- Department of Orthopedic Surgery, Wake Forest University Baptist Medical Center, Winston-Salem, NC, United States
Femoroacetabular impingement syndrome (FAIS) is an increasingly prevalent pathology in young and active patients, that has contributing factors from both abnormal hip morphology as well as abnormal hip motion. Disease progression can be detrimental to patient quality of life in the short term, from limitations on sport and activity, as well as the long term through early onset of hip arthritis. However, several concurrent or contributing pathologies may exist that exacerbate hip pain and are not addressed by arthroscopic intervention of cam and pincer morphologies. Lumbopelvic stiffness, for instance, places increased stress on the hip to achieve necessary flexion. Pathology at the pubic symphysis and sacroiliac joint may exist concurrently to FAIS through aberrant muscle forces. Additionally, both femoral and acetabular retro- or anteversion may contribute to impingement not associated with traditional cam/pincer lesions. Finally, microinstability of the hip from either osseous or capsuloligamentous pathology is increasingly being recognized as a source of hip pain. The present review investigates the pathophysiology and evaluation of alternate causes of hip pain in FAIS that must be evaluated to optimize patient outcomes.
Introduction
Hip pain is prevalent in the athletic population, comprising approximately 5%–6% of adult sports injuries and 10%–24% of pediatric sports injuries (1, 2), though the exact source of pain has many possible sources. Femoroacetabular impingement syndrome (FAIS), generally defined as the abnormal contact between femur and acetabulum, has recently garnered increased attention as being responsible for the majority of hip pathologies in the pre-arthritic population (3). It has also become evident that hip morphology plays a significant role in the development of hip osteoarthritis, even if asymptomatic (4, 5). As such, utilization of hip arthroscopy is increasingly utilized for management of hip conditions, most often FAIS, and indications continue to rapidly evolve (6–8). Despite the focus on FAIS, alternative and concurrent pathologies must also be considered as concomitant causes of hip pain. The diagnosis of pre-arthritic hip pathology is complex, and failure to address a contributing cause may result in inferior outcomes and additional surgical procedures. The purpose of this review is to highlight other potential concomitant sources of pain in patients with FAIS.
Imbalance in spinopelvic alignment and sacroiliac pathology
The role of the pelvis in sagittal balance has been an area of increased recent investigation. Spinopelvic parameters including pelvic tilt, sacral slope, and pelvic incidence influence how patients can distribute weight across their axial and appendicular skeletons (Figure 1). Of which, pelvic incidence is the only parameter that is independent of position (9). Importantly, the greater the pelvic incidence, a greater lumbar lordosis (particularly in the proximal segment) is required to maintain an upright posture (10). Patients with low pelvic incidence are theorized to compensate with increased forward tilt of the pelvis. This motion likely results in over-coverage of the anterior acetabulum, and thereby, places this pelvis prone to impingement in the hip joint (11). Gebhart et al. postulated the delicate balance of pelvic incidence wherein higher incidence places more mechanical force on the lumbar spine, while lower incidence places greater force through the hip joint with associated cam and pincer morphologies (9). These authors analyzed cadaveric specimen to support this hypothesis and found both cam and pincer-morphologies were associated with decreased pelvic incidence (9). Weinberg et al. corroborated these findings clinically, suggesting that decreased pelvic incidence is correlated with mixed-type FAI (12). Fader et al. explored this relationship further and observed that symptomatic FAIS patients had greater sacral slope when sitting, and a compensatory increase in pelvic tilt (13). This illustrates the concept that lumbopelvic stiffness may result in compensatory greater hip flexion, and thereby, a greater propensity for cam lesions to engage the acetabulum (13). Recent evidence would thereby suggest that patients with lumbar pathology or surgery, particularly fusion, have inferior clinical outcomes following hip arthroscopy (14–16).
