- Department of Orthopedics, Orthopedic Research Institute, West China Hospital, Sichuan University, Chengdu, China
Objective: To conduct a high-level meta-analysis of the RCTs to evaluate perioperative steroids use in the management of fusion rate, dysphagia, and VAS following anterior cervical spine surgery for up to 1 year.
Methods: We searched the database PubMed, EMBASE, Web of Science, Cochrane Library, Google Scholar, Ovid, and ClinicalTrials.gov without time restriction to identify RCTs that evaluate the effectiveness of perioperative steroids after anterior cervical spine surgery. A subgroup analysis was undertaken to investigate the effects of intravenous and local steroids. This study was registered in the PROSPERO database prior to initiation (CRD42022313444).
Results: A total of 14 RCTs were eligible for final inclusion. This meta-analysis showed that steroids could achieve lower dysphagia rate (p < 0.001), severe dysphagia rate within 1 year (p < 0.001), lower VAS scores at both 1 day (p = 0.005), 2 weeks (p < 0.001) and shorter hospital stay (p = 0.014). However, there was no significant difference between the two groups regarding operation time (p = 0.670), fusion rates (p = 0.678), VAS scores at 6 months (p = 0.104) and 1 year (p = 0.062). There was no significant difference between intravenous and local steroid administration regarding dysphagia rates (p = 0.82), fusion rate (p = 1.00), and operative time (p = 0.10).
Conclusion: Steroids intravenously or locally following anterior cervical spine surgery can reduce incidence and severity of dysphagia within 1 year, VAS score within 2 weeks, and shorten the length of hospital stay without affecting fusion rates, increasing the operating time, VAS score at 6 months and 1 year.
Introduction
Since first introduced in 1958 by Cloward (1), Robinson and Smith (2), anterior approach has become the standard approach in the treatment of spondylotic radiculopathy and myelopathy with demonstrated long-term clinical success. However, it is associated with complications such as dysphagia, presumably due to local tissue swelling, intraoperative excessive retraction, and laryngeal nerve palsy. Rates of postoperative dysphagia ranged in frequency from 1.7% to 67% according to previous reports (3–6). Dysphagia after ACDF has raised concerns about increasing morbidity, duration of hospitalization, and medical costs (7).
Many measures have been investigated to decrease the incidence of dysphagia and decreased cuff pressure and plate prominence are just a few (8–11). One promising therapeutic intervention is the use of perioperative steroids (12–14). In some studies, the steroid has resulted in decreased incidence and severity of dysphagia (13, 15). However, the effect of steroids has been equivocal in other studies (16). In addition to inconsistent results for dysphagia, there is concern about the adverse effects of steroids, such as delayed time to fusion (12). From the surgeon's point of view, solid bony fusion is of critical importance in the achievement of expected outcomes following anterior cervical spine surgery. Delayed bony fusion or even non-union after surgery greatly increases the risk of revision (17). In addition, it has been reported that steroids can reduce postoperative pain by reducing the inflammatory response (18). Nevertheless, the duration of this effect still remains controversial.
Considering these issues, it is important to perform a systematic review and meta-analysis to provide clear advice concerning the accurate effect of steroids on the incidence and severity of dysphagia, fusion rate and VAS score. Moreover, a subgroup analysis was needed to compare the effects of intravenous and local steroids as a consensus on the use of intravenous and local injections has not yet been reached.
Methods
This systematic review was conducted following the Preferred Reported Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines, the Cochrane Collaboration recommendations and AMSTAR (Assessing the methodological quality of systematic reviews) (19, 20), and the study protocol was registered in the international open-access Prospective Register of Systematic Reviews (PROSPERO, number: CRD42022313444) prior to data retrieval.
Search strategy
A comprehensive literature search was conducted on PubMed, EMBASE, Web of Science, Cochrane Library, Google Scholar, Ovid, and ClinicalTrials.gov from inception to February 19, 2022. Search terms included both entry terms and medical descriptors/MeSH terms such as “Glucocorticoids”, “Steroids”, “Methylprednisolone”, “Dexamethasone”, “anterior cervical discectomy and fusion”, “Anterior cervical surgery”, “Anterior cervical fusion”, “Anterior Cervical Corpectomy and Fusion”. Supplementary File S1 summarizes the search strategy used in each database.
Assessment of eligibility
Studies satisfying the following criteria were included: (1) population: adults with spondylotic radiculopathy and myelopathy undergoing anterior cervical spine surgery; (2) intervention: perioperative intravenous or local steroids administration; (3) comparison: placebo vs. steroids; (4) main outcomes: the event number of dysphagia, visual analog scale (VAS) at postoperative 1 day, 2 weeks, 6 months and 1 year, fusion rates at 1 year; (5) study design: RCT design.
The following studies were excluded: (1) Letters, editorials, conference abstracts, systematic reviews or meta-analyses, consensus statements, guidelines; (2) Had insufficient data this meta-analysis required; (3) Contained comparisons with other comparison protocols; (4) Full-text was not available.
Data extraction
Data extraction was conducted by two independent reviewers using a piloted and standardized data extraction form. Any disagreements were resolved by mutual consensus. The following data from each included study were retrieved: (1) Study characteristics: authors' information, publication year; (2) Patients' characteristics: size of each group, mean age, male-to-female ratio; (3) Intervention: route of administration and dose; (4) Outcomes: dysphagia events, fusion rate, VAS score, operation time, length of hospital stay.
Risk of bias and quality assessment
The quality and risk of bias were assessed by two independent reviewers using the Cochrane Handbook for Systematic Reviews of Interventions (20). Any disagreements were resolved by mutual consensus. This quality evaluation system includes seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias. Each domain was assessed as low, unclear, or high risk. Risk of bias graphs were plotted using the Revman software (version 5.3). The results of outcomes were assessed the quality of evidence by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) under the software GRADE profiler (https://gradeprofler.sofware.informer.com/download/).
Statistical analysis
We used Stata 14.0 for statistical analysis. Mean difference with 95% confidence intervals (CIs) was used to evaluate continuous data, and odds ratio was used for dichotomous data. p value was calculated and documented for each outcome measure. Statistical significance was defined as a p value less than 0.05 (p < 0.05).
Statistical heterogeneity was assessed using the I2 test. The I2 statistic describes the percentage of variation in each study due to heterogeneity rather than chance, while I2 values of 0%–25%, 25%–50%, 50%–75%, and >75% represent very low, low, medium, and high heterogeneity, respectively (21). A random-effect model was applied when the I2 value was over 50%, and a fixed-effect model was applied conversely.
In addition, a subgroup analyses by the route of administration (Local vs. Intravenous) was performed to further evaluate the effects of intravenous and local steroids. A sensitivity analysis that excluding studies one by one was performed to investigate the effect of steroid intervention on evaluation indicators.
Results
Search results
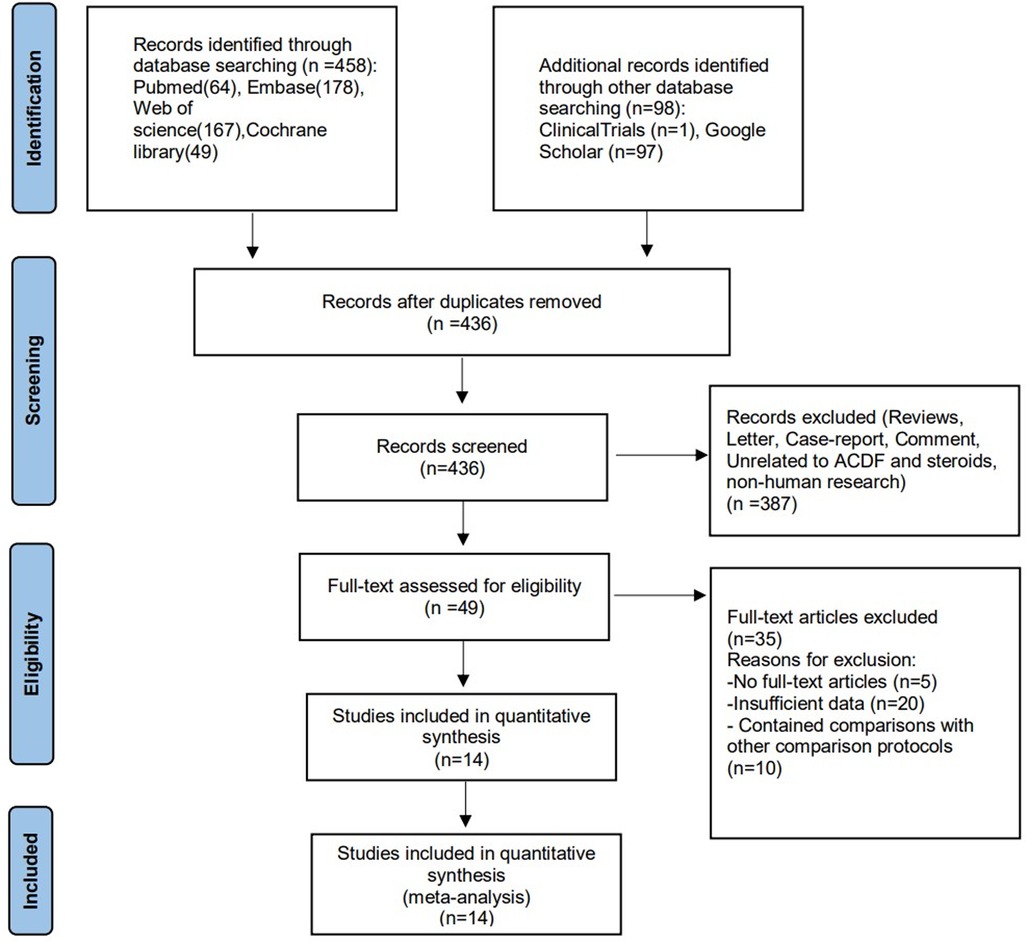
The systematic literature search initially identified 436 potentially eligible articles from PubMed, Embase, Web of Science, Cochrane Library, Google Scholar, and ClinicalTrials.gov (Figure 1). After excluding 120 duplicates, screening of the remaining 436 titles and abstracts yielded 49 potentially eligible articles. After full-text reviews of the 49 provisionally eligible articles, 35 articles were excluded due to no access to full-text (5), contained insufficient data (20), contained comparisons with other comparison protocols (10). Finally, 14 articles were included in this present systematic review and meta-analysis.
