
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 06 January 2023
Sec. Thoracic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1040224
 Jing Xin*
Jing Xin* Xiu-juan Fan
Xiu-juan Fan
Background: To investigate the effect of visual endotracheal tube combined with bronchial occluder on pulmonary ventilation and arterial blood gas in patients undergoing thoracic surgery.
Methods: Ninety patients who underwent thoracic surgery under anesthesia and required pulmonary ventilation at our hospital from May 2020 to December 2021 were collected. The patients were divided into three groups according to different intubation methods: visual double-lumen endotracheal tube group (VDLT group), bronchial occluder group (BO group), and VDLT + BO group. Clinical data and laboratory test data were collected from the three groups. Additionally, the three groups were compared in terms of peak airway pressure, time to correct positioning, pulmonary ventilation time, hemodynamics before and after intubation, intubation success rate, and postoperative recovery.
Results: The VDLT + BO group was superior to the BO group or VDLT group in airway peak pressure, time to correct positioning, pulmonary ventilation time, intubation success rate, and hemodynamics after intubation (P < 0.05). In the comparison of postoperative recovery, the postoperative pain score, white blood cell level, incidence rate of pneumonia, hospital stay and hospitalization costs in the VDLT + BO group were significantly lower than those in the BO group or VDLT group (P < 0.05).
Conclusion: The visual endotracheal tube combined with bronchial occluder is effective in pulmonary ventilation during thoracic surgery under anesthesia, and can improve arterial blood gas in patients.
At present, about 200,000 cases of thoracic surgery are performed in China each year, and the number is increasing at a rate of 5%–7% per year. Thoracoscopic surgery has many advantages such as small incision, wide surgical field, rapid postoperative recovery, and therefore has been widely applied in clinical practice (1). The key to thoracoscopic surgery is lung isolation and one-lung ventilation. Lung isolation is required to ensure ventilation and to prevent entry of blood, secretions, and tumor necrotic tissue from an affected lung into a non-diseased lung. Additionally, by using lung isolation techniques, fully lung collapse of the affected lung is achieved, contributing to improving surgical exposure and subsequent surgical procedures.
There are two common methods of lung isolation. The first is a double-lumen tube (DLT). It can effectively isolate both lungs to provide independent ventilation for each lung, can provide a sucker for sputum in the isolated lung, and effectively prevent various secretions from flowing to the healthy lung, especially suitable for patients with wet lung and empyema (2). However, due to the large outer diameter of the tube, intubation of DLT is relatively difficult and results in many problems and complications, such as hypoxemia, increased peak airway pressure, and airway injury (3). The second is a bronchial occluder (BO). BO is inserted into one bronchus (left or right) through an endotracheal tube, and then the cuff is inflated to seal the bronchus and achieve lung isolation (4). BO is more and more widely used because of its advantages of easy intubation, easy positioning, little injury and satisfactory occlusion effect, acting as an alternative to DLT (5, 6).
An endotracheal tube mounted camera is a new intubation tool with an embedded high-definition camera in the anterior wall at the tip of tube, along with a monitor connected to the camera, LED light, and a unique flush port for cleaning the camera (7). In patients without a difficult airway, the use of a visual endotracheal tube allows safe and rapid endotracheal intubation while not requiring laryngoscopic assistance (8, 9). However, there are no Chinese reports on the effect of visual endotracheal tube combined with BO on lung ventilation in thoracic surgery under anesthesia and its effect on arterial blood gas in patients. Therefore, this study comprehensively analyzed the clinical safety and advantages of the combination by measuring peak airway pressure, time to correct positioning, pulmonary ventilation time, hemodynamics and postoperative recovery.
We collected 90 patients undergoing thoracic surgery under anesthesia at our hospital and requiring pulmonary ventilation from May 2020 to December 2021 for a prospective randomized controlled trial. According to the random number table, they were divided into three groups: VDLT group (n = 30, visual DLT), BO group (n = 30, BO), VDLT + BO group (n = 30, visual DLT + BO).
