- 1Oral and Maxillofacial Radiology, Applied Oral Sciences and Community Dental Care, Faculty of Dentistry, The University of Hong Kong, Pok Fu Lam, Hong Kong SAR, China
- 2Oral and Maxillofacial Surgery, Faculty of Dentistry, The University of Hong Kong, Pok Fu Lam, Hong Kong SAR, China
Background: Chin implants have a long history, and its usage may be associated with mandibular bone resorption.
Objectives: This report analyzed data on this topic from existing literature to evaluate the overall resorption rate and scientific impact in terms of citations.
Method: PubMed, Web of Science, Scopus, and Google Scholar databases were searched to identify relevant publications. The search string was as follows: (chin) AND (augment* OR implant*) AND (resorb* OR resorp*) AND (bone OR osseous). A study was eligible if it recruited human subjects and reported resorption following any chin implantation based on radiographic examination.
Results: Twenty-eight patient studies were identified. Publication year seemed to have no effect on the mean depth of bone resorption and its prevalence as reported by the studies. The increased mean number of follow-up years seemed to have no effect on its prevalence but seem to be associated with deeper bone resorption. The majority of the studies had <5 years of follow-up and reported a mean of <2 mm of bone resorption. The most cited study had 69 citations. Citations rarely came from radiology journals. A limitation was that unpublished data could not be analyzed.
Conclusions: Mandibular bone resorption caused by chin implants of various materials is a common phenomenon. Its recognition and studies with a longer follow-up period should be further promoted.
Introduction
Chin implants have a long history. The earliest reports of causing bone resorption at the augmentation site could be traced back to the 1960s (1). The extent of bone resorption could be evaluated by plain radiography, such as panoramic imaging (to evaluate from the mesiodistal dimension, or “width”) and lateral cephalography (to evaluate the buccolingual extent, or “depth”). Three-dimensional imaging, such as cone-beam computed tomography (CBCT), would give a better visualization of bone resorption. The resorption might be influenced by the positioning of the chin implant. In addition, it is usually more severe at the superior end due to the contraction force of the mentalis muscle (2). Figure 1 shows a typical appearance of mandibular bone resorption caused by a chin implant, leaving an imprint on the labial surface of the mandible. If the resorption extended to the periapical region of the mandibular anterior teeth, the neurovascular bundles supplying these teeth could be severed, rendering them non-vital.
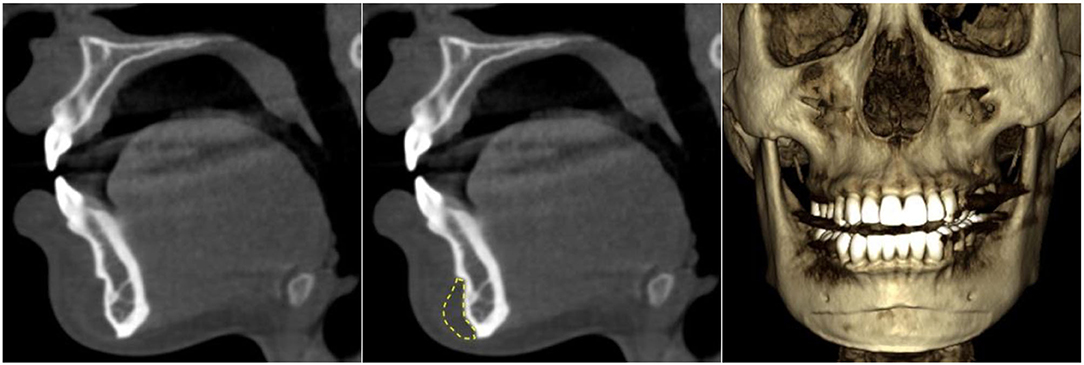
Figure 1. Mandibular bone resorption on the labial surface caused by a chin implant observed with cone-beam CT. The resorption was obvious in both sagittal view and volume rendering. The chin implant is circled yellow.
Half a century has elapsed since the earliest reports on the bone resorption caused by chin augmentation. This study aimed to evaluate the scientific evidence on radiographic bone resorption following chin implantation. The objectives were to analyze the reported prevalence and depth of such bone resorption and to reveal the amount of scientific attention paid to this topic in terms of citation count. To view the citation performance from another perspective, the relative citation ratio (RCR), a metric that indicates the relative citation performance of a publication as compared to other publications in its research area (with >1 means above the average) (3, 4), was recorded.