Characteristics of the included studies
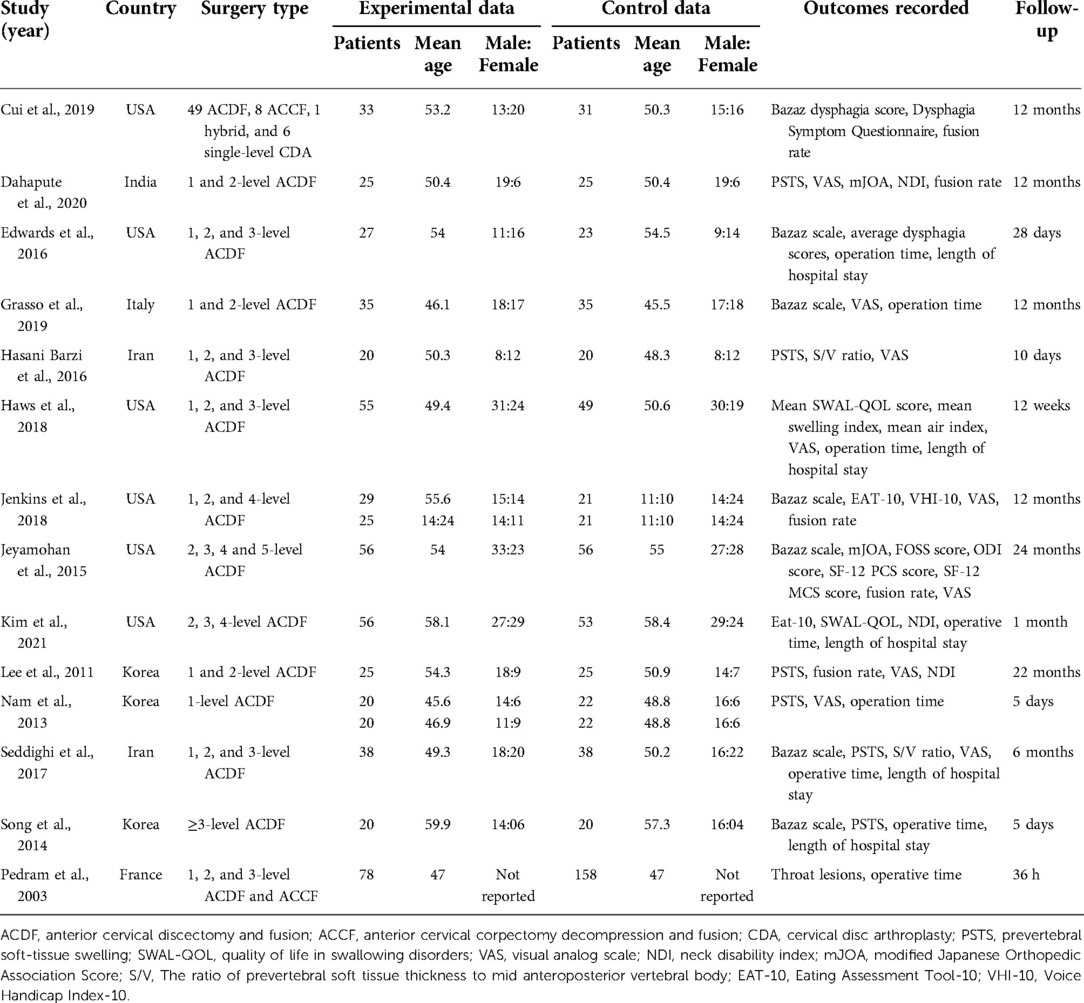
Details of study demographics of steroid-administered patients, details of the administration of the steroids, and steroids effects assessment after anterior cervical fusion are summarized in Table 1, 2. All the 14 articles (16, 18, 22–33) were prospective randomized controlled trials that were graded as the level of evidence 1, and three of them were double-blinded studies (22, 24, 30). A total of 1,181 patients were enrolled across all 14 randomized controlled studies. In total, 252 patients received intravenous steroids, 310 patients received topical steroids, and 619 patients served as controls. The corticosteroid treatment arms utilized IV dexamethasone (16, 22, 28, 29) or methylprednisolone (31, 33) or local injection of methylprednisolone (24–27, 30, 32) or triamcinolone (18, 23, 28).
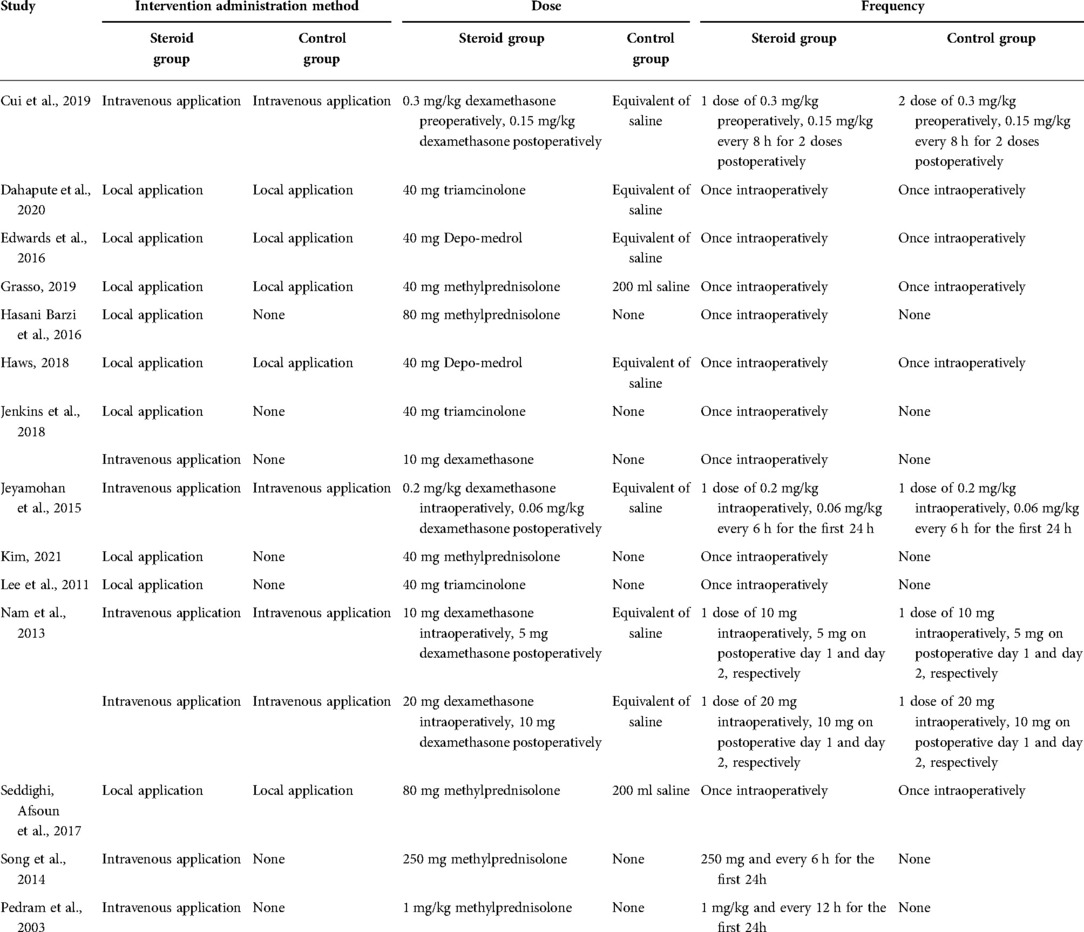
Table 2. The intervention administration methods, steroid dose and frequency in each included study.
