
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 09 May 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.814832
 Azuolas Kaminskas1
Azuolas Kaminskas1 Ausvydas Patasius2,3
Ausvydas Patasius2,3 Marius Kincius2
Marius Kincius2 Virginijus Sapoka3
Virginijus Sapoka3 Rytis Zilevicius1
Rytis Zilevicius1 Aušra Garnelytė4
Aušra Garnelytė4 Audrius Dulskas1,3*
Audrius Dulskas1,3*Background: Metastatic involvement of the penis in cases of rectal cancer is exceptionally rare condition. Our clinical case report and review of the literature will contribute in complementing currently limited data on penile metastasis from rectal cancer.
Case report: We report a case of a 64-year-old male diagnosed with penile metastasis from rectal cancer. The patient was treated with neoadjuvant chemoradiotherapy followed by total mesorectal excision (TME). However, penile metastasis developed 3 years later, clinically presenting as penile pain and solid formations along the entire length of the penis with visible tumor in the head of the penis. The amputation of penis was performed, and adjuvant chemotherapy was prescribed. The patient survived only 6 months.
Conclusion: Penile metastasis from rectal cancer in most cases is a lethal pathology that indicates wide dissemination of oncological disease and has a very poor prognosis. Aggressive surgical treatment is doubtful in metastatic disease as this will negatively affect the quality of life.
Colorectal cancer is one of the most common oncological diseases worldwide, which ranked third in terms of cancer incidence in 2020 (1). Most often, rectal cancer metastasizes to the liver, lungs, bones, and the peritoneum (2). Other atypical sites of metastases of rectal cancer are singular, and metastatic involvement of the penis is exceptionally rare condition, about which there is a relatively little information in the literature. According to our search, until now, there are only 72 cases reported in the literature (Table 1).
Here, we present a case of the patient who developed penile metastasis from rectal cancer and review the existing literature.
A 64-year-old male came to our clinic complaining of blood presence in the stool. The patient underwent a lower gastrointestinal tract endoscopy, and rectal cancer 7 cm from the anal verge was detected and confirmed with biopsy (moderately differentiated adenocarcinoma). The patient then underwent chest and abdominal computed tomography (CT) scan with pelvic magnetic resonance imaging (MRI) – the clinical diagnosis of middle rectal cancer (cT3N1) was confirmed. The patient was treated with neoadjuvant chemoradiotherapy (consisted of 50·4 Gray (Gy) in 28 fractions of 1·8 Gy per day for 5½ weeks with continuous infusion of fluorouracil (1,000 mg/m2 per day for 5 days) during the 1st and 5th weeks of radiotherapy). Eight weeks following the neoadjuvant treatment, follow-up MRI was performed. No tumor was visible, and only single suspicious lymph node in the mesorectum was seen. Patient underwent total mesorectal excision (totally 12 weeks following the neoadjuvant chemoradiotherapy). Resected specimen was examined by pathologists, and the diagnosis of moderately differentiated (G2) rectal adenocarcinoma with metastases to regional lymph nodes (ypT2N1b 2 of 15 lymph nodes), R0, and complete TME was confirmed. The postoperative course was uneventful, and adjuvant chemotherapy was not prescribed.
