- 1Department of Orthopedics, The Second Hospital of Anhui Medical University, Hefei, China
- 2Institute of Orthopedics, Research Center for Translational Medicine, The Second Hospital of Anhui Medical University, Hefei, China
There are three traditional surgical approaches to hemiarthroplasty (HA) for femoral neck fractures, respectively, the anterior approach (AA), the lateral approach (LA) and the posterior approach (PA). However, the optimum approach is still controversial, the purpose of this meta-analysis is to identify the merits and demerits of all three approaches. All clinical published studies in PubMed, Web of Science, Embase, and the Cochrane Library from January 2000 to April 2022 were searched which compared different surgical approaches and covered surgery-related outcomes and frequent complications. Five randomized controlled trials and 26 cohort studies for a total of 31 clinical trials were included in the meta-analysis. The dislocation of PA was significantly higher than LA (OR: 3.00 95% CI: 2.25–4.01 I2 = 27% P < 0.00001) and AA (OR: 6.61 95% CI: 2.28–19.13 I2 = 0% P = 0.0005); PA was substantially more than LA in terms of risk of postoperative reoperation (P < 0.05); meanwhile, AA has markedly shorter hospital length of stays than LA. The remaining items showed no significant differences in the results.The results of this meta-analysis demonstrated that the risk of PA dislocation and reoperation is higher with hemiarthroplasty, and AA has markedly shorter hospital length of stays than LA.
Introduction
Femoral neck fractures are a common type of fracture in elderly individuals, accounting for approximately 57%∼64% of hip fractures, with projections estimating the total number of hip fractures worldwide to be approximately 4 million in 2025 (1, 2). Hip arthroplasty is a clinically widespread surgical procedure for the therapy of severely aged femoral neck fractures (3). However, patients with a combination of multiple underlying illnesses, poor health conditions and lower functional demands are more appropriate for artificial femoral head hemiarthroplasty, which can reduce the operation time and allow patients to move early after surgery (4–6).
There are various approaches to hemiarthroplasty, such as the direct anterior approach (DAA) (7), the lateral approach (8), and the true posterior approach (9). Different approaches impact the patient's early postoperative mobility and the occurrence of complications (10). We took van's categorization methodology and classified all the diverse approaches inductively as the anterior approach (AA), the lateral approach (LA) and the posterior approach (PA) (11). Some clinical research has compared two or three of these approaches, but the specific approach with absolute superiority remains indistinguishable, and some authors have tried to perform an analysis using meta-analysis (11, 12), but the number of reports is low and not exhaustive, and the current evidence needs to be updated. Therefore, we performed a meta-analysis comparing the three approaches to examine their possible advantages in terms of complications, postoperative functional outcomes, and surgical outcomes.
Materials and methods
Methodology
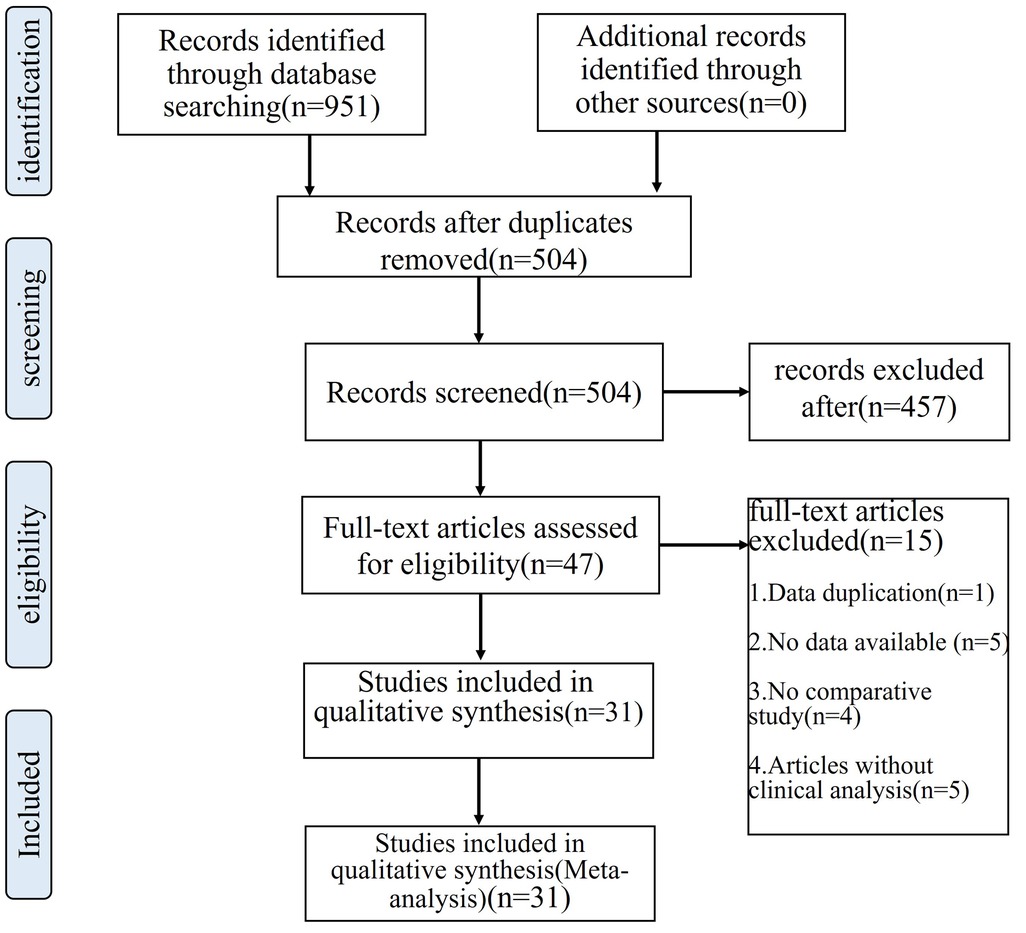
This systematic review adhered to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement. The literature search strictly followed the PICO (Participant, Intervention, Comparison, Outcome) principles. All personnel in this study were involved in designing the search strategy and were trained in search knowledge. A comprehensive search of known databases was conducted to find suitable articles for analysis.
We performed a literature search for studies published in PubMed (n = 233), EMBASE (n = 474), Web of Science (n = 181), and the Cochrane Central Register of Controlled Trials (n = 63), finding relevant research published from January 2000 to April 2022, regardless of language. Search for their subject terms and free words of “hemiarthroplasty”, “approach” and “hip”, and various combinations of related words, with the exact search formula referenced to van der Sijp (11). Through the combination of subject words and free words, the articles were screened comprehensively.
Data abstraction
Two separate writers entered data taken from the included research. Any differences were settled by consensus or dialog with the senior author. Titles and abstracts were reviewed, and inconsistencies were subjected to a full-text search to determine eligibility and settle conflicts by consensus. Sample size, research design, patient age, kind of operation, follow-up data, and outcome data were all retrieved (i.e., surgical outcomes, complications, clinical outcomes).