Quality assessment to risk of bias
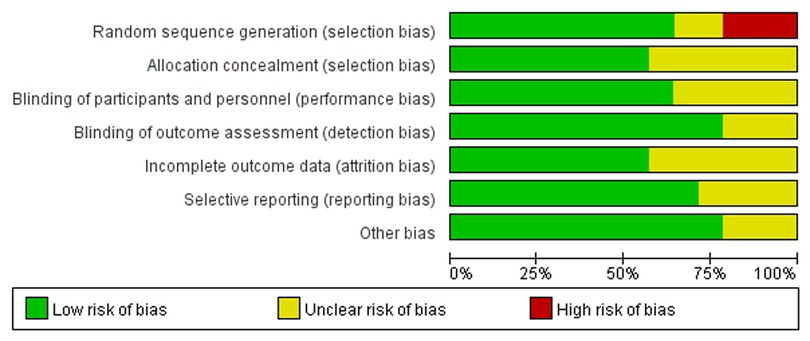
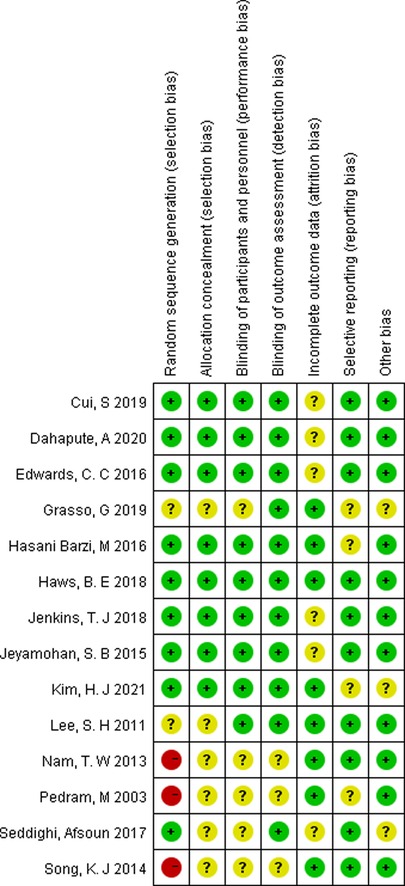
Two independent reviewers evaluated the quality of 14 RCTs according to the criteria of the Cochrane Collaboration for Systematic Reviews and any disagreements were solved through discussion and consensus. Three studies were found to have a “high” risk of bias, primarily attributed to the randomization process. The overall risk of bias of the included studies was determined to be low (Figures 2, 3).
Quality of evidence assessment by GRADE
The results of dysphagia event, Bazaz stratification of severity of dysphagia, fusion rate, VAS, operation time and length of hospital stay were assessed the quality of evidence by GRADE. The results qualities of VAS were low, and dysphagia event, Bazaz stratification of severity of dysphagia, fusion rate, operation time and length of hospital stay were moderate. None of high quality evidence was found in above outcomes (Table 3).
Results of meta-analysis
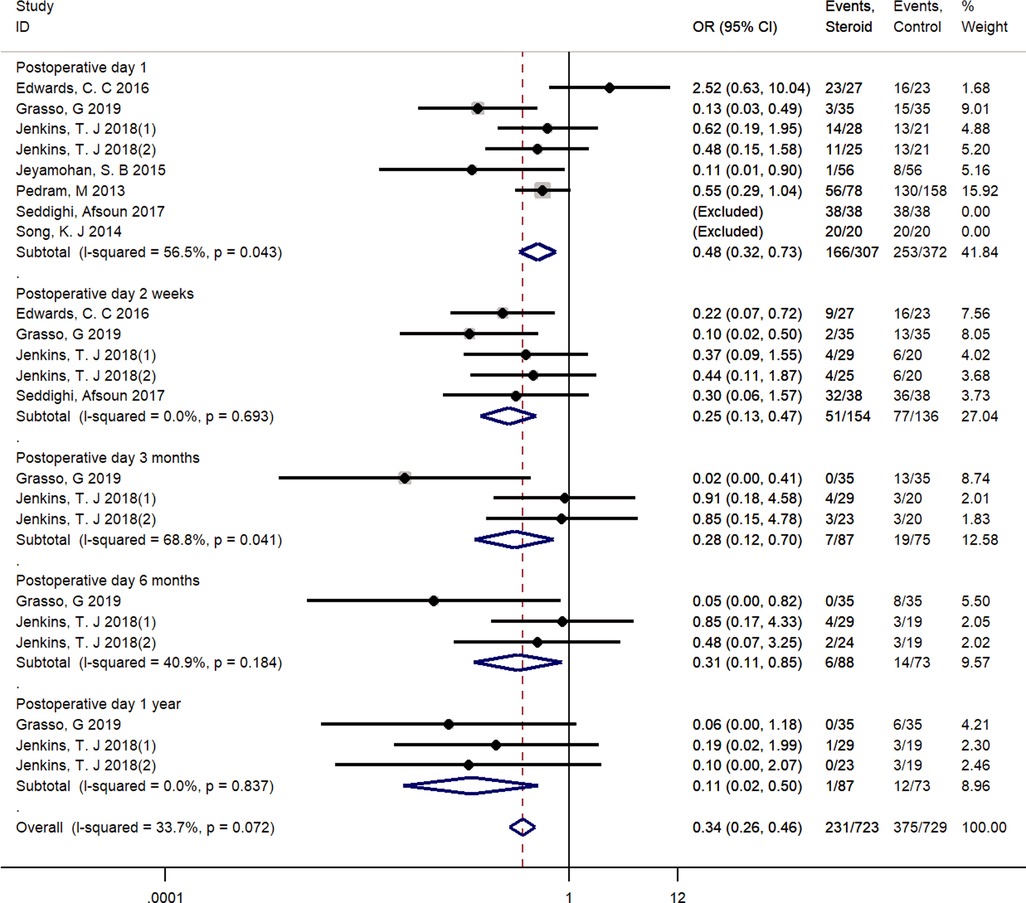
The use of steroids for dysphagia event from postoperative 1 day to 1 year
The most commonly used assessment tool for dysphagia was the Bazaz scale (25, 28, 29, 31–33). One study used its modified version, the Modified Dysphagia Scoring System (MDSS) (24). The pooled outcomes showed that steroid use achieved significantly lower dysphagia rates compared with the incidence in the control group (1 day, OR = 0.48, 95% CI: 0.32–0.73, 2 weeks, OR = 0.25, 95% CI: 0.13–0.47; 3 months, OR = 0.28, 95% CI: 0.12–0.70; 6 months, OR = 0.31, 95% CI: 0.11–0.85; 1 year, OR = 0.11, 95% CI: 0.02–0.50). With a fixed-effect model, a low heterogeneity among these studies was found in the pooled outcomes (I2 = 33.7%, p = 0.072) (Figure 4).
