- Department of Urology, Institute of Urology, West China Hospital, Sichuan University, Chengdu, China
Background: Ureteroscopy (URS) has been established as an effective treatment for stones in obese patients (OP). However, recent studies found that the efficacy of the procedure may be lower in patients with higher body mass index (BMI). In the current study, we aim to determine if obesity might influence the effectiveness and safety of URS.
Methods: In May 2021, a comprehensive search was conducted in the PubMed, EMBASE, Web of Science, Cochrane Library, and ClinicalTrials.gov to find eligible studies. Stone-free rate (SFR), operative time, length of stay, and complication rate were assessed utilizing RevMan 5.3.
Results: Thirteen studies involving 4,583 normal-weight patients (NWP), 2,465 OP, and 291 morbidly OP (MOP) were included. Pooled results showed that statistically similar SFR existed between OP and NWP [odds ratio (OR): 1.09; 95% CI: 0.79, 1.52; p = 0.59], and between MOP and NWP (OR: 1.03; 95% CI: 0.46, 2.31; p = 0.95). The operation time was similar between OP and NWP [mean difference (MD): −2.27; 95% CI: −8.98, 4.43; p = 0.51], and between MOP and NWP (MD: 4.85; 95% CI: −5.78, 15.47; p = 0.37). In addition, no significant difference regarding length of stay existed between OP and NWP (MD: −0.07; 95% CI: −0.20, 0.07; p = 0.33), and between MOP and NWP (MD: −0.06; 95% CI: −0.25, 0.14; p = 0.58). Furthermore, we observed similar minor complication rate between OP and NWP (OR: 1.04; 95% CI: 0.81, 1.32; p = 0.78), and between MOP and NWP (OR: 1.29; 95% CI: 0.80, 2.08; p = 0.30). The differences concerning major complication rate between OP and NWP (OR: 0.97; 95% CI: 0.39, 2.43; p = 0.95), and between MOP and NWP (OR: 2.01; 95% CI: 0.55, 7.30; p = 0.29) were also not significant.
Conclusions: Our study demonstrated that URS performed in MOP and OP appears to have the same efficacy and safety as well as in NWP group.
Introduction
Currently, the worldwide epidemic, obesity, and overweight affect one-third population of the world (1). The obesity rate has increased in all ages, regardless of countries, regions, ethnicity, and socioeconomic status. Currently, the WHO gives a clear definition on normal weight: a body mass index (BMI) value <25 kg/m2; whereas a BMI value >30 kg/m2 is regarded as obese patients (OP), and a BMI value above 40 kg/m2 is morbidly OP (MOP) (1). Obesity impairs normal physiological functions of the body and substantially increases the risks for developing many medical problems, such as diabetes mellitus (2), angiocardiopathy (3), musculoskeletal diseases (4), and several kinds of cancers (5). Recently, many researches have demonstrated that obesity also raised the risks of urolithiasis (6–8). Possible mechanisms underlying the association are changes in renal acid/base handling (9), alterations in urine composition (8, 10), insulin resistance, and increased production of fatty acids (11).
Obesity poses a management challenge in terms of imaging, anesthesia, and surgical methods to urologists (12). Usually, urolithiasis is diagnosed by ultrasound and CT scan, but the increased thickness of fat tissue prevents acquiring a high-quality image, and some obese individuals might be unable to fit into the CT scanner due to excessive weight or abdominal circumference (12). Furthermore, anesthesia can induce several respiratory function alterations in the OP, such as the decrease in the functional residual capacity and respiratory compliance (13).
As for surgical options of the obese individuals with kidney stones, Extracorporeal Shock Wave Lithotripsy might not be a suitable procedure choice due to the farther skin-to-stone distance (12); for another treatment method, percutaneous nephrolithotomy, the standard prone position can increase the respiratory impairment and impedes venous blood flow in OP (14). All above-mentioned make ureteroscopy (URS) is the only feasible procedure. Recently, several studies have been published to evaluate the effectiveness of BMI on URS with controversial results (15–27). Some authors reported that stone-free rate (SFRs), complications, operation time, and length of stay were independent of BMI (15–23, 25–27), while Krambeck et al. showed the SFR of the URS procedure in obese individuals was lower compared with normal-weight patients (NWP) group (24). Therefore, we performed a meta-analysis, for the first time, to determine if obesity might influence the effectiveness and safety of URS with NWP controlled. We hope the results of the presented study could be helpful for urologists and their patients in decision-making process. This will definitely increase the chance to select the best method for our patients.
Methods
Search Strategy
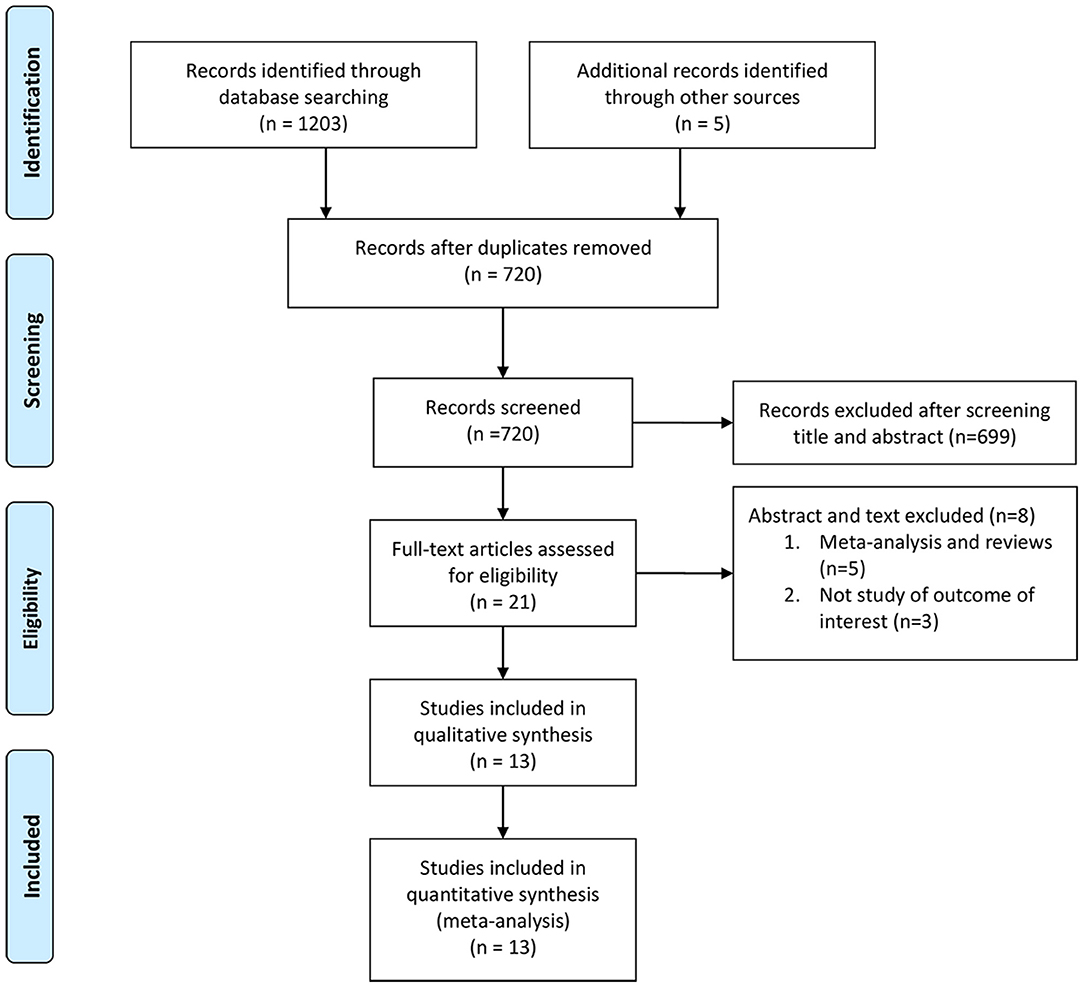
A comprehensive search in the PubMed, EMBASE, Web of Science, Cochrane Library, and ClinicalTrials.gov was conducted to find eligible studies before May 2021, following Cochrane standards and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (28). The language of publication was limited to English and conferences abstract were excluded. The following keywords were used: “endoscopy” or “ureteroscopy” or “lithotripsy” and “obese” or “obesity” or “body mass index” or “BMI” and “urolithiasis” or “calculi” or “stones.” The flowchart is presented in Figure 1. Additional studies were searched by the references of relevant articles.