Three years later, the patient started complaining of penile pain and solid formations along the entire length of the penis. During physical examination, a rough and raised tumor with unclear boundaries was observed in the head of the penis, and solid infiltrations were observed in the corpora cavernosa, extending all the way to the root of the penis. The patient underwent a CT scan, which showed irregular accumulation of contrast in the penis without distant metastases (Figure 1). The patient was discussed by a multidisciplinary team, and it was decided to treat the patient by performing an amputation of the penis. Pathological examination of the resected specimen revealed the penile metastasis of low-grade (G2) adenocarcinoma of the colon with lymphovascular invasion and visible tumor structures in the resection margins (R1). Histologically, tumor was composed of irregular glandular and cribriform structures lined with columnar cells with eosinophilic cytoplasm and polymorphic-stratified nuclei. The tumor contained abundant necrotic debris (“dirty necrosis”) in the lumen of the structures. The tumor was located in penile glans and corpus, spreading to both corpus spongiosum and cavernosum, infiltrating surrounding adipose and striated muscle tissues. Perineural and lymphovascular invasions were observed as well. Immunohistochemically, the tumor cells were positive for CDX2, which is a marker of the intestinal epithelium and helps to determine the primary location of metastatic colorectal adenocarcinomas (Figures 2–5). The patient was scheduled for adjuvant chemotherapy with XELOX regimen with a reduced dose of Capecitabine because of the DPYD gene polymorphism heterozygous variant. Almost 3 months after the operation, hematuria occurred, and then suprapubic cystostomy was performed. Later, the patient complained of severe pain in his right leg, and x-ray with bone scintigraphy imaging tests showed osteolytic-type metastases, and massive bone damage with tumor masses in both legs (Figure 2). Due to the progression of the disease while on chemotherapy and deteriorating general condition of the patient, it was decided to apply symptomatic (palliative) treatment. The patient died 3 months later (see the timeline in Figure 6).
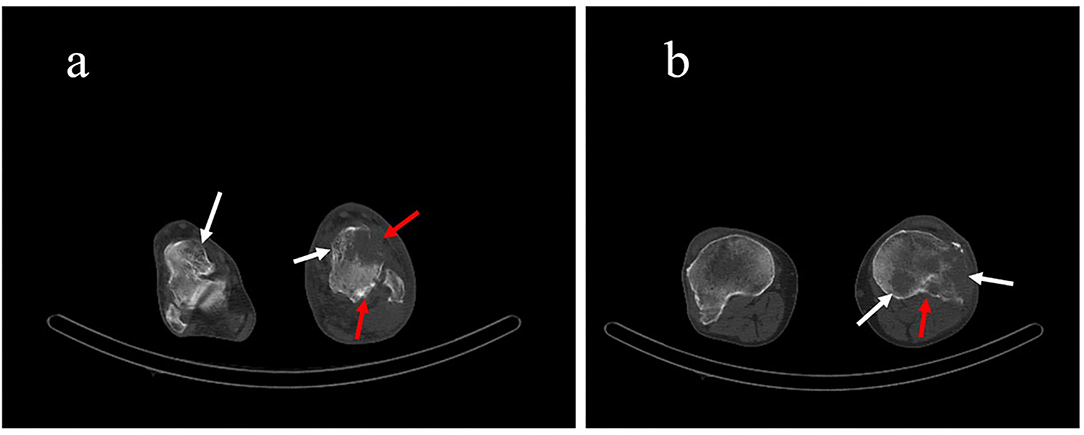
Figure 1. (a) Axial and (b) sagittal computed tomography scan planes, showing irregular accumulation of contrast in the penis without distant metastases (white arrows).
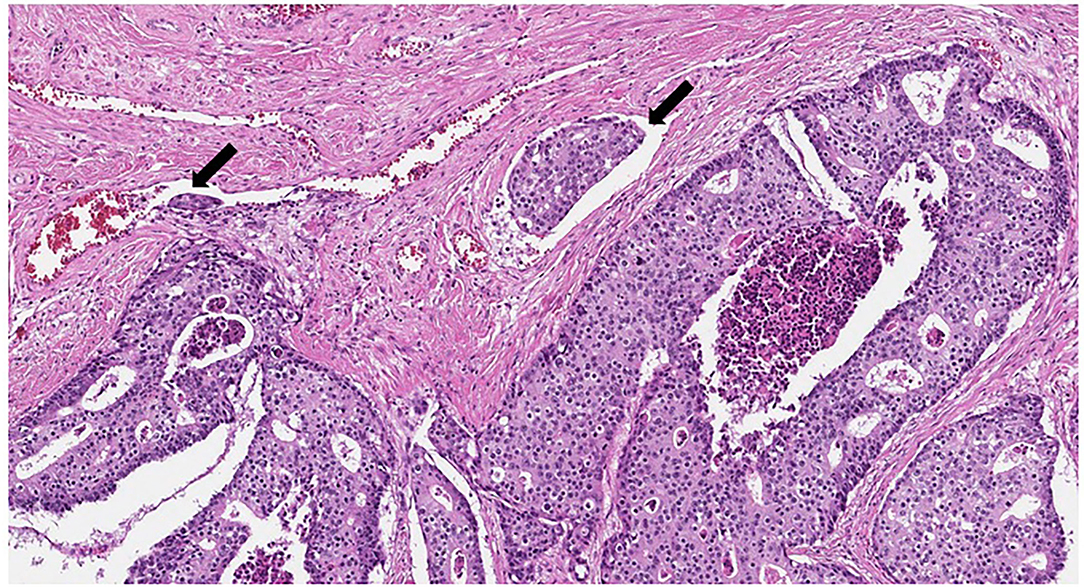
Figure 4. Cribriform tumor structures with dirty necrosis. Lymphovascular invasion (marked with arrows) (HE, original magnification ×100).