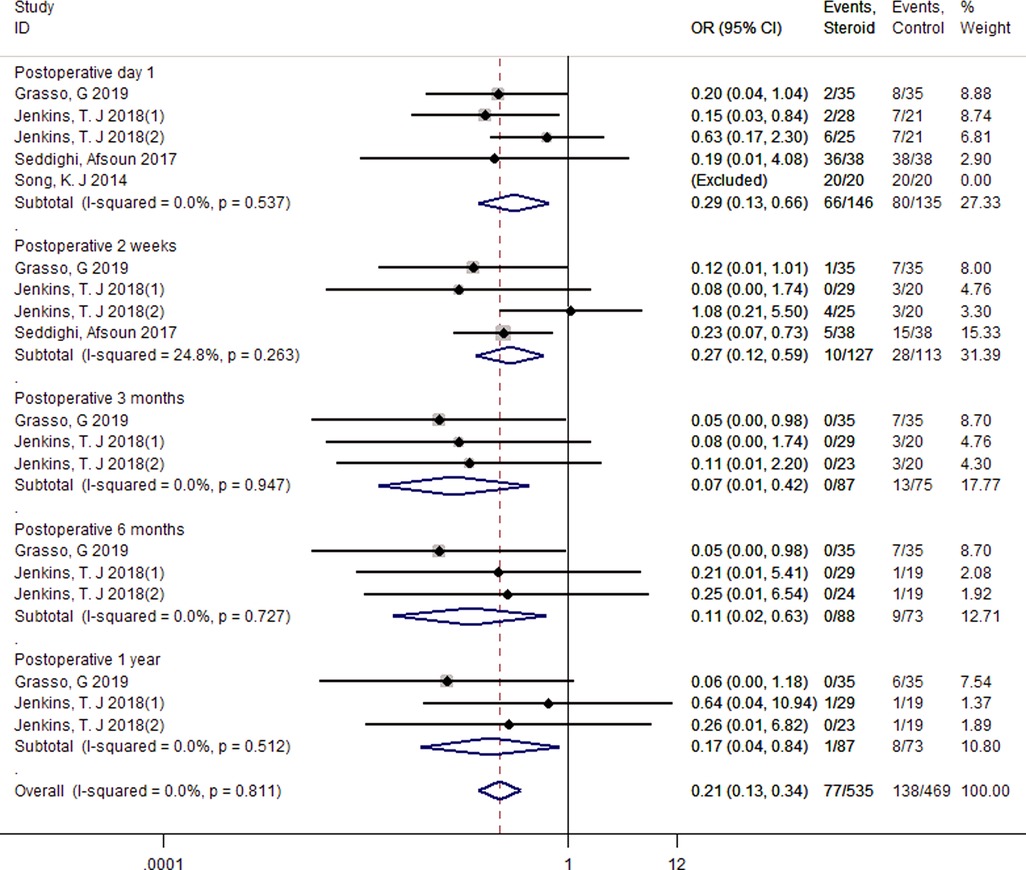
Bazaz stratification of severity of dysphagia (moderate + severe) from postoperative 1 day to 1 year
A fixed-effect model was used to pool the total moderate and severe Bazaz stratification because there was no significant heterogeneity across four studies (I2 = 0.00%, p = 0.811) (25, 28, 32, 33). The pooled analysis revealed less moderate and severe events in the steroid group compared with the control group within 1 year after surgery (1 day, OR = 0.29, 95% CI: 0.13–0.66; 2 weeks, OR = 0.27, 95% CI: 0.12–0.59; 3 months, OR = 0.07, 95% CI: 0.01–0.42; 6 months, OR = 0.11, 95% CI: 0.02–0.63; 1 year, OR = 0.17, 95% CI: 0.04–0.84) (Figure 5).
The use of steroids for fusion rate at 1-year follow-up
Five studies reported numbers of fusion events at 1-year follow-up time and were included (18, 22, 23, 28, 29). There existed no significant difference between groups regarding fusion rate (OR = 0.87, 95% CI: 0.46–1.65), and no significant heterogeneity among these studies was found with a fixed-effect model (I2 = 0.0%, p = 0.999) (Figure 6).
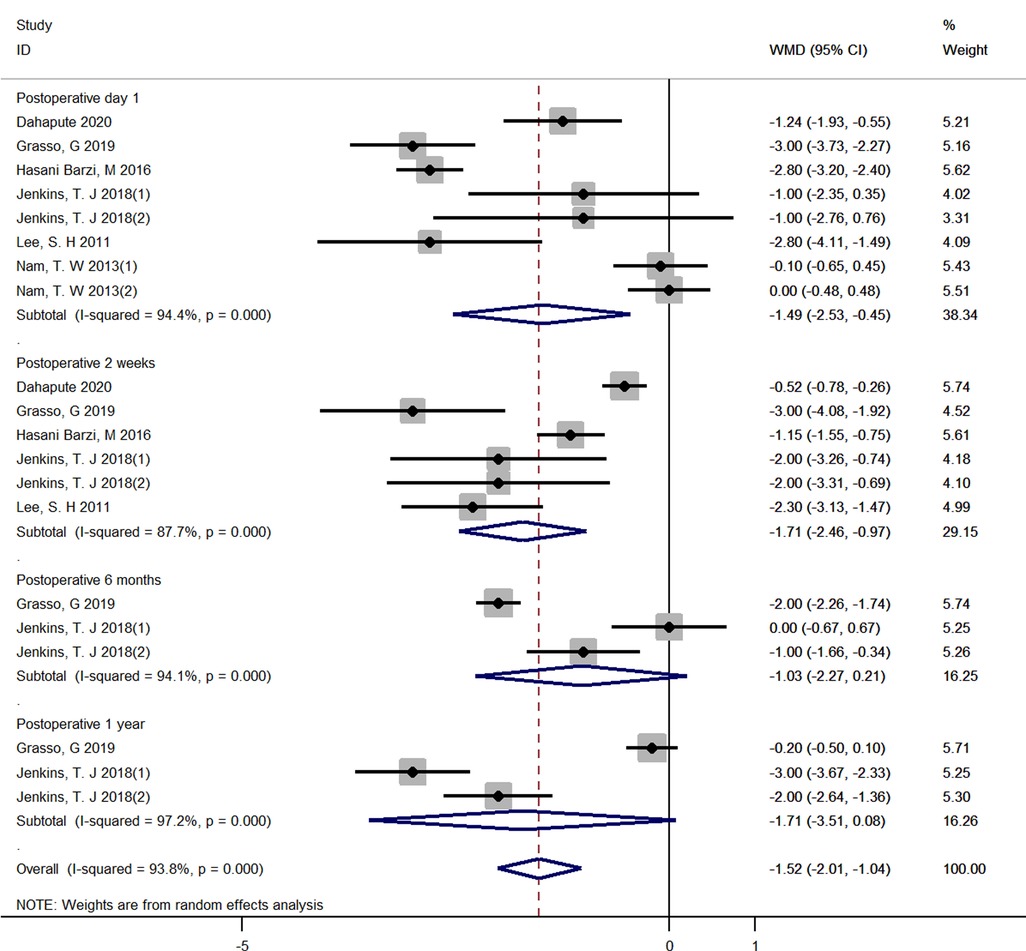
The use of steroids for VAS from postoperative 1 day to 1 year
Six RCTs reported the detailed VAS score and were included (16, 18, 23, 25, 26, 28). A random-effect model was applied due to the high heterogeneity (I2 = 93.4%, p < 0.001). A significant decrease regarding VAS score in the steroid group was observed compared with that in the control group at both 1 day, 2 weeks after surgery (1 day, WMD = −1.49, 95% CI: −2.53 to −0.45; 2 weeks, WMD = −1.71, 95% CI: −2.46 to −0.97). However, Pooled analysis revealed no significant difference in the VAS score between two groups at both 6 months and 1 year after surgery (6 months, WMD = −1.03, 95% CI: −2.27 to 0.21; 1 year, WMD = −1.71, 95% CI: −3.51 to 0.08) (Figure 7).
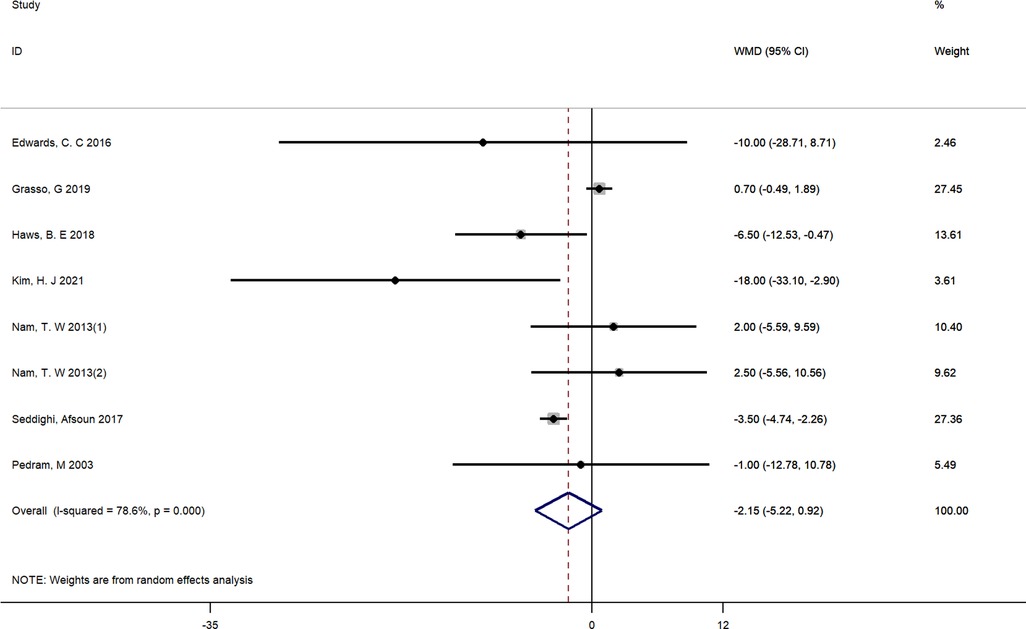
Operation time
Seven studies reported the detailed operation time and were included (16, 24, 25, 27, 30–32). There was significant heterogeneity between studies (I2 = 78.6%, p < 0.01), and a random-effect model was adopted. Pooled results demonstrated that there was no significant difference between groups in operating time (WMD = −2.15, 95% CI: −5.22 to 0.92) (Figure 8).