Quality assessment
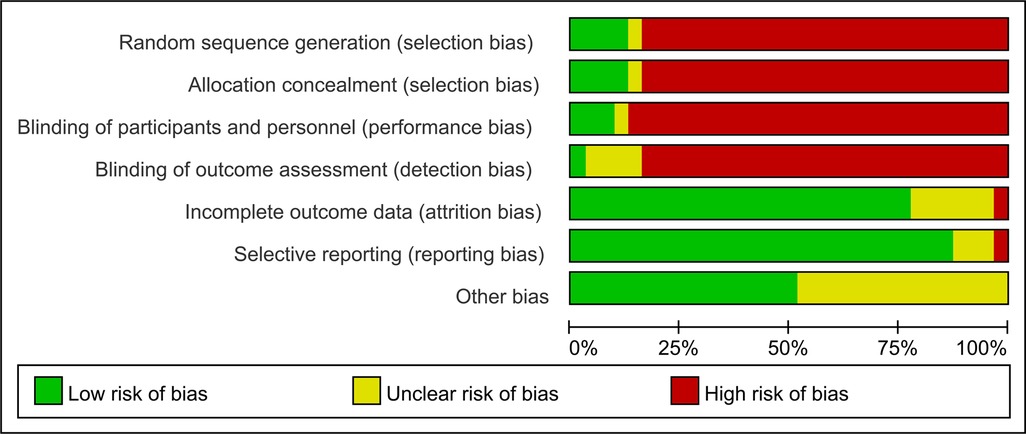
Two writers independently assessed the risk of bias in the papers that were included; if there was a disagreement regarding the results, it was addressed through conversation or with the help of a third investigator. The quality of the methodology of the enrolled research was assessed on the basis of the Cochrane Quality Assessment Form provided by Review Manager (RevMan) 5.4 software in six main areas: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases (13). Each type of bias was judged as low risk, high risk, or unclear risk, and a risk of bias map was generated.
Statistical analysis
Review Manager (RevMan) [Computer program]. Version 5.4.1, The Cochrane Collaboration, 2020, was used to analyze the selected studies. For data extraction, the basic information mainly included study type, follow-up time, sample size of control and intervention groups, age, body mass index (BMI), etc. Specific indicators were surgical outcomes, complications, and clinical outcomes.
The standard deviation (SD) was utilized to compute the mean difference (MD) or Std. mean difference (SMD) and 95 percent confidence interval for continuous data such as length of hospitalization, operation time and surgical blood loss. The odds ratio (OR) and 95% confidence interval (CI) were used for dichotomous data. The χ2 test result and the value of I2 were used to examine statistical heterogeneity.
Different authors provide various figures, including medians, ranges or quartiles, and we converted the desired results into means and standard deviations by referring to the statistical method introduced by Wan (14), which is an improvement on the one provided by Hozo and Bland (15, 16), thus bringing the individual values closer to the true value of the data itself and minimizing errors.
To begin, I2 was used to test the heterogeneity of the results of the included literature; if I2 > 50%, P < 0.1, which means that there is a large heterogeneity in the included studies; we will explore the reasons for the heterogeneity and conduct sensitivity analysis. In case it is still impossible to eliminate the heterogeneity of the literature, providing clinical consistency, then use the random effect model. If the heterogeneity of the literature was low, a fixed effects model was used.
Results
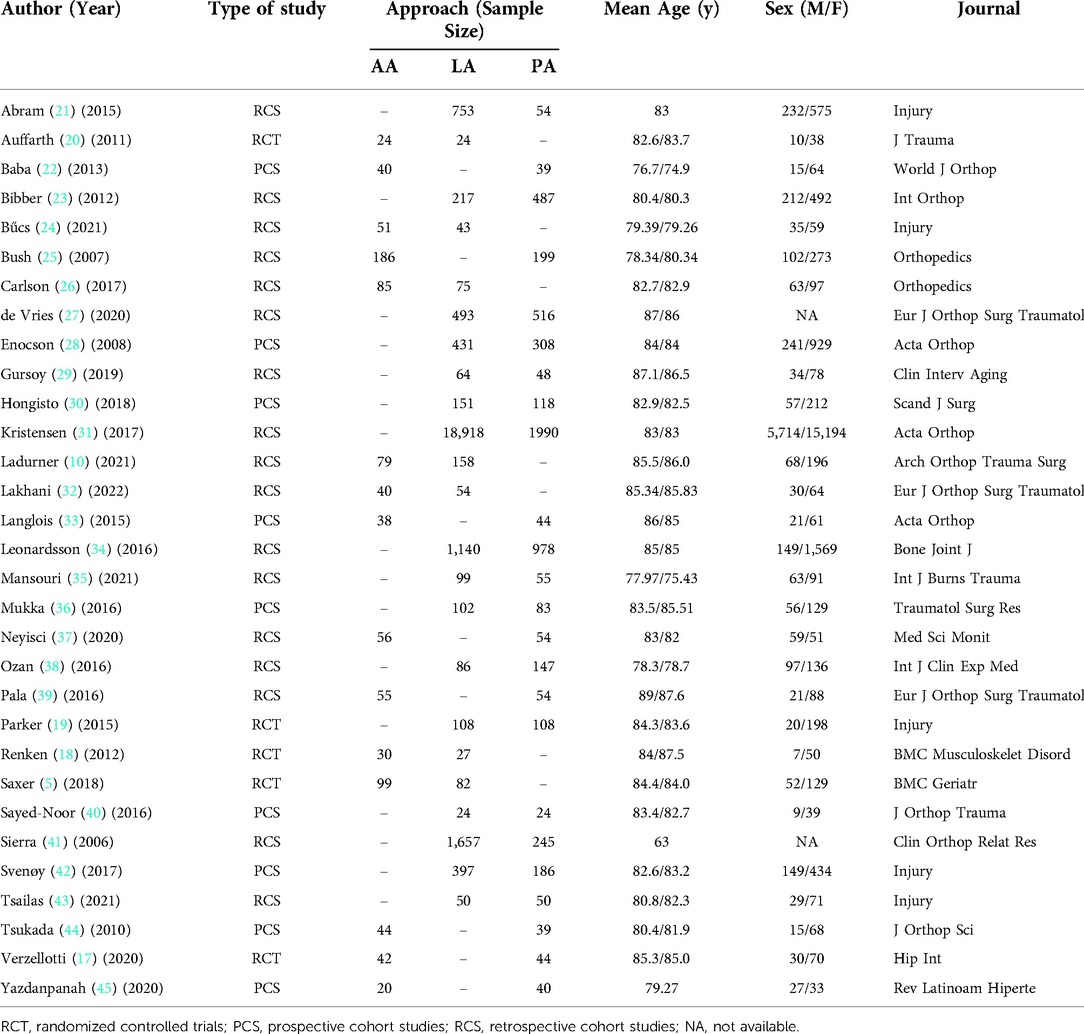
A series of 951 relevant articles were accessed in the search database for this research, and after analysis of titles, abstracts, and full text, 31 studies involving the hip were qualified and incorporated into the definitive meta-analysis Figure 1. Detailed descriptions of the characteristics and patient demographics for each study are listed in Table 1. Five were randomized controlled trials (5, 17–20) (RCTs) including 588 hips and the others were cohort studies.
The danger of selection bias was considerable since just five of the included studies were assigned randomly, accounting for approximately 16% of the total. Because there were so few participants and personnel blinding procedures were used, performance and detection biases were very substantial. The risk of attrition and reporting bias was low, but the risk of other biases was moderate, as shown in Figure 2.
