- Department of Radiology, Sichuan Provincial People’s Hospital, Sichuan Academy of Medical Sciences, Chengdu, China
Objective: Fluorodeoxyglucose Positron emission tomography/computerized tomography (FDG PET/CT) has become popular for diagnosing periprosthetic joint infections (PJI). However, the diagnostic accuracy for this technique has varied from report to report. This meta-analysis was performed to assess the accuracy of FDG PET/CT for PJI diagnosis.
Material and Methods: We conducted a systematic search of online academic databases for all studies reporting the diagnostic accuracy of FDG PET/CT for PJI. Meta-analysis was performed using STATA software.
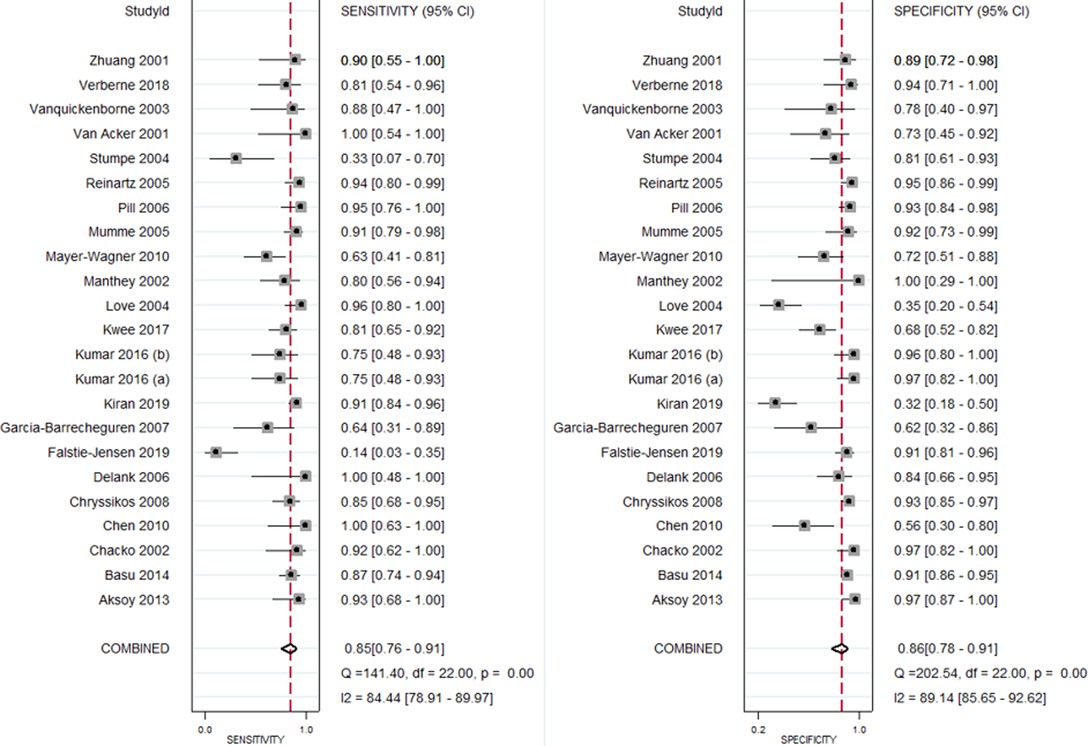
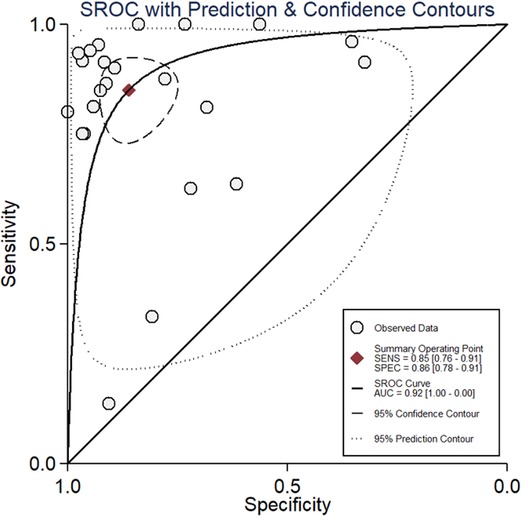
Results: 23 studies, containing data on 1,437 patients, met inclusion criteria. Pooled sensitivity and specificity of FDG PET/CT for diagnosing PJI were 85% (95% CI, 76%, 91%) and 86% (95% CI, 78%, 91%), respectively with an AUC of 0.92. LRP was 6.1 (95% CI, 3.8, 9.7) and LRN was 0.17 (0.11, 0.28), indicating that FDG PET/CT cannot be used for confirmation or exclusion of PJI. There was significant inter-study heterogeneity, but no significant publication bias was noted.