Materials and Methods
On June 17, 2021, four literature databases (PubMed, Web of Science, Scopus, and Google Scholar) were searched. The search string was as follows: (chin) AND (augment* OR implant*) AND (resorb* OR resorp*) AND (bone OR osseous). For PubMed, the search covered the fields of article title and abstract. For Web of Science and Scopus, the search covered article title, abstract, and keywords. Because Google Scholar searched all fields of the publications including their full texts and reference lists, the abovementioned search string returned with many irrelevant articles focusing on dental implants. To be more specific, the search string was modified for Google Scholar as “chin augmentation resorption,” and the first 100 publications were screened. Hand search on the reference lists of the screened publications was also performed. No limitation was set for the publication year, but the publications must be written in English. The searches initially returned with 384 publications. After removing duplicates, 218 publications remained. The statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS) was as follows: participants—human subjects; interventions—chin implantation but not bone augmentation; comparisons—within-subject comparison; outcome—radiographic evaluation of mandibular bone resorption; and study design—a longitudinal study. After screening and excluding unsuitable publications for specific reasons, 28 studies remained for review (Figure 2). Ethical approval was not applicable to this review. This systematic review was not pre-registered in PROSPERO or other databases.
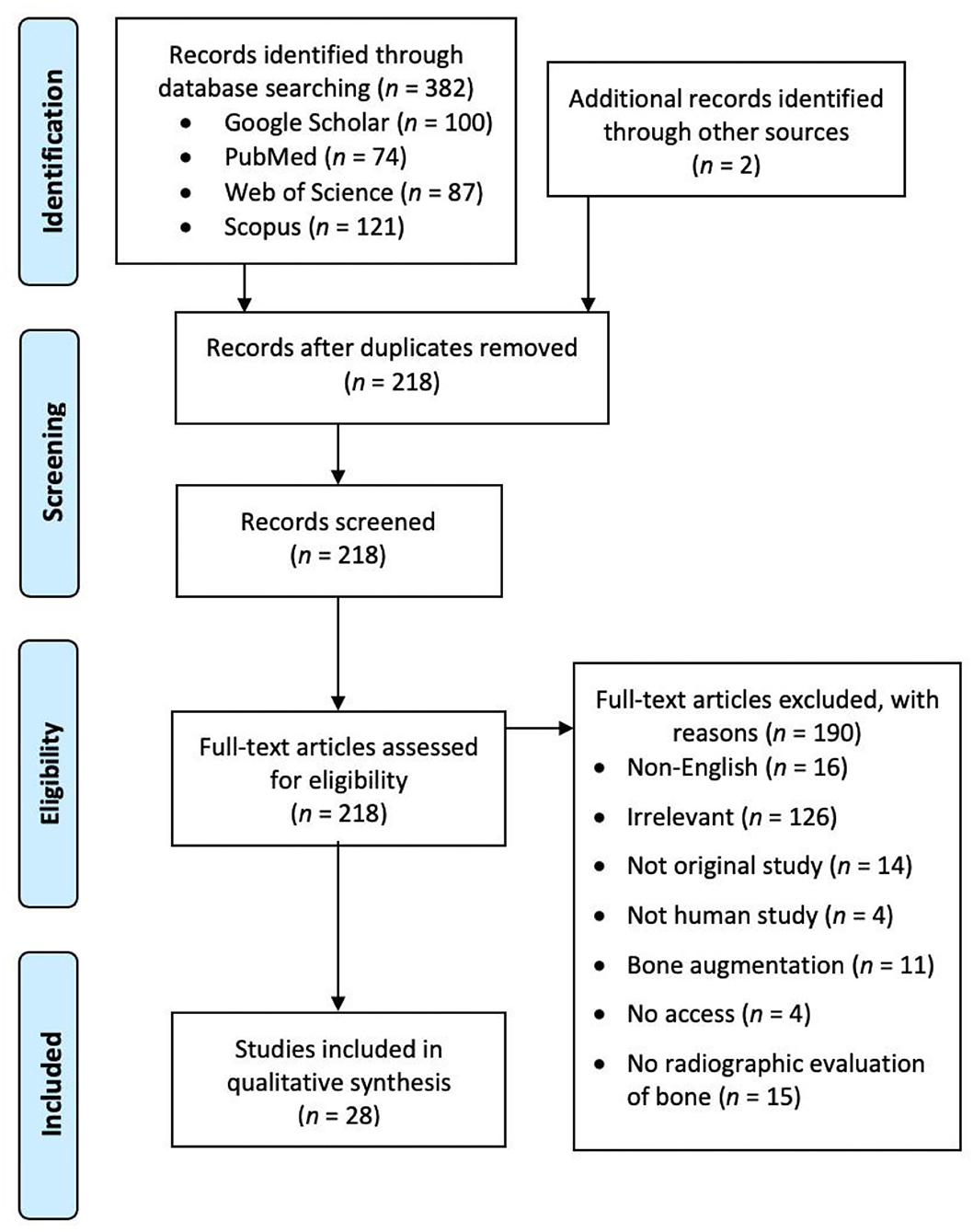
Figure 2. A preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow chart showing the screening process of the literature search.
