
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 16 January 2023
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1107883
This article is part of the Research Topic Improving Patient Outcomes and Education in Minimally Invasive Spine Surgery View all 10 articles
 Xiaokang Cheng1,2,†,‡
Xiaokang Cheng1,2,†,‡ Beixi Bao1,†
Beixi Bao1,† Yuxuan Wu1
Yuxuan Wu1 Yuanpei Cheng3
Yuanpei Cheng3 Chunyang Xu1
Chunyang Xu1 Yang Ye1
Yang Ye1 Chentao Dou2
Chentao Dou2 Bin Chen2
Bin Chen2 Hui Yan1
Hui Yan1 Jiaguang Tang1*
Jiaguang Tang1*
Purpose: To compare the clinical outcomes of percutaneous transforaminal endoscopic discectomy (PTED) and unilateral biportal endoscopic discectomy (UBE) for the treatment of single-level lumbar disc herniation (LDH).
Materials and methods: From January 2020 to November 2021, 62 patients with single-level LDH were retrospectively reviewed. All patients underwent spinal surgeries at the Affiliated Hospital of Chengde Medical University and Beijing Tongren Hospital, Capital Medical University. Among them, 30 patients were treated with UBE, and 32 were treated with PTED. The patients were followed up for at least one year. Patient demographics and perioperative outcomes were reviewed before and after surgery. The Oswestry Disability Index (ODI), visual analog scale (VAS) for back pain and leg pain, and modified MacNab criteria were used to evaluate the clinical outcomes. x-ray examinations were performed one year after surgery to assess the stability of the lumbar spine.
Results: The mean ages in the UBE and PTED groups were 46.7 years and 48.0 years, respectively. Compared to the UBE group, the PTED group had better VAS scores for back pain at 1 and 7 days after surgery (3.06 ± 0.80 vs. 4.03 ± 0.81, P < 0.05; 2.81 ± 0.60 vs. 3.70 ± 0.79, P < 0.05). The UBE and PTED groups demonstrated significant improvements in the VAS score for leg pain and ODI score, and no significant differences were found between the groups at any time after the first month (P > 0.05). Although the good-to-excellent rate of the modified MacNab criteria in the UBE group was similar to that in the PTED group (86.7% vs. 87.5%, P > 0.05), PTED was advantageous in terms of the operation time, estimated blood loss, incision length, and length of postoperative hospital stay.
Conclusions: Both UBE and PTED have favorable outcomes in patients with single-level LDH. However, PTED is superior to UBE in terms of short-term postoperative back pain relief and perioperative quality of life.
Lumbar disc herniation (LDH), with the disc material extruded outside the normal intervertebral space, is the main cause of low back and lower extremity pain (1). Although conservative care remains the main strategy for treatment, discectomy is required when clinical symptoms cannot be resolved via nonsurgical treatment (2, 3).
With advances in medical technology, open discectomy has been gradually replaced by minimally invasive spine surgery, and microdiscectomy has become an important part of the treatment of LDH (4). Facilitated by the development of endoscopic equipment and techniques, a variety of modified minimally invasive lumbar surgical techniques have been developed (5).
To protect the normal spinal structure, percutaneous transforaminal endoscopic discectomy (PTED) for LDH was developed after it was proposed by Yeung in 1997 and Hoogland in 2003 (6, 7). Based on the safety area of the lumbar posterolateral zone, PTED could remove the herniated disc effectively under local anesthesia (8). With favorable clinical results and good perioperative quality of life, PTED is appreciated by many spinal surgeons and patients (9). However, in addition to its steep learning curve, this technique requires specialized equipment, and discectomy is limited by the working channel (10).
In recent years, unilateral biportal endoscopic discectomy (UBE) with an arthroscopy system has become increasingly popular, especially in Asia (11). UBE decompression is performed on the ipsilateral side via two small separated surgical portals. Compared to PTED, UBE is not limited by the uniportal tube (12). The surgeons could perform discectomy and annulus fibrosus suture in a magnified surgical field with a high-definition arthroscope and a clear surgical field with saline irrigation (13). Previous reports have also shown satisfactory clinical outcomes of UBE for cervical and thoracic spinal disease (14, 15).
Few studies have directly compared PTED and UBE for the treatment of LDH (16). Therefore, to explore the differences between the two surgical techniques, this study compared the clinical efficacy of UBE and PTED for treating single level LDH.