Inclusion criteria were: (1) Patients who need thoracic surgery; (2) Aged 18–80 years old; (3) Normal pulmonary function or mild ventilation dysfunction; (4) The American Society of Anesthesiologists (ASA) class I-IV. Exclusion criteria were: (1) Patients with thoracic deformity or trauma; (2) Patients with abnormal cardiopulmonary function; (3) Bronchi variation with anatomical abnormality; (4) Suspected difficult airway, such as thyromental distance <6 cm, mouth opening <3 fingers, and Mallampati airway class III–IV; (5) Patients with malignant arrhythmia; (5) Patients with severe liver and kidney dysfunction; (6) Patients with mental illness, severe cognitive impairment or language problems. This study was approved by the ethics committee of our hospital, and both patients and their families understood the purpose of this study and had signed an informed consent. This study was approved by the Ethics Committee of Ordos Center Hospital (20200116).
All patients were admitted to the operating room for routine opening of venous access, followed by an infusion of lactated Ringer's balanced solution. Patients' heart rate (HR), non-invasive blood pressure (NIBP), oxygen saturation (SpO2), electrocardiogram (ECG), partial pressure of end-tidal carbon dioxide (PETCO2), and depth of anesthesia by Narcotrend. The endotracheal tube suitable for the patients was selected based on their gender, height, body mass, and surgical approach. Induction of anesthesia was achieved with intravenous injection of 0.05–0.07 mg/kg midazolam, 4 μg/kg fentany l, 2 mg/kg propofol, and 0.2 mg/kg cisatracurium, and effective manual ventilation with a mask was given for 3 min. With completely relaxed muscle, the Narcotrend index of 37–64, and SpO2 reaching 100%, endotracheal intubation was started. All procedures were performed in cooperation with two experienced anesthesiologists.
In the VDLT group, the tube was inserted until it entered one of the main bronchus, and the cuff was inflated. The edges of the blue cuff, primary carina, and the other main bronchus were visible at the same time, suggesting correct placement. Additionally, the auscultation method proved successful tube positioning. Finally, the tube was fixed. In the BO group, the occluder was placed directly in the main bronchus requiring occlusion under the guidance of a fiberoptic bronchoscope. In the VDLT + BO group, the occluder was directly advanced to the target mainstem bronchus through the DLT mounted camera; both lungs were auscultated and the occluder position was continuously monitored. In the latter two groups, after confirming the correct position of the BO, one-lung ventilation was performed to adjust the respiratory parameters and the anesthesia ventilator was connected for volume-controlled ventilation. The position of the tube and occluder was monitored throughout the operation and adjusted in time if the surgical position changed.
The peak airway pressure, time to correct positioning and pulmonary ventilation time before and after intubation were compared among the three groups. Hemodynamic changes, including mean arterial pressure (MAP), HR, SpO2, arterial partial pressure of carbon dioxide (PaCO2), partial pressure of oxygen (PaO2), forced expiratory volume in 1 s (FEV1), and forced vital capacity (FVC), were compared. In addition, the airway class, and success rate of intubation as well as the pain score (10), white blood cell level, incidence rate of pneumonia, length of hospital stay and hospitalization costs of patients after thoracic surgery were compared among the three groups.
SPSS 22.0 statistical software was used for statistical analysis. Measurement data were expressed as mean ± standard deviation (SD); A Student's t test was used for comparison between the two groups, and a one-way analysis of variance was used for comparison between multiple groups. Enumeration data were expressed as rates, and chi-square test was used for analysis. P < 0.05 was considered as statistically significant.
A total of 90 patients receiving thoracic surgery were collected, divided into VDLT group (17 males, 13 females), BO group (19 males, 11 females), and VDLT + BO group (19 males, 11 females), with 30 cases in each group. There were no significant differences among the groups in age, gender, body mass index, ASA classification, systolic blood pressure, diastolic blood pressure, duration of hypertension, history of previous myocardial infarction, smoking history, history of alcoholism, complications, disease type, and preoperative levels of MAP, FEV1, and FVC (all P > 0.05), indicating that the groups were comparable (Table 1).