Inclusion Criteria and Exclusion Criteria
All eligible articles were selected based upon: (1) researches presenting the outcomes of URS in the OP for urolithiasis and (2) references of included researches were also assessed for eligibility.
The exclusion criteria were: (1) data description was not clear enough; (2) non-English researches; and (3) studies published as review, case reports or comments.
Data Extraction
The following items were repeatedly extracted by two authors (WW and XSG): author, publication year, country, subgroup, age, number of patients, demographics, stone size, SFR (the definition of SFR was complete stone clearance or presence of residual fragment smaller than 4 mm by ultrasound, CT scan, intravenous pyelography [IVP] or a kidneys-ureters-bladder radiography after the initial procedure), operation time, length of stay, complications based on modified Clavien–Dindo classification system (29). Disagreements were solved by discussing with the third reviewer (XW).
Quality Assessment
WW and XSG assessed all included studies independently for methodological quality and levels of evidence (LE), and the disagreements were solved by discussion. The Oxford Center for Evidence-Based Medicine (30) was used to estimate the LE of each eligible study. We evaluated the methodological quality of the included reports on the basis of Newcastle Ottawa Scale (31). Additionally, Risk of Bias in Non-randomized Studies-of Interventions (ROBINS-I) was employed to identify the confounding factors for non-randomized studies (32).
Statistical Analysis
Analysis was performed to utilizing Review Manager Version 5.3 software. Dichotomous data were extracted to utilizing odds ratio (OR) and 95% CI, and continuous data were extracted by weighted mean difference (MD) and 95% CI. The p-value was calculated from the Z-test, and a p ≤ 0.05 was deemed as statistically significant. We assessed the heterogeneity of the included studies by Q and I2 statistics. The p-value lower than 0.1 and I2 value higher than 50% were considered as high heterogeneity among studies, and the random-effects model was performed; if not, indicated low heterogeneity, and the fixed-effects model was conducted. Sensitivity analysis was performed to utilizing a single-item removal method. We utilized a funnel plot to assess publication bias.