We performed a retrospective review in two hospitals of patients who underwent UBE and PTED from January 2020 to November 2021 after a diagnosis of single-level LDH. These surgeries were performed by two experienced surgeons. They had open lumbar surgery experience of more than 15 years, and PTED and UBE experience of more than 3 years. The baseline parameters of their demographic characteristics are given in Table 1. This retrospective study was approved by the Ethics Committee of the Chengde Medical University Affiliated Hospital, and written informed consent was obtained from the participants before data collection. The inclusion criteria were: (1) significant lower extremity radiating pain due to single-level LDH on x-ray, CT and MRI; (2) the absence of improvement after conservative treatment for at least three months; and (3) follow-up of at least 12 months after surgery. The exclusion criteria were: (1) mainly back pain symptoms or segmental instability on x-ray; (2) prior lumbar surgery; (3) tumor, infection, or trauma; and (4) inability to tolerate general anesthesia. The perioperative outcomes and complications were reviewed. An independent surgeon evaluated the VAS and ODI scores and modified MacNab criteria. x-ray examinations were performed one year after surgery to assess the segmental instability in both groups.
For the UBE group, the surgical procedure (based on the L4-L5 segment of LDH) was performed following methods reported in the literature (17). After successful general anesthesia with tracheal intubation, the patient was placed in a prone position with the abdomen draped, and the L4-L5 intervertebral space was marked with x-ray fluoroscopy. The initial target point is located at the junction of the inferior lamina and the spinous process of L4. The surgical bed is adjusted until the responsible intervertebral space is vertical to the floor to make the first horizontal line, and the second line is drawn along the inner edge of the pedicles of L4-L5. The observation and operation incision points on the body surface along the second line were approximately 0.5–1.0 cm from the intersection of the two lines (Figure 1). Two incisions were made, 0.8 cm–1.0 cm long, in the skin and subcutaneous fascia. Then, we bluntly expanded and separated the soft tissue covering the surface of the lamina to form the working and observation portals. With irrigation, the arthroscopic system was inserted into the observation portal. The soft tissue on the surface of the intervertebral space was removed by the plasma scalpel in the working portal. Next, the ipsilateral spinolaminar junction at the L4-L5 level was identified, laminotomy was performed with part of the inferior lamina of L4, and the superior lamina of L5 was removed with a drill. After the exposed ligamentum flavum was removed, the discectomy was conducted with Kerrison forceps. Finally, a drainage tube was placed after hemostasis. x-ray, CT and MRI were performed after surgery (Figure 2).
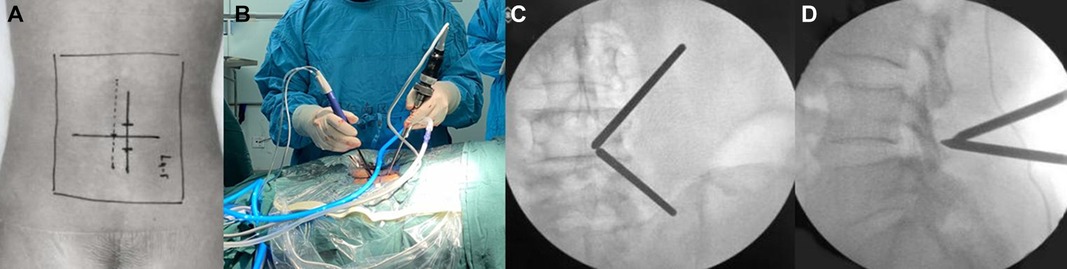
Figure 1. Intraoperative positioning and access establishment of UBE. (A,B) Body markers of L4/5 intervertebral space and the surgical approach. (C,D) The frontal and lateral view of the viewing and working portal.
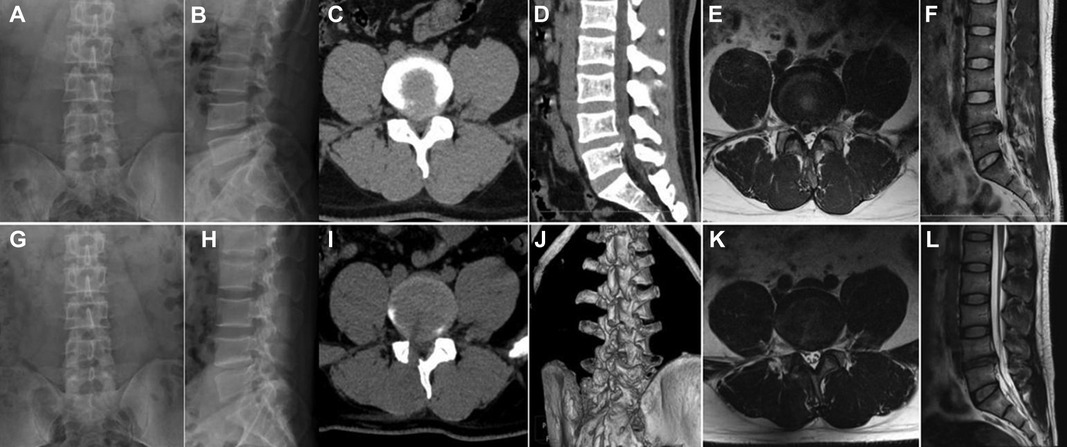
Figure 2. Pre- and postoperative x-ray, CT and MRI of UBE. (A,B) Preoperative x-ray. (C–F) Preoperative CT and MRI showing disc herniation. (G,H) Postoperative x-ray. (H,I) Postoperative CT and MRI showing the extruded disc was removed.