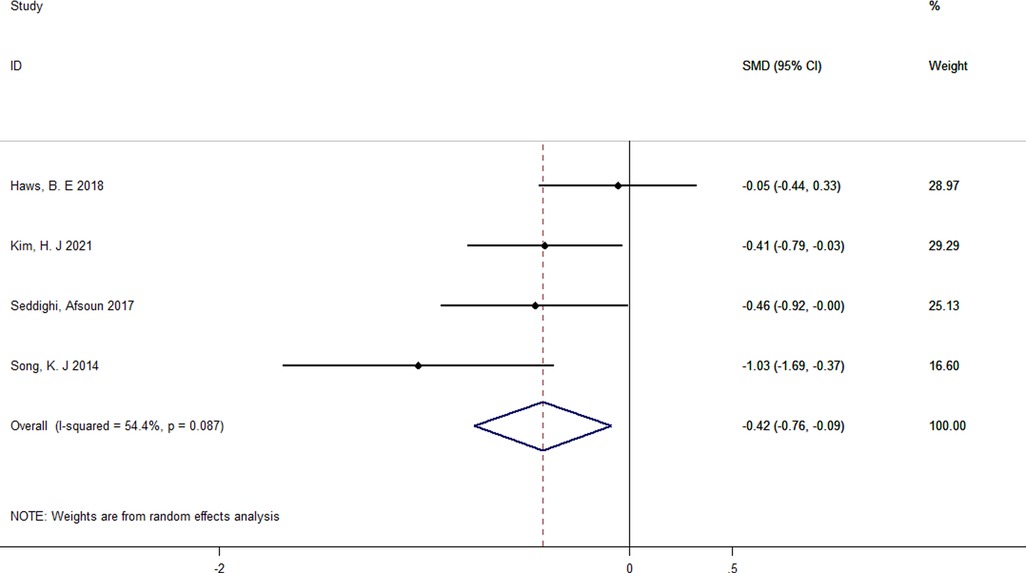
Length of hospital stay
Four studies reported the detailed length of hospital stay and were included (27, 30, 32, 33). A random-effect model was used because the heterogeneity across the three studies was high (I2 = 54.4%, p = 0.087). Pooled results demonstrated a significant reduction in the length of hospital stay compared with that in the control group (SMD = −0.42; 95% CI: −0.76 to −0.09) (Figure 9).
Subgroup analysis
We performed subgroup analyses by the route of administration (Local vs. Intravenous). Due to the limited number of included studies, we only have sufficient data exploring the effect of local and intravenous application of steroids on dysphagia rates at postoperative 1 day, VAS score at postoperative 1 day, fusion rate and operative time. There was no significant difference between intravenous and local steroid administration regarding dysphagia rates (Local: OR = 0.58, 95% CI: 0.12 to 2.88 vs. Intravenous: OR = 0.47, 95% CI: 0.26 to 0.84, p = 0.82, Figure 10), fusion rate (Local: OR = 0.88, 95% CI: 0.22 to 3.46 vs. Intravenous: OR = 0.87, 95% CI: 0.43 to 1.79, p = 1.00, Figure 11), and operation time (Local: WMD = −3.55, 95% CI: −7.29 to 0.19 vs. Intravenous: WMD = 1.65, 95% CI: −3.35 to 6.65, p = 0.10, Figure 12). However, there existed a significant difference between intravenous and local steroid administration regarding VAS score at postoperative 1 day (Local: WMD = −2.22, 95% CI: −3.03 to −1.42 vs. Intravenous: WMD = −0.10, 95% CI: −0.46 to 0.25, p < 0.001, Figure 13).
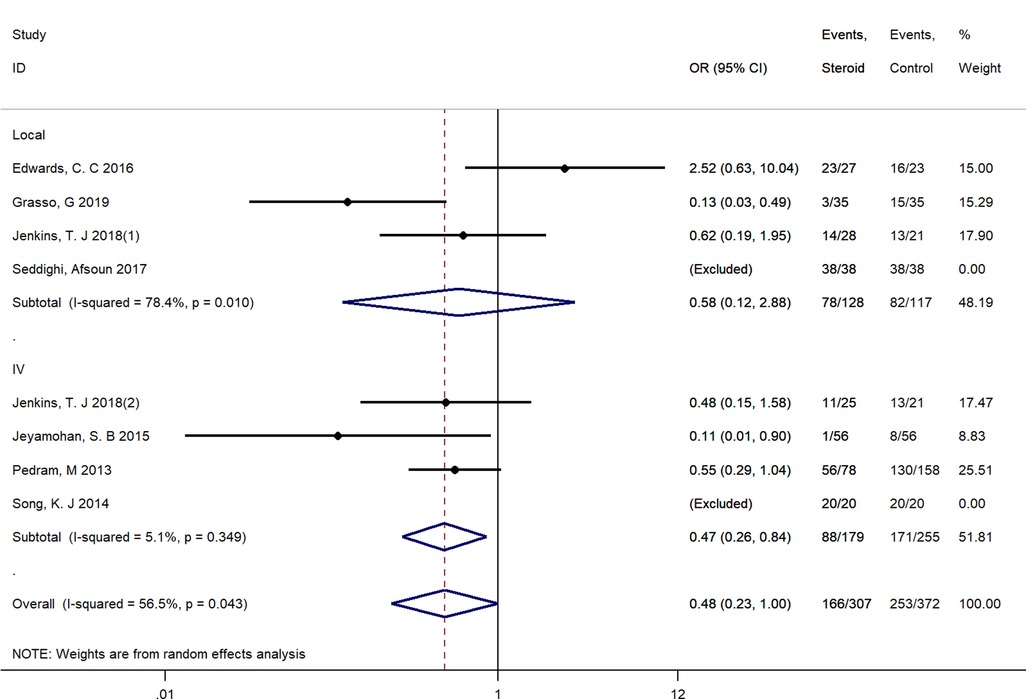
Figure 10. A subgroup analysis between intravenous and local steroid administration regarding dysphagia rates. IV, intravenous.
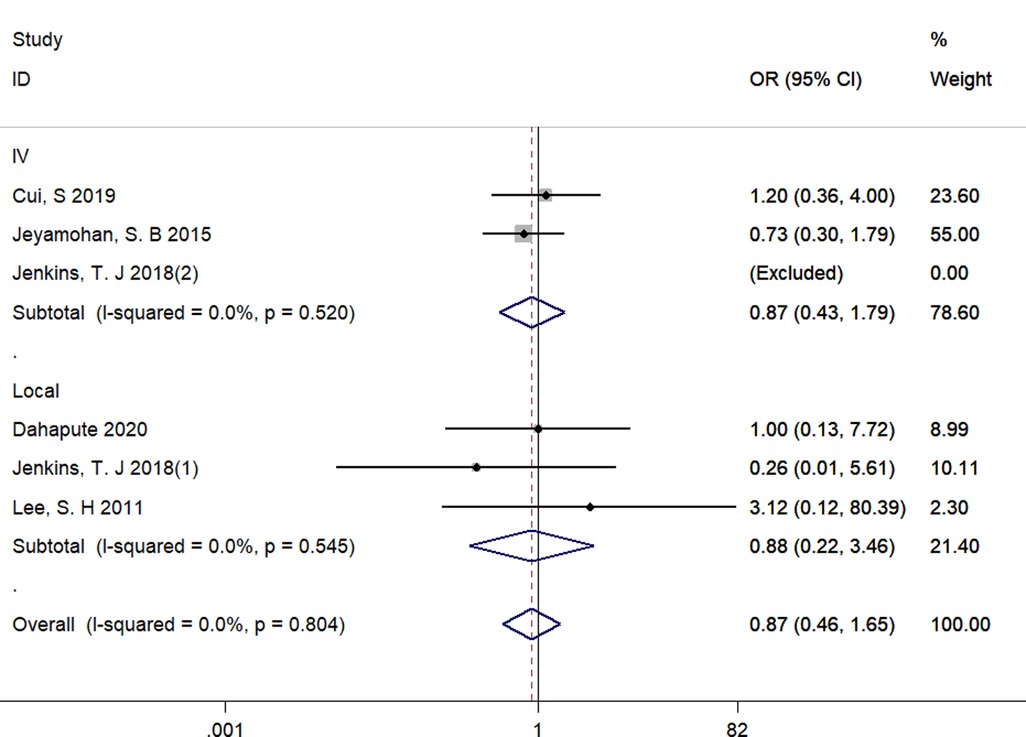
Figure 11. A subgroup analysis between intravenous and local steroid administration regarding fusion rates. IV, intravenous.