Length of hospitalization
Regarding patient length of stay, four studies (10, 24, 26, 32) reported results comparing AA with LA as well as six studies (22, 25, 33, 37, 39, 44) showed results for PA and AA. The meta-analysis showed a statistically significant difference in length of stay when comparing AA with LA (SMD: −2.79 95% CI: −4.40–1.19 I2 = 98% P = 0.0006 Figure 3A). There was no significant difference between PA and AA (MD: 0.68 95% CI: −1.52–2.87 I2 = 86% P = 0.55 Figure 3B). Nevertheless, the number of reported cases for PA and LA was too small, and only de Vries (27) (P = 0.58) and Tsailas (43) (P = 0.25) were compared, both without differences.
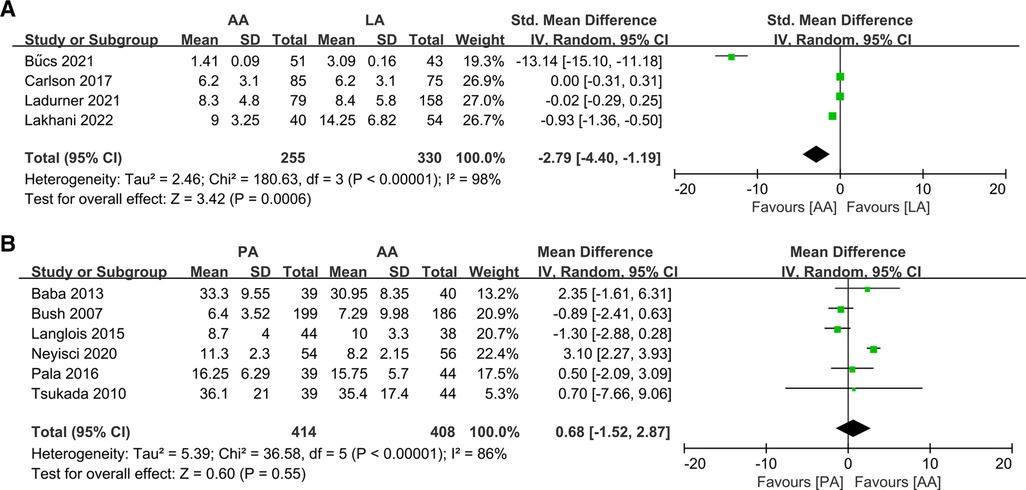
Figure 3. Forest plot comparison of length of hospitalization. (A) Anterior approach and lateral approach, (B) Anterior approach and posterior approach.
Operation time
Sixteen studies reported the operation time of the 2 methods. The analysis showed no statistically significant differences in all comparisons of operative times: AA vs. LA (10, 20, 24, 26, 32) (MD: −1.01 95% CI: −7.05–5.04 I2 = 91% P = 0.74 Figure 4A); PA vs. LA (29, 31, 36, 42, 43) (MD: −6.11 95% CI: −14.27–2.06 I2 = 97% P = 0.14 Figure 4B); PA vs. AA (17, 22, 33, 39, 44, 45) (MD: 4.55 95% CI: −13.40–22.51 I2 = 99% P = 0.62 Figure 4C). All I2 ≥ 50% and there was statistical heterogeneity, hence the random effects model was used for analysis.
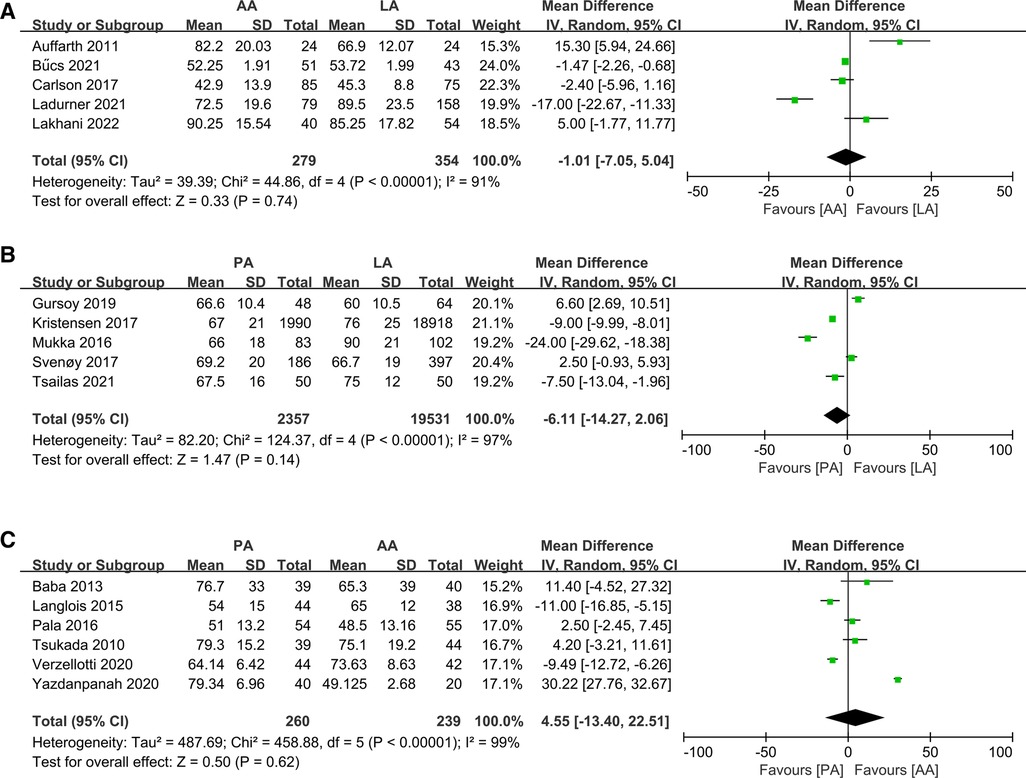
Figure 4. Forest plot comparison of operation time. (A) Anterior approach and lateral approach, (B) Posterior approach and lateral approach, (C) Posterior approach and anterior approach.
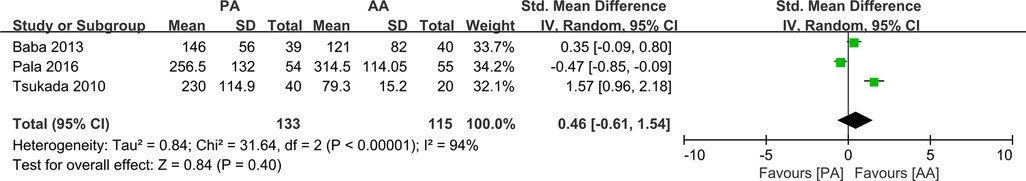
Surgical blood loss
Numerous reports have compared surgical blood loss in different methods, including intraoperative blood loss or transfusion in different units, changes in preoperative and postoperative hemoglobin levels, transfusion rates, and hematoma formation. However, only comparative studies of AA and PA could be converted to uniform units for analysis (22, 39, 44). The outcome demonstrated no significant difference in surgical blood loss between the PA and AA groups (SMD: −0.46 95% CI: −0.61–1.54 I2 = 94% P = 0.40 Figure 5).
Dislocation
Postoperative dislocation rates were reported in all 15 papers (19, 21, 23, 27–30, 34–36, 38, 40–43), and heterogeneity analysis showed no significant heterogeneity with I2 = 27% P = 0. 16, and meta-analysis was conducted using a fixed effects model. The data showed a statistically significant difference in the dislocation rate between the PA and LA groups (OR: 3.00 95% CI: 2.25–4.01 I2 = 27% P < 0.00001 Figure 6A). Simultaneously, after analyzing the data provided by the six articles comparing PA and AA (22, 25, 33, 39, 44, 45), a statistically significant difference was found (OR: 6.61 95% CI: 2.2819.13 I2 = 0% P = 0.0005 Figure 6B). As can be seen, the rate of dislocation was significantly higher in the PA group than in the other two groups. Carlson (26) and Lakhani (32) reported complications of DA and LA dislocation, and although statistical analysis could not be performed, no significant differences were detected on either side.