For the PTED group, the following steps (based on the L4-L5 segment of LDH) were performed following methods reported in the literature that we have published (18). A soft pillow was placed under the patient's waist while the patient was in the lateral decubitus position with their knee and hip flexed. The incision was located 8 cm–12 cm from the midline horizontally and 2 cm–4 cm above the iliac on the side with leg pain. A mixed local anesthetic, which consisted of 30 ml 1:200,000 epinephrine and 20 ml 2% lidocaine, was used. After 5 ml of the mixed anesthetic was inserted into the skin at the entry point, 20 ml was inserted into the trajectory, 15 ml was inserted into the articular process, and 10 ml was inserted into the foramen. Then, 0.8 cm–1.0 cm of skin and the subcutaneous fascia were incised. Drills were used to resect the ventral osteophytes on the superior articular process of L5. The PTED system (Hoogland Spine Products, Germany) was inserted (Figure 3). Parts of the ipsilateral ligamentum flavum and the extruded lumbar disc were completely resected with endoscopic forceps. The drainage tube was placed after hemostasis. X-ray, CT and MRI were performed after surgery (Figure 4).
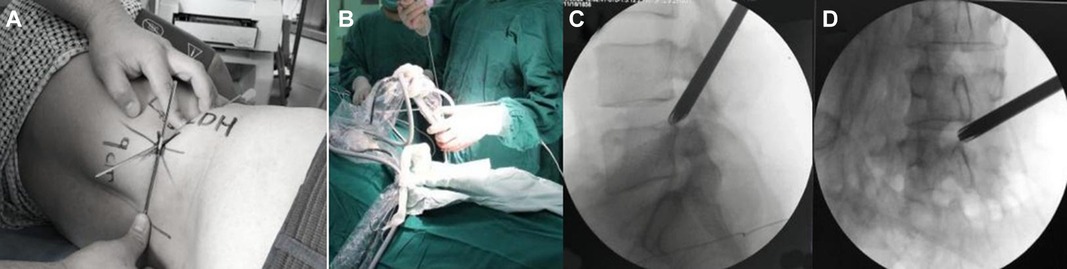
Figure 3. Intraoperative position and access establishment of PTED. (A,B) Body marker of L4/L5 intervertebral space and the surgical approach. (C,D) The lateral and frontal view of the working cannula.
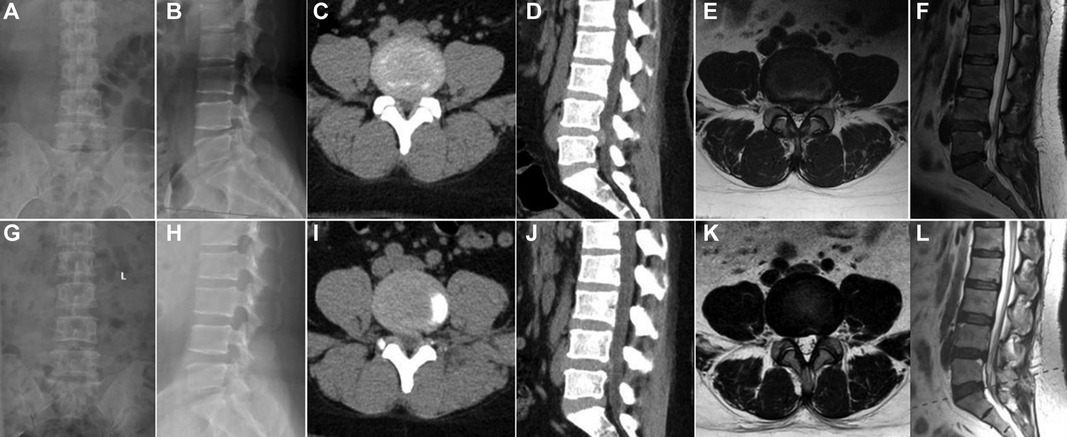
Figure 4. Pre- and postoperative x-ray, CT and MRI of PTED. (A,B) Preoperative x-ray. (C–F) Preoperative CT and MRI showing disc herniation. (G,H) Postoperative x-ray. (H,I) Postoperative CT and MRI showing the disc was removed.