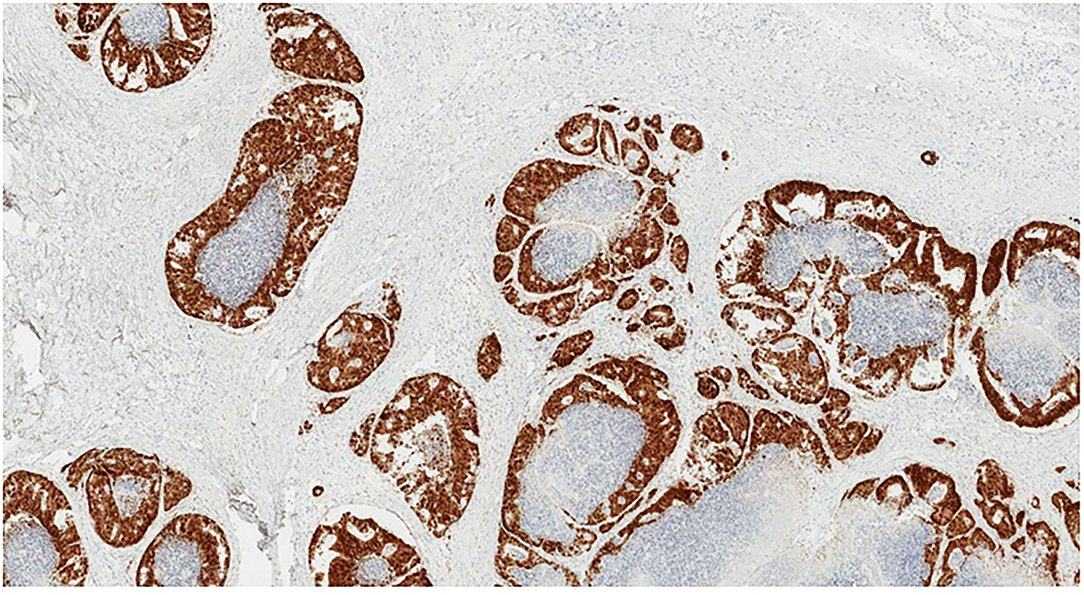
Figure 5. CDX2 immunohistochemistry. Positive nuclear staining in tumor cells (original magnification ×40).
Here, we present a rare case of rectal cancer metastasis to penis with fast deterioration and an unfavorable ending.
The location of the penis is closely surrounded by other anatomical structures, which are often the sites of origin of primary tumors. Moreover, sufficient blood flow of the penis is ensured by an abundant amount of vascular structures (71). However, despite these factors, metastatic involvement of the penis is extremely rare (14, 65, 72, 73). So far, only 72 cases have been described in the literature (Table 1). The most common sites of origin include the bladder, prostate, rectum (as in our and previous cases), and kidneys (65, 73, 74). To this day, it has not been entirely clear how primary tumors metastasize to the penis. The literature indicates several possible ways of primary tumors spread to the penis (73, 75, 76), such as direct extension, retrograde venous metastasis, retrograde lymphatic metastasis, direct extension into arterial pathways, spread by instrumentation, secondary, tertiary or paradoxical embolism (the retrograde venous mechanism is considered as the main pathway of tumor spread to the penis) (73, 75, 76). In our case, it is not entirely clear which of these mechanisms played the main role. We consider that retrograde venous or lymphatic mechanisms are most likely because the patient was diagnosed with rectal adenocarcinoma metastasing to the regional lymph nodes(ypT2N1b).