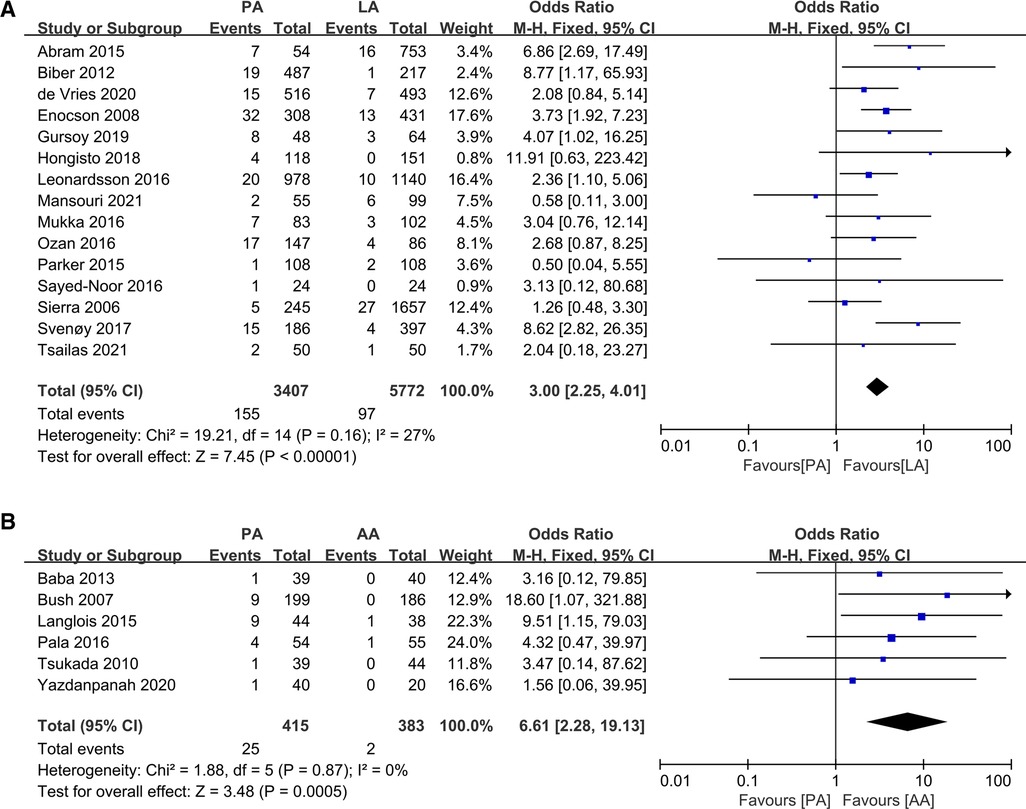
Figure 6. Forest plot comparison of dislocation. (A) Anterior approach and lateral approach, (B) Posterior approach and anterior approach.
Wound infections
All four studies (5, 20, 26, 32) concluded that no statistically significant difference in the risk of infection was observed between PA and AA, and we did not detect a statistically significant difference when we performed an aggregate analysis (OR: 1.85 95% CI: 0.77–4.43 I2 = 0% P = 0.17 Figure 7A). We obtained the same conclusion in the PA and LA studies (19, 23, 27, 29, 34–36, 38, 42) (OR: 1.18 95% CI: 0.87–1.59 I2 = 0% P = 0.28 Figure 7B).
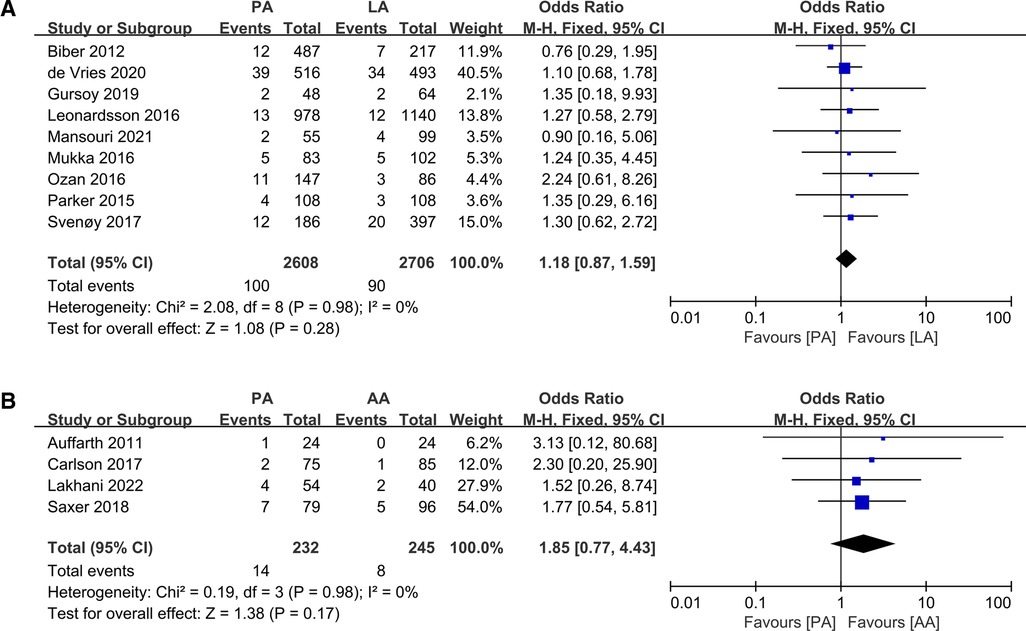
Figure 7. Forest plot comparison of wound infections. (A) Posterior approach and lateral approach, (B) Posterior approach and anterior approach.
Fractures
A series of 15 studies investigating surgery-related fracture complications were reported. Pooling data from 3 studies (20, 26, 32) comparing LA and AA did not reveal statistically significant differences (OR: 0.56 95% CI: 0.16–1.98 I2 = 0% P = 0.37 Figure 8A), while 8 studies (19, 23, 27, 29, 34, 36, 42, 43) analyzed PA and LA (OR: 0.87 95% CI: 0.55–1.36 I2 = 0% P = 0.53 Figure 8B), and another 4 (22, 39, 44, 45) compared LA with AA (OR: 0.71 95% CI: 0.18–2.79 I2 = 0% P = 0.62 Figure 8C).