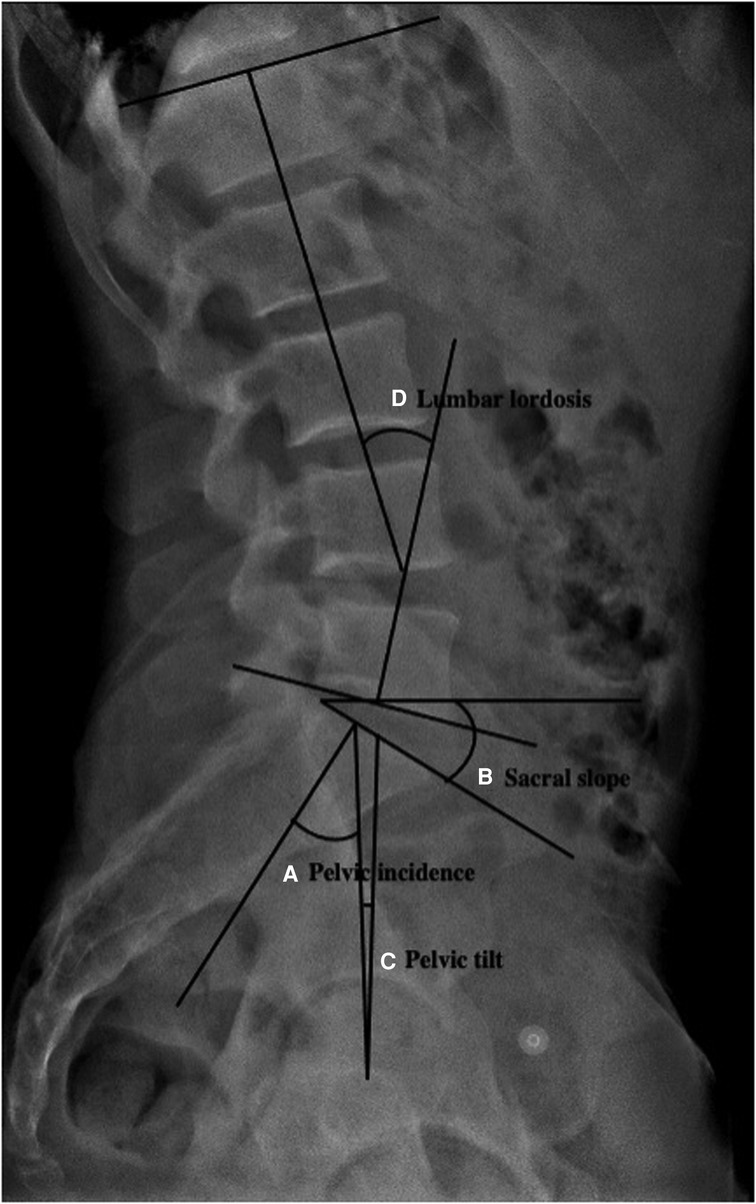
Figure 1. Radiographic measurements of (A) pelvic incidence, (B) sacral slope, (C) pelvic tilt, and (D) lumbar lordosis from lateral lumbar view radiograph.
In addition to identifying potential spinopelvic sagittal imbalances, a thorough examination of the sacroiliac joint should be performed as it has potential to elicit generalized hip pain. The sacroiliac joint plays a pivotal role in spinopelvic biomechanics by absorbing torsion and transferring load during movement. Previous studies have demonstrated that patients with altered hip range of motion have evidence of sacroiliac dysfunction (17). Altered range of motion may be caused by muscular imbalances, particularly hip rotators and extensors, but may also be caused by bony abnormalities leading to impingement. Indeed, a recent study by Krishnamoorthy and colleagues demonstrated that patients who underwent hip arthroscopy for treatment of FAIS and demonstrated SI joint abnormalities incidentally found on preoperative radiographs had lower outcomes when compared to patients who did not have SI joint abnormalities (18). Other studies have indicated that 17%–25% of patients have concomitant hip and SI joint pathology (18, 19). The growing evidence of concomitant lumbosacral pathology in patients with FAIS and other hip abnormalities may indicate a causal relationship between both that should be further evaluated in future studies.
Work-up for evaluation of spinopelvic derangements should include standing lumbar AP and lateral radiographs in order to evaluate spinopelvic derangements. Clinical findings such as positive FABER (flexion abduction, and external rotation) test, sacroiliac joint shear test, or Gaenslen's test may point to the SI joint as a cause for hip pain (20). While no single provocation test can accurately identify pain related to SI dysfunction, positive response to 3 or more maneuvers has a sensitivity of 77%–87% (21). Additional imaging studies including MRI may be ordered if the SI joint is suspected to be a source of hip pain, as it is the most sensitive imaging technique for detecting sacroiliitis (22).
Athletic pubalgia and osteitis pubis
Athletic pubalgia is a pathology often affecting those participating in sports with repetitive pivoting and cutting including soccer, and hockey (23). The rectus abdominis and hip adductor tendons (pectinius, gracilis, adductor longus/brevis and magnus) attach to the pubic ramus and provide pelvic stability. Athletic pubalgia is defined as injury to these musculotendinous structures near their bony insertion, resulting in pain and instability. It frequently coexists in patients with FAIS, reportedly in as high as 43.48% of patients with FAIS (24–27). Patients with decreased hip motion from FAIS are believed to compensate in motion through the pubic symphysis (28). The compensatory increased motion through the pubic symphysis causes increased stress and strain that can result in pathology to the symphysis (29, 30).