Conclusions: Our study found that FDG PET/CT has an important role as a diagnostic tool for PJI with high sensitivity and specificity. Further studies exploring its accuracy in different PJI locations remain necessary.
Introduction
Alongside increasing life expectancies, the worldwide prevalence of adults aged 50 years or more living with a prosthesis has been estimated at 2.3%, with the proportion rising to 6% for individuals 80 years of age or older (1). In particular, joint arthroplasty incidence has increased substantially over recent decades (2). This has created an issue where a considerable portion of these prostheses must be revised within five or ten years (3). Common reasons for prosthetic revision include aseptic (55%) and septic loosening (7%), dislocation (12%), and periprosthetic fracture (6%) (4). While dislocations and periprosthetic fractures can be readily diagnosed, it is often challenging to differentiate aseptic from septic loosening (5). In the United States, two-stage exchange is the procedure of choice, while in European countries, one-stage procedure is preferred whenever feasible if the pathogen is known and the skin & bone are in good condition (6). Hence, this differentiation is very important clinically since the treatment of aseptic loosening follows either of these procedures and use of beads carries a risk of colonization (6).
American Academy of Orthopaedic Surgeons (AAOS) guidelines for periprosthetic joint infection (PJI) diagnosis recommends erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) testing in all the patients (7). Radiographs are also routinely obtained in the suspected PJI work-up. Whether joint aspiration is required is then decided based on ESR/CRP results and PJI probability (7). AAOS guidelines also state that positron emission tomography/computed tomography (PET/CT) could be used in certain patients, and over the past decade, several studies have assessed the utility of PET/CT for diagnosing PJI (8–10). The results of previous studies have varied from report to report. FDG PET/CT use may reduce diagnostic procedure durations, thereby improving the quality of care. Moreover, the early diagnosis of PJI can lead to more effective therapeutic management. No up-to-date meta-analysis that assesses the diagnostic accuracy of FDG PET/CT currently exists, with the most recent one having been published in 2010 (11). The present study therefore aimed to perform a pooled analysis on all available literature concerning the diagnostic accuracy of FDG PET/CT for PJI.
Material and Methods
Eligibility Criteria
Included Study Types
This study included all studies examining the diagnostic accuracy of FDG PET/CT for PJI regardless of study design, participant characteristics, and assessed PJI type. We only included studies that reported the sensitivity and specificity of employed diagnostic techniques or provided sufficient data to calculate those values. Studies without accessible full-text manuscripts were excluded. Case reports and studies with sample sizes under 10 were also excluded.
Index Test
This study included studies examining the diagnostic accuracy of FDG PET/CT for PJI.
Reference Standards
We included studies only if the diagnostic accuracy of FDG PET/CT was compared with that of an intraoperative positive culture, regardless of whether it was combined with histopathological evidence concerning periprosthetic tissue acute inflammation caused by surgical debridement or prosthesis removal and/or the presence of the sinus tract that communicates with the prosthesis.
Outcome Measures
The number of patients who were true positives, false positives, true negatives, and false negatives for PJI.
Search Strategy
We conducted a comprehensive, systematic, and extensive search of electronic databases including PubMed Central, EMBASE, MEDLINE, SCOPUS, and the Cochrane Library. We used both medical subject headings (MeSH) and free-text words to query all searched databases. Keywords and their synonyms were employed using appropriate truncations, wildcards, and proximity searching. The following MeSH terms and free text terms were used in various combinations: “Validation Studies”, “Periprosthetic Joint Infection”, “Positron Emission Tomography/Computed Tomography”, “PET/CT”, “18FDG PET/CT”, “Fluoride PET/CT”, “Histopathology” “Sensitivity”, “Specificity”, “Diagnosis”, and “Diagnostic Accuracy Studies”. Searches were also conducted in each database for key concepts using corresponding subject headings. The final search was carried out by combining individual search results using the appropriate Boolean operators (“OR” and “AND”). Only publications published prior to February 2021 and published in the English language were considered.