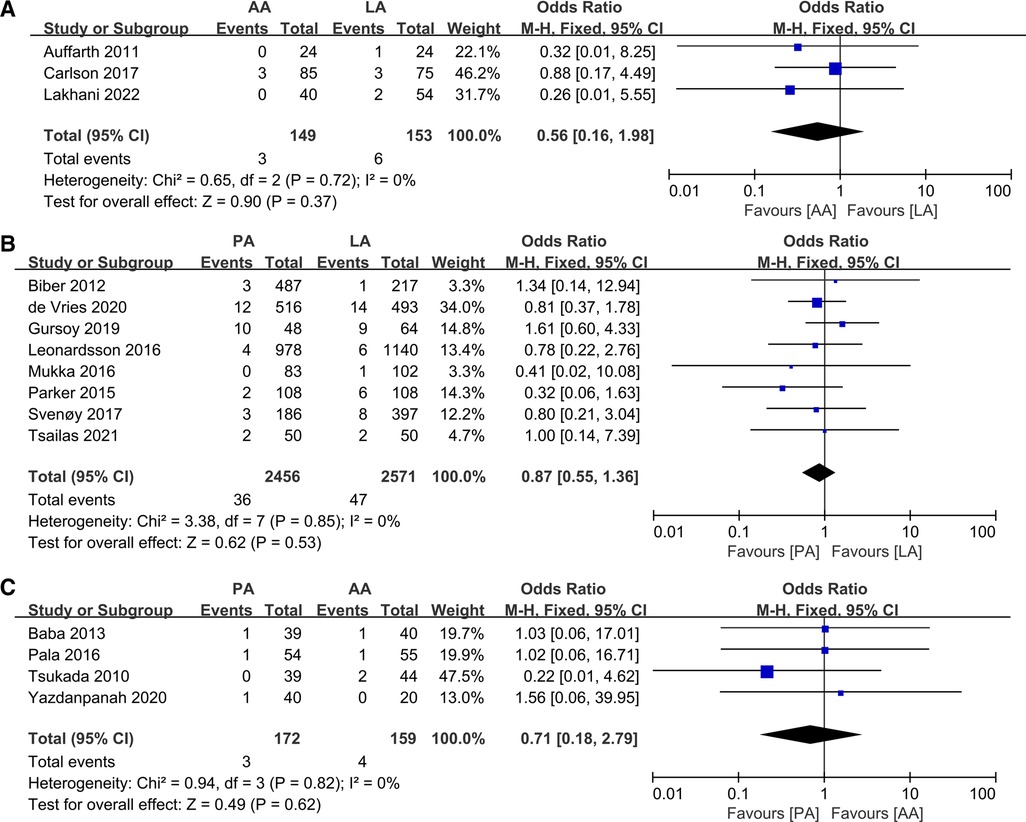
Figure 8. Forest plot comparison of fractures. (A) Anterior approach and lateral approach, (B) Posterior approach and lateral approach, (C) Posterior approach and anterior approach.
Reoperations
Six papers (5, 10, 18, 20, 26, 32) reported reoperation rates for AA and LA, with no significant heterogeneity between them, and meta-analysis was conducted using a fixed-effects model. The data revealed no statistically significant differences (OR: 0.83 95% CI: 0.42–1.62 I2 = 0% P = 0.58 Figure 9A). Nevertheless, 8 articles (19, 21, 31, 34–36, 41, 43) offered data on PA and LA reoperation, of which Kristensen (31) et al. provided only the rate of postoperative dislocation, without clarifying whether surgical treatment or conservative management was taken after dislocation, and they were excluded from the analysis. The results showed a significant discrepancy (OR: 1.45 95% CI: 1.02–2.06 I2 = 0% P = 0.04 Figure 9B), which may be impacted by the rate of surgical dislocation. Only Langlois (33) et al. compared reoperation rates for PA vs. AA, but no significant difference was reported.
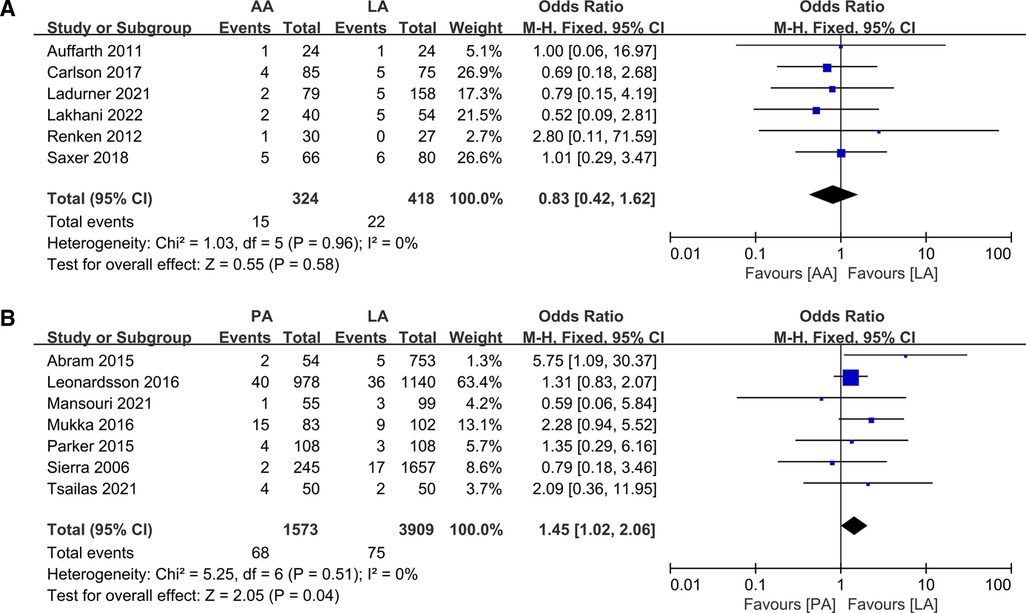
Figure 9. Forest plot comparison of reoperation. (A) Anterior approach and lateral approach, (B) Posterior approach and lateral approach.
Mortality
Mortality was examined in 17 studies with a total of 7,496 patients and 1,584 deaths. Numerous studies had variable follow-up times for mortality, including 1 month, 3 months, 6 months, 12 months and final mortality, and we adopted the use of most data with 1 year of follow-up for the analysis. There was no significant difference between the groups. The details are as follows, (OR: 0.78 95% CI: 0.52–1.17 I2 = 41% P = 0.24 Figure 10A), (OR: 0.95 95% CI: 0.53–1.71 I2 = 0% P = 0.87 Figure 10B), (OR: 1.00 95% CI: 0.88–1.13 I2 = 0% P = 0.99 Figure 1C), respectively.
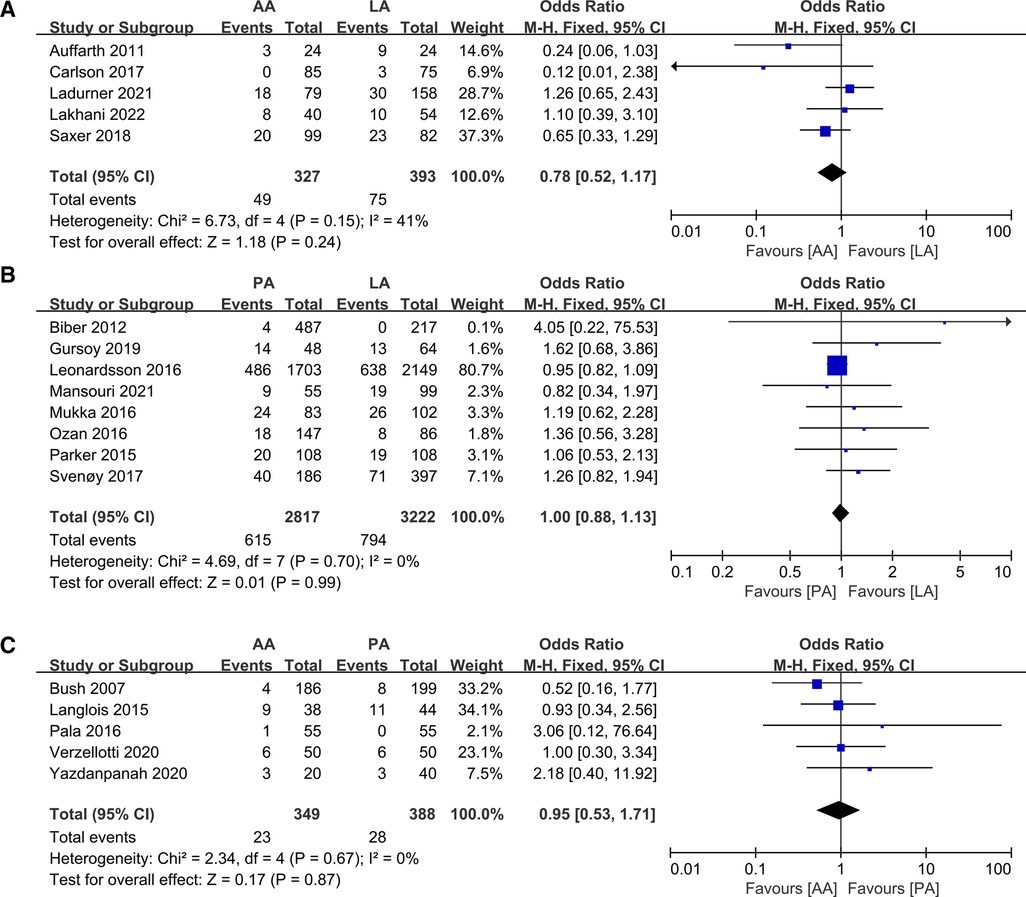
Figure 10. Forest plot comparison of mortality. (A) Anterior approach and lateral approach, (B) Posterior approach and lateral approach, (C) Posterior approach and anterior approach.