According to our review, the mean patients' age presenting with penile metastases is 62 years. Moreover, our findings are consistent with data from other studies, indicating that, on average, penile metastases occur 2–3 years (in our findings – 27 months), following the treatment of the primary tumors (27, 67). Clinical presentation consists of nodules, masses or induration of the penis, lesions/ulcerations, priapism, urination problems, penile or perineal pain (67, 73, 75–77). We found that the most common initial signs and symptoms were nodules and urination difficulties. The diagnosis of penile metastasis can be confirmed histologically by performing biopsy or fine-needle aspiration (73). Other noninvasive diagnostic tests, such as ultrasound scan, magnetic resonance imaging or computed tomography scan, could be informative and can help to detail local margins of the tumor as well as to visualize systemic dissemination of the disease (73). In our case, the patient was 64 years old, and was presented with penile pain, solid formations, and rough and raised tumor 3 years after the treatment of rectal cancer. We used CT scan with contrast to detail the possible spread of the tumor. We did not perform pelvic MRI because of the degree of presented symptoms. The patient needed urgent surgery for pain management and urinary dysfunction.
As this entity is very rare, there are no international or national treatment guidelines. Possible treatment modalities alone or in combinations include local excision of the tumor, total penectomy, chemotherapy, radiotherapy, and palliative treatment only (14, 39, 50, 67, 69). In our review, chemotherapy (alone or in combination with radiotherapy or surgical treatment) was the most often suggested treatment. Other studies suggest that radical surgical treatment could be the best option for patient survival improvement. However, the current data are lacking (14, 22, 67). Most commonly, penile metastases accompany systemic spread, and only palliative treatment is possible to improve the patient's quality of life. One should keep in mind that radical surgical treatment will definitely worsen the quality of life (38, 67). In our case, we initially treated the patient by performing total penectomy and prescribing adjuvant chemotherapy as he presented with painful masses and urinary dysfunction. However, the disease progressed instantly, and the patient then was scheduled for palliative care only.
Despite possible radical treatment modalities, such as total penectomy, the prognosis of patients with penile metastases is poor. Usually, penile metastases indicate widespread oncological disease, and the survival of these patients ranges from a few to several months only (4, 14, 27, 38, 67). Of the 72 cases reviewed, 31 patients had systemic spread of the disease at the time of the diagnosis of penile metastasis. It is important to note that not all authors provided information on the systemic spread of the disease, so the actual number of cases with disseminated pathology may be higher. The average survival from the time of the diagnosis of penile metastasis was about 9 months. Our patient developed metastases to the bones almost 3 months after total penectomy, and the overall survival of the patient was 6 months following amputation of penis.
To conclude, penile metastases from rectal cancer are extremely rare, indicating wide dissemination of the oncological process with a very poor prognosis. Aggressive surgical treatment is doubtful in metastatic disease as this will negatively affect the quality of the patient's life.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by National Cancer Institute Review Board. The patients/participants provided their written informed consent to participate in this study.
AD and AP conceived the idea. AK and AD wrote the article draft. RZ, MK, VS, AD, and AK performed the literature search. VS performed the analysis of the data. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
2. Riihimäki M, Hemminki A, Sundquist J, Hemminki K. Patterns of metastasis in colon and rectal cancer. Sci Rep. (2016) 6:29765. doi: 10.1038/srep29765
3. Eberth CJ. Krebsmetastasen des Corpus cavernosum penis. Arch Für Pathol Anat Physiol Für Klin Med. (1870) 51:145–6. doi: 10.1007/BF01879422
4. Cattell RB, Mace AJ. Metastasis to the penis from carcinoma of the rectum. J Am Med Assoc. (1951) 146:1230–1. doi: 10.1001/jama.1951.63670130010012e
5. Bowersox WA, Frerichs JB. Adenocarcinoma of the colon with primary complaint of tumor of penis; report, with considerations of mode of occurrence. J Urol. (1952) 68:897–902. doi: 10.1016/S0022-5347(17)68300-9
6. Poutasse EF. Metastasis to the penis: report of four cases. J Urol. (1954) 72:1196–200. doi: 10.1016/S0022-5347(17)67732-2
7. Boyd HL. Metastatic carcinoma of the penis secondary to carcinoma of the rectum: a review of the literature and report of a case. J Urol. (1954) 71:82–90. doi: 10.1016/S0022-5347(17)67760-7
8. Oehlschlaegel G. [The corpora cavernosa penis as a site for secondary tumor seeding in cancer of the rectum]. Z Haut Geschlechtskr. (1966) 41:425–9.