The SPSS 26 program (IBM Corporation, United States) was used for statistical analysis. Repeated-measures analysis of variance was used to compare the VAS and ODI scores between the two groups. The independent-sample t test and Mann–Whitney U test or Fisher's exact test were used to assess the demographic characteristics and the perioperative outcomes. The level of statistical significance was set at P < 0.05.
Of the 62 patients who met the study inclusion criteria, 30 underwent UBE, and 32 underwent PTED. The surgical parameters, including the operative time, estimated blood loss, incision length, times of x-ray, length of hospital stay and number of complications, are shown in Table 2. Except times of x-ray, the perioperative outcomes of the patients who underwent PTED were better than those of the patients who underwent UBE.
Preoperatively, the mean VAS and ODI scores were similar between the two groups. Compared to the UBE group, the PTED group had better VAS scores for back pain at 1 day and 7 days after surgery (3.06 ± 0.80 vs. 4.03 ± 0.81, P < 0.05; 2.81 ± 0.60 vs. 3.70 ± 0.79, P < 0.05). At 12 months, we observed similar improvements in the mean VAS scores for back and leg pain and ODI scores in the PTED and UBE groups (Figure 5). Moreover, there were no differences between the groups at any follow-up time point after the first month (P > 0.05). Based on the modified MacNab criteria, the good-to-excellent rate was 86.7% (26/30) in the UBE group and 87.5% (28/32) in the PTED group at the final follow-up. During the one-year follow-up in both groups, no segmental instability occurred.
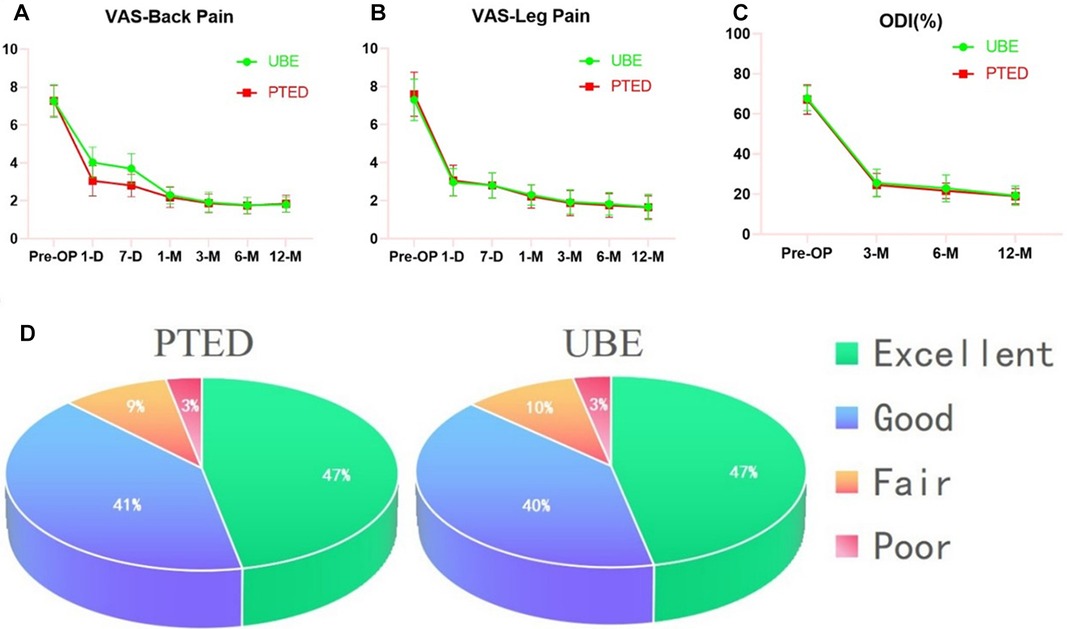
Figure 5. Clinical outcomes at different follow-up time points. (A) VAS score for back pain in both groups. (B) VAS score for leg pain in both groups. (C) ODI score for both groups. (D) The modified MacNab for both groups.
Three patients in the UBE group had a dural tear, and one experienced cerebrospinal fluid leakage and headache after the operation. These symptoms were relieved by adequate rest in the hospital bed and prolonging the drainage time. In the PTED group, one patient complained of dysesthesia and weakness of the tibialis anterior, which improved after a week with neurotrophic drugs; another patient had a dural tear without cerebrospinal fluid leakage. There were no serious complications related to surgery.