Clinical outcomes
For perioperative pain results, researchers have applied several kinds of scores, including the VAS score (5, 18, 20, 31, 34, 37), a modified Charnley pain score (19), pain numeric rating scale (PNRS) (36), and mean pain postop (NRS) (39) but none of the data could be analyzed in aggregate. In both the AA and PA studies, Pala and Neyisci concluded that the AA group was less painful and that the difference was statistically significant, but Langlois concluded that there was no difference between the groups. Renken (18) et al. and Saxer (5) et al. found that patients in the AA group suffered less pain at all time points than those in the LA group, which may be related to less surgical trauma in the AA group. The difference was that Renken derived a significant difference in pain late (16 days, 40 days), while Saxer considered it to be early (5 days). More importantly, Auffarth (20) arrived at the opposite idea from the two formers.
Hip function was evaluated with the Harris Hip Score (HHS) (20, 36, 45) and the Western Ontario and McMaster Universities Arthritis (WOMAC) (36) index, the University of California, Los Angeles (UCLA) (38) hip scoring assessment, but the number of available databases is insufficient and a meta-analysis of these results is also not feasible. In conclusion, no statistically significant differences were found in all studies, regardless of the functional scores. Lakhani (32) and Sayed-Noor (40) reported the problem of Trendelenburg gait after surgery, Lakhani found no cases of Trendelenburg gait in the DAA group after surgery, while three cases of Trendelenburg gait in the DLA group. Sayed-Noor et al. saw that Trendelenburg sign occurred in 37.5% (9/24) of patients after DL approach and 4% (1/24) of patients after PL approach, further analyzing the DL approach as a factor contributing to Trendelenburg gait.
Discussion
The different approaches of hemiarthroplasty for femoral neck fractures are used routinely in clinical situations, but their risks and benefits have been controversial. This review is aimed at providing objective theoretical evidence for clinical diagnosis and treatment through meta-analysis of their data. The outcomes revealed that the time of hospitalization was shorter in AA than in LA, and regarding complications, PA had a significantly higher subluxation hazard in comparison to LA and AA, and PA increased the incidence of reoperation than AA, all of which were statistically significant, with no significant differences seen in the remaining outcomes in all aspects that allowed for data analysis.
Heavy heterogeneity existed in clinical data regarding operative time, intraoperative blood loss, and length of hospital stay (I2 > 75%), and we used a random-effects model analysis and discovered that AA had a longer length of stay than LA, which may be relevant to the surgical approach.
The AA operation is mostly carried out using the minimally invasive direct anterior approach (DAA), which reduces postoperative pain and allows for faster recovery by preserving the muscles during the approach to the hip joint (46–48), with minimal postoperative impact on hip mobility and daily life (39). Nevertheless, many reports have found a prolonged duration of surgery, although we did not analyze a significant difference (20, 32).
Dislocation was the most disparate outcome in the meta-analysis and an essential indicator for evaluating the results of the surgery. The PA is at greater risk of dislocation than the other two approaches and may be related to surgical incision of soft tissue anatomy such as the capsule, short external rotators, and piriformis (49).There may also be a relationship with patient cognitive status and sex, with some findings of higher dislocation rates in women and patients with cognitive impairment (29).
Patient reoperation was also statistically significant, and one of the major factors was dislocation of the hip on the patient's side of surgery. Some of the surgeries involved repair of the short external rotators with the posterior capsule to reduce the incidence of dislocation, but the efficacy is conflicting (29, 50). This is a shortcoming of PA and may lead the operator to prefer other modalities when choosing a surgical approach.
We did not undertake a meaningful statistical analysis to demonstrate which approach had less postoperative pain (5, 18, 37, 39), but the literature screened generally concluded that AA had better outcomes than PA and LA, which was related to surgical trauma. However, differently, Renken (18) et al. yielded a significant difference in pain between groups at the late stages (16 days, 40 days), whereas Saxer (5) found that the difference occurred at the early stage (5 days).
We can see that PA has more risk of dislocation and reoperation rate, which may be the primary factor for clinicians to avoid. Less of the length of hospitalization is beneficial for AA to be promoted in clinical practice, in addition, whether it can reduce postoperative pain, need to be validated and supported by more clinical trial data in the future.
Limitations
Although there are more data analyzed in this paper, the randomized controlled trials included in it are only 5, the rest are cohort studies, the quality of evidence is not high level. The double-blind control of these surgical randomization groups and investigators, patients, is comparatively weak, and the likelihood of breaching the blind is higher. Second, different types and manufacturers of prostheses were used for the surgery, and according to the patients' demand, cemented and noncemented prostheses were also employed, all of which had an impact on the experimental results, whereas we were unable to perform a statistical analysis. Third, we only searched common databases and failed to provide comprehensive coverage of published articles, and there were subjective influences of researchers in the selection process of articles, which may lead to the omission of any literature. Furthermore, the included literature reported data for the three approaches, and the number of some indicators was too limited for analysis. For common postoperative hip scores and pain, various scoring criteria used in different studies failed to be analyzed effectively, which is pivotal to the evaluation of the trial, and more literature reporting and unification of routine scoring scales would be more helpful for the study in the future.
Conclusion
Generally, the risk of dislocation was higher in PA than in the other two approaches, the odds of complications requiring reoperation were also higher in PA than in LA, and PA was not found to be superior to the other two approaches in other aspects. In terms of hospitalization time, AA was shorter than LA, and there was no difference between both in operation time, intraoperative blood loss, all sorts of complications, postoperative pain, and hip function. At present, AA is seemingly more successful, but its literature is limited and has higher heterogeneity. More qualitative literature and postoperative data reported in the future will facilitate the final determination of which approach is superior. The ultimate choice of the operation mode should be considered by the surgical operators based on a combination of factors.
Author contributions
LS: collected the data and completed the article. WH and DS: performed the data analysis. WF: made the graphs and tables. JJ and LJ: provided the topic selection and article review. All authors contributed to the article and approved the submitted version.
