (2017) 32:691–7. doi: 10.1007/s00384-017-2765-0
21. Zhen L, Wang Y, Zhang Z, Wu T, Liu R, Li T, et al. Effectiveness between early and late temporary ileostomy closure in patients with rectal cancer: a prospective study. CurrProbl Cancer. (2017) 41:231–40. doi: 10.1016/j.currproblcancer.2017.02.007
22. Li W, Ozuner G. Does the timing of loop ileostomy closure affect outcome: a case-matched study. Int J Surg. (2017) 43:52–55. doi: 10.1016/j.ijsu.2017.05.039
23. Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. (2009) 24:711–23. doi: 10.1007/s00384-009-0660-z
24. Abegg RM, Brokelman W, van Bebber IP, Bosscha K, Prins HA, Lips DJ. Results of construction of protective loop ileostomies and reversal surgery for colorectal surgery. Eur Surg Res. (2014) 52:63–72. doi: 10.1159/000357053
25. Mengual-Ballester M, García-Marín JA, Pellicer-Franco E, Guillén-Paredes M, García-García M, Cases-Baldó M, et al. Protective ileostomy: complications and mortality associated with its closure. Rev Esp Enferm Dig. (2012) 104:350–4. doi: 10.4321/S1130-01082012000700003
26. Lee KH, Kim HO, Kim JS, Kim JY. Prospective study on the safety and feasibility of early ileostomy closure 2 weeks after lower anterior resection for rectal cancer. Ann Surg Treat Res. (2019) 96:41–6. doi: 10.4174/astr.2019.96.1.41
27. Menahem B, Lubrano J, Vallois A, Alves A. Early closure of defunctioning loop ileostomy: is it beneficial for the patient? A meta-analysis. World J Surg. (2018) 42:3171–8. doi: 10.1007/s00268-018-4603-0
28. Danielsen AK, Park J, Jansen JE, Bock D, Skullman S, Wedin A, et al. Early closure of a temporary ileostomy in patients with rectal cancer: a multicenter randomized controlled trial. Ann Surg. (2017) 265:284–90. doi: 10.1097/SLA.0000000000001829
29. Farag S, Rehman S, Sains P, Baig MK, Sajid MS. Early vs delayed closure of loop defunctioning ileostomy in patients undergoing distal colorectal resections: an integrated systematic review and meta-analysis of published randomized controlled trials. Colorectal Dis. (2017) 19:1050–7. doi: 10.1111/codi.13922
30. Robertson JP, Puckett J, Vather R, Jaung R, Bissett I. Early closure of temporary loop ileostomies: a systematic review. Ostomy Wound Manage. (2015) 61:50–7.
31. da-Fonseca LM, Buzatti KC de LR, Castro LL, Lacerda Filho A, Correia MITD, da-Silva RG. Factors preventing restoration of bowel continuity in patients with rectal cancer submitted to anterior rectal resection and protective ileostomy. Rev Col Bras Cir. (2019) 45:e1998. doi: 10.1590/0100-6991e-20181998
32. Chiu A, Chan HT, Brown CJ, Raval MJ, Phang PT. Failing to reverse a diverting stoma after lower anterior resection of rectal cancer. Am J Surg. (2014) 207:708–11; discussion 711. doi: 10.1016/j.amjsurg.2013.12.016
33. Lindgren R, Hallbook O, Rutegard J, Sjodahl R, Matthiessen P. What is the risk for a permanent stoma after low anterior resection of the rectum for cancer? A six-year follow-up of a multicenter trial. Dis Colon Rectum. (2011) 54:41–7. doi: 10.1007/DCR.0b013e3181fd2948
34. David GG, Slavin JP, Willmott S, Corless DJ, Khan AU, Selvasekar CR. Loop ileostomy following anterior resection: is it really temporary? Colorectal Dis. (2010) 12:428–32. doi: 10.1111/j.1463-1318.2009.01815.x
35. Gustafsson CP, Gunnarsson U, Dahlstrand U, Lindforss U. Loop-ileostomy reversal-patient-related characteristics influencing time to closure. Int J Colorectal Dis. (2018) 33:593–600. doi: 10.1007/s00384-018-2994-x
36. Cipe G, Erkek B, Kuzu A, Gecim E. Morbidity and mortality after the closure of a protective loop ileostomy: analysis of possible predictors. Hepatogastroenterology. (2012) 59:2168–72. doi: 10.5754/hge12115
Keywords: protective loop-ileostomy, enterostomy, closure surgery, surgical complications, dysfunctional digestion
Citation: Werner JM, Kupke P, Ertl M, Opitz S, Schlitt HJ and Hornung M (2022) Timing of Closure of a Protective Loop-Ileostomy Can Be Crucial for Restoration of a Functional Digestion. Front. Surg. 9:821509. doi: 10.3389/fsurg.2022.821509
Received: 24 November 2021; Accepted: 28 February 2022;
Published: 28 March 2022.
Edited by:
Sven Flemming, University Hospital of Wuerzburg, GermanyReviewed by:
Ulf Gunnarsson, Umeå University, SwedenCopyright © 2022 Werner, Kupke, Ertl, Opitz, Schlitt and Hornung. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jens M. Werner, amVucy53ZXJuZXJAdWtyLmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.