The significant improvements in the VAS score, ODI score and modified MacNab criteria revealed acceptable patient satisfaction in both groups, indicating that both PTED and UBE were effective in treating LDH. However, apartfrom times of x-ray, PTED is advantageous regarding the operative time, estimated blood loss, incision length, length of postoperative hospital stay, and short-term postoperative back pain relief.
For the surgical treatment of LDH, the most classic decompression is open laminectomy with or without fusion (19). However, open laminectomy destroys the paraspinal muscles and the posterior stabilizing structures. Therefore, a less invasive approach is needed to reduce injury and minimize surgical wounds during the treatment of lumbar disease (20).
As a microinvasive technique, PTED is widely applied for treating LDH with faster postoperative rehabilitation and less surgical injury. Compared to conventional open discectomy, PTED has the advantage of protecting the posterior ligament structures, facet joint and lamina. It avoids the need for nerve-root retraction and has a shorter hospitalization, reduced intraoperative bleeding, and faster recovery (21).
PTED can be completed under local anesthesia (22). After lidocaine combined with epinephrine hydrochloride solution is administered, the surgical field is clearer without obvious drug-related complications. The pressure of irrigation can also be appropriately reduced, theoretically reducing the incidence of spinal hypertension reactions (23). In addition, if the surgical equipment stimulates the nerve root during the operation, the awake patient will experience an abnormal sensation, and the surgeon can stop the process in a timely manner. The patient can be asked whether they subjectively feel their symptoms being alleviated, and the straight-leg test can be performed; these responses can be used to determine whether the operation should be terminated. Local anesthesia also reduces complications related to general anesthesia in elderly patients.
However, most hospitals in developing countries cannot afford to purchase these types of equipment and cannot master the technology quickly due to its steep learning curve. In addition, it is not easy to place the tube at the target point of the lateral approach if the iliac crest is high. In addition, the working places and visual field are limited to a single rigid working cannula.
Since first reported by De Antoni in 1996, UBE with arthroscopy has achieved good clinical effects (24). However, the development of UBE was limited due to the lack of power motor drills and the radiofrequency used to remove the lamina and achieve hemostasis. In recent years, with the emergence of endoscopic surgical instruments, UBE has been widely used in the treatment of LDH and lumbar spinal stenosis (25, 26).
Soliman proposed the application of this minimally invasive technology for the treatment of LDH in 2013 (27). He concluded that the surgical field of vision was expanded with different channels, and vascular bleeding was less under irrigation. The decompression process and instruments of UBE are similar to those used for open posterior discectomy, and thus this procedure can be carried out after only a short training period (28). Therefore, the learning curve of UBE is relatively flat and short. Xu demonstrated that the learning curve for mastering UBE is 54 cases (29).
The operating instruments and observation port are in different channels. The working port does not restrict the operating instruments of UBE. The working efficiency can be greatly improved with the use of conventional, large-sized surgical instruments, such as an osteotome, rongeur, forceps, and nerve retractor (30). In addition, surgeons in developing countries can complete the procedure without purchasing specialized supporting surgical instruments and other endoscopic systems. Moreover, unlike PTED, the UBE approach is not affected by a high iliac crest (31).
In our research, the operative time of UBE is longer than PTED. For one reason, the operative time for UBE is from the beginning of general anesthesia until a drainage tube is placed after hemostasis; the operative time for PTED is from the insertion of a local anesthetic to a drainage tube placed. For another, before laminotomy, the water pressure is 35 cm–40 cm H2O (32). But when performing the discectomy, to avoid potential neurological complications caused by the increased epidural and intracranial pressure and muscle edema caused by the high pressure of irrigation fluid, we lower the water pressure to 25 cm H2O (33). The time of hemostasis may be longer. So, the total operative time of UBE is longer than PTED in our research. But this does not mean that the efficiency of UBE is inferior to PTED in the progress of discectomy.
As for times of x-ray, the UBE group is superior to PTED in this research(6.13 ± 1.28 vs. 11.16 ± 3.71). Among the procedure of PTED, the times of x-ray was higher and mainly included: the process of local anesthesia, sequential dilators and bone drills insertion to expand the soft and osseous tissues by resecting the ventral osteophytes on the superior articular process, and the working cannula placement. In the UBE, the purpose of fluoroscopy is to find the junction of the inferior lamina and the spinous process and prevent mismaking of the target lumbar segment. So in terms of times of x-ray, the UBE group is superior to PTED.