According to the comparison shown in Table 2, the peak airway pressure of patients in the VDLT + BO group was the smallest after intubation (22.64 ± 1.54 mmHg), significantly lower than that in the VDLT group (27.08 ± 1.51 mmHg) and the BO group (24.70 ± 1.70 mmHg) (P < 0.01). Also, the VDLT + BO group had the shortest time to correct positioning and longest pulmonary ventilation time (P < 0.01).
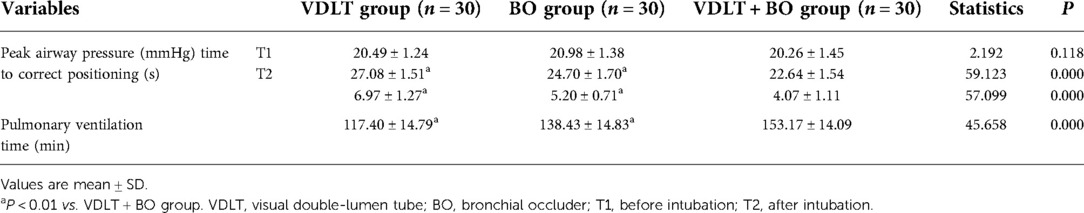
Table 2. Comparison of peak airway pressure, time to correct positioning and pulmonary ventilation time before and after intubation .
As shown in Table 3, in patients with different airway classes, the VDLT + BO group had the highest number of patients who completed intubation (27/30), but there was no significant difference among the groups (P > 0.05).
As shown in Table 4, there was no significant difference in all hemodynamic parameters before intubation among the three groups (P > 0.05). After tracheal intubation, MAP, HR, SpO2, PaCO2, PaO2, FEV1 and FVC in the VDLT + BO group were significantly better than those in the BO group and the VDLT group, with the worst performance in the VDLT group (P < 0.05).
Finally, we compared the postoperative recovery of patients in the three groups (Table 5). Patients in the VDLT + BO group had significantly lower postoperative pain scores, lowest incidence of infection, longer hospital stays, and required less costs than patients compared with the VDLT group and the BO group.
DLT has the advantages of good lung isolation, safety, and easy fixation, but it has a large diameter, special shape, and hard texture. DLT is difficult to operate, easily causing greater stimulation to the body during intubation and extubation, damage to the airway, increased airway pressure, and prolonged time to correct positioning (11–13). Therefore, DLT is not conducive to stable progress of thoracic surgery. As a new lung isolation method and new one-lung ventilation technique, BO is selected by clinicians and patients because of its small outer diameter and 50% increase in the area of one-lung ventilation tube compared with DLT, which just compensates for the disadvantages of DLT (2, 14). In this study, a combination of visual DLT and BO was innovatively used for lung isolation. Such a combination can obtain clear real-time visual monitoring during intubation and the advantages of both methods.
At present, the application advantages of visual endotracheal tube combined with BO in clinical surgery are significant. Liang (15) et al. compared the visual single-lumen endotracheal tube combined with BO in thoracic surgery with common single-lumen endotracheal tube combined with BO, and found that the former was superior in intraoperative time to correct positioning, postoperative pneumonia infection rate and postoperative airway mucosal injury degree. In our study, patients who received a combination of visual DLT and BO had significantly better rates of postoperative pulmonary infection, less postoperative pain, shorter length of hospital stay, and lower costs than those who received visual DLT or BO alone.
Peak airway pressure refers to the highest airway pressure in mechanical ventilation, and once BO cuff displaces, peak airway pressure is directly affected, which has also been a problem for clinicians (16, 17). Our study found that patients who underwent thoracic surgery with visual DLT combined with BO intubation had the smallest peak airway pressure after surgery (22.64 ± 1.54 mmHg), while patients who were intubated with visual DLT alone had the largest value. Additionally, the ADLT + BO group was superior to the other two groups in time to correct positioning, pulmonary ventilation time, airway classification and intubation success rate as well as hemodynamic comparison, and the performance of BO alone was better than visual DLT alone. Similarly, Xu (18) et al. found that the time to correct positioning and intubation time of BO alone were shorter than those of common DLT, and the airway pressure was lower. However, a meta-analysis (19) showed that compared with common DLT alone in thoracic surgery, BO alone required shorter time to correct positioning and was safer, but was associated with higher incidence and severity of airway injury. Anesthesiologists' familiarity with airway anatomy and proficiency in the procedure brings some difference in effect.