Study Screening
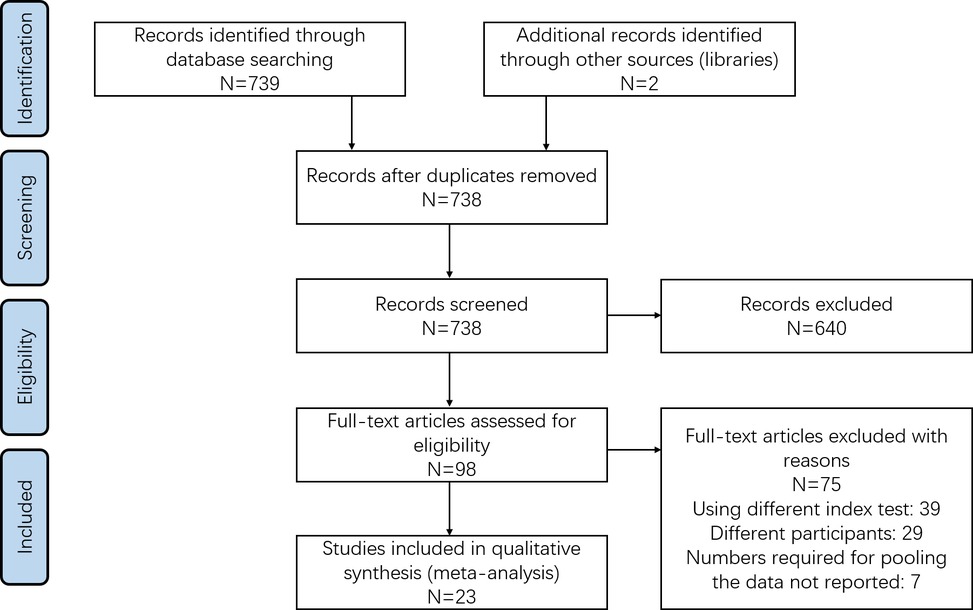
Preliminary screening, involving title and abstract assessment, was performed by two reviewers. Here, all hits returned by search queries were imported to a specified Endnote library. After duplicates were removed, the library was manually scanned to identify short-list candidates. The full-text articles were retrieved for these shortlisted studies and reviewed by the same two reviewers. Shortlisted studies not satisfying eligibility criteria were excluded, with the reason for exclusion noted. Any disagreements between the two reviewers were resolved through arbitration with a third investigator. This process is outlined in Figure 1 and took place in accordance with PRISMA guidelines (12).
Data Extraction and Management
Study data was extracted using a pre-defined data extraction form. Extracted data included design, setting, index test, reference standards (gold standard), PJI site, sample size, average age, inclusion and exclusion criteria, test positives (true & false), and test negatives (true & false). Data was transferred into STATA software. Data quality was checked and verified by the third investigator who arbitrated disputes during the study screening process
Bias Risk Assessment
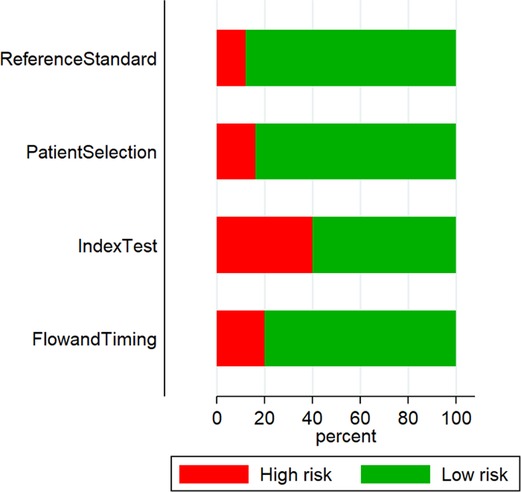
Two independent reviewers assessed bias risk in included studies using the “Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool” (13). The following domains were examined: patient selection, index tests, reference standards, flow and timing of assessments. Grades were assigned as high, low, and unclear for each domain.