Results
Study Selection
On the basis of the literature search and the inclusion criteria, 1,208 studies were initially identified. Ultimately, 13 studies (15–27) were included in our analysis, with 4,583 NWP, 2,465 OP, and 291 MOP. Figure 1 shows the literature search and selection process.
Study Characteristics and Assessment of Quality
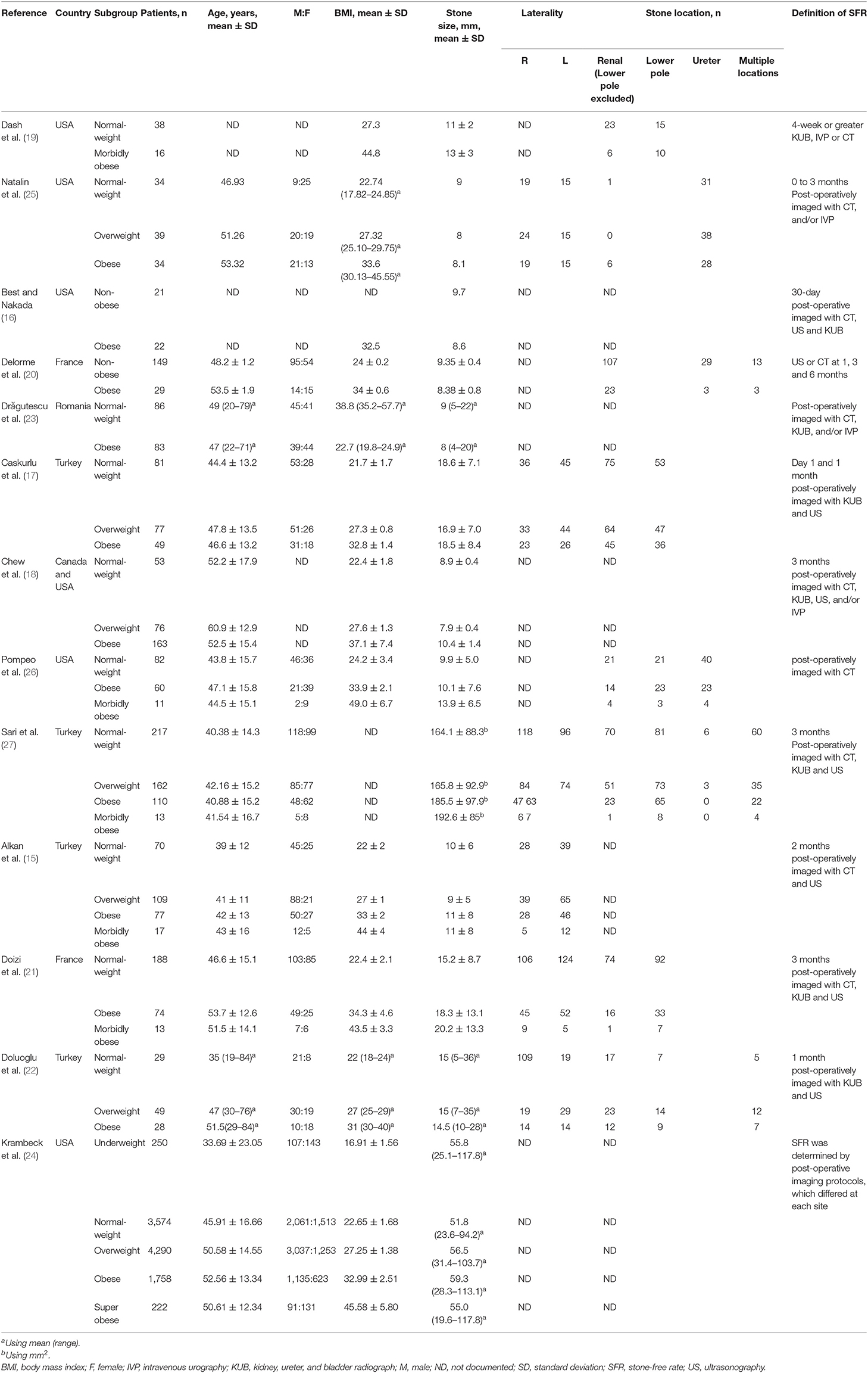
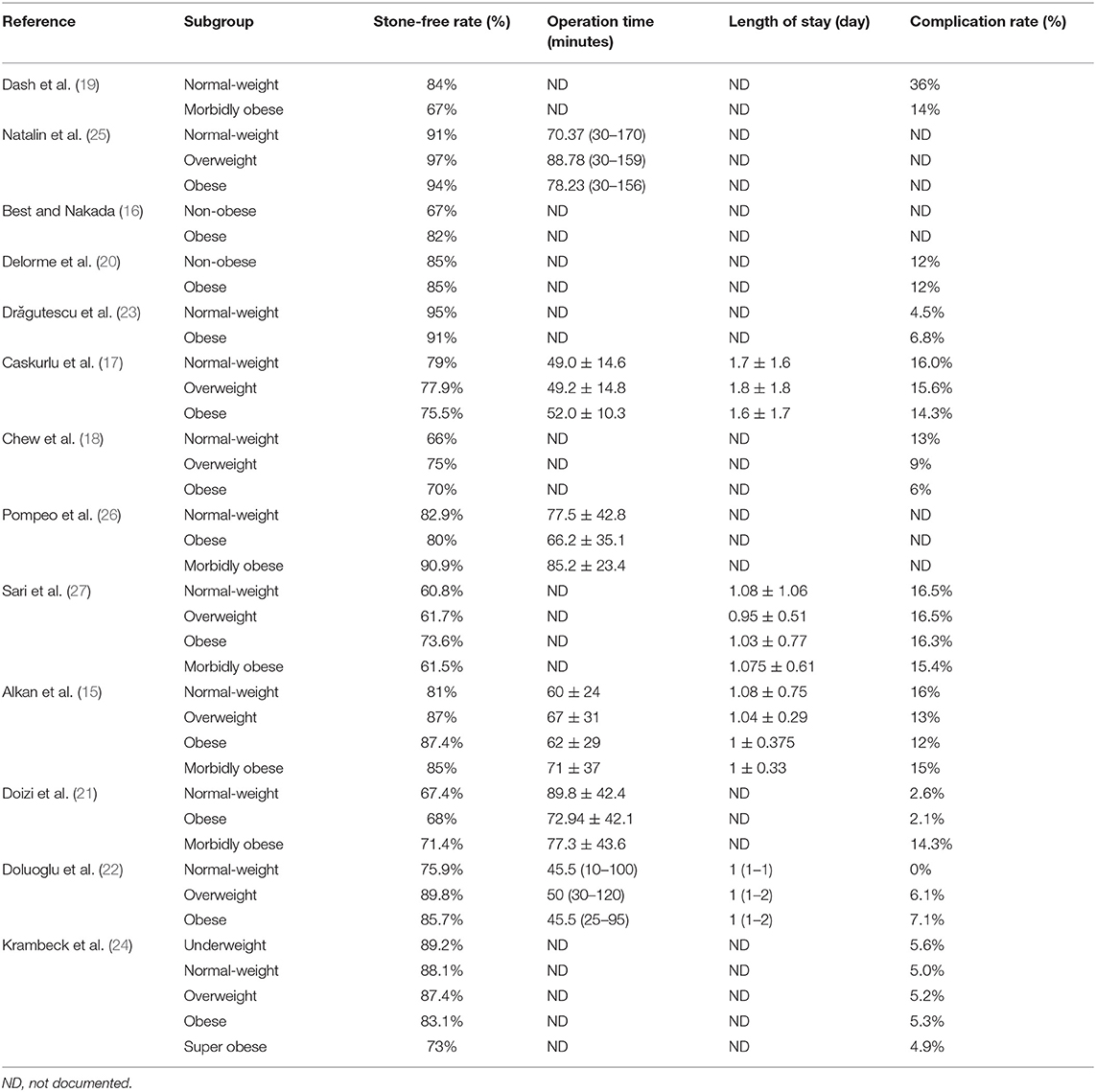
Thirteen studies (15–27) were finally included. All were retrospective and the LE of the eligible studies was 3b. Table 1 demonstrated the characteristics of the eligible research. Nine studies (15, 17, 19–22, 25–27) were presented the data regarding stone position, and no statistically difference regarding stone side (p = 0.184) and stone location (p = 0.061) was observed in the three different populations. There were more category 1 patients of American Society of Anesthesiology (ASA) in the normal weight group relative to the overweight and obese groups (18) (p < 0.0001). Predictably, there were more overweight and obese patients categorized as ASA 2 and ASA 3. Therefore, the ASA score is not similar between groups. Additionally, as shown in Table 1, the stone dimension was not different across the groups. Three included studies (16, 20, 21) were provided data regarding stone composition. Best and Nakada reported that nearly 80% of stones consisted of calcium oxalate and uric acid (16). Delorme et al. demonstrated that 64% of stones in OP were calcium oxalate and uric acid (20). Similarly, Doizi et al. revealed that 78% of stones in OP were composed of calcium oxalate and uric acid (21). In all patients, the flexible ureteroscope was advanced up to the kidney after insertion of a ureteral access sheath or guidewire. The outcome parameters of included studies are shown in Table 2. The methodological quality of eligible studies is demonstrated in Supplementary Table 1. The risk of bias of five non-randomized studies is displayed in Supplementary Table 2, and the overall risk of bias judgment of eligible studies was moderate to serious. We performed the forest plots to evaluate the effectiveness of URS for OP.