Results
The 28 identified studies are listed in Table 1 (1, 2, 5–30). Several key points to summarize the data were as follows:
(1) Publication year seemed to have no effect on the mean depth of bone resorption and its prevalence as reported by the studies (Figures 3A,B).
(2) Increased mean number of follow-up years seemed to associate with deeper bone resorption. However, readers should notice that the majority of the studies had <5 years of follow-up and reported a mean of <2 mm of bone resorption. Only four studies had >10 years of follow-up on average, with one of them reporting a resorption rate of 75%, whereas the remaining three reported positive cases only (Figure 3C).
(3) Mean number of follow-up years seemed to have no effect on the prevalence of bone resorption as reported by the studies (Figure 3D). Seven studies reported 0% prevalence. On the other hand, 5 studies reported a prevalence of >85%.
(4) Sub-periosteal placement of chin implants seemed to be the mainstream. Only two studies solely evaluated supra-periosteal chin implants. Both reported an absence of bone resorption.
(5) Silicone (silastic) was the most common implant material, with highly varied depth and prevalence of bone resorption.
(6) These reports were mainly published in surgery journals. Only one was published in a radiology journal (neuroradiology).
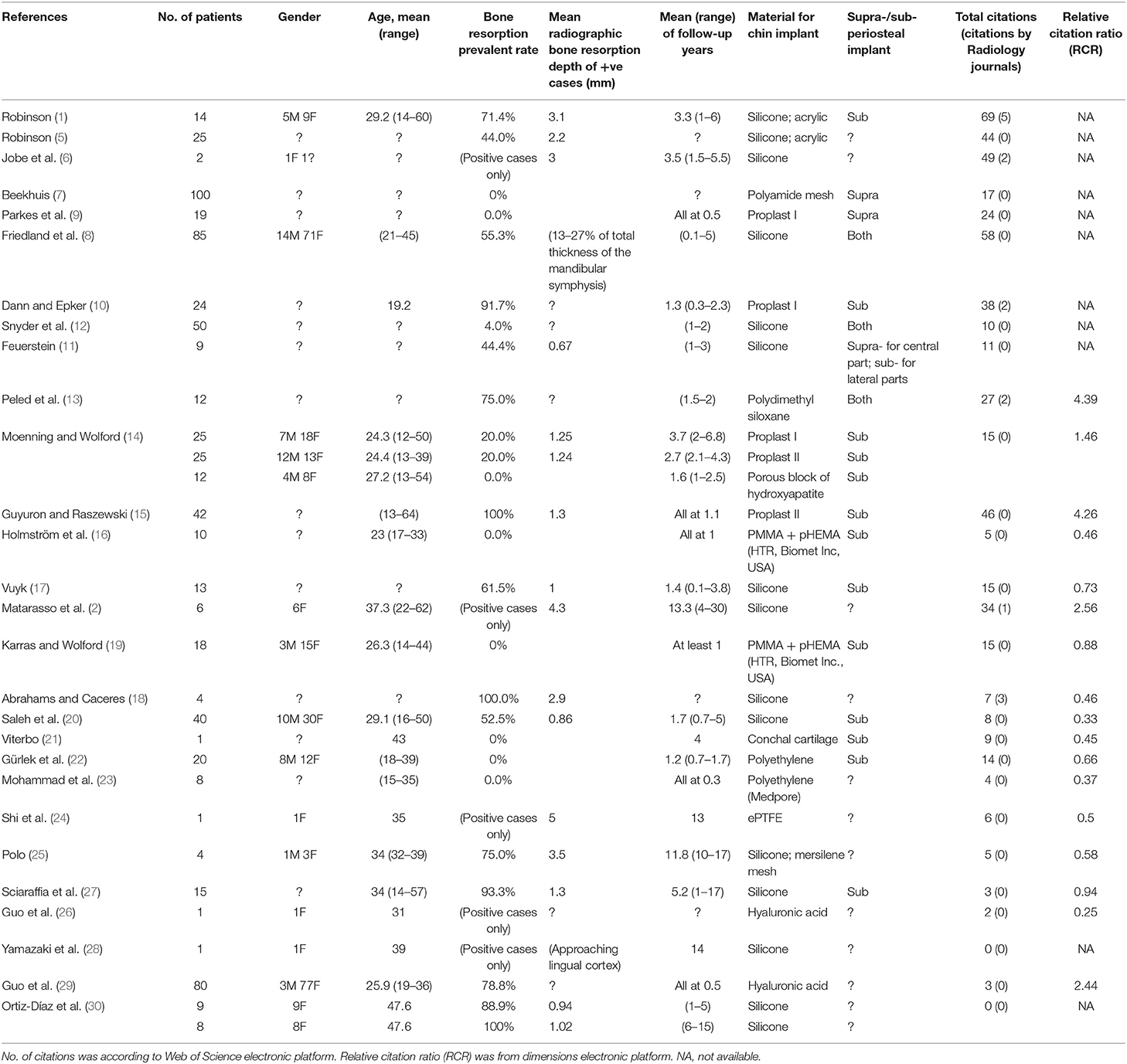
Table 1. Details of the 28 included studies of reporting mandibular bone resorption caused by chin implant.
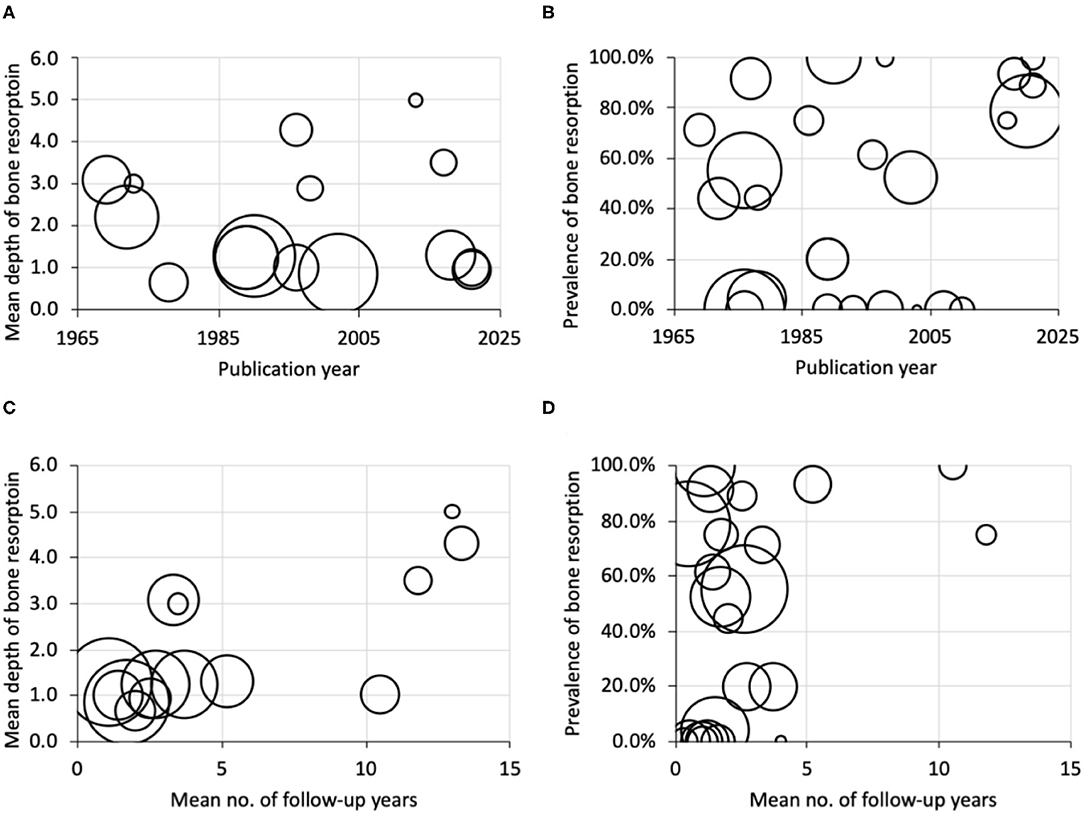
Figure 3. Bubble plots of publication year against (A) mean depth of bone resorption, (B) prevalence of bone resorption, and of the mean number of follow-up years against, (C) mean depth of bone resorption, and (D) prevalence of bone resorption. Bubble size indicates the sample size.