9. Tagart RE. Secondary deposit of rectal carcinoma in the penis. Proc R Soc Med. (1967) 60:501. doi: 10.1177/003591576706000524
10. Pond HS, Wade JC. Urinary obstruction secondary to metastatic carcinoma of the penis: a case report and review of the literature. J Urol. (1969) 102:333–5. doi: 10.1016/S0022-5347(17)62140-2
12. Bachrach P, Dahlen CP. Metastatic tumors to the penis. Urology. (1973) 1:359–62. doi: 10.1016/0090-4295(73)90287-2
13. Selikowitz SM, Olsson CA. Metastatic urethral obstruction. Arch Surg. (1973) 107:906–8. doi: 10.1001/archsurg.1973.01350240070020
14. Rees BI. Secondary involvement of the penis by rectal cancer. Br J Surg. (1975) 62:77–9. doi: 10.1002/bjs.1800620118
15. Baron M, Pinck BD. Penile metastasis from carcinoma of the rectum. J Med Soc N J. (1979) 76:444–5.
17. Zanetti PP, Calabrò B, Gagna G, Obialero M, Peradotto F, Rosa G, et al. [Metastasis to the corpus cavernosum of the penis from a rectal cancer]. Minerva Urol. (1983) 35:69–71.
18. Okumura S, Hirasawa S, Yui Y, Yoshida K, Nishimura T, Akimoto M. [A clinical case of secondary tumor of the penis from the rectum, with malignant priapism]. Hinyokika Kiyo. (1984) 30:205–15.
19. Honda M, Kameoka H, Miyoshi S, Iwao N, Mizutani S. [Secondary penile tumors: report of two cases]. Hinyokika Kiyo. (1985) 31:2273–9.
20. Khubchandani M. Metachronous metastasis to the penis from carcinoma of the rectum. Report of a case. Dis Colon Rectum. (1986) 29:52–4. doi: 10.1007/BF02555289
21. Mukamel E, Farrer J, Smith RB. deKernion JB. Metastatic carcinoma to penis: when is total penectomy indicated? Urology. (1987) 29:15–8. doi: 10.1016/0090-4295(87)90589-9
22. Haddad FS, Manne RK. Involvement of the penis by rectocolic adenocarcinoma: report of a case and review of the literature. Dis Colon Rectum. (1987) 30:123–9. doi: 10.1007/BF02554950
23. Doré B, Grange P, Aubert J. [Penile metastasis disclosing cancer of the rectum. Apropos of a case]. Ann Urol. (1989) 23:158–60.
24. Comandone A, Bau G, Mo A, Bretti S, Alberghina A, Frigerio A, et al. [Metastasis to the penis from carcinoma of the rectum. A clinical case]. Minerva Gastroenterol Dietol. (1992) 38:49–52.
25. Ben-Yosef R, Kapp DS. Cancer metastatic to the penis: treatment with hyperthermia and radiation therapy and review of the literature. J Urol. (1992) 148:67–71. doi: 10.1016/S0022-5347(17)36512-6
26. Kupfer HW, Theunissen P, Delaere KP. Urethral metastasis from a rectal carcinoma. Acta Urol Belg. (1995) 63:31–2.
27. Cuvillier X, Donnaint A, Rigot JM, Mazeman E. [Report of a case of penile metastasis. Review of the literature] Prog Urol. (1995) 5:1009–11.
28. Lange G, Fagot H, Faulques B, Hoepffner JL, Lange S. [Penile metastasis of recto-sigmoid adenocarcinoma. Apropos of a case]. Ann Chir. (1997) 51:294–6.
