
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 06 January 2023
Sec. Pediatric Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1040487
This article is part of the Research Topic Advances on Clinical and Basic Translational Research of Neonatal Babies with Surgical Issues View all 27 articles
Background: Testicular torsion (TT) is a common urological emergency posing serious health problem in children. Prompt diagnosis and treatment of TT are very important for children to protect the affected testis. The aim of this study was to evaluate the historical features, physical examination findings, laboratory tests, and ultrasound examinations in children with TT, as well as to identify the predictors of testicular salvage in children.
Materials and methods: We conducted a retrospective record of clinical findings, laboratory data, ultrasound findings, operating results, and the results of follow-up in hospitalized children with TT from November 2004 to December 2021. A multivariable logistic regression model was used to identify predictors of testicular salvage.
Results: A total 102 hospitalized children who presented with TT were included. Patients were aged from 1 month to 16 years, with a median age of 7.71 years. TT is significantly more common in the winter. Of these patients, 77 torsions were left-sided, 24 were on the right side, and only 1 was on bilateral sides. Meanwhile, we detected that 88 children suffering from TT had intravaginal torsion of the spermatic cord, and the rest were outside. Anticlockwise torsion was found in 65 cases (63.73%) and clockwise torsion in 37 (36.27%). As a result, 60 underwent orchidectomy, while 42 had a scrotal exploration with fixation of the testis. Multivariate analysis showed that cause of TT, time to intervention, white blood cell (WBC), and mean platelet volume (MPV) were correlated with the risk of a surgical outcome.
Conclusion: Only a small proportion of TT children received timely surgical management. Testicular salvage can be predicted by cause of TT, time to intervention, WBC, and MPV. Early scrotal exploration based on careful physical examination decreases the risk of misdiagnosis of spermatic cord torsion. A certain percentage of children with TT presenting with scrotal trauma or epididymo-orchitis should have their testicles checked to make sure that they do not have torsion, especially those who visit in the cold season.
Testicular torsion (TT) is one of the most common diseases encountered in a pediatric hospital emergency department, with its incidence rate being about 1 in 4,000 males under the age of 25 (1). It is often caused by obstruction of testicular blood flow through a twisting of the longitudinal axis of the spermatic cord. TT is a time-dependent urgent event (2). Active management can relieve the suffering of patients, protect the testicular function, and improve male fertility (3, 4). It is well known that the two main determinants for testicular salvage include the degree of cord twisting and the timing of patient presentation after symptom onset. Thus, prompt diagnosis and treatment of TT should be performed immediately as long-term torsion may result in pain, testicular atrophy, or even totally loss of the affected testis.
Children who are diagnosed with TT usually have a loss of the cremasteric reflex on the affected side and abnormal testicle direction. The most common sign and symptom of torsion is sudden onset, severe, and unrelenting scrotal or/and inguinal pain (5). Some children may suffer from fever, nausea, and vomiting (6). However, it is often difficult to distinguish TT from other causes of acute pediatric scrotum syndrome such as epididymo-orchitis, infected hydrocele, and torsion of the appendix of testis. Up to 15% of children presenting with acute scrotum syndrome are diagnosed with torsion (7). Even an experienced pediatrician cannot make a clear distinction between TT and epididymo-orchitis with full assurance. Thus, physical examination findings are important for the diagnosis of TT. In addition, color Doppler ultrasonography of the testis is widely used for fast examination in the diagnosis of TT. In general, the torsed testicle may be irreversibly lost if the symptom duration remains over 6 h after initial pain (8). Delayed surgical management of TT is often made owing to lack of experience on the identification and diagnosis of TT.
The aim of this retrospective study is to summarize the clinical manifestations, physical examinations, auxiliary examinations, and surgical outcomes of TT in order to improve the diagnosis and treatment, as well as to explore the risk factors for predicting the outcomes of pediatric patients diagnosed with TT at the children's hospital in China from November 2004 to December 2021.
Consent was not required from the Ethics Committee because of the retrospective nature of this study. Written informed consent was routinely obtained from each surgical patient or the legal guardian/next of kin for minors.