Data from Web of Science indicated that the most cited paper was Robinson (1) with 69 citations. It was also the paper with the highest citations from dental or medical radiology journals (5 citations). Only six of the 28 studies (21.4%) received citations from radiology journals. Overall, the 28 studies had a mean ± SD of 19.2 ± 19.1 citations, with 0.5 ± 1.2 citations from radiology journals.
Discussion
This work identified 28 studies reporting the prevalence and mean depth of mandibular bone resorption caused by chin implants in patients. They reported a very wide range of prevalence, specifically from 0 to 100%. The increased mean number of follow-up years seemed to associate with deeper bone resorption, but most studies had <5 years of follow-up and reported a mean of <2 mm of bone resorption. Silicone was the most common chin implant material used, and sub-periosteal placement was the most common technique. Subjects were mostly females who were young adults or middle-aged. The implant material, placement technique, and gender did not seem to have a profound effect on the resorption rate.
Unlike some incidental radiographic findings, such as medial sigmoid depression in the mandible for which the reports were seldom cited (31), the mandibular bone resorption caused by chin implant is well known and the reports were frequently cited. This review showed that these reports were cited 19.2 times on average, a figure even higher than that of osteoporosis detection by panoramic imaging (32). Surprisingly, this phenomenon was rarely mentioned by radiology journals and, thus, received few citations by the latter. In terms of RCR, most of the studies had a score <1, meaning that their citation performance was still below the average compared to other papers in the radiology and plastic surgery research areas. Chin implant and its associated bone resorption have important clinical implications as they may affect the mental foramen, causing chin hypoesthesia/dysesthesia and tooth root damage together with other potential complications (33). Evaluation of the positioning of a chin implant or the extent of bone resorption heavily relies on radiographic examinations that are not intrusive or traumatic. With the increasing number of patients undergoing plastic surgery in the head and neck region including the chin, a recommendation should be made to promote the awareness of this mandibular bone resorption. More long-term longitudinal research should be conducted on this topic to better understand the temporal profile of the progression of this bone resorption, e.g., whether it would progress continuously with time or become stable after a certain period. This bone resorption phenomenon is probably better known by oral and maxillofacial surgeons and plastic surgeons, but not dentomaxillofacial radiologists or general dentists. Regardless, they should all be more aware of bone resorption and its associated consequences. Readers should be aware that one limitation of this study was that unpublished data could not be analyzed. In addition, a citation could be supporting the cited findings, mentioning them, or contrasting them, which was not evaluated in this report.
Conclusions
To conclude, mandibular bone resorption caused by chin implants of various materials is frequently documented. It is an uncommon yet highly important post-surgery complication as the resorption may eventually erode the mental foramen and the roots of mandibular teeth. Hence, its recognition should be promoted. In addition, most studies had <5 years of follow-up with a mean of <2 mm of bone resorption. Studies with >10 years of follow-up had very small sample sizes. When all studies were considered together, an increased number of follow-up years seemed to associate with deeper bone resorption. Hence, longer follow-up periods in future studies should be further promoted.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
AY is responsible for design, data collection, analysis, and manuscript writing. NW is responsible for data collection and manuscript writing. Both authors contributed to the article and approved the submitted version.