Chronic compensatory movement of the pubic symphysis can lead to osteitis pubis, defined by inflammatory changes in the joint (Figure 2). Previous studies have demonstrated that FAIS patients with pubic symphysis abnormalities on MRI had inferior post-operative functional outcomes after arthroscopic treatment of FAIS impingement (18). While the prevalence of osteitis pubis was low (2.3%), the presence of this pathology has the potency to limit functional gain from surgery if not addressed (18). These findings are supported by Birmingham and colleagues who found that repetitive loading of the symphysis secondary to cam morphology and impingement causes increased motion at the pubic symphysis (31).
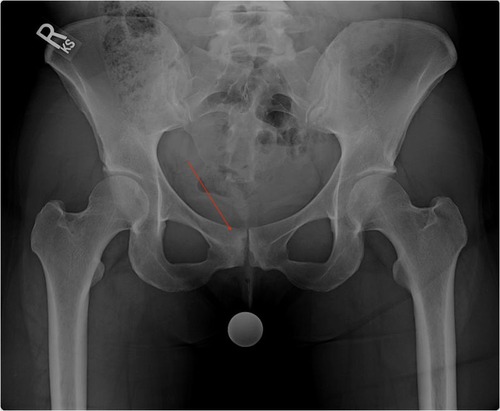
Figure 2. Anteroposterior radiographic image of a pelvis demonstrating bone edema (red arrow) and sclerotic changes in the pubic symphysis consistent with osteitis pubis.
Examination findings in patients with athletic pubalgia or osteitis pubis include pain with palpation of the pubis, inferior rectus abdominis, or adductor muscles, as well as exacerbated with resisted sit-ups at the inferolateral edge of the rectus abdominis (23). Tears and injury to other nearby musculotendinous structures including rectus femoris and iliopsoas tendinosis are associated with anterior hip pain as well (32). Test's including FABER test and tenderness over Scarpa's triangle may indicate either rectus femoris or iliopsoas tendonitis (32). A positive spring test may help differentiate osteitis pubis to that of athletic pubalgia. This test may be performed through palpation of the pubic rami, and results in pain in the symphysis (23). However, advanced imaging modalities, including MRI, may be necessary to confirm the presence of both and assist in directing further management. Previous studies have indicated that MRI has high specificity in identifying tendon tears associated with sports hernia, as well as osteitis pubis (33).
Impact of femoral and acetabular version
FAIS is typically recognized as impingement caused by acetabular over-coverage (pincer lesion), bony morphological changes at the femoral head-neck junction (cam lesion), or a combination of both. However, deviations in acetabular and femoral version may also cause impingement that may often go overlooked in traditional 2-dimensional radiographic workup. While the definition of acetabular retroversion remains debated, it is associated with crossover sign, ischial spine sign, and posterior wall sign (34, 35). Previous studies have demonstrated that patients with acetabular retroversion have higher rates of sub-spine impingement as well as larger femoral head coverage, when compared to patients with normal acetabular version (34). Historically, reverse periacetabular osteotomy has been used as the gold standard for treating acetabular retroversion, however, recent studies have demonstrated that patients with labral tears in the presence of acetabular retroversion can be treated arthroscopically without the need of acetabular osteotomies (36).
Femoral version may also play a role in FAIS not associated with traditional cam or pincer lesions. Recently, Lerch and colleagues determined that hips with decreased femoral version have decreased range of motion, specifically hip flexion and internal rotation in 90° of flexion (37). Additionally, the authors observed decreased femoral version was associated with both intra- and extraarticular impingement. Previous studies have evaluated whether femoral version has an impact on outcomes in patients who underwent arthroscopic treatment for FAI syndrome. Fabricant et al. analyzed outcomes among 243 patients and when stratified by femoral version, the authors observed that patients with femoral retroversion had statistically smaller magnitudes of postoperative improvements when compared to patients with normal femoral version (38). However, the literature is limited on whether solely addressing femoral or acetabular version in the absence of labral tears improves patient function or improves hip biomechanics.
Physical evaluation of abnormal femoral torsion includes assessing internal and external range of hip motion. Previous studies have found that patients with greater external rotation are associated with retroversion while greater internal rotation are associated with femoral neck anteversion (39). However, these measurements can be subjective and not diagnostic, particularly in adults (40). Provocative maneuvers during the clinical exam can assist in further evaluation of femoral torsion including the trochanteric prominence angle test (TPAT) also know as the Craig's test (41). Diagnosis and measurement of femoral neck torsion is performed typically using CT images by measuring the angle formed between a line down the middle of the femoral neck and a line parallel to the posterior aspect of the femoral condyles (42). The normal version of the femur is anteversion, with a normal range of approximately 10–20 degrees (17, 42).