A retrospective analysis of the medical records on TT from November 2004 to December 2021 was conducted at our institution. Only cases confirmed by scrotal exploration were consecutively included in this study. Patients whose parents refused surgical exploration were excluded from this study in addition to negative scrotal exploration, neonatal torsion, or testicular appendix torsion. We extracted clinical data including age, duration of symptoms onset, birth weight, gestational age of mother, mode of delivery, feeding pattern, concomitant diagnose, ultrasound characteristics, laboratory testing, and direction and degree of spermatic cord twisting. Meanwhile, some children also had other concomitant diagnoses, namely, contained hydrocele, cryptorchidism, inguinal hernia, or testicular microlithiasis. Children diagnosed with TT underwent orchiectomy and/or surgical detorsion. The contralateral testis was routinely fixed in the same fashion unless parents refused to testicular fixation.
The patients were followed up at 1, 3, and 6 months postoperatively, and then examined once a year in the clinic. In addition, color Doppler ultrasound was widely used as a helpful tool for follow-up visits. We collected the number of testicular atrophies based on ultrasound after orchiopexy (defined as a >20% difference in volume compared to the contralateral testis).
First, the scrotal skin and tunica vaginalis of the affected side were incised under general anesthesia. Second, a small incision was made in the tunica albuginea to check the blood supply, and then the affected testis was covered with a piece of moistened gauze with warm saline for 10–30 min. Third, after a moment, the affected testis was rechecked for potential salvageability. Generally, orchidopexy was performed if the testicular blood flow was restored. Otherwise, the nonviable testis was removed, and then fixation of contralateral testis was performed. In practice, an in-depth communication with parents was made to decide which kind of surgery (orchidopexy or orchiectomy) is suitable for their children in the face of coagulative necrosis of the testicular parenchyma. In Meanwhile, parents also decided whether to fix the contralateral testis.
SPSS version 19.0 (SPSS Inc., Chicago, IL, United States) was applied for statistical analysis. Categorical variables were presented as ratios (%) and continuous variables were presented by mean ± standard deviation (SD). All continuous variables were tested for normality using the Shapiro–Wilk test. For normal distributed data, Student's t test was used. For non-normal data distribution, the Kruskal–Wallis test was applied instead. Comparisons were conducted by χ2 test or Fisher's exact test for dichotomous outcomes and unordered multiple outcomes, and by Kruskal–Wallis test for ordered multiple outcomes. A P-value less than 0.05 was considered statistically significant.
A retrospective record of 102 patients who were diagnosed with TT to our institution was made after surgery from November 2004 to December 2021. The primary characteristics of the patients are presented in Table 1. The age of the patients enrolled ranged from 1 month to 16 years, wherein TT mainly occurred in the first year of life and between the ages of 13 and 16 years. Most patients had a history of breast feeding and normal birth weight. The duration of pain or symptoms was 1 h to 15 days. The common causes of TT included scrotal trauma and epididymo-orchitis. However, most causes were still unknown. Thirty patients had concomitant diagnosis, namely, cryptorchidism, hydrocele, inguinal hernia, and testicular microlithiasis. Acute scrotal pain was the most common finding in the TT patients, followed by lower abdominal or inguinal pain. Moreover, we also found that TT often occurs in winter compared to other seasons (Table 1).
These boys underwent surgery promptly after hospitalization. The common complications included bleeding and scrotal edema after operation. No serious complication was detected. Operative findings and surgical outcomes in patients with TT are shown in Table 2. From Table 2, the range of twisting in the torsion could be identified as 90°–1,080°. Of these patients, 77 (75.49%) torsions were left-sided, 24 were on the right side, and only 1 was bilateral sides. Meanwhile, we detected that 88 children suffering from TT had intravaginal torsion of the spermatic cord, and the rest were outside. Anticlockwise torsion was found in 65 cases (63.73%) and clockwise torsion in 37 (36.27%). As a result, 60 underwent orchidectomy, while 42 had a scrotal exploration with fixation of the testis. In addition, the contralateral testis was fixed in 33 of 102 (32.35%) cases according to the agreement from their guardians. Of the cases of testicular salvage, two patients developed subsequent testicular atrophy after follow-up of half a year.