Stone-Free Rate
The 4,583 NWP, 2,465 OP, and 291 MOP were identified. As the heterogeneity was high between OP and NWP (p = 0.005, I2 = 59%) and between MOP and NWP (p = 0.005, I2 = 70%), we used the random-effects model, which indicates no statistically significant difference exist between OP and NWP (OR: 1.09; 95% CI: 0.79, 1.52; p = 0.59), and between MOP and NWP (OR: 1.03; 95% CI: 0.46, 2.31; p = 0.95; Figure 2).
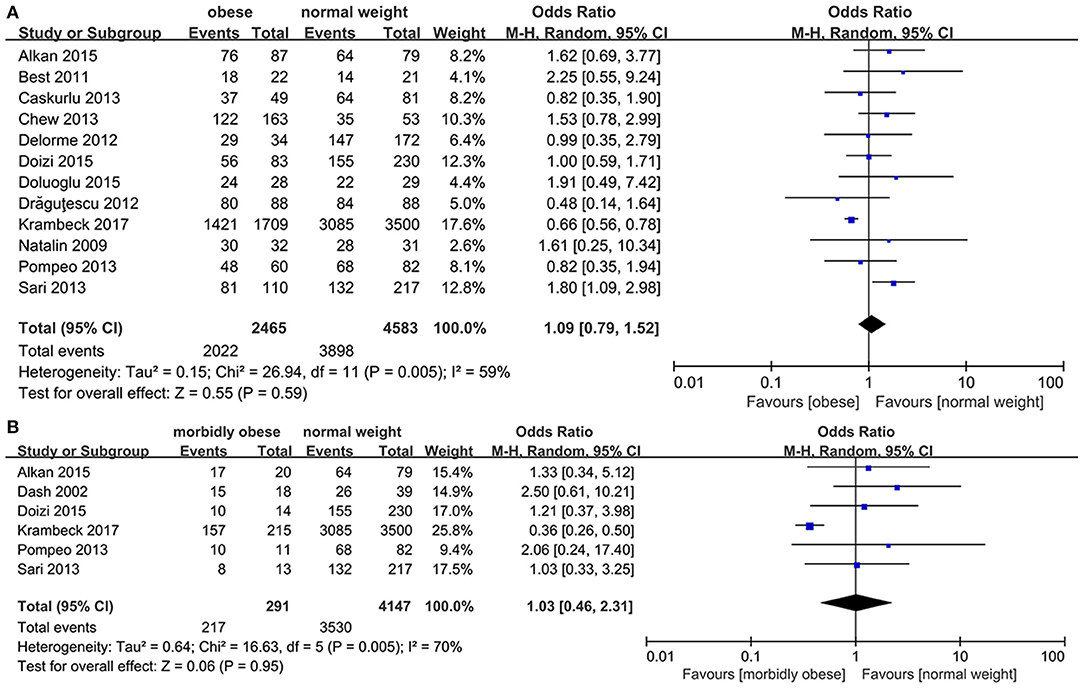
Figure 2. Forest plot of stone-free rate (SFR). (A) Obese vs. normal-weight. (B) Morbidly obese vs. normal-weight.
Operation Time
The three groups were compared concerning operative time. The heterogeneity was high between OP and NWP (p = 0.007, I2 = 68%), and the random-effects model demonstrated that the operation time was similar between two groups (MD: −2.27; 95% CI: −8.98, 4.43; p = 0.51).
As low heterogeneity exists between studies between MOP and NWP, we used the fixed-effects model, which revealed that the operating time was similar between two groups (MD: 4.85; 95% CI: −5.78, 15.47; p = 0.37; Figure 3).
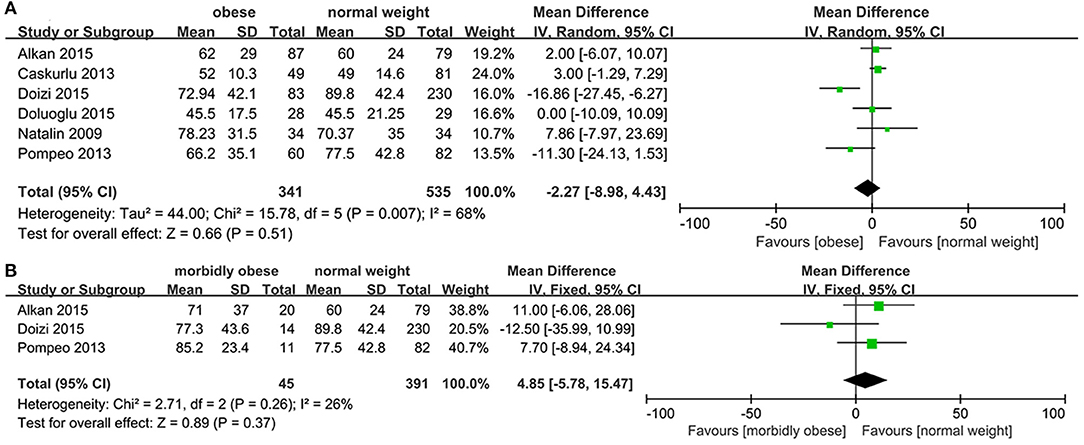
Figure 3. Forest plot of operation time. (A) Obese vs. normal-weight. (B) Morbidly obese vs. normal-weight.
Length of Stay
No heterogeneity was seen between OP and NWP (p = 0.97, I2 = 0%), and between MOP and NWP (p = 0.71, I2 = 0%), and the fixed-effects model revealed no statistically significant difference regarding length of stay between OP and NWP (MD: −0.07; 95% CI: −0.20, 0.07; p = 0.33), and between MOP and NWP (MD: −0.06; 95% CI: −0.25, 0.14; p = 0.58; Figure 4).
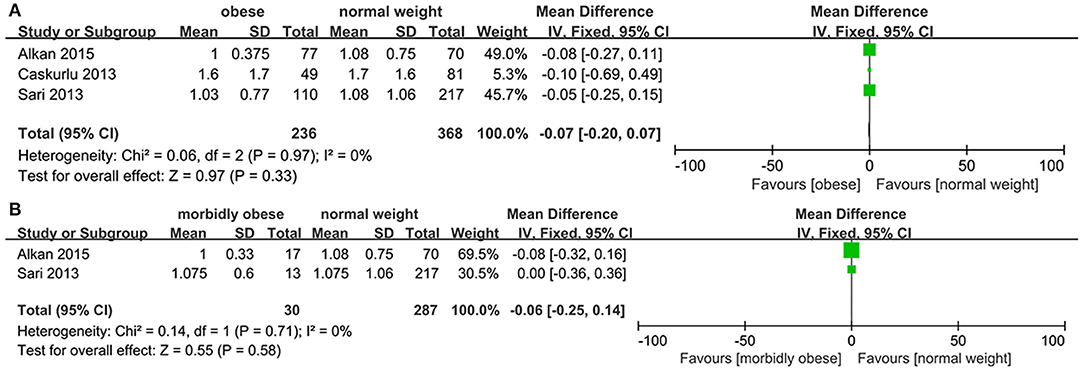
Figure 4. Forest plot of length of stay. (A) Obese vs. normal-weight. (B) Morbidly obese vs. normal-weight.