Clinical evaluation of acetabular retroversion can be challenging in the absence of concomitant conditions (i.e. SCFE, dysplasia). Trochanteric pain with radiating pain laterally on the thigh is frequency observed in patients with acetabular retroversion. The most frequent physical finding in retroversion is limited internal rotation during maximal flexion and adduction of the hip. (43, 44). The Drehmann sign (passive external rotation with hip flexion) may also be seen in retroversion, however it may also be present in patients with SCFE or osteoarthritis (45–47). Plain radiographs are the first diagnostic tool used to evaluate acetabular version. The presence of the anterior and posterior acetabular borders crossing (crossover sign) (Figure 3) or deficient posterior acetabular wall observed on anteroposterior hip radiographs are indicative of possible retroversion. However, to measure acetabular version, CT imaging is typically necessary. Using the axial view, acetabular version is the angle formed by a line connecting the anterior and posterior acetabular margins and a perpendicular line that is transverse to the reference line through either the femoral head centers, posterior acetabular walls, or respective posterior aspect of the ischial bones (48). Physiologic acetabular anteversion is approximately 12–20 degrees in adults, however, this can also be variable (40, 49–51).
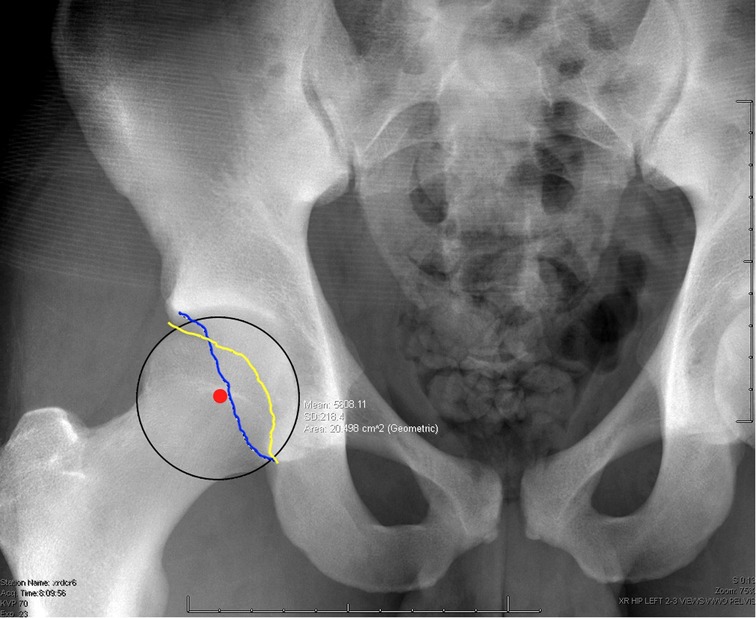
Figure 3. Anteroposterior radiograph of the hip demonstrating the cross oversign associated with acetabular retroversion. In the image the yellow line represents the anterior rim of the acetabulum, blue line reprents the posterior rim, and the red dot is the middle of the femoral head.
Microinstability
Despite the hip being one of the most stable joints in the human body, there is increased recognition of microinstability as a pathologic process associated with significant hip pain (52). Stability of the hip, much like that of any joint, is attributable to its constrained osseous anatomy, acetabular labrum that expands the volume, intracapsular and extracapsular ligamentous structures, and the 17 muscles that traverse the hip joint providing dynamic stability (52). However, pathology to single components may cause instability, without frank dislocations, that contribute to pain within the hip joint.
Osseous abnormalities, most notably in developmental dysplasia of the hip, is a source of likely microinstability of the hip. Patients with mild dysplasia, often termed borderline dysplasia, may often go unnoticed into their adult life, and is reported to be prevalent in 0.1% of the U.S. population (53). The lateral center-edge angle under 20o is often used as a marker for dysplasia (Figure 4). In previous studies, a decreased angle has been noted in 4% of hips with labral tears (54).
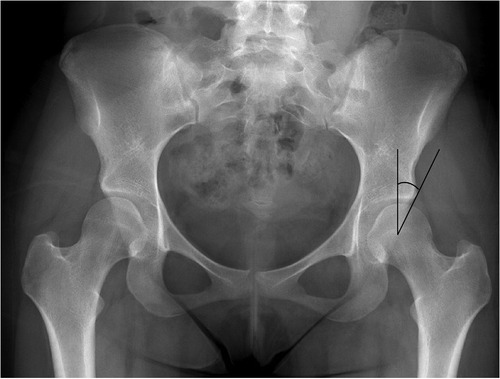
Figure 4. Anteroposterior radiographic image of a pelvis demonstrating left hip dysplasia, which is defined as the lateral center edge angle less than 20o.