Funding
This work was supported by departmental funding.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
2. Matarasso A, Elias AC, Elias RL. Labial incompetence: a marker for progressive bone resorption in silastic chin augmentation. Plast Reconstr Surg. (1996) 98:1007–14. doi: 10.1097/00006534-199611000-00012
3. Hutchins BI, Yuan X, Anderson JM, Santangelo GM. Relative citation ratio (RCR): a new metric that uses citation rates to measure influence at the article level. PLoS Biol. (2016) 14:e1002541. doi: 10.1371/journal.pbio.1002541
4. Hutchins BI, Hoppe TA, Meseroll RA, Anderson JM, Santangelo GM. Additional support for RCR: a validated article-level measure of scientific influence. PLoS Biol. (2017) 15:e2003552. doi: 10.1371/journal.pbio.2003552
5. Robinson M. Bone resorption under plastic chin implants: follow-up of a preliminary report. Arch Otolaryngol. (1972) 95:30–2. doi: 10.1001/archotol.1972.00770080078006
6. Jobe R, Iverson R, Vistnes L. Bone deformation beneath alloplastic implants. Plast Reconstr Surg. (1973) 51:169–75. doi: 10.1097/00006534-197302000-00012
7. Beekhuis GJ. Augmentation mentoplasty using polyamide mesh. Laryngoscope. (1976) 86:1602–5. doi: 10.1288/00005537-197610000-00016
8. Friedland JA, Coccaro PJ, Converse JM. Retrospective cephalometric analysis of mandibular bone absorption under silicone rubber chin implants. Plast Reconstr Surg. (1976) 57:144–51. doi: 10.1097/00006534-197602000-00002
9. Parkes ML, Kamer FM, Merrin ML. Proplast chin augmentation. Laryngoscope. (1976) 86:1829–35. doi: 10.1002/lary.5540861207
10. Dann JJ, Epker BN. Proplast genioplasty: a retrospective study with treatment recommendations. Angle Orthod. (1977) 47:173–85.
11. Feuerstein SS. Intraoral augmentation mentoplasty with a hinged silastic implant: a three-year xerographic follow-up study. Arch Otolaryngol. (1978) 104:383–7. doi: 10.1001/archotol.1978.00790070021005
12. Snyder GB, Courtiss EH, Kaye BM, Gradinger GP. A new chin implant for microgenia. Plast Reconstr Surg. (1978) 61:854–61. doi: 10.1097/00006534-197861060-00004
13. Peled IJ, Wexler MR, Ticher S, Lax EE. Mandibular resorption from silicone chin implants in children. J Oral Maxillofac Surg. (1986) 44:346–8. doi: 10.1016/S0278-2391(86)80028-3
14. Moenning J, Wolford L. Chin augmentation with various alloplastic materials: a comparative study. Int J Adult Orthodon Orthognath Surg. (1989) 4:175–87.
15. Guyuron B, Raszewski RL. A critical comparison of osteoplastic and alloplastic augmentation genioplasty. Aesthetic Plast Surg. (1990) 14:199–206. doi: 10.1007/BF01578350
16. Holmström H, Kahnberg K-E, Lessard L. The use of preformed Htr® polymer implants for chin augmentation a preliminary report. Scand J Plast Reconstr Surg Hand Surg. (1993) 27:109–12. doi: 10.3109/02844319309079792
17. Vuyk H. Augmentation mentoplasty with solid silicone. Clin Otolaryngol Allied Sci. (1996) 21:106–18. doi: 10.1111/j.1365-2273.1996.tb01312.x
18. Abrahams JJ, Caceres C. Mandibular erosion from silastic implants: evaluation with a dental CT software program. Am J Neuroradiol. (1998) 19:519–22.