Complication Rate
Nine studies (15, 17, 18, 20–24, 27) were provided data regarding the complication rate between OP and NWP. The overall complication rate of MOP and OP was 8.3 and 5.1%, respectively. This is comparable to the complication rate of NWP (4.9%). The pooled result showed that the heterogeneity was low among these studies (p = 0.78, I2 = 0%), and fixed-effects model displayed that no statistically significant difference regarding the overall complication rate were observed between OP and NWP (OR: 1.03; 95% CI: 0.81, 1.31; p = 0.80; Figure 5A). Additionally, no statistically significant difference concerning the minor complications (OR: 1.04; 95% CI: 0.81, 1.32; p = 0.78) and the major complications (OR: 0.97; 95% CI: 0.39, 2.43; p = 0.95; Figure 5A) were found between OP and NWP.
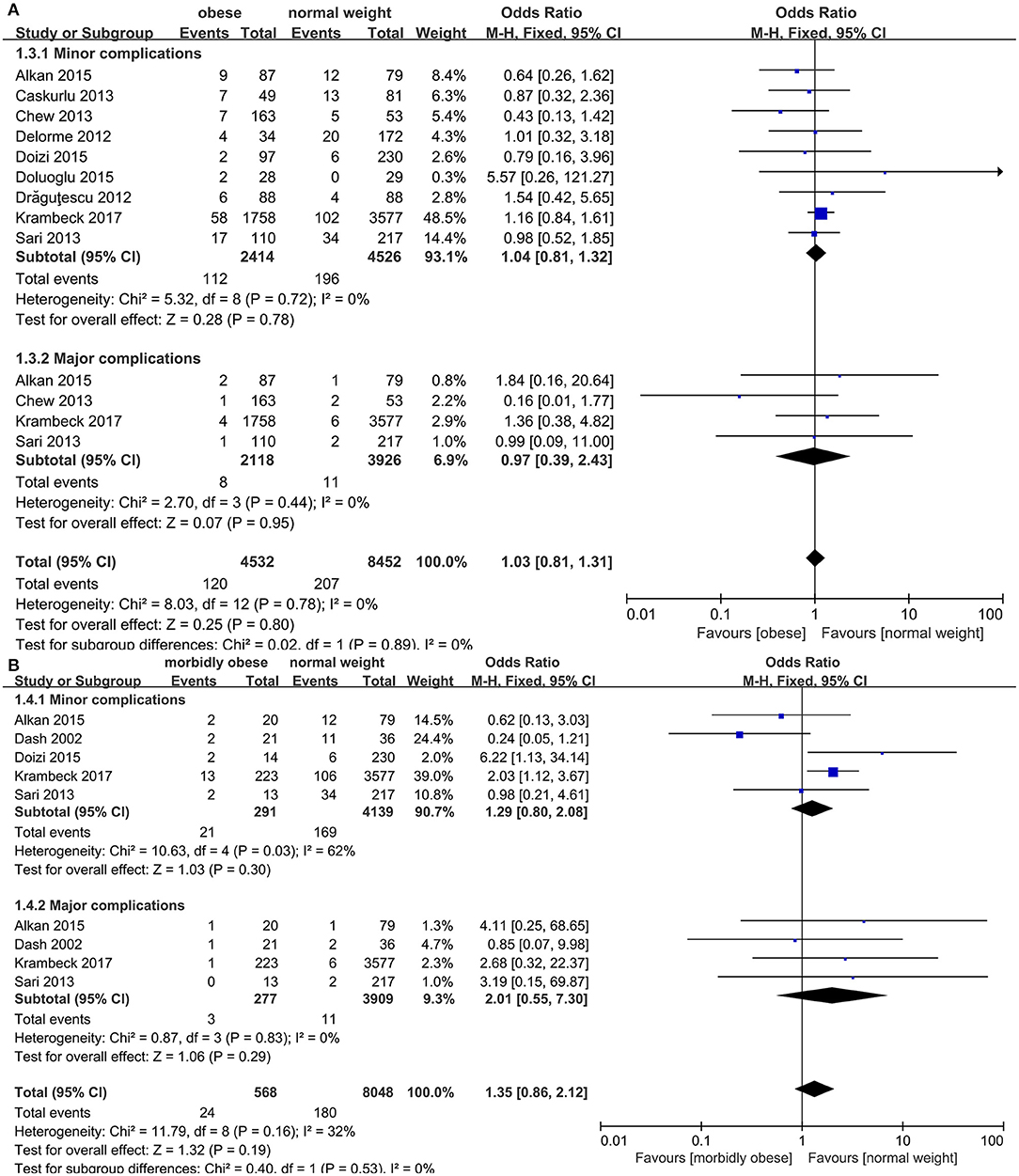
Figure 5. Forest plot of complication rate. (A) Obese vs. normal-weight. (B) Morbidly obese vs. normal-weight.
Five studies (15, 19, 21, 24, 27) were providing data in terms of the complication rate among MOP and NWP. The heterogeneity was low (p = 0.16, I2 = 32%) and fixed-effect model revealed that the overall complication rate was similar between two groups (OR: 1.35; 95% CI: 0.86, 2.12; p = 0.19; Figure 5B). Moreover, no statistically significant difference concerning the minor complications (OR: 1.29; 95% CI: 0.80, 2.08; p = 0.30) and the major complications (OR: 2.01; 95% CI: 0.55, 7.30; p = 0.29; Figure 5B) were seen between MOP and NWP.
Sensitivity Analysis and Publication Bias
Sensitivity analysis was performed and demonstrated the stable results. When it was applied to SFR between OP and NWP, and between MOP and NWP, one study (24) was the main source for high heterogeneity; after removal of the study, no heterogeneity was seen and the results did not change. Similarly, one study (21) was the main reason for the high heterogeneity of operative time between OP and NWP; after excluding the study, the heterogeneity was declined significantly and the results were remained unchanged. We utilized a funnel plot to estimate publication bias, and the symmetrical distribution indicated no obvious existence of publication bias (Figure 6).