Statistical analysis
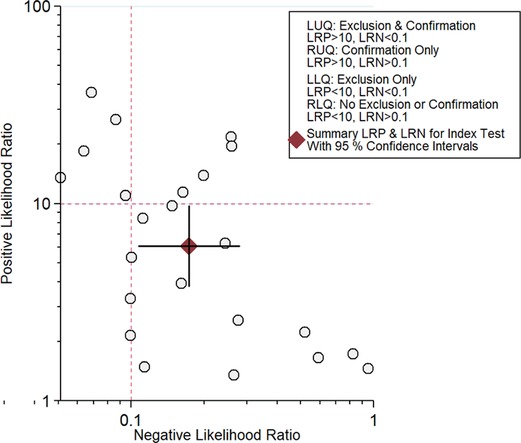
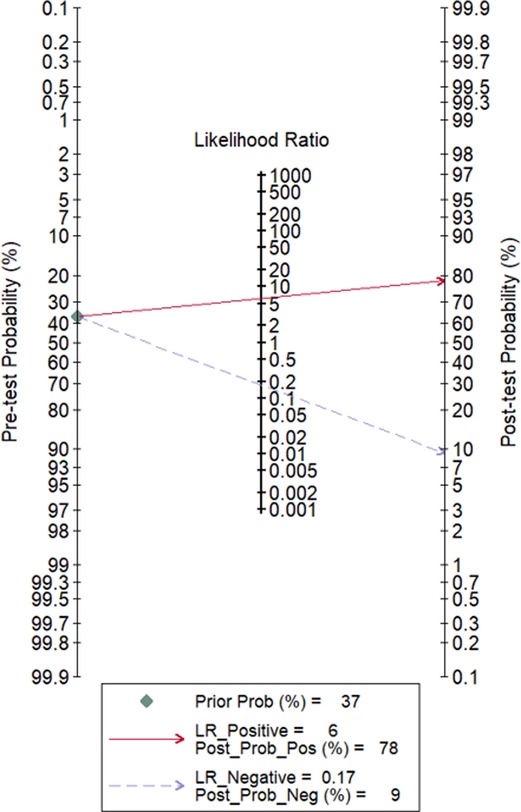
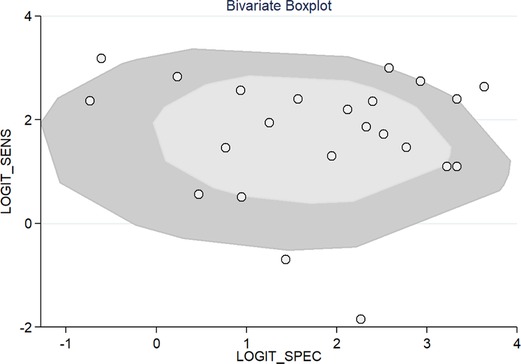
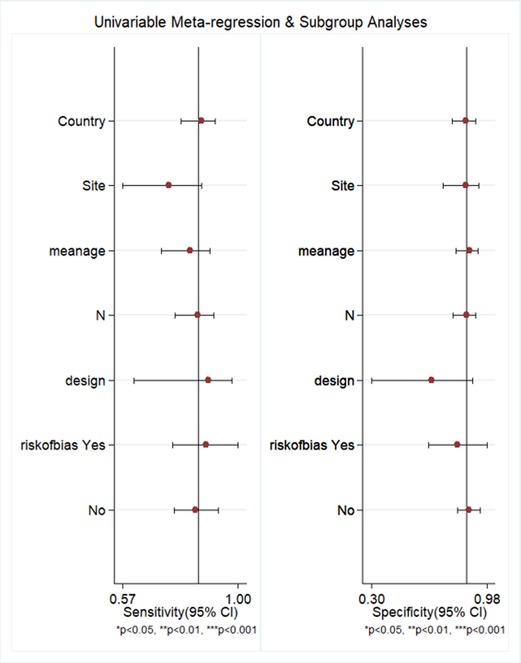
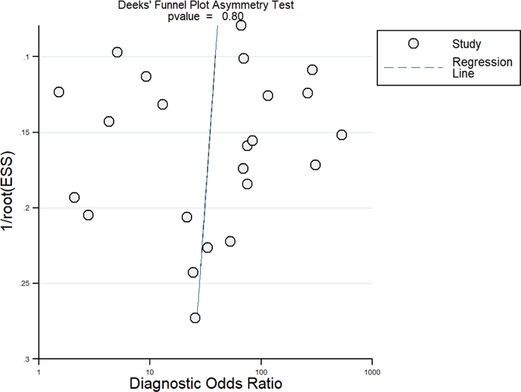
The meta-analysis was performed using STATA software version 14.2 (StataCorp, College Station, TX, USA) to obtain pooled sensitivity, specificity, positive likelihood ratio (LRP), negative likelihood ratio (LRN), and summary diagnostic odds ratio (DOR) values for PET/CT. Summary Receiver Operator Characteristic curves (sROC) were constructed and summarized as area under the curve (AUC). Study-specific and pooled estimates were graphically represented through Forest plots. A Fagan plot was constructed to demonstrate how much a PET/CT result changes the probability that a patient has PJI. LR scattergram was used to determine the clinical value of FDG PET/CT. The presence of between-study variance due to heterogeneity was assessed using three methods: graphical representation via a bivariate box plot, the chi square test for heterogeneity, and I2 statistics to quantify inconsistency (<25%: mild, 25%–75%: moderate, >75%: substantial). Subgroup analysis and meta-regression was performed as well. Publication bias was assessed and graphically represented using a funnel plot, with the asymmetry of the plot tested using Deek’s test.
Results
Study Selection
The literature search revealed 739 unique articles, and 98 were shortlisted for full-text retrieval. We also retrieved full-texts for two additional articles found by screening references cited by other retrieved studies. A total of 23 studies, containing information on 1,437 patients, met inclusion criteria and were used for meta-analysis (Figure 1) (8–10, 14–33).