To determine the factors influencing the surgical procedures, patients were classified into two groups depending on whether they underwent orchidopexy or orchiectomy. On univariable analysis, we found that those in the orchidopexy group tended to have significantly lower degrees of twisting (P = 0.002) and shorter duration of symptoms (P = 0.001) when compared to their viable counterparts (Table 3). In addition, there was a statistical difference in the group of TT causes (P = 0.003). There was no statistical difference in other variables between the two groups (P > 0.05).
There were significant differences between orchidopexy and orchiectomy in terms of white blood cell (WBC) and mean platelet volume (MPV). However, there was no statistically significant difference in other hematologic parameters between the two groups (Table 4). Likewise, a multivariate analysis of the two groups revealed that cause of TT, time to intervention, WBC, and MPV were correlated with the risk of a nonsalvageable testis (Table 5).
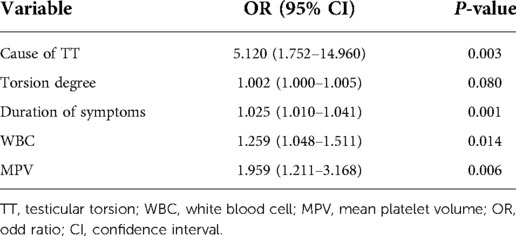
Table 5. Results of multivariable analysis between patients underwent orchidopexy and orchiectomy by logistic regression analysis.
TT is a surgical emergency and may affect testicular function and male fertility if not treated timely. Approximately 30% children with acute scrotum had delayed surgical management of TT because they were not first treated in a tertiary hospital. Patients transferred from primary and secondary healthcare units were more likely to delay management owing to the lack of experience on the identification and diagnosis of TT. Thus, it is important to continuously promote public awareness of TT, and improve pediatrician ability of diagnosis and therapy of TT from primary and secondary healthcare units.
Acute severe scrotal pain is a symptom that can be identified in clinical presentation. Other common signs and symptoms of torsion, as well as other causes of acute pediatric scrotum syndrome, include sudden abdominal or inguinal pain, nausea, and vomiting. Not all TT cases have acute severe scrotal pain. Actually, we often need to make an accurate differential diagnosis of an undescended TT from acute abdomen or incarcerated hernia through proper abdominal and inguinal examination, especially for defective children or infants. It may be difficult to distinguish from other causes of acute pediatric scrotum syndrome such as epididymo-orchitis, infected hydrocele, and torsion of the appendix of testis. Surgery is the primary treatment after suspicion of TT. The duration of pain or symptom was a critical factor of surgical selection (9). However, the definition of delayed surgery was still not well established. To date, the “golden window of opportunity” to testicular salvage after symptom onset is suggested to be 0–6 h, as not intervening within this time decreases function and increases the rate of orchiectomy (10, 11). If treated within 6 h from the onset of symptoms, 90%–100% affected testicles will be saved. If symptoms last beyond 12 h, salvage rates will decrease to 50%. The incidence of testicular salvage is even less than 10% over 24 h (12).
Previous studies have always have explored the risk factors of TT and found that age is an important risk factor. TT can occur at any age but usually occurs in young males, especially in the first year of life and around puberty (13, 14). Children under the age of 6 could not express themselves and judge the severity of the scrotal pain, resulting in delayed management of TT (15). There was a similar age distribution in our study, with peaks of incidence during age less than 1 (18.63%, 19/102) and around puberty (39.22%, 40/102). In addition, environmental temperature has been associated with variations in the incidence of TT. Cremaster muscle spasm in response to cold weather has been implied in the occurrence of TT. Cold weather, as well as the resultant cremasteric hyperactivity, can be risk factors for torsion in individuals with unfavorable anatomy including testicles with a greater horizontal axis (16). It has been reported that over 75% of TT cases were found more commonly in cold season with a low ambient temperature below 15°C (17). Furthermore, Ekici et al. (18) reported that approximately 46% of TT cases were detected in the winter months in their study. This is similar to the rate found in our present study. More TT cases were detected during winter (36.25%) in the present study. Scrotal trauma also may result in TT by an abrupt vigorous contraction of the cremaster muscle, accounting for 4%–8% of all TT cases (19, 20). Traumatic torsion was often observed in patients with risk factors for TT such as bell clapper deformity and horizontal lie of the testes (19). These patients required a high index of suspicion of TT, and then an urgent ultrasound scan was performed. Moreover, about 5% of patients who presented with torsion suffered from cryptorchidism, which may be explained by incorrect spasm or contraction of cremasteric muscle (21, 22).