Collectively, our study demonstrates that the visual DLT combined with BO provides good ventilation, better hemodynamics, and high safety. Therefore, it shows high application value as an important method to achieve lung isolation; endobronchial blockers suitable for specific surgery procedure should be selected based on their characteristics and indications, thus minimizing the damage to patients.
The limitation of this study is the lack of observation of long-term prognosis of patients, and the types of thoracic surgery performed inside the groups were different, which existed certain bias when exploring outcomes such as postoperative complications, postoperative length of stay, or post-extubation values of pulmonary performance and gas exchange. These will be further improved in future studies, requiring large multicenter cohorts and more in-depth studies using prospective settings.
In summary, during thoracic surgery under anesthesia, visual endotracheal tube combined with BO offers the advantages of lower peak airway pressure and better performance in oxygenation, hemodynamic parameters, postoperative recovery of patients. Therefore, such a combination is a good choice to safely and effectively achieve single-lung ventilation during thoracic surgery under anesthesia.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ordos Center Hospital(20200116). The patients/participants provided their written informed consent to participate in this study.
JX and XF conceived and supervised the study. JX wrote the manuscript. XF collected the data and performed statistical analyses. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
DLT, double-lumen tube; BO, bronchial occluder; HR, heart rate, NIBP, non-invasive blood pressure; SpO2, oxygen saturation; ECG, electrocardiogram; PETCO2, partial pressure of end-tidal carbon dioxide; MAP, mean arterial pressure; PaCO2, arterial partial pressure of carbon dioxide; PaO2, partial pressure of oxygen; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
1. Das K, Rothberg M. Thoracoscopic surgery: historical perspectives. Neurosurg Focus. (2000) 9(4):e10. doi: 10.3171/foc.2000.9.4.10
2. Ruetzler K, Grubhofer G, Schmid W, Papp D, Nabecker S, Hutschala D, et al. Randomized clinical trial comparing double-lumen tube and EZ-Blocker for single-lung ventilation. Br J Anaesth. (2011) 106:896–902. doi: 10.1093/bja/aer086
3. Ghosh S, Klein AA, Prabhu M, Falter F, Arrowsmith JE. The papworth BiVent tube: a feasibility study of a novel double-lumen endotracheal tube and bronchial blocker in human cadavers. Br J Anaesth. (2008) 101:424–8. doi: 10.1093/bja/aen167
4. Gothard J. Lung injury after thoracic surgery and one-lung ventilation. Curr Opin Anaesthesiol. (2006) 19:5–10. doi: 10.1097/01.aco.0000192783.40021.c1
5. Campos JH, Kernstine KH. A comparison of a left-sided Broncho-Cath with the torque control blocker univent and the wire-guided blocker. Anesth Analg. (2003) 96:283–9. doi: 10.1097/00000539-200301000-00056
6. Knoll H, Ziegeler S, Schreiber JU, Buchinger H, Bialas P, Semyonov K, et al. Airway injuries after one-lung ventilation: a comparison between double-lumen tube and endobronchial blocker: a randomized, prospective, controlled trial. Anesthesiology. (2006) 105:471–7. doi: 10.1097/00000542-200609000-00009
7. Grensemann J, Eichler L, Kahler S, Jarczak D, Simon M, Pinnschmidt HO, et al. Bronchoscopy versus an endotracheal tube mounted camera for the peri-interventional visualization of percutaneous dilatational tracheostomy - a prospective, randomized trial (VivaPDT). Crit Care. (2017) 21:330. doi: 10.1186/s13054-017-1901-0