Characteristics of Included Studies
Twenty out of 23 studies were prospective. The USA was the most represented setting, with six studies conducted in that country. They were followed by Germany (5) and India (2). The mean age of study participants within individual studies ranged from 53.0 to 76.4 years. Sample sizes in individual studies ranged from 17 to 221 patients. Fourteen studies assessed patients with suspected PJI in the hip, while seven looked at PJI in both the hip and knee. Most of the studies used a combination of intraoperative findings with histopathological, microbiological, and clinical examinations as the reference standard (Table 1).
Risk of Bias Assessment
QUADAS tool results found that 3 out of 23 studies had a high risk of patient selection bias, 10 had a high risk of conduct and interpretation of index test bias, 5 had a high risk of patient flow and interval between index tests and reference standards bias, and 2 had a high risk of reference standard bias (Figure 2 and Table 2).
Diagnostic Accuracy of FDG PET/CT for PJI
All 23 included studies reported on the utility of FDG PET/CT for diagnosing PJI (8–10, 14–33). Pooled sensitivity and specificity of FDG PET/CT for diagnosing PJI were 85% (95% CI, 76%, 91%) and 86% (95% CI, 78%, 91%), respectively, with an AUC value of 0.92 (Figures 3, 4). The DOR was 35 (95% CI, 17, 74), LRP was 6.1 (95% CI, 3.8, 9.7), and LRN was 0.17 (95% CI, 0.11, 0.28). LR scattergram (Figure 5) showed LRP and LRN in the right lower quadrant, indicating that the PET/CT cannot be used for confirmation or exclusion. Figure 6 shows a high clinical utility of PET/CT for diagnosing PJI (Positive: 78%; Negative: 9%), differing significantly from the pre-test probability (37%). We also found significant inter-study variability (heterogeneity) with a chi-square p value <0.001 and an I2 > 75%. The bivariate box plot further confirmed this heterogeneity (Figure 7).
We performed meta-regression to find heterogeneity sources, using factors such as study design, PJI site, country, sample size, mean age, and quality related factors (Figure 8). However, we could not find any factors to be significantly associated using the sensitivity and specificity model, while only mean age (p < 0.001) was found to be a source of heterogeneity using the joint model. Deek’s test showed a non-significant p-value (p = 0.80), thus indicating the absence of publication bias. This was confirmed by the symmetrically-shaped funnel plot (Figure 9).
Subgroup analysis delineating based on study design type revealed that prospective studies alone had similar pooled sensitivity (85%) and specificity (88%) values relative to the entire dataset. Studies possessing low bias risk had higher specificity (87%) compared to studies with high bias risk (81%). However, we did not find any significant difference in specificity between low-bias risk and high-bias risk studies (85% in both subgroups). Subgroup analysis delineating based on PJI site found that the hip location possessed similar sensitivity (87%) and specificity (85%) relative to the overall estimate. Insufficient sample size prevented subgroup analysis on other locations.
Discussion
The diagnostic approach for patients with suspected PJI has varied considerably across different healthcare centers globally and depends on the experience of the health professional and the availability of the latest technological equipment (34). Presently, radiography is widely used as an initial diagnostic protocol, with PET/CT a popular modality for its reported diagnostic accuracy (25–33). However, this accuracy has not been confirmed through a systematic evaluation. Hence, our goal here was to determine the diagnostic accuracy of FDG PET/CT for PJI.
Our systematic literature search found 23 studies reporting the utility of FDG PET/CT for diagnosing PJI. We found a high pooled sensitivity (85%) and specificity (86%) for FDG PET/CT in PJI diagnosis. Moreover, the clinical utility of FDG PET/CT was demonstrated by how Fagan’s nomogram showed a significant rise in post-PET/CT probability compared to pre-PET/CT probability. Our findings are similar to those previously reported (11, 35–37). Over the past few years, PET/CT has been used as a standard scan system for PET in several medical centers around the world. A metallic prosthesis following the surgery can produce a strong artifact in the CT images, resulting in underestimation or overestimation of the concentration of activity around these metallic prostheses. Hence, correction of PET images by CT-based attenuation provides accurate images and misinterpretation of the image tracer accumulation can be reduced using the newer metal artifact reduction systems (8, 38).
We also noted that FDG PET/CT diagnostic efficacy did not differ significantly depending on study bias and PJI site. Certain studies have reported that labeled leukocyte/marrow imaging is a superior diagnostic tool to FDG PET/CT (24). The possible reason for this finding is that the indication for PET-CT in PJI is limited to special situations in which a painful implant may stem from aseptic or septic loosening. If joint aspiration is dry or the surgeon wants to gather information on the whole implant, imaging modalities gain importance. In those revision situations which usually involve older patients, time of imaging and radiation exposure are not of utmost interest. Thus, WBC scintigraphy is the more accurate option, if available. In addition, FDG PET/CT is not a part of standard definition of protocol for PJI diagnosis. This is mainly because it is considered that there is no place of nuclear imaging for acute infections. However, FDG PET/CT has certain advantages in terms of feasibility, availability, and logistics (requiring only one radiotracer injection). Thus, PET/CT can be added as part of the standard diagnostic protocol for PJI if WBC scintigraphy is unavailable and diagnosis needs imaging.