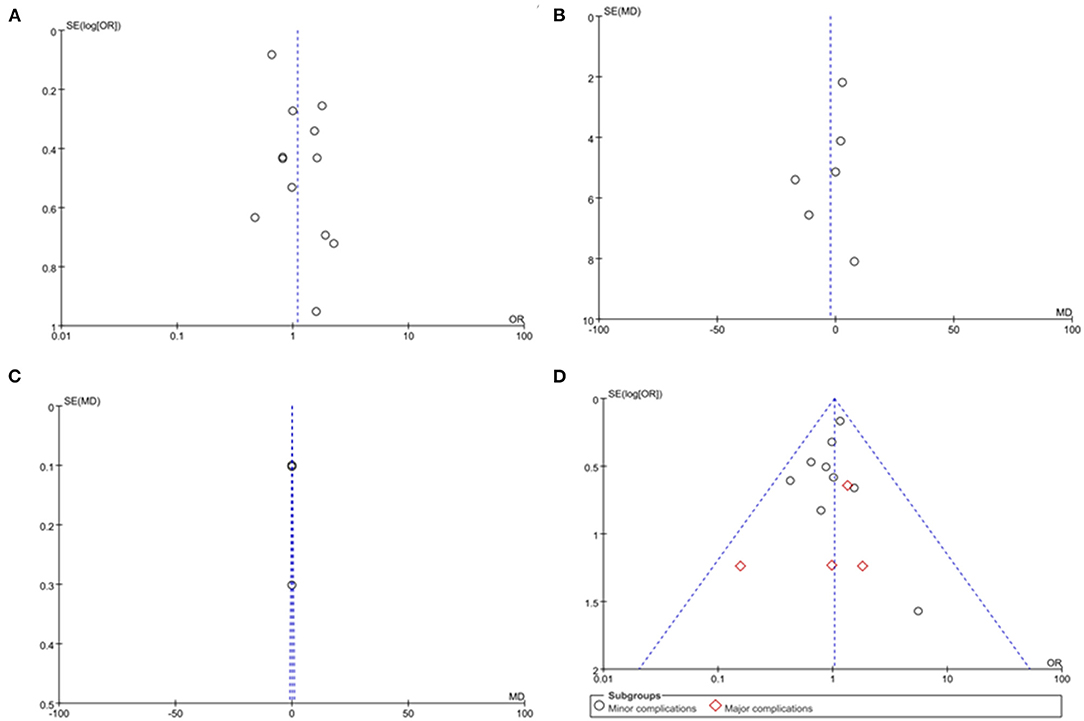
Figure 6. Funnel plot evaluating the publication bias. (A) Stone-free rate. (B) Operation time. (C) Length of stay. (D) Complication rate.
Discussion
The worldwide incidence of obesity is rapidly growing during the last decades. It is estimated that the number of OP grows from 400 million in 2005 to 700 million in 2015 (33). Obesity is related to many health problems such as diabetes mellitus (2), hypertension (3), cardiomyopathy (4), and prostate cancers (5). It is also well-documented that there exist is an association between obesity and a higher risk of urolithiasis (34). Scales et al. uncovered that the prevalence of urolithiasis in obese and normal-weight individuals was 11.2 and 6.1%, respectively (35). Studies reported that stones in OP mainly consisted of calcium oxalate and uric acid (36), which is consistent with our analysis. Insulin resistance caused by obesity might be the most important factor associated with urolithiasis. Strohmaier et al. reported that insulin resistance decreased the production and transportation of ammonia, leading to a low urine pH (37), whereas an acid urine pH facilitated the formation of uric acid stones (34). In contrast, calcium oxalate stones, as the most common composition of stones in OP, are hardly influenced by obesity. When faced with the OP with urolithiasis, urologists are likely to stick in a dilemma of how to manage these individuals because the removal of stones is risky and difficult. Due to cardiovascular, respiratory, and metabolic alteration, obese individuals are susceptible to perioperative comorbidities and increase morbidity (13). Therefore, it is recommended to use mini-invasive procedures rather than open surgery in obese individuals.
Technological development in endoscope equipment has prompted the emergence of smaller scope with a better angle of deflection and laser technology, which renders more efficacious stone fragmentation while retaining hemostasis. All these make URS an attractive procedure to manage urolithiasis (38). In our study, we comprehensively assessed the effectiveness and safety of URS on obese individuals with normal weight persons controlled. We noticed that no statistically significant difference existed between OP and NWP, and between MOP and NWP groups regarding SFR, complications, operation time, and length of stay, indicating that URS performed on OP and MOP is equally secure and efficacious to NWP.
Stone-free rate is a critical outcome variable to assess the effectiveness of endourological surgery. Chew et al. reported that MOP was associated with a relatively lower SFR compared with NWP (18). However, only eight MOPs were enrolled in their study. In addition, a study published by Krambeck et al., includes 11,885 patients concluded that the obesity was related to lower SFR and the efficacy of URS procedure was decreased compared with normal weight group (24). But the median stone burden in this study exceeded 50 mm in each group, which might significantly affect the SFR of URS procedure. Furthermore, the authors utilized the results of a multicenter study, in which SFR status differed at each site and was not clearly clarified (24). The reason why obesity has no influence on SFR in our analysis might be that the external fat tissue has no necessary connection with abnormal internal anatomy. In addition, URS procedure is performed by inserting the scope into the ureter, and this process is not influenced by increased retroperitoneal fat tissue. Specially, two included studies (19, 21) presented SFR in patients whose stone sizes were <10 mm. Dash et al. reported that the success rates for stones <10 mm were 100 and 69% in MOP and NWP groups, respectively. However, they did not observe a significant difference between two groups (p = 0.43). Similarly, Doizi et al. found that no significant differences regarding SFR for stones <10 mm existed between OP and NWP, and between MOP and NWP (93% SFR in NWP, 100% SFR in OP, and 100% SFR in MOP).
No statistically differences existed in operation time and length of stay between OP and NWP, and between MOP and NWP groups in our study. Ishii et al. conducted a meta-analysis and demonstrated that the mean operation time for the OP and MOP was 68.5 and 68.9 min, respectively (39). In another study by Alkan et al. revealed that the mean hospital stay for the OP and MOP was 1 ± 0.375 and 1 ± 0.33 day, respectively. Similarly, no statistically significant difference existed between OP and NWP, and between MOP and NWP groups regarding operation time and length of stay in our analysis, indicating that URS performed in MOP and OP appear to have the same safety as well as in the NWP group.