However, the trauma of UBE is relatively larger than that of PTED (34). Due to the lack of a rigid cannula to dilate the soft tissue, the longissimus pectoralis and multifidus muscle need to be bluntly dissected to create a working space before decompression. The artificial creation of the operation spaces may damage the muscle attached to the lamina and the other anatomical structures. Therefore, theoretically, UBE would result in greater blood loss and worse postoperative back pain than PTED. The probability of cerebrospinal fluid leakage caused by dural injury when retraction of the nerve root is relatively high under general anesthesia (35).
In this research, three patients in the UBE group underwent dural tears when the anatomical structure was retracted to expose the disc. One of them experienced cerebrospinal fluid leakage and postoperative headache. The first dural tear occurred during the removal of the ligament flavum by the forceps with the low water pressure and the bleeding vision. The othe two dural tears were caused when the traversing roots was pushed by the assistant in a medial direction to expose the disc. We suggest that vigorous force cannot be used while pulling on the dura and an experienced assistant is needed. Besides, thorough hemostasis is needed when bleeding occurs before the next steps.
Additionally, one patient complained of weakness of the tibialis anterior in the PTED group. The working channel compresses the nerve root when the bone drill graves the upper articular of L5, which results in radicular symptoms. Another patient had a dural tear during the procedure but without cerebrospinal fluid leakage after the surgery. To avoid these complications, the surgeon should be careful when performing the foraminoplasty with a bone drill.
This study has some limitations. First, it was a retrospective study with a relatively short follow-up period and a small sample size. Second, the operation choices were limited. To confirm the long-term outcomes, a prospective and multicenter study with different surgical procedures and a larger sample size is necessary in future research.
Both UBE and PTED showed favorable outcomes for the treatment of single-level LDH. With less bone and muscle damage, PTED under local anesthesia exhibited less intraoperative blood loss, a shorter operation time, and shorter postoperative hospitalization than the UBE group.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Chengde Medical University Affiliated Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Conception and design: XKC, BXB and JGT. Acquisition of data: XKC, YXW and CYX. Drafting of the article: XKC and BXB. Critical revision of the article: JGT and HY. Statistical analysis: XKC, CTD and YPC. Administrative, technical and material support: BC, HY and JGT. Study supervision: JGT. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
LDH, lumbar disc herniation; PTED, Percutaneous transforaminal endoscopic discectomy; UBE, unilateral biportal endoscopic discectomy; DDD, Degenerative disc disease; VAS, The visual analog scale; ODI, Oswestry Disability Index.
1. Gadjradj PS, Rubinstein SM, Peul WC, Depauw PR, Vleggeert-Lankamp CL, Seiger A, et al. Full endoscopic versus open discectomy for sciatica: randomised controlled non-inferiority trial. Br Med J. (2022) 376:e065846.
2. Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. Br Med J. (2008) 336(7657):1355–8. doi: 10.1136/bmj.a143
3. Bailey CS, Glennie A, Rasoulinejad P, Kanawati A, Taylor D, Sequeira K, et al. Discectomy compared with standardized nonoperative care for chronic sciatica due to a lumbar disc herniation: a secondary analysis of a randomized controlled trial with 2-year follow-up. J Bone Joint Surg Am. (2021) 103(23):2161–9. doi: 10.2106/JBJS.21.00448
4. Chen Z, Zhang L, Dong J, Xie P, Liu B, Chen R, et al. Percutaneous transforaminal endoscopic discectomy versus microendoscopic discectomy for lumbar disc herniation: 5-year long-term results of a randomized controlled trial. Spine (Phila Pa 1976). (2023) 48(2):79–88. doi: 10.1097/BRS.0000000000004468