Our review has certain strengths. This meta-analysis involved a large number of studies with high sample sizes (23 studies with >1,400 participants). Most included studies had high quality across most of the domains under the QUADAS-2 tool, and we did not find any significant publication bias, which further adds to the credibility of results in our analysis. Deek’s test results and funnel plot showed a possibility of the absence of a significant publication bias. However, there are several limitations to this meta-analysis. First, we found significant inter-study heterogeneity, limiting our ability to interpret or infer the pooled results. Although we investigated potential reasons for such high heterogeneity using meta-regression, we could not identify any factors other than mean age. Second, FDG PET/CT diagnostic accuracy in practice depends on various factors, such as assessment timing, PJI site, number and experience of interpreters, FDG dose, time interval between FDG administration and scanning and additional patient co-morbidities. However, we could not assess the influence of any of these factors due to a lack of available data.
Despite these shortcomings, our findings provide valuable information and important implications for the clinical management of PJI and suggest that FDG PET/CT can be used as an effective screening and diagnostic tool. Moreover, early diagnoses of PJI can further lead to the more effective therapeutic management of the diagnosed patients. Further updated reviews should compare the diagnostic performance of PET/CT with other similar imaging techniques. In addition, large-scale longitudinal studies are required to check the diagnostic accuracy of PET/CT based on the different sites of PJI because most available studies have hip as the site of PJI and limited study available on knee and shoulder PJI.
Conclusion
Our study found that can have an important role as a diagnostic tool in certain situations of PJI, given its high sensitivity and specificity. However, the finding should be interpreted with caution given the higher level of heterogeneity. In the future, studies should seek to compare the diagnostic performance of FDG PET/CT with other similar imaging techniques. Similarly, large-scale longitudinal studies are required to examine the diagnostic accuracy of FDG PET/CT for different PJI sites.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
MH designed the project; GC and LL were involved in data collection and data analysis; LS prepared the manuscript; MH and LL edited the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. (2015) 97:1386–97. doi: 10.2106/JBJS.N.01141
2. Lam V, Teutsch S, Fielding J. Hip and knee replacements: a neglected potential savings opportunity. JAMA. (2018) 319:977–8. doi: 10.1001/jama.2018.2310
3. Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. (2011) 93:293–7. doi: 10.1302/0301-620X.93B3.25467
4. Kwee RM, Kwee TC. 18F-FDG PET for diagnosing infections in prosthetic joints. PET Clin. (2020) 15:197–205. doi: 10.1016/j.cpet.2019.11.005
5. Kapadia BH, Berg RA, Daley JA, Fritz J, Bhave A, Mont MA. Periprosthetic joint infection. Lancet. (2016) 387:386–94. doi: 10.1016/S0140-6736(14)61798-0
6. Izakovicova P, Borens O, Trampuz A. Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev. (2019) 4:482–94. doi: 10.1302/2058-5241.4.180092
7. Tubb CC, Polkowksi GG, Krause B. Diagnosis and prevention of periprosthetic joint infections. J Am Acad Orthop Surg. (2020) 28:e340–8. doi: 10.5435/JAAOS-D-19-00405
8. Basu S, Kwee TC, Saboury B, Garino JP, Nelson CL, Zhuang H, et al. FDG PET for diagnosing infection in hip and knee prostheses: prospective study in 221 prostheses and subgroup comparison with combined (111)In-labeled leukocyte/(99 m)Tc-sulfur colloid bone marrow imaging in 88 prostheses. Clin Nucl Med. (2014) 39:609–15. doi: 10.1097/RLU.0000000000000464