There is increased controversy regarding the management of patients with borderline dysplasia. From review of the literature, Kirsch et al. found hip arthroscopy to be a viable option for patients with mild dysplasia, however, outlined contraindications as follows: (1) lateralization of femur >1 cm, break in Shenton's line, lateral center edge angle <20o, excess femoral and acetabular anteversion, excess coxa valga, dysplastic proximal femur, tonnis angle >10o, and pain with standing and straight-ahead walking (55). Parvizi and colleagues found that patients with dysplasia that underwent arthroscopic surgery had good short term outcomes (at 6 weeks), however, in the long-term, patients had an accelerated rate of osteoarthritis (46.7%), femoral head migration (43.3%), and need for further operative intervention (53.3%) (56).
Ligamentous structures of the hip also provide areas of possible pathology. The ligamentum teres and iliofemoral, pubofemoral, and ischiofemoral ligaments all confer stability to the hip (52). Damage to these ligamentous structures may be increasingly relevant in posttraumatic instability following hip dislocation or acetabular fracture. Alternatively, microinstability of the hip will have a higher differential in patients with history of connective tissue disorders such as Marfan's or Ehrler's Danlos syndromes.
Microinstability of the hip may be a result of FAIS or occur concurrently with the above-mentioned pathologies. Physical examination is a key aspect in identifying patients at risk. Three key provocative test maneuvers are the anterior apprehension test (performed in supination with the examinee holding the contralateral knee flexed to the chest and the examiner passively hyperextending the opposite knee), the abduction-extension-external rotation test (performed in lateral decubitus with the examined leg abducted to 30o and the examiner applying anteriorly directed force to the posterior greater trochanter), and the prone external rotation test (performed prone in neutral hip flexion and the examinee externally rotates the hip with the knee flexed and places anterior directed force on the posterior greater trochanter) (52). If all three tests are positive, there is a 95% likelihood of confirmation intraoperatively of microinstability (57). Magnetic resonance imaging is the key imaging modality for diagnosis of hip instability. However, magnetic resonance arthrograms may also be considered to confirm capsular defects visible with extravasation of fluid (57, 58).
Conclusion
The treatment of pre-arthritic hip pain is complex and often challenging as it may be multifactorial. While FAIS is a predominant etiology, multiple other considerations should be evaluated prior to surgery. Associated conditions discussed within the present review have the capacity to negatively impact patient outcomes when not addressed. Thereby, it is imperative that thorough physical exam maneuvers and advanced imaging is performed in the preoperative assessment to limit confounding diagnoses in the management of FIAS.
Author contributions
AKG: Conceptualization, methodology, validation, investigation, resources, writing- original draft, writing- review and editing, visualization. ECB: Conceptualization, methodology, validation, investigation, resources, writing- original draft, writing- review and editing, visualization. APT: Conceptualization, writing- original draft, writing- review and editing. CE: Conceptualization, writing- original draft, writing- review and editing. AJS: Conceptualization, methodology, investigation, resources, writing- original draft, writing- review and editing, visualization, supervision, project administration. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. DeAngelis NA, Busconi BD. Assessment and differential diagnosis of the painful hip. Clin Orthop Relat Res. (2003) 406:11–8. doi: 10.1097/01.blo.0000043039.84315.be
2. Boyd KT, Peirce NS, Batt ME. Common hip injuries in sport. Sports Med (Auckland, NZ). (1997) 24:273–88. doi: 10.2165/00007256-199724040-00005