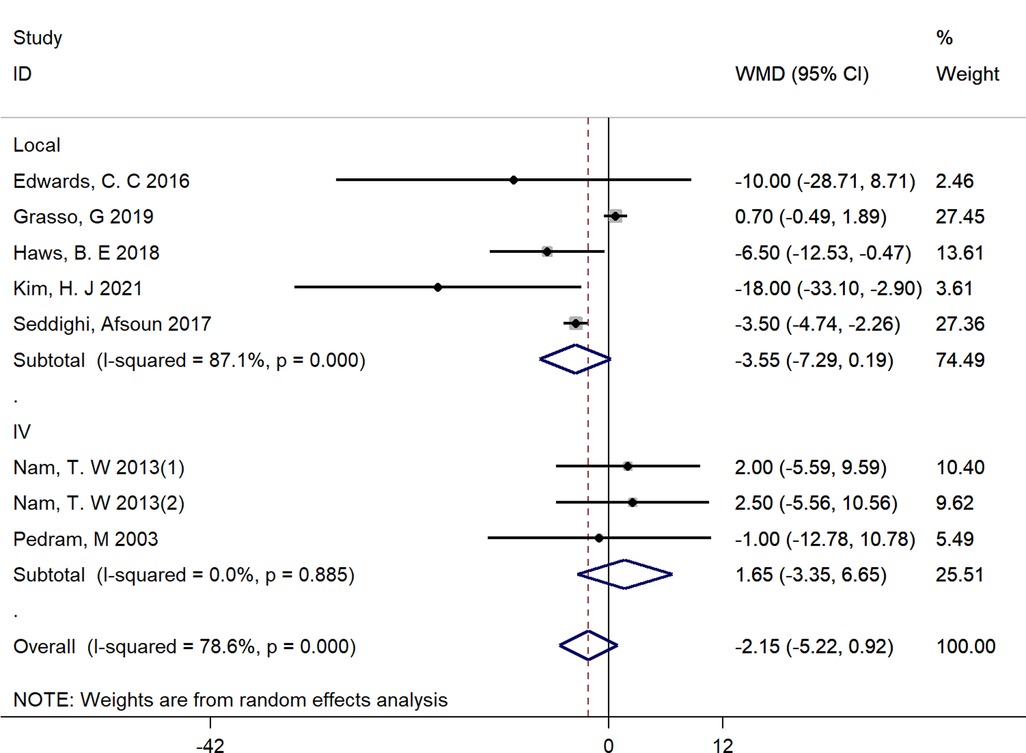
Figure 12. A subgroup analysis between intravenous and local steroid administration regarding operation time. IV, intravenous.
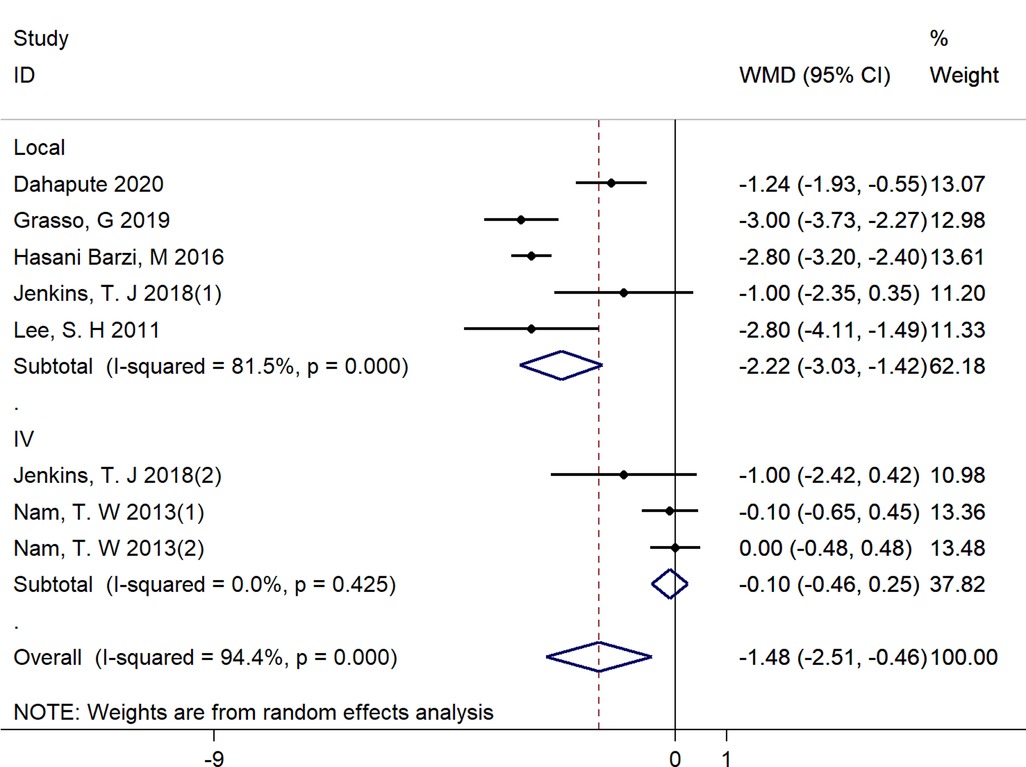
Figure 13. A subgroup analysis between intravenous and local steroid administration regarding VAS score at postoperative 1 day. IV, intravenous.
Sensitivity analyses and publication bias
Through the sensitivity analyses, we found that excluding studies one by one did not significantly alter the effect of steroid intervention on evaluation indicators. We did not perform the funnel plot to illustrate the publication bias of the primary outcome because less than 10 articles were included in quantitative analysis of a single outcome.
Discussion
Anterior cervical surgery has been wildly accepted as the gold standard surgical treatment for patients with cervical disc disease who failed conservative measures (34, 35). Despite the satisfactory clinical outcomes of anterior cervical surgery, up to 79% of patients experienced postoperative dysphagia. Our meta-analysis of 14 RCTs showed that perioperative steroid use could reduce the incidence and severity of dysphagia within 1 year after ACDF, reduce VAS scores within 2 weeks after surgery, and shorten the length of hospital stay without increasing operating time, VAS scores at 6 months and 1 year, and affecting fusion rates.
The principal findings of the present meta-analysis were consistent with those of the previous meta-analysis. Song et al. (36) performed a meta-analysis of six RCTs and two case-control studies and concluded that retropharyngeal steroid use could reduce dysphagia rate, severe dysphagia rate following anterior cervical surgery, without increasing operating time. A meta-analysis of seven RCTs conducted by Garcia et al. (37) concluded that patients treated with corticosteroids intravenously or locally had significantly decreased severity of dysphagia. Yu et al. (38) performed a meta-analysis of 8 RCTs and concluded that perioperative local retropharyngeal steroids could reduce the incidence and severity of dysphagia compared with placebo control. Nevertheless, obvious differences between our meta-analysis and the meta-analysis mentioned above should be taken into account. Most importantly, we dynamically investigated the effect of steroids on dysphagia rate and its severity at 1 day, 2 weeks, 3 months, 6 months, and 1 year after anterior cervical surgery. The above studies may have included too few studies and ignored time as an influencing factor, often taking the last follow-up as the endpoint event. Second, we exhaustively searched various databases with a standardized and detailed search strategy and finally included 14 RCTs of 1,181 patients. The overall risk of bias of the included studies was determined to be low. Third, we performed a subgroup analysis to investigate the effects of intravenous and local steroids. The results showed that there was no significant difference between intravenous and local steroid administration regarding dysphagia rates (p = 0.82), fusion rate (p = 1.00), and operative time (p = 0.10). However, the above studies did not quantitatively compare the efficacy of topical or intravenous administration of the steroids.
From our analysis, the incidence and severity of dysphagia significantly decreased with steroids within 1 year following anterior cervical surgery. Previous reviews have consistently reported the benefit of steroids on dysphagia and its severity. Zadegan et al. (39) reviewed 7 RCTs and 2 non-RCTs, and concluded that the incidence and severity of dysphagia was significantly lower in the steroid group. Cheng et al. (40) reviewed 3 RCTs and 2 retrospective cohort studies, and concluded that local corticosteroid application could reduce the incidence and severity of dysphagia following ACDF. Adenikinju et al. (41) reviewed 5 RCTs and 2 retrospective cohort studies, and concluded that patients received systemic and local steroids benefit from reductions in rate and severity of dysphagia postoperatively. However, our finding is a novelty because we performed a qualitative synthesis of RCTs and discuss dysphagia without the differences in time points. In our subgroup analysis, we only have sufficient data exploring the effect of local and intravenous application of steroids on dysphagia rates at postoperative 1 day and found that there was no significant difference between intravenous and local steroid administration regarding dysphagia rates. This is consistent with the findings from 1 previous systematic review that Garcia et al. (37) performed a high-quality meta-analysis of 7 RCTs and found that there was no significant difference between intravenous and local steroid administration. Further high-quality RCTs are needed to directly compare the effect of local and intravenous application of steroids on dysphagia and its severity.