In terms of post-operative morbidity, we assessed the complication rate between the different groups and no statistically significant difference was observed. In our analysis, the overall complication rate of MOP and OP was 8.3 and 5.1%, respectively. This is comparable to the complication rate of NWP (4.9%). Ishii et al. reported that the complication rate in the OP was 8.4%, which is consistent with our results. But they only observed 16 complications in MOP (17.6%) (39). They concluded that the complication rate tended to be higher in MOP. The reason for the relatively higher complication rate in their study might be that only 91 MOP was included in the analysis so the results were inaccurate and biased. Additionally, 5 included studies (15–17, 19, 22) followed their patients up to 1 month post-operatively, and 5 included studies (18, 20, 21, 24, 27) saw their patients after 3 months in our analysis. Other authors did not specify the follow-up interval. The different time period of follow-up of included study might also contribute to distinguishing complication rate. However, the majority of complications were Clavien I or II, and no death occurred in our analysis, which corresponds to the previous study (39). Therefore, we can conclude that URS performed on OP and MOP is equally safe to NWP.
Life style modification is the most important method for the prevention of recurrence of urolithiasis in OP (40). A diet containing a variety of fruits, vegetables, whole grains, and low-fat food is beneficial to OP (40). Besides, the combination of healthy diet and exercise will benefit patients more effective than diet or exercise alone (40).
A previous systematic review that included 7 studies involving 131 individuals found that URS could be conducted effectively and safely on OP, and SFR increased when stones size was <20 mm (14). However, this study was the small sample sized and did not sub-categorize the findings into obese and morbidly obese groups. Another systematic review demonstrated that URS was a secure and efficacious treatment choice for OP (39). Nonetheless, the authors failed to assess the effectiveness and safety of obesity on URS with a matched group of normal-weight individuals. They compared the outcomes of URS in the OP and MOP, concluding that the complications tended to be higher in MOP (39). However, the overall complication rate in MOP (8.3%) was close to OP (5.1%), and both were comparable to NWP (4.9%) in our analysis. In addition, the number of patients in our analysis was around 3 times (2465 OP and 291 MOP) more compared with the previous study (39).
Additionally, several limitations need to be mentioned in the present analysis. First, all the eligible studies were retrospective, which are associated with methodology bias. Second, the definition of SFR was not standardized, several studies considered residual stones ranging from 0 to 4 mm as stone-free status (15–17, 19, 21), while two studies only defined SFR as no fragments of any size (18, 20). In addition, there were various radiological methods for determining SFR in the included studies, such as ultrasound, CT scan, and IVP, and without a good clarification that which one is the best technique. Next, considering the patient positioning issue, the total operative room time should also be evaluated in addition to procedure time. But none of our included studies presented this data. Future studies providing more complete information are needed. However, our analysis incorporated a group of NWP as controlled and is the largest sample sized studies that determined the URS outcome variables in OP and MOP.
Conclusion
The URS procedure demonstrated similar results in MOP, OP, and NWP. Therefore, URS performed in MOP and OP appears to have the same efficacy and safety as well as in NWP group.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
WW and TJ collected and analyzed the data and prepared the manuscript. XG collected the data. LP analyzed the data and prepared a manuscript. All authors have read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.736641/full#supplementary-material
Abbreviations
URS, ureteroscopy; BMI, body mass index; SFR, stone-free rate; OR, odds ratio; MD, weighted mean difference; IVP, intravenous pyelography; LE, levels of evidence; NOS, Newcastle Ottawa Scale.
References
1. Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. (2019) 92:6–10. doi: 10.1016/j.metabol.2018.09.005
2. Singh GM, Danaei G, Farzadfar F, Stevens GA, Woodward M, Wormser D, et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS ONE. (2013) 8:e65174. doi: 10.1371/journal.pone.0065174
3. Czernichow S, Kengne AP, Stamatakis E, Hamer M, Batty GD. Body mass index, waist circumference and waist-hip ratio: which is the better discriminator of cardiovascular disease mortality risk?: Evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies. Obes Rev. (2011) 12:680–7. doi: 10.1111/j.1467-789X.2011.00879.x
4. Anandacoomarasamy A, Caterson I, Sambrook P, Fransen M, March L. The impact of obesity on the musculoskeletal system. Int J Obes. (2008) 32:211–22. doi: 10.1038/sj.ijo.0803715
5. Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body fatness and cancer–viewpoint of the IARC working group. N Engl J Med. (2016) 375:794–8. doi: 10.1056/NEJMsr1606602
6. Curhan GC, Willett WC, Rimm EB, Speizer FE, Stampfer MJ. Body size and risk of kidney stones. J Am Soc Nephrol. (1998) 9:1645–52. doi: 10.1681/ASN.V991645
7. Sorensen MD, Chi T, Shara NM, Wang H, Hsi RS, et al. Activity, energy intake, obesity, and the risk of incident kidney stones in postmenopausal women: a report from the Women's Health Initiative. J Am Soc Nephrol. (2014) 25:362–9. doi: 10.1681/ASN.2013050548
8. Taylor EN, Stampfer MJ, Curhan GC. Obesity, weight gain, and the risk of kidney stones. JAMA. (2005) 293:455–62. doi: 10.1001/jama.293.4.455
9. Ekeruo WO, Tan YH, Young MD, Dahm P, Maloney ME, Mathias BJ, et al. Metabolic risk factors and the impact of medical therapy on the management of nephrolithiasis in obese patients. J Urol. (2004) 172:159–63. doi: 10.1097/01.ju.0000128574.50588.97
10. Del Valle EE, Negri AL, Spivacow FR, Rosende G, Forrester M, Pinduli I. Metabolic diagnosis in stone formers in relation to body mass index. Urol Res. (2012) 40:47–52. doi: 10.1007/s00240-011-0392-8
11. Bobulescu A. Renal lipid metabolism and lipotoxicity. Curr Opin Nephrol Hypertens. (2010) 19:393–402. doi: 10.1097/MNH.0b013e32833aa4ac
12. Türk C, Neisius A, Petrík A, Seitz C, Thomas K, Skolarikos A. EAU guidelines on urolithiasis 2021. In: European Association of Urology Guidelines. 2021 Edition. Arnhem: The European Association of Urology Guidelines Office (2021).