3. Reiman MP, Agricola R, Kemp JL, Heerey JJ, Weir A, van Klij P, et al. Consensus recommendations on the classification, definition and diagnostic criteria of hip-related pain in young and middle-aged active adults from the International Hip-related Pain Research Network, Zurich 2018. Br J Sports Med. (2020) 54:631–41. doi: 10.1136/bjsports-2019-101453
4. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. (2003) 417:112–20. doi: 10.1097/01.blo.0000096804.78689.c2
5. Sankar WN, Nevitt M, Parvizi J, Felson DT, Agricola R, Leunig M. Femoroacetabular impingement: defining the condition and its role in the pathophysiology of osteoarthritis. J Am Acad Orthop Surg. (2013) 21(Suppl 1):S7–S15. doi: 10.5435/JAAOS-21-07-S7
6. Schairer WW, Nwachukwu BU, Suryavanshi JR, Yen Y-M, Kelly BT, Fabricant PD. A shift in hip arthroscopy use by patient age and surgeon volume: A New York state-based population analysis 2004 to 2016. Arthroscopy. (2019) 35:2847–2854.e1. doi: 10.1016/j.arthro.2019.05.008
7. Montgomery SR, Ngo SS, Hobson T, Nguyen S, Alluri R, Wang JC, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. (2013) 29:661–5. doi: 10.1016/j.arthro.2012.11.005
8. Kremers HM, Schilz SR, Van Houten HK, Herrin J, Koenig KM, Bozic KJ, et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty. (2017) 32:750–5. doi: 10.1016/j.arth.2016.09.004
9. Gebhart JJ, Streit JJ, Bedi A, Bush-Joseph CA, Nho SJ, Salata MJ. Correlation of pelvic incidence with cam and pincer lesions. Am J Sports Med. (2014) 42:2649–53. doi: 10.1177/0363546514548019
10. Pesenti S, Lafage R, Stein D, Elysee JC, Lenke LG, Schwab FJ, et al. The amount of proximal lumbar lordosis is related to pelvic incidence. Clin Orthop Relat Res. (2018) 476:1603–11. doi: 10.1097/CORR.0000000000000380
11. Yoshimoto H, Sato S, Masuda T, Kanno T, Shundo M, Hyakumachi T, et al. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine. (2005) 30:1650–7. doi: 10.1097/01.brs.0000169446.69758.fa
12. Weinberg DS, Gebhart JJ, Liu RW, Salata MJ. Radiographic signs of femoroacetabular impingement are associated with decreased pelvic incidence. Arthroscopy. (2016) 32:806–13. doi: 10.1016/j.arthro.2015.11.047
13. Fader RR, Tao MA, Gaudiani MA, Turk R, Nwachukwu BU, Esposito CI, et al. The role of lumbar lordosis and pelvic sagittal balance in femoroacetabular impingement. Bone Joint J. (2018) 100-B:1275–9. doi: 10.1302/0301-620X.100B10.BJJ-2018-0060.R1
14. Beck EC, Nwachukwu BU, Chapman R, Gowd AK, Waterman BR, Nho SJ. The influence of lumbosacral spine pathology on minimum 2-year outcome after hip arthroscopy: A nested case-control analysis. Am J Sports Med. (2020) 48:403–8. doi: 10.1177/0363546519892916
15. Heaps BM, Feingold JD, Swartwout E, Turcan S, Greditzer HG 4th, Kelly BT, et al. Lumbosacral transitional vertebrae predict inferior patient-reported outcomes after hip arthroscopy. Am J Sports Med. (2020) 48:3272–9. doi: 10.1177/0363546520961160
16. Haskel JD, Baron SL, Zusmanovich M, Youm T. Does concomitant lumbar spine disease adversely affect the outcomes of patients undergoing hip arthroscopy? Am J Sports Med. (2020) 48:2178–84. doi: 10.1177/0363546520929344
17. Cibulka MT, Sinacore DR, Cromer GS, Delitto A. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine. (1998) 23:1009–15. doi: 10.1097/00007632-199805010-00009
18. Krishnamoorthy VP, Kunze KN, Beck EC, Cancienne JM, O’Keefe LS, Ayeni OR, et al. Radiographic prevalence of symphysis pubis abnormalities and clinical outcomes in patients with femoroacetabular impingement syndrome. Am J Sports Med. (2019) 47:1467–72. doi: 10.1177/0363546519837203
19. Sembrano JN, Polly DW Jr. How often is low back pain not coming from the back? Spine. (2009) 34:E27–32. doi: 10.1097/BRS.0b013e31818b8882
20. Broadhurst NA, Bond MJ. Pain provocation tests for the assessment of sacroiliac joint dysfunction. J Spinal Disord. (1998) 11:341–5. doi: 10.1097/00002517-199808000-00013
21. Gartenberg A, Nessim A, Cho W. Sacroiliac joint dysfunction: pathophysiology, diagnosis, and treatment. Eur Spine J. (2021) 30:2936–43. doi: 10.1007/s00586-021-06927-9