29. Al-Mashat F, Sibiany A, Rakha S, Olumide F. Penile metastasis from rectal carcinoma. Saudi Med J. (2000) 21:379–81.
30. Sukumar N, Qureshi A. Adenocarcinoma of rectum metastasizing to penis. Med J Malaysia. (2001) 56:255–6.
31. Tan BKT, Nyam DCNK, Ho YH. Carcinoma of the rectum with a single penile metastasis. Singapore Med J. (2002) 43:39–40.
32. Yilmaz E, Batislam E, Altinok G, Altinok D, Kara S, Başar M. Isolated late penile metastasis of an adenocarcinoma of the rectum. Urol Int. (2004) 72:261–3. doi: 10.1159/000077127
34. Cathomas R, Geldart TR, Iveson T, Singh N, Rowen D. An unusual differential diagnosis of penile warts: metastases from rectal carcinoma. Int J STD AIDS. (2006) 17:491–2. doi: 10.1258/095646206777689107
35. Appu S, Lawrentschuk N, Russell JM, Bright NF. Metachronous metastasis to the penis from carcinoma of the rectum. Int J Urol Off J Jpn Urol Assoc. (2006) 13:659–61. doi: 10.1111/j.1442-2042.2006.01379.x
36. Añibarro Laca E, Pérez-Irezabal Pindado JC, Ibáñez Calle T, Llarena Ibarguren R. [Metastases from a rectal adenocarcinoma to the prepuce]. Arch Esp Urol. (2006) 59:737–9. doi: 10.4321/S0004-06142006000700011
37. Pellicé i Vilalta C. [Subcutaneous prepuce metastasis secondary to rectal adenocarcinoma]. Arch Esp Urol. (2006) 59:926–7.
38. Cherian J, Rajan S, Thwaini A, Elmasry Y, Shah T, Puri R. Secondary penile tumors revisited. Int Semin Surg Oncol. (2006) 3:33. doi: 10.1186/1477-7800-3-33
39. Ketata S, Boulaire JL, Soulimane B, Bargain A. metachronous metastasis to the penis from a rectal adenocarcinoma. Clin Colorectal Cancer. (2007) 6:657–9. doi: 10.3816/CCC.2007.n.035
40. Murhekar KM, Majhi U, Mahajan V, Satheesan B. Penile metastasis from rectal carcinoma. Indian J Cancer. (2007) 44:155–6. doi: 10.4103/0019-509X.39378
41. Chung T-S, Chang HJ, Kim DY, Jung KH, Lim S-B, Choi HS, et al. Synchronous penile metastasis from a rectal carcinoma. Int J Colorectal Dis. (2008) 23:333–4. doi: 10.1007/s00384-007-0383-y
42. Küronya Z, Bodrogi I, Lövey J, Plótár V, Manninger S, Pápai Z. [Metachronous metastasis from rectal adenocarcinoma to the penis-case report]. Magy Onkol. (2009) 53:263–6. doi: 10.1556/MOnkol.53.2009.3.5
43. Park JC, Lee WH, Kang MK, Park SY. Priapism secondary to penile metastasis of rectal cancer. World J Gastroenterol. (2009) 15:4209–11. doi: 10.3748/wjg.15.4209
44. Yildirim M, Coskun A, Pürten M, Oztekin O, Ilhan E. A clinical case of the penile metastasis from the rectal carcinoma. Radiol Oncol. (2010) 44:121–3. doi: 10.2478/v10019-010-0004-1
45. ER M-M, Enrique N-G, Medina A-Z, Alberto C-G, Eduardo T-M., A V-CM, et al. Adenocarcinoma of the rectum with metastasis to the penis. Rev Mex Urol. (2010) 70:312–4.