Debate always exists regarding contralateral testicle fixation, arguing that the low risk of contralateral torsion outweighs the risk of complications from orchidopexy (23). The exact risk of contralateral torsion is still unknown. However, a previous study found that the contralateral testis often had some predisposing factors in 78% of pubertal TT cases, such as the bell clapper deformity and horizontal lie of the testes (24). Furthermore, some bilateral torsion may present with unilateral signs (25). In our study, there was only one contralateral torsion 1 year after orchiectomy. Given these findings, the contralateral testicle should undergo fixation to reduce the risk of torsion.
Though we collected the medical records of TT cases from the past decade, some limitations still existed. First, our study design was a retrospective study and restricted the accuracy of results. Second, only patients with TT in our pediatric center were included, which could not completely represent the general condition. Finally, some potential or undiscovered factors may affect the ultimate results, such as family history of TT, medical insurance, and guardians’ work. Therefore, a prospective, well-designed, and large-scale study should be performed.
Only a small proportion of TT children received timely surgical management. Testicular salvage can be predicted by cause of TT, time to intervention, WBC, and MPV. Early scrotal exploration based on careful physical examination decreases the risk of misdiagnosis of spermatic cord torsion. A certain percentage of children with TT presenting with scrotal trauma or epididymo-orchitis should have their testicles checked to make sure that they do not have torsion, especially those who visit the in cold season.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
KZ and YZ contributed to study design and data collection. KZ contributed to data analysis and literature analysis. KZ and MC contributed to preparation of manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lemini R, Guanà R, Tommasoni N, Mussa A, Di Rosa G, Schleef J. Predictivity of clinical findings and Doppler ultrasound in pediatric acute scrotum. Urol J. (2016) 13:2779–83. doi: 10.22037/uj.v13i4.3359
2. Greear GM, Romano MF, Katz MH, Munarriz R, Rague JT. Testicular torsion: epidemiological risk factors for orchiectomy in pediatric and adult patients. Int J Impot Res. (2020) 33:184–90. doi: 10.1038/s41443-020-0331-8
3. Zhao L, Lautz T, Meeks J, Maizels M. Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward improving the quality of care. J Urol. (2011) 186:2009–13. doi: 10.1016/j.juro.2011.07.024
4. Aggarwal D, Parmar K, Sharma AP, Tyagi S, Kumar S, Singh SK, et al. Long-term impact of testicular torsion and its salvage on semen parameters and gonadal function. Indian J Urol. (2022) 38:135–9. doi: 10.4103/iju.iju_328_21
5. Ann Kroger-Jarvis M, Gillespie GL. Presentation of testicular torsion in the emergency department. Adv Emerg Nurs J. (2016) 38:295–9. doi: 10.1097/TME.0000000000000119
6. Srinivasan A, Cinman N, Feber KM, Gitlin J, Palmer LS. History and physical examination findings predictive of testicular torsion: an attempt to promote clinical diagnosis by house staff. J Pediatr Urol. (2011) 7:470–4. doi: 10.1016/j.jpurol.2010.12.010
7. Burgher SW. Acute scrotal pain. Emerg Med Clin N Am. (1998) 16:781–809. doi: 10.1016/S0733-8627(05)70033-X
8. Mäkelä E, Lahdes-Vasama T, Rajakorpi H, Wikström S. A 19-year review of paediatric patients with acute scrotum. Scand J Surg. (2007) 96:62–6. doi: 10.1177/145749690709600112
9. Ramachandra P, Palazzi KL, Holmes NM, Marietti S. Factors influencing rate of testicular salvage in acute testicular torsion at a tertiary pediatric center. West J Emerg Med. (2015) 16:190–4. doi: 10.5811/westjem.2014.11.22495