13. Bazurro S, Ball L, Pelosi P. Perioperative management of obese patient. Curr Opin Crit Care. (2018) 24:560–7. doi: 10.1097/MCC.0000000000000555
14. Aboumarzouk OM, Somani B, Monga M. Safety and efficacy of ureteroscopic lithotripsy for stone disease in obese patients: a systematic review of the literature. BJU Int. (2012) 110(8 Pt B):E374–80. doi: 10.1111/j.1464-410X.2012.11086.x
15. Alkan E, Arpali E, Ozkanli AO, Basar MM, Acar O, Balbay MD. RIRS is equally efficient in patients with different BMI scores. Urolithiasis. (2015) 43:243–8. doi: 10.1007/s00240-015-0750-z
16. Best SL, Nakada SY. Flexible ureteroscopy is effective for proximal ureteral stones in both obese and nonobese patients: a two-year, single-surgeon experience. Urology. (2011) 77:36–9. doi: 10.1016/j.urology.2010.05.001
17. Caskurlu T, Atis G, Arikan O, Pelit ES, Kilic M, Gurbuz C. The impact of body mass index on the outcomes of retrograde intrarenal stone surgery. Urology. (2013) 81:517–21. doi: 10.1016/j.urology.2012.12.008
18. Chew BH, Zavaglia B, Paterson RF, Teichman JM, Lange D, Zappavigna C, et al. A multicenter comparison of the safety and effectiveness of ureteroscopic laser lithotripsy in obese and normal weight patients. J Endourol. (2013) 27:710–4. doi: 10.1089/end.2012.0605
19. Dash A, Schuster TG, Hollenbeck BK, Faerber GJ, Wolf JS. Jr. Ureteroscopic treatment of renal calculi in morbidly obese patients: a stone-matched comparison. Urology. (2002) 60:393–7. doi: 10.1016/S0090-4295(02)01776-4
20. Delorme G, Huu YN, Lillaz J, Bernardini S, Chabannes E, Guichard G, et al. Ureterorenoscopy with holmium-yttrium-aluminum-garnet fragmentation is a safe and efficient technique for stone treatment in patients with a body mass index superior to 30 kg/m2. J Endourol. (2012) 26:239–43. doi: 10.1089/end.2011.0391
21. Doizi S, Letendre J, Bonneau C S, Gil Diez de Medina, O. Traxer. Comparative study of the treatment of renal stones with flexible ureterorenoscopy in normal weight, obese, and morbidly obese patients. Urology. (2015) 85:38–44. doi: 10.1016/j.urology.2014.08.028
22. Doluoglu OG, Karakan T, Kabar M, Ozgur BC, Hascicek AM, Huri E, et al. Effectiveness of retrograde intrarenal stone surgery in obese patients. Irish J Med Sci. (2016) 185:847–51. doi: 10.1007/s11845-015-1379-1
23. Drăgutescu M, Multescu R, Geavlete B, Mihai B, Ceban E, Geavlete P. Impact of obesity on retrograde ureteroscopic approach. J Med Life. (2012) 5:222–5.
24. Krambeck A, Wijnstok N, Olbert P, Mitroi G, Bariol S, Shah HN, et al. The influence of body mass index on outcomes in ureteroscopy: results from the Clinical Research Office of Endourological Society URS Global Study. J Endourol. (2017) 31:20–6. doi: 10.1089/end.2016.0514
25. Natalin R, Xavier K, Okeke Z, Gupta M. Impact of obesity on ureteroscopic laser lithotripsy of urinary tract calculi. Int Braz J Urol. (2009) 35:36–41. doi: 10.1590/S1677-55382009000100006
26. Pompeo A, Molina WR, Juliano C, Sehrt D, Kim FJ. Outcomes of intracorporeal lithotripsy of upper tract stones is not affected by BMI and skin-to-stone distance (SSD) in obese and morbid patients. Int Braz J Urol. (2013) 39:702–9. doi: 10.1590/S1677-5538.IBJU.2013.05.13
27. Sari E, Tepeler A, Yuruk E, Resorlu B, Akman T, Binbay M, et al. Effect of the body mass index on outcomes of flexible ureterorenoscopy. Urolithiasis. (2013) 41:499–504. doi: 10.1007/s00240-013-0590-7
28. Moher D, Liberati A, Tetzlaff J, G D. Altman: preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
29. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. (2009) 250:187–96. doi: 10.1097/SLA.0b013e3181b13ca2
30. Alon E, Baumann H. Anesthesiologic management of cesarean section in a patient with transposition of the great vessels. Regional Anaesth. (1988) 11:28–31.
31. Baran O, Aykac A, Sari S, Ates A, Ozok U, Sunay M. Retrograde intrarenal surgery for stone disease under spinal anaesthesia, a minimally invasive technique. A retrospective analysis of 1,467 cases. Actas Urol Esp. (2019) 43:248–53. doi: 10.1016/j.acuroe.2019.04.004
32. Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. (2016) 355:i4919. doi: 10.1136/bmj.i4919
33. Levy DT, Mabry PL, Wang YC, Gortmaker S, Huang TTK, Marsh T, et al. Simulation models of obesity: a review of the literature and implications for research and policy. Obes Rev. (2011) 12:378–94. doi: 10.1111/j.1467-789X.2010.00804.x
34. Carbone A, Al Salhi Y, Tasca A, Palleschi G, Fuschi A, De Nunzio C, et al. Obesity and kidney stone disease: a systematic review. Minerva Urol Nefrol. (2018) 70:393–400. doi: 10.23736/S0393-2249.18.03113-2
35. Scales CD Jr, Smith AC, Hanley JM, Saigal CS. Prevalence of kidney stones in the United States. Eur Urol. (2012) 62:160–5. doi: 10.1016/j.eururo.2012.03.052
36. Mosli HA, Mosli HH, Kamal WK. Kidney stone composition in overweight and obese patients: a preliminary report. Res Rep Urol. (2013) 5:11–5. doi: 10.2147/RRU.S39581
37. Strohmaier WL, Wrobel BM, Schubert G. Overweight, insulin resistance and blood pressure (parameters of the metabolic syndrome) in uric acid urolithiasis. Urol Res. (2012) 40:171–5. doi: 10.1007/s00240-011-0403-9
38. Abbott JE, Sur RL. Ureterorenoscopy: current technology and future outlook. Minerva Urol Nefrol. (2016) 68:479–95.
39. Ishii H, Couzins M, Aboumarzouk O, Biyani CS, Somani BK. Outcomes of systematic review of ureteroscopy for stone disease in the obese and morbidly obese population. J Endourol. (2016) 30:135–45. doi: 10.1089/end.2015.0547
Keywords: ureteroscopy, urolithiasis, obesity, meta-analysis, systematic review
Citation: Wang W, Gao X, Peng L and Jin T (2022) Ureteroscopy Is Equally Efficient and Safe in Obese and Morbidly Obese Patients: A Systematic Review and Meta-Analysis. Front. Surg. 9:736641. doi: 10.3389/fsurg.2022.736641
Received: 04 August 2021; Accepted: 20 January 2022;
Published: 18 February 2022.
Edited by:
Idir Pierre Ouzaid, Hôpital Bichat-Claude-Bernard, FranceReviewed by:
Ewelina Malanowska, Pomorskiej Akademii Medycznej, PolandRandi M. Pose, Martini Klinik Prostate Cancer Center, Germany
Copyright © 2022 Wang, Gao, Peng and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Jin, amludGFvamludGFvOTdAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Wei Wang
Wei Wang XiaoShuai Gao
XiaoShuai Gao Liao Peng
Liao Peng Tao Jin
Tao Jin