5. Wang Y, Liang Z, Wu J, Tu S, Chen C. Comparative clinical effectiveness of tubular microdiscectomy and conventional microdiscectomy for lumbar disc herniation: a systematic review and network meta-analysis. Spine (Phila Pa 1976). (2019) 44(14):1025–33. doi: 10.1097/BRS.0000000000003001
6. Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976). (2002) 27(7):722–31. doi: 10.1097/00007632-200204010-00009
7. Hoogland T, Schubert M, Miklitz B, Ramirez A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976). (2006) 31(24):E890–7. doi: 10.1097/01.brs.0000245955.22358.3a
8. Ge R, Liu Z, Huang W. Percutaneous transforaminal endoscopic discectomy is a safer approach for lumbar disc herniation. Am J Transl Res. (2022) 14(9):6359–67.36247293
9. Cheng XK, Chen B. Percutaneous transforaminal endoscopic decompression for geriatric patients with central spinal stenosis and degenerative lumbar spondylolisthesis: a novel surgical technique and clinical outcomes. Clin Interv Aging. (2020) 15:1213–9. doi: 10.2147/CIA.S258702
10. Jiang HW, Chen CD, Zhan BS, Wang YL, Tang P, Jiang XS. Unilateral biportal endoscopic discectomy versus percutaneous endoscopic lumbar discectomy in treating lumbar disc herniation: a retrospective study. J Orthop Surg Res. (2022) 17(1):30. doi: 10.1186/s13018-022-02929-5
11. Wang B, He P, Liu X, Wu Z, Xu B. Complications of unilateral biportal endoscopic spinal surgery for lumbar spinal stenosis: A systematic review of the literature and meta-analysis of single-arm studies. Orthop Surg. (2022). doi: 10.1111/os.13437. [Epub ahead of print]
12. Yuan C, Wen B, Lin H. Clinical analysis of minimally invasive percutaneous treatment of severe lumbar disc herniation with UBE two-channel endoscopy and foraminal single-channel endoscopy technique. Oxid Med Cell Longev. (2022) 2022:9264852.36275895
13. Hong YH, Kim SK, Hwang J, Eum JH, Heo DH, Suh DW, et al. Water dynamics in unilateral biportal endoscopic spine surgery and its related factors: an in vivo proportional regression and proficiency-matched study. World Neurosurg. (2021) 149:e836–43. doi: 10.1016/j.wneu.2021.01.086
14. Park JH, Jun SG, Jung JT, Lee SJ. Posterior percutaneous endoscopic cervical foraminotomy and diskectomy with unilateral biportal endoscopy. Orthopedics. (2017) 40(5):e779–83.28585996
15. Deng Y, Yang M, Xia C, Chen Y, Xie Z. Unilateral biportal endoscopic decompression for symptomatic thoracic ossification of the ligamentum flavum: a case control study. Int Orthop. (2022) 46(9):2071–80. doi: 10.1007/s00264-022-05484-0
16. Hao J, Cheng J, Xue H, Zhang F. Clinical comparison of unilateral biportal endoscopic discectomy with percutaneous endoscopic lumbar discectomy for single l4/5-level lumbar disk herniation. Pain Pract. (2022) 22(2):191–9. doi: 10.1111/papr.13078
17. Chang H, Xu J, Yang D, Sun J, Gao X, Ding W. Comparison of full-endoscopic foraminoplasty and lumbar discectomy (FEFLD), unilateral biportal endoscopic (UBE) discectomy, and microdiscectomy (MD) for symptomatic lumbar disc herniation. Eur Spine J. (2022) doi: 10.1007/s00586-022-07510-6. [Epub ahead of print]
18. Cheng XK, Cheng YP, Liu ZY, Bian FC, Yang FK, Yang N, et al. Percutaneous transforaminal endoscopic decompression for lumbar spinal stenosis with degenerative spondylolisthesis in the elderly. Clin Neurol Neurosurg. (2020) 194:105918. doi: 10.1016/j.clineuro.2020.105918
19. Hu ZX, Han J, Sun YF, Tian XL. Comparison of percutaneous endoscopic lumbar discectomy vs. Minimally invasive transforaminal lumbar interbody fusion for the treatment of single-segment lumbar disc herniation: a meta-analysis. Eur Rev Med Pharmacol Sci. (2022) 26:6678–90.36196718
20. Li WS, Yan Q, Cong L. Comparison of endoscopic discectomy versus non-endoscopic discectomy for symptomatic lumbar disc herniation: a systematic review and meta-analysis. Global Spine J. (2022) 12(5):1012–26. doi: 10.1177/21925682211020696
21. Wei FL, Zhou CP, Zhu KL, Du MR, Liu Y, Heng W, et al. Comparison of different operative approaches for lumbar disc herniation: a network meta-analysis and systematic review. Pain Physician. (2021) 24(4):E381–92.34213864
22. Youn MS, Shin JK, Goh TS, Son SM, Lee JS. Endoscopic posterior decompression under local anesthesia for degenerative lumbar spinal stenosis. J Neurosurg Spine. (2018) 29:661–6. doi: 10.3171/2018.5.SPINE171337