46. Lee JI, Kang WK, Kim HJ, Kim SH, Oh ST. Unusual metastasis from a rectal adenocarcinoma: penile metastasis. ANZ J Surg. (2011) 81:102. doi: 10.1111/j.1445-2197.2010.05623.x
47. Goris Gbenou MC, Wahidy T, Llinares K, Cracco D, Perrot A, Riquet D. Atypical phimosis secondary to a preputial metastasis from rectal carcinoma. Case Rep Oncol. (2011) 4:542–6. doi: 10.1159/000334747
48. Maestro MA, Martínez-Piñeiro L, Moreno SS, Rodríguez JD, Quevedo AL. Penile metastasis of rectal carcinoma. Case report and bibliographic review. Arch Esp Urol. (2011) 64:981–4.
49. Dorsett F, Hou J, Shapiro O. Metastasis to the penis from rectal adenocarcinoma. Anticancer Res. (2012) 32:1717–9.
50. Kimura Y, Shida D, Nasu K, Matsunaga H, Warabi M, Inoue S. Metachronous penile metastasis from rectal cancer after total pelvic exenteration. World J Gastroenterol. (2012) 18:5476–8. doi: 10.3748/wjg.v18.i38.5476
51. McGuinness LA, Floyd MS, Lucky M, Parr NJ. Penile metastases treated with partial glansectomy and adjuvant radiotherapy 5 years after an initial diagnosis of rectal cancer. BMJ Case Rep. (2013) 2013:bcr2013200829. doi: 10.1136/bcr-2013-200829
52. Persec Z, Persec J, Sovic T, Rako D, Savic I, Marinic DK. Penile metastases of rectal adenocarcinoma. J Visc Surg. (2014) 151:53–5. doi: 10.1016/j.jviscsurg.2013.08.009
53. Papaefthymiou V, Hall A, Ladoyanni E. Metachronous metastasis to glans penis from colorectal cancer. Austin J Dermatolog. (2014) 1:1002.
54. Luo N-Q, Zhang Z-H, Ma Y. [Penile metastasis from rectal carcinoma: a case report and literature review]. Zhonghua Nan Ke Xue Natl J Androl. (2014) 20:359–62.
55. Hajianfar R, Muniesa M, Gomez E, Belles F, Pallisera A, Ortiz de. Zarate L. Metastasis of rectal adenocarcinoma to the penis. Arch Esp Urol. (2014) 67:353–6.
56. Chang C-F, Hsu S-N, Chien S-T, Wang C-T, Ni Y-J, Hsu C-W, et al. Urethral metastasis from rectal adenocarcinoma: a case report and review of the literature. Low Urin Tract Symptoms. (2015) 7:162–5. doi: 10.1111/luts.12069
57. Cholin L, Perz S, Mahmood F, Zafar S. Palpable penile metastases: a bizarre presentation of rectal adenocarcinoma. Case Rep Urol. (2015) 2015:876464. doi: 10.1155/2015/876464
58. Brønserud MM, Sørensen FB, Rahr H, Osther PJS. [Penile metastasis from rectum cancer primarily interpreted as Peyronie's disease]. Ugeskr Laeger. (2015) 177:120–1.
59. Alzayed MF, Artho G, Nahal A, Hickeson M. Penile metastasis from rectal cancer by PET/CT. Clin Nucl Med. (2015) 40:e245–250. doi: 10.1097/RLU.0000000000000635
60. Delto JC, Morlote D, Recine MA, Bhandari A. A Case of Colon Cancer Metastasis to the Penis. Urology. (2015) 86:16–8. doi: 10.1016/j.urology.2015.02.003
61. Nunes B, Matias M, Alves A, Jorge M. Metastasis to the glans penis: an unusual site of rectal cancer recurrence. Acta Med Port. (2015) 28:525–7. doi: 10.20344/amp.5775
62. Fabiani A, Filosa A, Fioretti F, Mammana G. Penile plaque as predictor of an advanced anorectal carcinoma: a case report. Arch Ital Urol Androl Organo Uff Soc Ital Ecogr Urol E Nefrol. (2015) 87:171–2. doi: 10.4081/aiua.2015.2.171
63. Christodoulidou M, Sahdev V, Muneer A, Nigam R. A rare case of metachronous penile and urethral metastases from a rectal mucinous adenocarcinoma. BMJ Case Rep. (2015) 2015:bcr2015212706. doi: 10.1136/bcr-2015-212706