Funding
Basic and Clinical Cooperative Research Promotion Plan of Anhui Medical University (grant no. 2020xkjT040); Clinical Research cultivation Program of the Second Affiliated Hospital of Anhui Medical University (grant no. 2020LCZD20).
Acknowledgments
Thanks to LJ and JJ for their helpful suggestions on the article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. (2018) 49(8):1458–60. doi: 10.1016/j.injury.2018.04.015
2. Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. (1992) 2(6):285–9. doi: 10.1007/bf01623184
3. Cha YH, Yoo JI, Kim JT, Park CH, Ahn YS, Choy WS, et al. Dual mobility total hip arthroplasty in the treatment of femoral neck fractures. Bone Joint J. (2020) 102(11):1457–66. doi: 10.1302/0301-620x.102b11.Bjj-2020-0610.R2
4. Li X, Luo J. Hemiarthroplasty compared to total hip arthroplasty for the treatment of femoral neck fractures: a systematic review and meta-analysis. J Orthop Surg Res. (2021) 16(1):172. doi: 10.1186/s13018-020-02186-4
5. Saxer F, Studer P, Jakob M, Suhm N, Rosenthal R, Dell-Kuster S, et al. Minimally invasive anterior muscle-sparing versus a transgluteal approach for hemiarthroplasty in femoral neck fractures-a prospective randomised controlled trial including 190 elderly patients. BMC Geriatr. (2018) 18(1):222. doi: 10.1186/s12877-018-0898-9
6. Chang JD, Kim IS, Lee SS, Yoo JH, Hwang JH. Unstable intertrochanteric versus displaced femoral neck fractures treated with cementless bipolar hemiarthroplasty in elderly patients; a comparison of 80 matched patients. Orthop Traumatol Surg Res. (2016) 102(6):695–9. doi: 10.1016/j.otsr.2016.04.007
7. Kain MS, Willier D 3rd. Hemiarthroplasty through a direct anterior approach for femoral neck fractures. J Orthop Trauma. (2020) 34:S25–s6. doi: 10.1097/bot.0000000000001820
8. Skowronek P, Wojciechowski A, Wypniewski K, Sibiński M, Polguj M, Maksymiuk-Kłos A, et al. Time efficiency of direct anterior hip arthroplasty compared to postero-lateral approach in elderly patients. Arch Med Sci. (2021) 17(1):106–12. doi: 10.5114/aoms/86185
9. Nakamura T, Yamakawa T, Hori J, Goto H, Nakagawa A, Takatsu T, et al. Conjoined tendon preserving posterior approach in hemiarthroplasty for femoral neck fractures: a prospective multicenter clinical study of 322 patients. J Orthop Surg. (2021) 29(3):23094990211063963. doi: 10.1177/23094990211063963
10. Ladurner A, Schöfl T, Calek AK, Zdravkovic V, Giesinger K. Direct anterior approach improves in-hospital mobility following hemiarthroplasty for femoral neck fracture treatment. Arch Orthop Trauma Surg. (2021):1–10. doi: 10.1007/s00402-021-04087-5
11. van der Sijp MPL, van Delft D, Krijnen P, Niggebrugge AHP, Schipper IB. Surgical approaches and hemiarthroplasty outcomes for femoral neck fractures: a meta-analysis. J Arthroplasty. (2018) 33(5):1617–27.e9. doi: 10.1016/j.arth.2017.12.029
12. Kunkel ST, Sabatino MJ, Kang R, Jevsevar DS, Moschetti WE. A systematic review and meta-analysis of the direct anterior approach for hemiarthroplasty for femoral neck fracture. Eur J Orthop Surg Traumatol. (2018) 28(2):217–32. doi: 10.1007/s00590-017-2033-6
13. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343:d5928. doi: 10.1136/bmj.d5928
14. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. (2014) 14(1):1–13. doi: 10.1186/1471-2288-14-135
15. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) 5(1):13. doi: 10.1186/1471-2288-5-13
16. Bland M. Estimating mean and standard deviation from the sample size, three quartiles, minimum, and maximum. Int J Stat Med Res. (2015) 4(1):57–64. doi: 10.6000/1929-6029.2015.04.01.6
17. Verzellotti S, Candrian C, Molina M, Filardo G, Alberio R, Grassi FA. Direct anterior versus posterolateral approach for bipolar hip hemiarthroplasty in femoral neck fractures: a prospective randomised study. Hip Int. (2020) 30(6):810–7. doi: 10.1177/1120700019872117
18. Renken F, Renken S, Paech A, Wenzl M, Unger A, Schulz AP. Early functional results after hemiarthroplasty for femoral neck fracture: a randomized comparison between a minimal invasive and a conventional approach. BMC Musculoskelet Disord. (2012) 13:141. doi: 10.1186/1471-2474-13-141
19. Parker MJ. Lateral versus posterior approach for insertion of hemiarthroplasties for hip fractures: a randomised trial of 216 patients. Injury. (2015) 46(6):1023–7. doi: 10.1016/j.injury.2015.02.020
20. Auffarth A, Resch H, Lederer S, Karpik S, Hitzl W, Bogner R, et al. Does the choice of approach for hip hemiarthroplasty in geriatric patients significantly influence early postoperative outcomes? A randomized-controlled trial comparing the modified smith-petersen and hardinge approaches. J Trauma. (2011) 70(5):1257–62. doi: 10.1097/TA.0b013e3181eded53
21. Abram SG, Murray JB. Outcomes of 807 thompson hip hemiarthroplasty procedures and the effect of surgical approach on dislocation rates. Injury. (2015) 46(6):1013–7. doi: 10.1016/j.injury.2014.12.016
22. Baba T, Shitoto K, Kaneko K. Bipolar hemiarthroplasty for femoral neck fracture using the direct anterior approach. World J Orthop. (2013) 4(2):85–9. doi: 10.5312/wjo.v4.i2.85
23. Biber R, Brem M, Singler K, Moellers M, Sieber C, Bail HJ. Dorsal versus transgluteal approach for hip hemiarthroplasty: an analysis of early complications in seven hundred and four consecutive cases. Int Orthop. (2012) 36(11):2219–23. doi: 10.1007/s00264-012-1624-4
24. Bűcs G, Dandé Á, Patczai B, Sebestyén A, Almási R, Nöt LG, et al. Bipolar hemiarthroplasty for the treatment of femoral neck fractures with minimally invasive anterior approach in elderly. Injury. (2021) 52:S37–s43. doi: 10.1016/j.injury.2020.02.053
25. Bush JB, Wilson MR. Dislocation after hip hemiarthroplasty: anterior versus posterior capsular approach. Orthopedics. (2007) 30(2):138–44. doi: 10.3928/01477447-20070201-05
26. Carlson VR, Ong AC, Orozco FR, Lutz RW, Duque AF, Post ZD. The direct anterior approach does not increase return to function following hemiarthroplasty for femoral neck fracture. Orthopedics. (2017) 40(6):e1055–e61. doi: 10.3928/01477447-20170925-08
27. de Vries EN, Gardenbroek TJ, Ammerlaan H, Steenstra F, Vervest A, Hogervorst M, et al. The optimal approach in hip hemiarthroplasty: a cohort of 1,009 patients. Eur J Orthop Surg Traumatol. (2020) 30(4):569–73. doi: 10.1007/s00590-019-02610-4