Many spine surgeons worry that steroids negatively impact bony fusion rates and are reluctant to use steroids. Our results demonstrated that there was no difference in fusion rates at 1-year follow-up between the steroids group and control group, which were consistent with those of prior studies of perioperative steroids (18, 22, 29, 39, 41). Nevertheless, the steroids may hinder early fusion. Jeyamohan et al. (29) reported that fusion rates at 6 months proved to decrease in the steroid group but lost significance at 12 months. In addition, it should be taken into account that the definition of fusion was not the same in these five included studies. Cui et al. (22) considered fusion to be achieved if radiographs demonstrated <1 mm of interspinous motion between flexion and extension or if CT or MRI demonstrated clear evidence of bone bridging from end plate to end plate. Dahapute et al. (23) and Jenkins et al. (28) used a CT scan to confirm fusion without giving a detailed definition of fusion. Jeyamohan et al. (29) considered the spine was fused if bridging osseous trabeculae were observed spanning each operative level without any intervening radiographic lucencies. Similarly, Lee et al. (18) considered that the presence of bony extension into the space between the graft and the absence of segmental motion supported the fusion. Future studies with large sample sizes, uniform standards and longer follow-up time for bony fusion are needed to validate our findings.
Our results showed that a significant decrease regarding VAS score in the steroid group was observed compared with that in the control group in the short-term follow up. Previous studies have demonstrated the benefits of steroid use regarding to direct feelings calculated by the VAS at postoperative 2 weeks (18, 23, 25, 26, 28). In our included RCTs, Dahapute et al. (23) found that VAS score at postoperative 1 day and 2 weeks proved to decrease in the steroid group but lost significance at 2 months. Jenkins found that there existed a significant difference between steroids and control group regarding VAS score at postoperative 1 day and 2 weeks but lost significance at 3 months. Both support the short-term of benefits of steroids on VAS score. Considering the heterogeneity of the results obtained by our quantitative calculation of VAS, it is unsafe to conclude that steroids can reduce VAS score with such a good effect, but it can be inferred that the steroids have a short-term effect in terms of VAS score after surgery. In our subgroup analysis, there existed a significant difference between intravenous and local steroid administration regarding VAS score at postoperative 1 day (Local: WMD = −2.22, 95% CI: −3.03 to −1.42 vs. Intravenous: WMD = −0.10, 95% CI: −0.46 to 0.25). However, in an RCT conducted by Jenkins et al. (28), their results showed that there was no significant difference between intravenous and local steroid administration regarding VAS score. Additionally, when removing the study of Nam et al. (16), the findings for VAS score were consistent with previous analysis. We should interprete the finding with caution and look forward more high-quality RCTs that directly compare the effect of local and intravenous application of steroids VAS score.
In our series, we found that patients receiving steroids had shorter length of hospital stay compared to the control groups. This is consistent with the findings of previous studies (13, 15, 29, 33). This may be explained by the improved symptoms of dysphagia incidence and severity in the steroid group. Next, we investigated the effect of steroids on operation time and the results showed there was no significant difference between groups in operating time, which indicated that steroids do not increase the risk of prolonged surgery. In the included 7 RCTs that reported the detailed operation time, only Kim et al. (30) reported fewer operation time in steroid group compared with control group. It is possible that the operation time in their study was about twice as long as in the other studies, amplifying the effect of steroids on operation time.
Major concerns regarding the use of steroids are steroid-related complications. Despite the reported increased infection rate related with steroid application in general (42, 43), the present meta-analysis showed that there was no significantly increased risk of infections with steroid use in any of the included studies. Esophageal perforation is one of the most dreadful complications of ACDF with an incidence of 0.02%–1.52% (44). Lee et al. (45) cautioned that esophageal perforation was a potential complication of local perioperative steroids in the late post-operative period of ACDF. However, this complication was not reported in any of the included studies. Actually, the two cases reported in the literature of esophageal perforation were both on chronic steroids, therefore, it is uncertain whether the esophageal perforation was directly associated with perioperative steroids. Taken together, steroids application does not increase the risk of early potential complications, but future studies are still necessary to evaluate the potential long-term complication associated with steroids administration.
The current meta-analysis observed some limitations. First, various doses and steroid types were adopted in the included studies, exact dose and type of steroid for desired effect on incidence and severity of dysphagia remains unclear. Though we performed a subgroup analysis by the route of administration (Local vs. Intravenous), it is still insufficient to account for a long-term effect of local and intravenous steroids on dysphagia. Second, even though we included 14 RCTs, only a few were used for quantitative analysis when comparing a specific outcome. This is due to differences in the way dysphagia was assessed and the variety of outcomes reported between studies. Finally, the number of fusion levels also varied across studies, exposing patients to different risks and potentially leading to different responses to interventions. In addition, the Grade results qualities of VAS were low, and dysphagia event, Bazaz stratification of severity of dysphagia, fusion rate, operation time and length of hospital stay were moderate. None of high quality evidence was found in above outcomes. Therefore, further high-quality studies are required to determine which subpopulations are most likely to benefit or not, and more individualized treatment is needed.
Conclusion
The current meta-analysis demonstrates the benefits of perioperative steroid administration in anterior cervical surgery without increasing the risk of early potential complications. Future high-quality RCTs are warranted to recommend the administration of steroids in anterior cervical surgery.
Author contributions
XZ and HL: designed the study. XZ, YY and Y-WS: searched and screened relevant literature. K-RZ, and L-TM: data collection. XZ and YY: completed the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (grant number 82172522) and the Chengdu Science and Technology Program (grant number 2021-YF05-00436-SN).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.1040166/full#supplementary-material.
References
1. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. (1958) 15(6):602–17. doi: 10.3171/jns.1958.15.6.0602
2. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. (1958) 40-a(3):607–24. doi: 10.2106/00004623-195840030-00009
3. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine. (2007) 32(21):2310–7. doi: 10.1097/BRS.0b013e318154c57e
4. Frempong-Boadu A, Houten JK, Osborn B, Opulencia J, Kells L, Guida DD, et al. Swallowing and speech dysfunction in patients undergoing anterior cervical discectomy and fusion: a prospective, objective preoperative and postoperative assessment. J Spinal Disord Tech. (2002) 15(5):362–8. doi: 10.1097/00024720-200210000-00004
5. Vaishnav AS, Saville P, McAnany S, Patel D, Haws B, Khechen B, et al. Predictive factors of postoperative dysphagia in single-level anterior cervical discectomy and fusion. Spine. (2019) 44(7):e400–7. doi: 10.1097/BRS.0000000000002865
6. Tasiou A, Giannis T, Brotis AG, Siasios I, Georgiadis I, Gatos H, et al. Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg. (2017) 3(3):444–59. doi: 10.21037/jss.2017.08.03
7. Starmer HM, Riley LH 3rd, Hillel AT, Akst LM, Best SR, Gourin CG. Dysphagia, short-term outcomes, and cost of care after anterior cervical disc surgery. Dysphagia. (2014) 29(1):68–77. doi: 10.1007/s00455-013-9482-9
8. Riley LH 3rd, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG. Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine. (2005) 30(22):2564–9. doi: 10.1097/01.brs.0000186317.86379.02
9. Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine. (2002) 27(22):2453–8. doi: 10.1097/00007632-200211150-00007
10. Ratnaraj J, Todorov A, McHugh T, Cheng MA, Lauryssen C. Effects of decreasing endotracheal tube cuff pressures during neck retraction for anterior cervical spine surgery. J Neurosurg. (2002) 97(2 Suppl):176–9. doi: 10.3171/spi.2002.97.2.0176
11. Chin KR, Eiszner JR, Adams SB Jr. Role of plate thickness as a cause of dysphagia after anterior cervical fusion. Spine. (2007) 32(23):2585–90. doi: 10.1097/BRS.0b013e318158dec8
12. Gandhi SD, Wahlmeier ST, Louie P, Sauber R, Tooley TR, Baker KC, et al. Effect of local retropharyngeal steroids on fusion rate after anterior cervical discectomy and fusion. Spine J. (2020) 20(2):261–5. doi: 10.1016/j.spinee.2019.08.018
13. Koreckij TD, Davidson AA, Baker KC, Park DK. Retropharyngeal steroids and dysphagia following multilevel anterior cervical surgery. Spine. (2016) 41(9):E530–534. doi: 10.1097/BRS.0000000000001293
14. Schroeder J, Weinstein J, Salzmann SN, Kueper J, Shue J, Sama AA, et al. Effect of steroid-soaked gelatin sponge on soft tissue swelling following anterior cervical discectomy and fusion: a radiographic analysis. Asian Spine J. (2018) 12(4):656–61. doi: 10.31616/asj.2018.12.4.656
15. Cancienne JM, Werner BC, Loeb AE, Yang SS, Hassanzadeh H, Singla A, et al. The effect of local intraoperative steroid administration on the rate of postoperative dysphagia following ACDF: a study of 245,754 patients. Spine. (2016) 41(13):1084–8. doi: 10.1097/BRS.0000000000001407
16. Nam TW, Lee DH, Shin JK, Goh TS, Lee JS. Effect of intravenous dexamethasone on prevertebral soft tissue swelling after anterior cervical discectomy and fusion. Acta Orthop Belg. (2013) 79(2):211–5.23821974
17. van Eck CF, Regan C, Donaldson WF, Kang JD, Lee JY. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion: a study of 672 consecutive patients. Spine. (2014) 39(26):2143–7. doi: 10.1097/BRS.0000000000000636
18. Lee SH, Kim KT, Suk KS, Park KJ, Oh KI. Effect of retropharyngeal steroid on prevertebral soft tissue swelling following anterior cervical discectomy and fusion: a prospective, randomized study. Spine. (2011) 36(26):2286–92. doi: 10.1097/BRS.0b013e318237e5d0
19. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J. (2009) 339:b2700. doi: 10.1136/bmj.b2700
20. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions version 6.3. (2022). Cochrane. (2022). Available at: www.training.cochrane.org/handbook.
21. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. (2003) 327(7414):557–60. doi: 10.1136/bmj.327.7414.557
22. Cui S, Daffner SD, France JC, Emery SE. The effects of perioperative corticosteroids on dysphagia following surgical procedures involving the anterior cervical spine: a prospective, randomized, controlled, double-blinded clinical trial. J Bone Joint Surg Am. (2019) 101(22):2007–14. doi: 10.2106/JBJS.19.00198
23. Dahapute A, Sonone S, Bhaladhare S, Sakhare K, Marathe N, Balasubramanian SG, et al. Prospective randomized controlled trial to study the effect of local steroids in the retropharyngeal space after anterior cervical discectomy and fusion. Global Spine J. (2021) 11(6):826–32. doi: 10.1177/2192568220925782
24. Edwards CC, Dean C, Phillips D, Blight A. Can dysphagia following anterior cervical fusions with rhBMP-2 be reduced with local depomedrol application? A prospective, randomized, placebo-controlled, double-blind trial. Spine. (2016) 41(7):555–62. doi: 10.1097/BRS.0000000000001284
25. Grasso G, Leone L, Torregrossa F. Dysphagia prevention in anterior cervical discectomy surgery: results from a prospective clinical study. World Neurosurg. (2019) 125:e1176–82. doi: 10.1016/j.wneu.2019.01.273
26. Hasani BM, Nikoobakht M, Hasani BN, Khanali F, Yazdi Z. The effect of local steroid injection on prevertebral soft tissue swelling after anterior cervical discectomy and fusion. J Babol Univ Medical Sci. (2016) 18(10):7–12.
27. Haws BE, Khechen B, Narain AS, Hijji FY, Bohl DD, Massel DH, et al. Impact of local steroid application on dysphagia following an anterior cervical discectomy and fusion: results of a prospective, randomized single-blind trial. J Neurosurg Spine. (2018) 29(1):10–7. doi: 10.3171/2017.11.SPINE17819
28. Jenkins TJ, Nair R, Bhatt S, Rosenthal BD, Savage JW, Hsu WK, et al. The effect of local versus intravenous corticosteroids on the likelihood of dysphagia and dysphonia following anterior cervical discectomy and fusion: a single-blinded, prospective, randomized controlled trial. J Bone Joint Surg Am. (2018) 100(17):1461–72. doi: 10.2106/JBJS.17.01540
29. Jeyamohan SB, Kenning TJ, Petronis KA, Feustel PJ, Drazin D, DiRisio DJ. Effect of steroid use in anterior cervical discectomy and fusion: a randomized controlled trial. J Neurosurg Spine. (2015) 23(2):137–43. doi: 10.3171/2014.12.SPINE14477
30. Kim HJ, Alluri R, Stein D, Lebl D, Huang RS, Lafage R, et al. Effect of topical steroid on swallowing following ACDF results of a prospective double-blind randomized control trial. Spine. (2021) 46(7):413–20. doi: 10.1097/BRS.0000000000003825
31. Pedram M, Castagnera L, Carat X, Macouillard G, Vital JM. Pharyngolaryngeal lesions in patients undergoing cervical spine surgery through the anterior approach: contribution of methylprednisolone. Eur Spine J. (2003) 12(1):84–90. doi: 10.1007/s00586-002-0495-6
32. Seddighi A, Nikouei A, Seddighi AS, Arjmand Y. Effect of local steroid injection on prevertebral soft tissue swelling following anterior cervical discectomy and fusion. Int Clin Neurosci J. (2017) 4(3):84–90. doi: 10.22037/icnj.v4i3.18461
33. Song KJ, Lee SK, Ko JH, Yoo MJ, Kim DY, Lee KB. The clinical efficacy of short-term steroid treatment in multilevel anterior cervical arthrodesis. Spine J. (2014) 14(12):2954–8. doi: 10.1016/j.spinee.2014.06.005
34. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. (1993) 75(9):1298–307. doi: 10.2106/00004623-199309000-00005
35. Emery SE, Bohlman HH, Bolesta MJ, Jones PK. Anterior cervical decompression and arthrodesis for the treatment of cervical spondylotic myelopathy. Two to seventeen-year follow-up. J Bone Joint Surg Am. (1998) 80(7):941–51. doi: 10.2106/00004623-199807000-00002
36. Song J, Yi P, Wang Y, Gong L, Sun Y, Yang F, et al. The retropharyngeal steroid use during operation on the fusion rate and dysphagia after ACDF? A systematic review and meta-analysis. Eur Spine J. (2022) 31(2):288–300. doi: 10.1007/s00586-021-06727-1
37. Garcia S, Schaffer NE, Wallace N, Butt BB, Gagnier J, Aleem IS. Perioperative corticosteroids reduce dysphagia severity following anterior cervical spinal fusion: a meta-analysis of randomized controlled trials. J Bone Joint Surg Am. (2021) 103(9):821–8. doi: 10.2106/JBJS.20.01756
38. Yu H, Dong H, Ruan B, Xu X, Wang Y. Intraoperative use of topical retropharyngeal steroids for dysphagia after anterior cervical fusion: a systematic review and meta-analysis. Dis Markers. (2021) 2021:7115254. doi: 10.1155/2021/7115254
39. Zadegan SA, Jazayeri SB, Abedi A, Bonaki HN, Vaccaro AR, Rahimi-Movaghar V. Corticosteroid administration to prevent complications of anterior cervical spine fusion: a systematic review. Global Spine J. (2018) 8(3):286–302. doi: 10.1177/2192568217708776
40. Cheng L, Guan J, Zhang C, Ma L, Yao Q, Wang K, et al. The effect of local intraoperative corticosteroid application on postoperative dysphagia following anterior cervical spine surgery. Neurosurg Rev. (2022) 45(1):63–70. doi: 10.1007/s10143-019-01207-z
41. Adenikinju AS, Halani SH, Rindler RS, Gary MF, Michael KW, Ahmad FU. Effect of perioperative steroids on dysphagia after anterior cervical spine surgery: a systematic review. Int J Spine Surg. (2017) 11(2):9. doi: 10.14444/4009
42. Anstead GM. Steroids, retinoids, and wound healing. Adv Wound Care. (1998) 11(6):277–85.10326344
43. Scanzello CR, Figgie MP, Nestor BJ, Goodman SM. Perioperative management of medications used in the treatment of rheumatoid arthritis. HSS J. (2006) 2(2):141–7. doi: 10.1007/s11420-006-9012-5
44. Halani SH, Baum GR, Riley JP, Pradilla G, Refai D, Rodts GE Jr, et al. Esophageal perforation after anterior cervical spine surgery: a systematic review of the literature. J Neurosurg Spine. (2016) 25(3):285–91. doi: 10.3171/2016.1.SPINE15898
Keywords: steroid, dysphagia, anterior cervical spine surgery, rct, meta-analysis steroid, meta-analysis introduction
Citation: Zhang X, Yang Y, Shen Y, Zhang K, Ma L and Liu H (2022) Effect of perioperative steroids application on dysphagia, fusion rate, and visual analogue scale (VAS) following anterior cervical spine surgery: A meta-analysis of 14 randomized controlled trials (RCTs). Front. Surg. 9:1040166. doi: 10.3389/fsurg.2022.1040166
Received: 9 September 2022; Accepted: 3 October 2022;
Published: 1 November 2022.
Edited by:
Jason Pui Yin Cheung, The University of Hong Kong, Hong Kong, SAR ChinaReviewed by:
Siddharth Chavali, AIG Hospitals, IndiaHui Dong, Northern Jiangsu People's Hospital (NJPH), China
© 2022 Zhang, Yang, Shen, Zhang, Ma and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Liu bGl1aGFvNjMwNEAxMjYuY29t
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Xiang Zhang†
Xiang Zhang† Yi-Wei Shen
Yi-Wei Shen Hao Liu
Hao Liu