64. Kozan AA, Smith AM, Ilsley DW, Rhodes N. First case of penile metastasis following abdominoperineal resection with VRAM flap reconstruction. J Surg Case Rep. (2016) 2016:rjw182. doi: 10.1093/jscr/rjw182
65. Gómez-de la Fuente F-J, Martínez-Rodríguez I, Alonso-Martín J, Jiménez-Bonilla J, Banzo I. A case report of penile metastases from rectal carcinoma. Cir Esp Engl Ed. (2017) 95:116–8. doi: 10.1016/j.cireng.2017.03.009
66. Efared B, Ebang GA, Tahirou S, Tahiri L, Sidibé IS, Erregad F, et al. Penile metastasis from rectal adenocarcinoma: a case report. BMC Res Notes. (2017) 10:564. doi: 10.1186/s13104-017-2901-5
67. Kuliavas J, Dulskas A, Drachneris J, Miseikyte-Kaubriene E, Samalavicius NE. Penile Metastasis from Rectal Carcinoma: Case Report and Review of the Literature. Visc Med. (2018) 34:389–92. doi: 10.1159/000491594
68. Marghich O, Dkhissi Y, Alila M, El Bouhaddouti H. Penile metastases of rectal adenocarcinoma after abdominoperineal resection: a case report. J Med Case Reports. (2019) 13:233. doi: 10.1186/s13256-019-2147-z
69. Lee T-G, Son S-M, Kim MJ, Lee S-J. Penile metastasis in rectal cancer with pathologic complete response after neoadjuvant chemoradiotherapy. Medicine. (2020) 99:e21215. doi: 10.1097/MD.0000000000021215
70. Zang S, Yang Y. Isolated penile metastasis from rectal carcinoma after abdominoperineal resection: a case report and review of the literature. ANZ J Surg. (2021) 91:E411–2. doi: 10.1111/ans.16432
71. Sam P, LaGrange CA. Anatomy, Abdomen and Pelvis, Penis. In: StatPearls. Treasure Island (FL): StatPearls Publishing (2021) [cited 2021 Oct 25]. Available online at: http://www.ncbi.nlm.nih.gov/books/NBK482236/ (accessed November 15, 2021).
72. Bates AW, Baithun SI. Secondary tumors of the penis. J R Soc Med. (2002) 95:162–3. doi: 10.1258/jrsm.95.3.162-a
73. Mearini L, Colella R, Zucchi A, Nunzi E, Porrozzi C, Porena M, et al. review of penile metastasis. Oncol Rev. (2012) 6:10. doi: 10.4081/oncol.2012.e10
74. Hizli F, Berkmen F. Penile metastasis from other malignancies. Urol Int. (2006) 76:118–21. doi: 10.1159/000090872
75. Paquin AJ Jr, Roland SI. Secondary carcinoma of the penis. A review of the literature and a report of nine new cases. Cancer. (1956) 9:626–32. doi: 10.1002/1097-0142(195605/06)9:3<626::AID-CNCR2820090330>3.0.CO;2-C
76. Abeshouse BS, Abeshouse GA. Metastatic tumors of the penis: a review of the literature and a report of two cases. J Urol. (1961) 86:99–112. doi: 10.1016/S0022-5347(17)65117-6
Keywords: penile metastasis, rectal cancer, corpus spongiosum, case report, literature review
Citation: Kaminskas A, Patasius A, Kincius M, Sapoka V, Zilevicius R, Garnelytė A and Dulskas A (2022) A Case Report and Review of the Literature of Penile Metastasis From Rectal Cancer. Front. Surg. 9:814832. doi: 10.3389/fsurg.2022.814832
Received: 14 November 2021; Accepted: 01 April 2022;
Published: 09 May 2022.
Edited by:
Yanwu Sun, Fujian Medical University Union Hospital, ChinaReviewed by:
Xiaojie Wang, Fujian Medical University, ChinaCopyright © 2022 Kaminskas, Patasius, Kincius, Sapoka, Zilevicius, Garnelytė and Dulskas. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Audrius Dulskas, YXVkcml1cy5kdWxza2FzQGdtYWlsLmNvbQ==; orcid.org/0000-0003-3692-8962
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.