22. Chung N-S, Jeon C-H, Lee H-D, Won S-H. Measurement of spinopelvic parameters on standing lateral lumbar radiographs: validity and reliability. Clin Spine Surg. (2017) 30:E119–23. doi: 10.1097/BSD.0000000000000448
23. Zarins B, Moncure A, Wakamatsu MM. Management of severe lower abdominal or inguinal pain in high-performance athletes. Am J Sports Med. (2000) 28:616–7. doi: 10.1177/03635465000280011501
24. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. (1982) 10:150–4. doi: 10.1177/036354658201000306
25. Nepple JJ, Brophy RH, Matava MJ, Wright RW, Clohisy JC. Radiographic findings of femoroacetabular impingement in National Football League Combine athletes undergoing radiographs for previous hip or groin pain. Arthroscopy. (2012) 28:1396–403. doi: 10.1016/j.arthro.2012.03.005
26. Munegato D, Bigoni M, Gridavilla G, Olmi S, Cesana G, Zatti G. Sports hernia and femoroacetabular impingement in athletes: A systematic review. World J Clin Cases. (2015) 3:823–30. doi: 10.12998/wjcc.v3.i9.823
27. Phillips E, Khoury V, Wilmot A, Kelly JD 4th. Correlation between cam-type femoroacetabular impingement and radiographic osteitis pubis. Orthopedics. (2016) 39:e417–22. doi: 10.3928/01477447-20160404-03
28. Lynch TS, Bedi A, Larson CM. Athletic hip injuries. J Am Acad Orthop Surg. (2017) 25:269–79. doi: 10.5435/JAAOS-D-16-00171
29. Kunduracioglu B, Yilmaz C, Yorubulut M, Kudas S. Magnetic resonance findings of osteitis pubis. J Magn Reson Imaging. (2007) 25:535–9. doi: 10.1002/jmri.20818
30. Omar IM, Zoga AC, Kavanagh EC, Koulouris G, Bergin D, Gopez AG, et al. Athletic pubalgia and “sports hernia”: optimal MR imaging technique and findings. Radiographics. (2008) 28:1415–38. doi: 10.1148/rg.285075217
31. Birmingham PM, Kelly BT, Jacobs R, McGrady L, Wang M. The effect of dynamic femoroacetabular impingement on pubic symphysis motion: a cadaveric study. Am J Sports Med. (2012) 40:1113–8. doi: 10.1177/0363546512437723
32. Kaya M. Impact of extra-articular pathologies on groin pain: An arthroscopic evaluation. Plos one. (2018) 13:e0191091. doi: 10.1371/journal.pone.0191091
33. Zoga AC, Kavanagh EC, Omar IM, Morrison WB, Koulouris G, Lopez H, et al. Athletic pubalgia and the “sports hernia”: mR imaging findings. Radiology. (2008) 247:797–807. doi: 10.1148/radiol.2473070049
34. Lerch TD, Siegfried M, Schmaranzer F, Leibold CS, Zurmühle CA, Hanke MS, et al. Location of intra-and extra-articular hip impingement is different in patients with pincer-type and mixed-type femoroacetabular impingement due to acetabular retroversion or protrusio acetabuli on 3D CT–based impingement simulation. Am J Sports Med. (2020) 48:661–72. doi: 10.1177/0363546519897273
35. Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: High validity of the “cross-over-sign.”. J Orthop Res. (2007) 25:758–65. doi: 10.1002/jor.20380
36. Maldonado DR, Chen JW, Kyin C, Rosinsky PJ, Shapira J, Karom JM, et al. Hips with acetabular retroversion can be safely treated with advanced arthroscopic techniques without anteverting periacetabular osteotomy: Midterm outcomes with propensity-matched control group. Am J Sports Med. (2020) 48:1636–46. doi: 10.1177/0363546520916737
37. Lerch TD, Boschung A, Todorski IA, Steppacher SD, Schmaranzer F, Zheng G, et al. Femoroacetabular impingement patients with decreased femoral version have different impingement locations and intra-and extraarticular anterior subspine FAI on 3D-CT–based impingement simulation: implications for hip arthroscopy. Am J Sports Med. (2019) 47:3120–32. doi: 10.1177/0363546519873666
38. Fabricant PD, Fields KG, Taylor SA, Magennis E, Bedi A, Kelly BT. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg. (2015) 97:537–43. doi: 10.2106/JBJS.N.00266
39. Fabry G, MacEwen GD, Shands AR. Torsion of the femur. A follow-up study in normal and abnormal conditions. J Bone Joint Surg Am. (1973) 55:1726–38. doi: 10.2106/00004623-197355080-00017
40. Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. (1999) 81:1747–70. doi: 10.2106/00004623-199912000-00014
41. Ruwe PA, Gage JR, Ozonoff MB, DeLuca PA. Clinical determination of femoral anteversion. A comparison with established techniques. J Bone Joint Surg Am. (1992) 74:820–30. doi: 10.2106/00004623-199274060-00003