9. Kwee RM, Broos WA, Brans B, Walenkamp GH, Geurts J, Weijers RE. Added value of 18F-FDG PET/CT in diagnosing infected hip prosthesis. Acta Radiol. (2018) 59:569–76. doi: 10.1177/0284185117726812
10. Verberne SJ, Temmerman OPP, Vuong BH, Raijmakers PG. Fluorodeoxyglucose positron emission tomography imaging for diagnosing periprosthetic hip infection: the importance of diagnostic criteria. Int Orthop. (2018) 42:2025–34. doi: 10.1007/s00264-018-3931-x
11. Kwee TC, Kwee RM, Alavi A. FDG-PET for diagnosing prosthetic joint infection: systematic review and metaanalysis. Eur J Nucl Med Mol Imaging. (2008) 35:2122–32. doi: 10.1007/s00259-008-0887-x
12. Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. (2011) 22:128; author reply 128. doi: 10.1097/EDE.0b013e3181fe7825
13. Whiting PF, Rutjes AWS, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. (2011) 155:529–36. doi: 10.7326/0003-4819-155-8-201110180-00009
14. Aksoy SY, Asa S, Ozhan M, Ocak M, Sager MS, Erkan ME, et al. FDG and FDG-labelled leucocyte PET/CT in the imaging of prosthetic joint infection. Eur J Nucl Med Mol Imaging. (2014) 41:556–64. doi: 10.1007/s00259-013-2597-2
15. Chacko TK, Zhuang H, Stevenson K, Moussavian B, Alavi A. The importance of the location of fluorodeoxyglucose uptake in periprosthetic infection in painful hip prostheses. Nucl Med Commun. (2002) 23:851–5. doi: 10.1097/00006231-200209000-00008
16. Chen SH, Ho KC, Hsieh PH, Lee MSS, Yen TC. Potential clinical role of 18F FDG-PET/CT in detecting hip prosthesis infection: a study in patients undergoing two-stage revision arthroplasty with an interim spacer. Q J Nucl Med Mol Imaging. (2010) 54:429–35.20823810
17. Chryssikos T, Parvizi J, Ghanem E, Newberg A, Zhuang H, Alavi A. FDG-PET imaging can diagnose periprosthetic infection of the hip. Clin Orthop Relat Res. (2008) 466:1338–42. doi: 10.1007/s11999-008-0237-0
18. Delank K-S, Schmidt M, Michael JW-P, Dietlein M, Schicha H, Eysel P. The implications of 18F-FDG PET for the diagnosis of endoprosthetic loosening and infection in hip and knee arthroplasty: results from a prospective, blinded study. BMC Musculoskelet Disord. (2006) 7:20. doi: 10.1186/1471-2474-7-20
19. Falstie-Jensen T, Lange J, Daugaard H, Vendelbo MH, Sørensen AK, Zerahn B, et al. 18F FDG-PET/CT has poor diagnostic accuracy in diagnosing shoulder PJI. Eur J Nucl Med Mol Imaging. (2019) 46:2013–22. doi: 10.1007/s00259-019-04381-w
20. García-Barrecheguren E, Rodríguez Fraile M, Toledo Santana G, Valentí Nín JR, Richter Echevarría JA. FDG-PET: a new diagnostic approach in hip prosthetic replacement. Rev Esp Med Nucl. (2007) 26:208–20. doi: 10.1157/13107972
21. Kiran M, Donnelly TD, Armstrong C, Kapoor B, Kumar G, Peter V. Diagnostic utility of fluorodeoxyglucose positron emission tomography in prosthetic joint infection based on MSIS criteria. Bone Joint J. (2019) 101-B:910–4. doi: 10.1302/0301-620X.101B8.BJJ-2018-0929.R2
22. Kumar R, Kumar R, Kumar V, Malhotra R. Comparative analysis of dual-phase 18F-fluoride PET/CT and three phase bone scintigraphy in the evaluation of septic (or painful) hip prostheses: a prospective study. J Orthop Sci. (2016) 21:205–10. doi: 10.1016/j.jos.2015.12.018
23. Kumar R, Kumar R, Kumar V, Malhotra R. Potential clinical implication of (18) F-FDG PET/CT in diagnosis of periprosthetic infection and its comparison with (18) F-Fluoride PET/CT. J Med Imaging Radiat Oncol. (2016) 60:315–22. doi: 10.1111/1754-9485.12444
24. Love C, Marwin SE, Tomas MB, Krauss ES, Tronco GG, Bhargava KK, et al. Diagnosing infection in the failed joint replacement: a comparison of coincidence detection 18F-FDG and 111In-labeled leukocyte/99mTc-sulfur colloid marrow imaging. J Nucl Med. (2004) 45:1864–71. PMID: 15534056
25. Manthey N, Reinhard P, Moog F, Knesewitsch P, Hahn K, Tatsch K. The use of [18 F]fluorodeoxyglucose positron emission tomography to differentiate between synovitis, loosening and infection of hip and knee prostheses. Nucl Med Commun. (2002) 23:645–53. doi: 10.1097/00006231-200207000-00009