8. Gaitini LA, Yanovski B, Mustafa S, Hagberg CA, Mora PC, Vaida SJ. A feasibility study using the VivaSight Single Lumen to intubate the trachea through the Fastrach laryngeal mask airway: a preliminary report of 50 cases. Anesth Analg. (2013) 116:604–8. doi: 10.1213/ANE.0b013e31827b278f
9. Kurowski A, Szarpak L, Truszewski Z, Czyzewski L. Can the ETView VivaSight SL rival conventional intubation using the macintosh laryngoscope during adult resuscitation by novice physicians?: a randomized crossover manikin study. Medicine (Baltimore). (2015) 94:e850. doi: 10.1097/MD.0000000000000850
10. Alfonsin MM, Chapon R, de Souza CAB, Genro VK, Mattia MMC, Cunha-Filho JS. Correlations among algometry, the visual analogue scale, and the numeric rating scale to assess chronic pelvic pain in women. Eur J Obstet Gynecol Reprod Biol X. (2019) 3:100037. doi: 10.1016/j.eurox.2019.100037
11. Zhang N, Liu HZ, Yang CX, Wen XJ. Comparison of bronchial blocker and double-lumen tube in thoracoscopic surgery. Guangdong Med J. (2012) 33:1163–5. doi: 10.3969/j.issn.1001-9448.2012.08.054
12. Hu B, Li ZJ, Shao WD, Zhou QM, Yang RY, Tu WF. Clinical observation of bronchial blocker for one lung ventlation during right-sided video-assisted thoracic surgery. Mil Med J South China. (2015) 29:817–20. doi: 10.3969/j.issn.1009-2595.2015.11.004
13. Chen JY, Liao SJ, Wang F. Influence of bronchial occluder on ventilation and hemodynamics in patients with thoracolaparoscopic esophagectomy. J Chin Pract Diagn Ther. (2017) 31:677–80. doi: 10.13507/j.issn.1674-3474.2017.07.015
14. Grichnik KP, Clark JA. Pathophysiology and management of one-lung ventilation. Thorac Surg Clin. (2005) 15:85–103. doi: 10.1016/j.thorsurg.2004.09.004
15. Liang F, Zheng S, Li J, Xiao XS, Wen LH, Lin JG. Application of visible single-lumen tube combined with bronchial occluder in one-lung ventilation surgery. Guangdong Med J. (2019) 40:1791–4. doi: 10.13820/j.cnki.gdyx.20186894
16. Vinay B, Sriganesh K, Gopalakrishna KN, Sudhir V. An unusual cause of high peak airway pressure: interpretation of displayed alarms. Saudi J Anaesth. (2015) 9:94–6. doi: 10.4103/1658-354X.146326
17. Tian X, Fang W, Wu J. The effects of different mechanical ventilation flow model on the peak airway pressure during cardiopulmonary resuscitation. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2014) 26:722–5. doi: 10.3760/cma.j.issn.2095-4352.2014.10.009
18. Xu HF, Zhai YJ. Comparison of double-lumen tube and bronchial occluder in patients undergoing thoracic surgery. China Pract Med. (2021) 16:100–2. doi: 10.14163/j.cnki.11-5547/r.2021.17.036
19. Clayton-Smith A, Bennett K, Alston RP, Adams G, Brown G, Hawthorne T, et al. A comparison of the efficacy and adverse effects of double-lumen endobronchial tubes and bronchial blockers in thoracic surgery: a systematic review and meta-analysis of randomized controlled trials. J Cardiothorac Vasc Anesth. (2015) 29:955–66. doi: 10.1053/j.jvca.2014.11.017
Keywords: thoracic surgery, visual endotracheal tube, bronchial occluder, pulmonary ventilation, arterial blood gas
Citation: Xin J and Fan X (2023) Effect of visual endotracheal tube combined with bronchial occluder on pulmonary ventilation and arterial blood gas in patients undergoing thoracic surgery. Front. Surg. 9:1040224. doi: 10.3389/fsurg.2022.1040224
Received: 9 September 2022; Accepted: 4 November 2022;
Published: 6 January 2023.
Edited by:
Mohsen Ibrahim, Sapienza University of Rome, ItalyReviewed by:
Yener Aydin, Atatürk University, Turkey© 2023 Xin and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Xin eGluMTk4MTEyMjZAMTYzLmNvbQ==
Specialty Section: This article was submitted to Thoracic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.