10. Morin OA, Carr MG, Holcombe JM, Bhattacharya SD. Optimal predictor of gonadal viability in testicular torsion: time to treat versus duration of symptoms. J Surg Res. (2019) 244:574–8. doi: 10.1016/j.jss.2019.06.033
11. Anderson M, Dunn J, Lipshultz L, Coburn M. Semen quality and endocrine parameters after acute testicular torsion. J Urol. (1992) 147:1545–50. doi: 10.1016/S0022-5347(17)37622-X
12. Nason GJ, Tareen F, McLoughlin D, McDowell D, Cianci F, Mortell A. Scrotal exploration for acute scrotal pain: a 10-year experience in two tertiary referral paediatric units. Scand J Urol. (2013) 47:418–22. doi: 10.3109/00365599.2012.752403
13. Beni-Israel T, Goldman M, Bar Chaim S, Kozer E. Clinical predictors for testicular torsion as seen in the pediatric ED. Am J Emerg Med. (2010) 28(7):786–9. doi: 10.1016/j.ajem.2009.03.025
14. Pogorelić Z, Mrklić I, Jurić I. Do not forget to include testicular torsion in differential diagnosis of lower acute abdominal pain in young males. J Pediatr Urol. (2013) 9:1161–5. doi: 10.1016/j.jpurol.2013.04.018
15. Yu C, Zhao J, Lu J, Wei Y, Jiang L, Zhao T, et al. Demographic, clinical, and socioeconomic factors associated with delayed diagnosis and management of pediatric testicular torsion in west China: a retrospective study of 301 cases in a single tertiary children's hospital. BMC Pediatr. (2021) 21:553. doi: 10.1186/s12887-021-03001-7
16. Shukla RB, Kelly DG, Daly L, Guiney EJ. Association of cold weather with testicular torsion. Br Med J. (1982) 285:1459–60. doi: 10.1136/bmj.285.6353.1459
17. Srinivasan AK, Freyle J, Gitlin JS, Palmer LS. Climatic conditions and the risk of testicular torsion in adolescent males. J Urol. (2007) 178:2585–8. doi: 10.1016/j.juro.2007.08.049
18. Ekici M, Ozgur BC, Senturk AB, Nalbant I. Relationship of low temperature with testicular torsion. J Coll Physicians Surg Pak. (2018) 28:378–80. doi: 10.29271/jcpsp.2018.05.378
19. Seng YJ, Moissinac K. Trauma induced testicular torsion: a reminder for the unwary. J Accid Emerg Med. (2000) 17:381–2. doi: 10.1136/emj.17.5.381
20. Zhong H, Bi Y. Pediatric trauma-induced testicular torsion: a surgical emergency. Urol Int. (2021) 105:221–4. doi: 10.1159/000511747
21. Komarowska MD, Pawelczyk A, Matuszczak E, Dębek W, Hermanowicz A. Is testicular torsion a real problem in pediatric patients with cryptorchidism? Front Pediatr. (2021) 8:575741. doi: 10.3389/fped.2020.575741
22. Naouar S, Braiek S, El Kamel R. Testicular torsion in undescended testis: a persistent challenge. Asian J Urol. (2017) 4:111–5. doi: 10.1016/j.ajur.2016.05.007
23. Arnbjörnsson E, Kullendorff CM. Testicular torsion in children—bilateral or unilateral operation. Acta Chir Scand. (1985) 151:425–7.
24. Fehér ÁM, Bajory Z. A review of main controversial aspects of acute testicular torsion. J Acute Dis. (2016) 5:1–8. doi: 10.1016/j.joad.2015.06.017
Keywords: orchiectomy, clinical characteristics, risk factors, testicular torsion, orchidopexy
Citation: Zhang K, Zhang Y and Chao M (2023) Clinical characteristics and identification of risk factors of testicular torsion in children: A retrospective study in a single institution. Front. Surg. 9:1040487. doi: 10.3389/fsurg.2022.1040487
Received: 9 September 2022; Accepted: 13 October 2022;
Published: 6 January 2023.
Edited by:
Bo Li, University of Toronto, CanadaReviewed by:
Edoardo Bindi, Salesi Hospital Foundation, Italy© 2023 Zhang, Zhang and Chao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Min Chao Y20wNjU0QHNpbmEuY29t
Specialty Section: This article was submitted to Pediatric Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.