28. Enocson A, Tidermark J, Tornkvist H, Lapidus LJ. Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop. (2008) 79(2):211–7. doi: 10.1080/17453670710014996
29. Gursoy S, Simsek ME, Akkaya M, Dogan M, Bozkurt M. Transtrochanteric approach can provide better postoperative care and lower complication rate in the treatment of hip fractures. Clin Interv Aging. (2019) 14:137–43. doi: 10.2147/cia.S194880
30. Hongisto MT, Nuotio MS, Luukkaala T, Väistö O, Pihlajamäki HK. Lateral and posterior approaches in hemiarthroplasty. Scand J Surg. (2018) 107(3):260–8. doi: 10.1177/1457496917748226
31. Kristensen TB, Vinje T, Havelin LI, Engesæter LB, Gjertsen JE. Posterior approach compared to direct lateral approach resulted in better patient-reported outcome after hemiarthroplasty for femoral neck fracture. Acta Orthop. (2017) 88(1):29–34. doi: 10.1080/17453674.2016.1250480
32. Lakhani K, Mimendia I, Porcel JA, Martín-Domínguez LA, Guerra-Farfán E, Barro V. Direct anterior approach provides better functional outcomes when compared to direct lateral approach in hip hemiarthroplasty following femoral neck fracture. Eur J Orthop Surg Traumatol. (2022) 32(1):137–43. doi: 10.1007/s00590-021-02941-1
33. Langlois J, Delambre J, Klouche S, Faivre B, Hardy P. Direct anterior hueter approach is a safe and effective approach to perform a bipolar hemiarthroplasty for femoral neck fracture: outcome in 82 patients. Acta Orthop. (2015) 86(3):358–62. doi: 10.3109/17453674.2014.1002987
34. Leonardsson O, Rolfson O, Rogmark C. The surgical approach for hemiarthroplasty does not influence patient-reported outcome: a national survey of 2118 patients with one-year follow-up. Bone Joint J. (2016) 98(4):542–7. doi: 10.1302/0301-620x.98b4.36626
35. Mansouri-Tehrani MM, Yavari P, Pakdaman M, Eslami S, Nourian SMA. Comparison of surgical complications following hip hemiarthroplasty between the posterolateral and lateral approaches. Int J Burns Trauma. (2021) 11(5):406–11.34858721
36. Mukka S, Mahmood S, Kadum B, Sköldenberg O, Sayed-Noor A. Direct lateral vs posterolateral approach to hemiarthroplasty for femoral neck fractures. Orthop Traumatol Surg Res. (2016) 102(8):1049–54. doi: 10.1016/j.otsr.2016.08.017
37. Neyisci C, Erdem Y, Bilekli AB, Bek D. Direct anterior approach versus posterolateral approach for hemiarthroplasty in the treatment of displaced femoral neck fractures in geriatric patients. Med Sci Monit. (2020) 26:e919993. doi: 10.12659/msm.919993
38. Ozan F, Oncel ES, Koyuncu S, Gurbuz K, Dogar F, Vatansever F, et al. Effects of hardinge versus moore approach on postoperative outcomes in elderly patients with hip fracture. Int J Clin Exp Med. (2016) 9(2):4425–31.
39. Pala E, Trono M, Bitonti A, Lucidi G. Hip hemiarthroplasty for femur neck fractures: minimally invasive direct anterior approach versus postero-lateral approach. Eur J Orthop Surg Traumatol. (2016) 26(4):423–7. doi: 10.1007/s00590-016-1767-x
40. Sayed-Noor AS, Hanas A, Sköldenberg OG, Mukka SS. Abductor muscle function and trochanteric tenderness after hemiarthroplasty for femoral neck fracture. J Orthop Trauma. (2016) 30(6):e194–e200. doi: 10.1097/bot.0000000000000532
41. Sierra RJ, Schleck CD, Cabanela ME. Dislocation of bipolar hemiarthroplasty: rate, contributing factors, and outcome. Clin Orthop Relat Res. (2006) 442:230–8. doi: 10.1097/01.blo.0000183741.96610.c3
42. Svenøy S, Westberg M, Figved W, Valland H, Brun OC, Wangen H, et al. Posterior versus lateral approach for hemiarthroplasty after femoral neck fracture: early complications in a prospective cohort of 583 patients. Injury. (2017) 48(7):1565–9. doi: 10.1016/j.injury.2017.03.024
43. Tsailas PG, Argyrou C, Valavanis A. Management of femoral neck fractures with the almis approach in elderly patients: outcomes compared to posterior approach. Injury. (2021) 52(12):3666–72. doi: 10.1016/j.injury.2021.06.036
44. Tsukada S, Wakui M. Minimally invasive intermuscular approach does not improve outcomes in bipolar hemiarthroplasty for femoral neck fracture. J Orthop Sci. (2010) 15(6):753–7. doi: 10.1007/s00776-010-1541-6
45. Yazdanpanah P, Mohammadi H. Short-term complications of hip bipolar hemiarthroplasty with anterior approach in patients with femoral neck fracture admitted to the emergency department of yasuj shahid beheshti hospital in 2016–2018. Rev Latinoam. (2020) 14(2):150–3. doi: 10.5281/zenodo.4074702
46. Alecci V, Valente M, Crucil M, Minerva M, Pellegrino CM, Sabbadini DD. Comparison of primary total hip replacements performed with a direct anterior approach versus the standard lateral approach: perioperative findings. J Orthop Traumatol. (2011) 12(3):123–9. doi: 10.1007/s10195-011-0144-0
47. Zawadsky MW, Paulus MC, Murray PJ, Johansen MA. Early outcome comparison between the direct anterior approach and the mini-incision posterior approach for primary total hip arthroplasty: 150 consecutive cases. J Arthroplasty. (2014) 29(6):1256–60. doi: 10.1016/j.arth.2013.11.013
48. Moskal JT, Capps SG, Scanelli JA. Anterior muscle sparing approach for total hip arthroplasty. World J Orthop. (2013) 4(1):12–8. doi: 10.5312/wjo.v4.i1.12
49. Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ. Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res. (2006) 447:34–8. doi: 10.1097/01.blo.0000218746.84494.df
Keywords: hemiarthroplasty (HA), anterior approach (AA), lateral approach (LA), posterior approach (PA), dislocation, meta-analysis
Citation: Shuai L, Huiwen W, Shihao D, Fangyuan W, Juehua J and Jun L (2023) A comparison of different surgical approaches to hemiarthroplasty for the femoral neck fractures: A meta-analysis. Front. Surg. 9:1049534. doi: 10.3389/fsurg.2022.1049534
Received: 20 September 2022; Accepted: 2 November 2022;
Published: 6 January 2023.
Edited by:
Paphon Sa-ngasoongsong, Mahidol University, ThailandReviewed by:
Osama Farouk, Assiut University Hospital, EgyptJian Wang, Southern Medical University, China
Hanbin Ouyang, Affiliated Hospital of Guangdong Medical College Hospital, China
© 2023 Shuai, Huiwen, Shihao, Fangyuan, Juehua and Jun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Juehua ampoaHVAc2luYS5jb20= Li Jun ZWZ5bGlqdW5wYXBlckAxNjMuY29t
†These authors share last authorship
‡ORCID Liang Shuai orcid.org/0000-0002-1397-0001 Li Jun orcid.org/0000-0001-6383-6065
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Liang Shuai1,2,‡
Liang Shuai1,2,‡ Jing Juehua
Jing Juehua Li Jun
Li Jun