42. Mesgarzadeh M, Revesz G, Bonakdarpour A. Femoral neck torsion angle measurement by computed tomography. J Comput Assist Tomogr. (1987) 11:799–803. doi: 10.1097/00004728-198709000-00011
43. Ratzlaff C, Simatovic J, Wong H, Li L, Ezzat A, Langford D, et al. Reliability of hip examination tests for femoroacetabular impingement. Arthritis Care Res (Hoboken). (2013) 65:1690–6. doi: 10.1002/acr.22036
44. Beaulé PE, Allen DJ, Clohisy JC, Schoenecker P, Leunig M. The young adult with hip impingement: deciding on the optimal intervention. J Bone Joint Surg Am. (2009) 91:210–21. doi: 10.2106/JBJS.H.00802
45. Drehmann F. Drehmann's sign. A clinical examination method in epiphysiolysis (slipping of the upper femoral epiphysis). Description of signs, aetiopathogenetic considerations, clinical experience (author's Transl). Z Orthop Ihre Grenzgeb. (1979) 117:333–44. PMID: 463224
46. Kamegaya M, Saisu T, Nakamura J, Murakami R, Segawa Y, Wakou M. Drehmann sign and femoro-acetabular impingement in SCFE. J Pediatr Orthop. (2011) 31:853–7. doi: 10.1097/BPO.0b013e31822ed320
47. Golfam M, Di Primio LA, Beaulé PE, Hack K, Schweitzer ME. Alpha angle measurements in healthy adult volunteers vary depending on the MRI plane acquisition used. Am J Sports Med. (2017) 45:620–6. doi: 10.1177/0363546516669138
48. van Bosse HJP, Lee D, Henderson ER, Sala DA, Feldman DS. Pelvic positioning creates error in CT acetabular measurements. Clin Orthop Relat Res. (2011) 469:1683–91. doi: 10.1007/s11999-011-1827-9
49. Kim WY, Hutchinson CE, Andrew JG, Allen PD. The relationship between acetabular retroversion and osteoarthritis of the hip. J Bone Joint Surg Br. (2006) 88:727–9. doi: 10.1302/0301-620X.88B6.17430
50. Direito-Santos B, França G, Nunes J, Costa A, Rodrigues EB, Silva AP, et al. Acetabular retroversion: diagnosis and treatment. EFORT Open Rev. (2018) 3:595–603. doi: 10.1302/2058-5241.3.180015
51. Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. (1999) 81:281–8. doi: 10.1302/0301-620x.81b2.8291
52. Safran MR. Microinstability of the hip-gaining acceptance. J Am Acad Orthop Surg. (2019) 27:12–22. doi: 10.5435/JAAOS-D-17-00664
53. Gala L, Clohisy JC, Beaulé PE. Hip dysplasia in the young adult. J Bone Joint Surg Am. (2016) 98:63–73. doi: 10.2106/JBJS.O.00109
54. Dolan MM, Heyworth BE, Bedi A, Duke G, Kelly BT. CT Reveals a high incidence of osseous abnormalities in hips with labral tears. Clin Orthop Relat Res. (2011) 469:831–8. doi: 10.1007/s11999-010-1539-6
55. Kirsch JM, Khan M, Bedi A. Does hip arthroscopy have a role in the treatment of developmental hip dysplasia? J Arthroplasty. (2017) 32:S28–31. doi: 10.1016/j.arth.2017.02.022
56. Parvizi J, Bican O, Bender B, Mortazavi SMJ, Purtill JJ, Erickson J, et al. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty. (2009) 24:110–3. doi: 10.1016/j.arth.2009.05.021
57. Magerkurth O, Jacobson JA, Morag Y, Caoili E, Fessell D, Sekiya JK. Capsular laxity of the hip: findings at magnetic resonance arthrography. Arthroscopy. (2013) 29:1615–22. doi: 10.1016/j.arthro.2013.07.261
Keywords: FAI (Femoroacetabular impingemet), sacroiliac pain, lumbosacral pain, osteitis pubis, pseudoradicular pain
Citation: Gowd AK, Beck EC, Trammell AP, Edge C and Stubbs AJ (2022) Evaluation of additional causes of hip pain in patients with femoroacetabular impingement syndrome. Front. Surg. 9:697488. doi: 10.3389/fsurg.2022.697488
Received: 19 April 2021; Accepted: 26 July 2022;
Published: 10 August 2022.
Edited by:
Olga Savvidou, National and Kapodistrian University of Athens, GreeceReviewed by:
Joseph M. Schwab, Medical College of Wisconsin, United StatesIoanna Bolia, University of Southern California, United States
© 2022 Gowd, Beck, Trammell, Edge and Stubbs. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anirudh K. Gowd YW5pcnVkaGtnb3dkQGdtYWlsLmNvbQ== Edward Charles Beck YmVja2Vkd2FyZDFAZ21haWwuY29t
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Anirudh K. Gowd
Anirudh K. Gowd Edward C. Beck
Edward C. Beck Amy P. Trammell
Amy P. Trammell Carl Edge
Carl Edge