26. Mayer-Wagner S, Mayer W, Maegerlein S, Linke R, Jansson V, Müller PE. Use of 18F-FDG-PET in the diagnosis of endoprosthetic loosening of knee and hip implants. Arch Orthop Trauma Surg. (2010) 130:1231–8. doi: 10.1007/s00402-009-1000-z
27. Mumme T, Reinartz P, Alfer J, Müller-Rath R, Buell U, Wirtz DC. Diagnostic values of positron emission tomography versus triple-phase bone scan in hip arthroplasty loosening. Arch Orthop Trauma Surg. (2005) 125:322–9. doi: 10.1007/s00402-005-0810-x
28. Pill SG, Parvizi J, Tang PH, Garino JP, Nelson C, Zhuang H, et al. Comparison of fluorodeoxyglucose positron emission tomography and (111)indium-white blood cell imaging in the diagnosis of periprosthetic infection of the hip. J Arthroplasty. (2006) 21:91–7. doi: 10.1016/j.arth.2006.05.021
29. Reinartz P, Mumme T, Hermanns B, Cremerius U, Wirtz DC, Schaefer WM, et al. Radionuclide imaging of the painful hip arthroplasty: positron-emission tomography versus triple-phase bone scanning. J Bone Joint Surg Br. (2005) 87:465–70. doi: 10.1302/0301-620X.87B4.14954
30. Stumpe KDM, Nötzli HP, Zanetti M, Kamel EM, Hany TF, Görres GW, et al. FDG PET for differentiation of infection and aseptic loosening in total hip replacements: comparison with conventional radiography and three-phase bone scintigraphy. Radiology. (2004) 231:333–41. doi: 10.1148/radiol.2312021596
31. Van Acker F, Nuyts J, Maes A, Vanquickenborne B, Stuyck J, Bellemans J, et al. FDG-PET, 99mtc-HMPAO white blood cell SPET and bone scintigraphy in the evaluation of painful total knee arthroplasties. Eur J Nucl Med. (2001) 28:1496–504. doi: 10.1007/s002590100603
32. Vanquickenborne B, Maes A, Nuyts J, Van Acker F, Stuyck J, Mulier M, et al. The value of (18)FDG-PET for the detection of infected hip prosthesis. Eur J Nucl Med Mol Imaging. (2003) 30:705–15. doi: 10.1007/s00259-002-1109-6
33. Zhuang H, Duarte PS, Pourdehnad M, Maes A, Van Acker F, Shnier D, et al. The promising role of 18F-FDG PET in detecting infected lower limb prosthesis implants. J Nucl Med. (2001) 42:44–8. PMID: 11197979
34. Signore A, Sconfienza LM, Borens O, Glaudemans AWJM, Cassar-Pullicino V, Trampuz A, et al. Consensus document for the diagnosis of prosthetic joint infections: a joint paper by the EANM, EBJIS, and ESR (with ESCMID endorsement). Eur J Nucl Med Mol Imaging. (2019) 46:971–88. doi: 10.1007/s00259-019-4263-9
35. Verberne SJ, Raijmakers PG, Temmerman OPP. The accuracy of imaging techniques in the assessment of periprosthetic hip infection: a systematic review and meta-analysis. J Bone Joint Surg Am. (2016) 98:1638–45. doi: 10.2106/JBJS.15.00898
36. Verberne SJ, Sonnega RJA, Temmerman OPP, Raijmakers PG. What is the accuracy of nuclear imaging in the assessment of periprosthetic knee infection? A meta-analysis. Clin Orthop Relat Res. (2017) 475:1395–410. doi: 10.1007/s11999-016-5218-0
37. Hao R, Yuan L, Kan Y, Yang J. 18F-FDG PET for diagnosing painful arthroplasty/prosthetic joint infection. Clin Transl Imaging. (2017) 5:315–22. doi: 10.1007/s40336-017-0237-8
Keywords: meta-analysis, periprosthetic joint infection, positron emission tomography, validation studies, systematic review
Citation: Hu M, Chen G, Luo L and Shang L (2022) A Systematic Review and Meta-Analysis on the Accuracy of Fluorodeoxyglucose Positron Emission Tomography/ Computerized Tomography for Diagnosing Periprosthetic Joint Infections. Front. Surg. 9:698781. doi: 10.3389/fsurg.2022.698781
Received: 22 April 2021; Accepted: 17 May 2022;
Published: 1 June 2022.
Edited by:
Andor W.J.M. Glaudemans, University Medical Center Groningen, NetherlandsReviewed by:
Ricvan Dana Nindrea, Andalas University, IndonesiaStergios Lazarinis, Uppsala University, Sweden
Copyright © 2022 Hu, Chen, Luo and Shang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lan Shang c2hhbmdsYW44MjgyQDE2My5jb20=
†These authors have contributed equally to this work
Specialty section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
 Mei Hu†
Mei Hu† Lan Shang
Lan Shang