23. Cho JY, Lee SH, Lee HY. Prevention of development of postoperative dysesthesia in transforaminal percutaneous endoscopic lumbar discectomy for intracanalicular lumbar disc herniation: floating retraction technique. Minim Invasive Neurosurg. (2011) 54(5-6):214–8.22287030
24. De Antoni DJ, Claro ML, Poehling GG, Hughes SS. Translaminar lumbar epidural endoscopy: anatomy, technique, and indications. Arthroscopy. (1996) 12:330–4. doi: 10.1016/S0749-8063(96)90069-9
25. Kwon O, Yoo SJ, Park JY. Comparison of unilateral biportal endoscopic discectomy with other surgical technics: A systemic review of indications and outcomes of unilateral biportal endoscopic discectomy from the current literature. World Neurosurg. (2022) 168:349–58. doi: 10.1016/j.wneu.2022.06.153
26. Aygun H, Abdulshafi K. Unilateral biportal endoscopy versus tubular microendoscopy in management of single level degenerative lumbar canal stenosis: a prospective study. Clin Spine Surg. (2021) 34(6):E323–8. doi: 10.1097/BSD.0000000000001122
27. Soliman HM. Irrigation endoscopic discectomy: a novel percutaneous approach for lumbar disc prolapse. Eur Spine J. (2013) 22(5):1037–44. doi: 10.1007/s00586-013-2701-0
28. Chen L, Zhu B, Zhong HZ, Wang YG, Sun YS, Wang QF, et al. The learning curve of unilateral biportal endoscopic (UBE) spinal surgery by CUSUM analysis. Front Surg. (2022) 9:873691. doi: 10.3389/fsurg.2022.873691
29. Xu J, Wang D, Liu J, Zhu C, Bao J, Gao W, et al. Learning curve and complications of unilateral biportal endoscopy: cumulative sum and risk-adjusted cumulative sum analysis. Neurospine. (2022) 19(3):792–804. doi: 10.14245/ns.2143116.558
30. Zheng B, Xu S, Guo C, Jin L, Liu C, Liu H. Efficacy and safety of unilateral biportal endoscopy versus other spine surgery: a systematic review and meta-analysis. Front Surg. (2022) 9:911914. doi: 10.3389/fsurg.2022.911914
31. Eun SS, Eum JH, Lee SH, Sabal LA. Biportal endoscopic lumbar decompression for lumbar disk herniation and spinal canal stenosis: a technical note. J Neurol Surg A Cent Eur Neurosurg. (2017) 78(4):390–6. doi: 10.1055/s-0036-1592157
32. Kang MS, Park HJ, Hwang JH, Kim JE, Choi DJ, Chung HJ. Safety evaluation of biportal endoscopic lumbar discectomy: assessment of cervical epidural pressure during surgery. Spine (Phila Pa 1976). (2020) 45(20):E1349–1356. doi: 10.1097/BRS.0000000000003585
33. Kang T, Park SY, Lee SH, Park JH, Suh SW. Assessing changes in cervical epidural pressure during biportal endoscopic lumbar discectomy. J Neurosurg Spine. (2020) 30:1–7. doi: 10.3171/2020.6.SPINE20586
34. Choi KC, Shim HK, Hwang JS, Shin SH, Lee DC, Jung HH, et al. Comparison of surgical invasiveness between microdiscectomy and 3 different endoscopic discectomy techniques for lumbar disc herniation. World Neurosurg. (2018) 116:e750–758. doi: 10.1016/j.wneu.2018.05.085
35. Chu PL, Wang T, Zheng JL, Xu CQ, Yan YJ, Ma QS, et al. Global and current research trends of unilateral biportal endoscopy/biportal endoscopic spinal surgery in the treatment of lumbar degenerative diseases: a bibliometric and visualization study. Orthop Surg. (2022) 14(4):635–43. doi: 10.1111/os.13216
Keywords: lumbar disc herniation, percutaneous transforaminal endoscopic discectomy, unilateral biportal endoscopic discectomy, endoscopic, minimally invasive surgery
Citation: Cheng X, Bao B, Wu Y, Cheng Y, Xu C, Ye Y, Dou C, Chen B, Yan H and Tang J (2023) Clinical comparison of percutaneous transforaminal endoscopic discectomy and unilateral biportal endoscopic discectomy for single-level lumbar disc herniation. Front. Surg. 9:1107883. doi: 10.3389/fsurg.2022.1107883
Received: 25 November 2022; Accepted: 30 December 2022;
Published: 16 January 2023.
Edited by:
Ji Tu, University of New South Wales, AustraliaReviewed by:
Keyi Yu, Peking Union Medical College Hospital (CAMS), China© 2023 Cheng, Bao, Wu, Cheng, Xu, Ye, Dou, Chen, Yan and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiaguang Tang dGFuZ2ppYWd1YW5nMjAxM0AxNjMuY29t
†These authors have contributed equally to this work and share first authorship
‡ORCID Xiaokang Cheng orcid.org/0000-0002-9709-2428
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.