19. Karras SC, Wolford LM. Augmentation genioplasty with hard tissue replacement implants. J Oral Maxillofac Surg. (1998) 56:549–52. doi: 10.1016/S0278-2391(98)90449-9
20. Saleh H, Lohuis P, Vuyk H. Bone resorption after alloplastic augmentation of the mandible. Clin Otolaryngol Allied Sci. (2002) 27:129–32. doi: 10.1046/j.1365-2273.2002.00546.x
21. Viterbo F. Chin augmentation with conchal cartilage. Plast Reconstr Surg. (2003) 111:899–903. doi: 10.1097/01.PRS.0000041614.35184.C6
22. Gürlek A, Frat C, Aydogan H, Celik M, Ersöz-Öztürk A, Klnç H. Augmentation mentoplasty with diced high-density porous polyethylene. Plast Reconstr Surg. (2007) 119:684–91. doi: 10.1097/01.prs.0000246524.59092.1b
23. Mohammad S, Dwivedi CD, Singh R, Singh V, Pal U. Medpore versus osseous augmentation in genioplasty procedure: a comparison. Natl J Maxillofac Surg. (2010) 1:1. doi: 10.4103/0975-5950.69147
24. Shi L, Zhang Z-Y, Tang X-J. Severe bone resorption in expanded polytetrafluoroethylene chin augmentation. J Craniofac Surg. (2013) 24:1711–2. doi: 10.1097/SCS.0b013e31828b7304
25. Polo M. Bone resorption under chin implants: the orthodontist's role in its diagnosis and management. Am J Orthod Dentofacial Orthop. (2017) 151:201–8. doi: 10.1016/j.ajodo.2016.06.035
26. Guo X, Song G, Zong X, Jin X. Bone resorption in mentum induced by unexpected soft-tissue filler. Aesthet Surg J. (2018) 38:NP147–9. doi: 10.1093/asj/sjy156
27. Sciaraffia CE, Ahumada MF, Parada FJ, Gonzalez E, Prado A. Bone resorption after use of silicone chin implants, long-term follow-up study with lateral chin radiography. Plast Reconstr Surg Glob Open. (2018) 6:e1850. doi: 10.1097/GOX.0000000000001850
28. Yamazaki F, Takahashi K, Aoki A, Yano T, Tajima M, Ito K, et al. Bone resorption after alloplastic chin augmentation found incidentally in a patient with a toothache: report of a case. J Oral Maxillofac Surg Med Pathol. (2019) 31:275–9. doi: 10.1016/j.ajoms.2019.03.010
29. Guo X, Zhao J, Song G, Zong X, Zhang D, Lai C, et al. Unexpected bone resorption in mentum induced by the soft-tissue filler hyaluronic acid: a preliminary retrospective cohort study of Asian patients. Plast Reconstr Surg. (2020) 146:147e−55e. doi: 10.1097/PRS.0000000000006979
30. Ortiz-Díaz C, Echevarría E, Guerrero LM, Rivas-Tumanyan S, Elias A. Bone remodeling under screw-fixed chin implants in patients with microgenia: a cross-sectional study. Am J Cosm Surg. (2021) 38:75–85. doi: 10.1177/0748806820954747
31. Yeung AWK, Wong NSM. Medial sigmoid depression of the mandibular ramus as a lesion-mimicking anatomical variation: a systematic review. Int J Environ Res Public Health. (2021) 18:4271. doi: 10.3390/ijerph18084271
32. Yeung AWK, Mozos I. The innovative and sustainable use of dental panoramic radiographs for the detection of osteoporosis. Int J Environ Res Public Health. (2020) 17:2449. doi: 10.3390/ijerph17072449
Keywords: craniofacial surgery, radiology, cone-beam computed tomography, chin, diagnosis
Citation: Yeung AWK and Wong NSM (2022) Mandibular Bone Resorption Following Chin Augmentation: A Systematic Review. Front. Surg. 9:815106. doi: 10.3389/fsurg.2022.815106
Received: 15 November 2021; Accepted: 28 February 2022;
Published: 25 March 2022.
Edited by:
Feng Wang, Shanghai Jiao Tong University, ChinaReviewed by:
Riham Eldibany, Alexandria University, EgyptS. M. Balaji, Balaji Dental and Craniofacial Hospital, India
Copyright © 2022 Yeung and Wong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andy Wai Kan Yeung, bmR5ZXVuZ0Boa3UuaGs=
 Andy Wai Kan Yeung
Andy Wai Kan Yeung Natalie Sui Miu Wong2
Natalie Sui Miu Wong2