- 1Department of Urology, the First College of Clinical Medical Science, China Three Gorges University, Yichang Central People's Hospital, Yichang, China
- 2Department of Urology, Yidu People's Hospital, Yichang, China
- 3Department of Intensive Care Unit, the First College of Clinical Medical Science, China Three Gorges University, Yichang Central People's Hospital, Yichang, China
- 4Department of Urology, Peking University First Hospital, Institute of Urology, Peking University, National Urological Cancer Center, Beijing, China
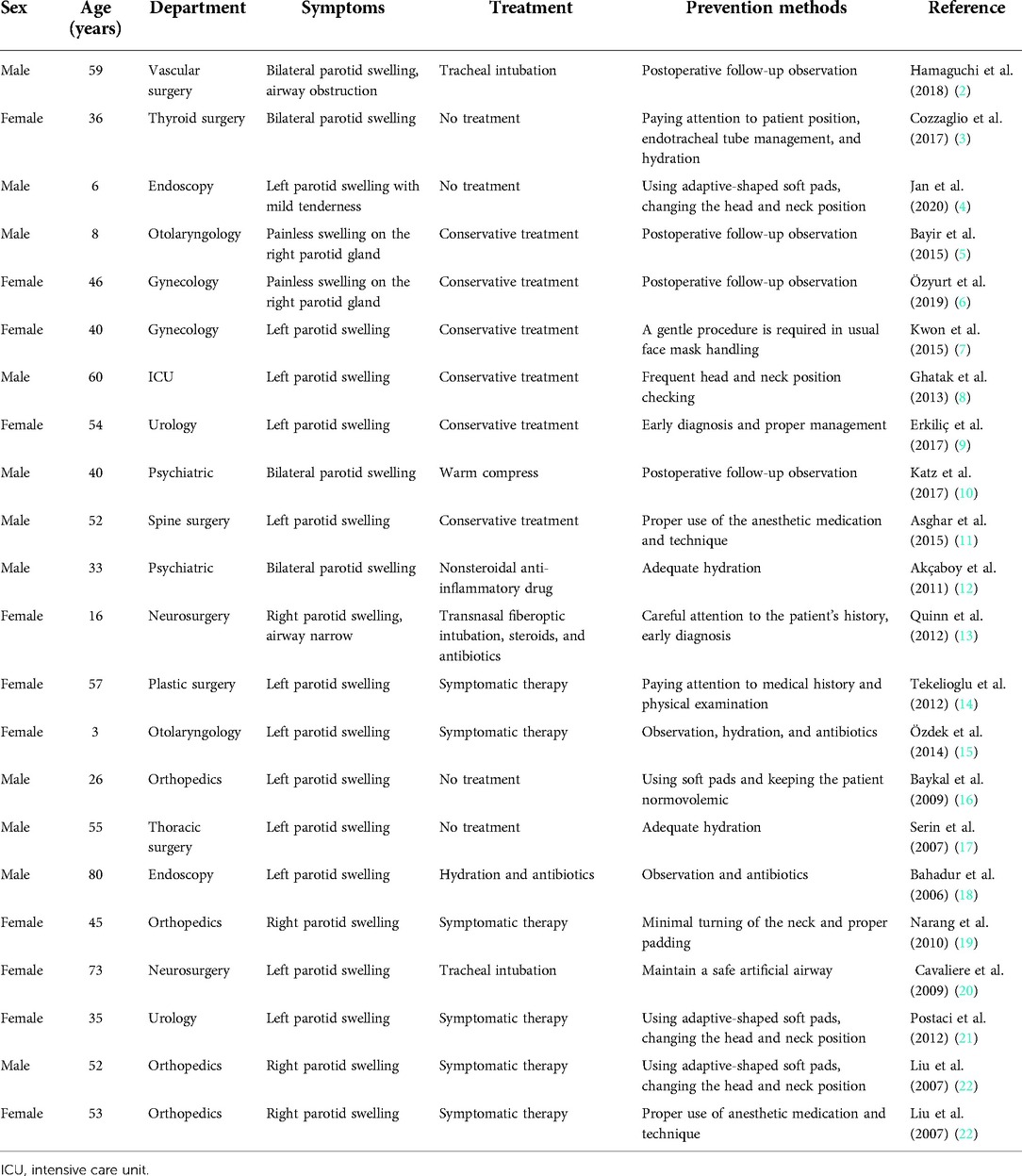
Anesthesia mumps have rarely been reported. This article presents the diagnosis and treatment of a case of anesthesia mumps with airway obstruction in the urology department and reviews previous cases of the disease. A 58-year-old man had a history of hypertension and diabetes, and his blood pressure and glucose levels were well controlled. He underwent laparoscopic radical nephrectomy for a right renal tumor. Postoperatively, a swelling of approximately 5 × 4 cm was observed in the left parotid region and left eyelid, no palpable crepitation was detected, and the skin overlying the left parotid gland was mildly hyperemic and tender. Enhanced computed tomography of the head and neck revealed obvious swelling of the laryngopharyngeal airway, and electronic laryngoscopy showed narrow airway. Laboratory test results including white blood cell count, C-reactive protein, serum amylase, and lipase levels were normal. Glycosylated hemoglobin level was 6.8%, and the salivary culture from Stensen's duct was negative. The patient was managed with endotracheal intubation and a ventilator to maintain breathing along with anti-infection, expectorant, and symptomatic treatment. The swelling in the left parotid gland gradually resolved without recurrence, and the patient was extubated on the 7th postoperative day. In this case, the pathophysiology of anesthesia mumps may have been related to the incorrect positioning of the thick short neck and the use of a head ring, which can result in the squeezing of vessels. In most cases, the salivary gland swelling resolves with observation and symptomatic treatment. In patients with anesthesia mumps, emergency airway management and careful observation are necessary if upper airway obstruction occurs. This case report should increase awareness of anesthesia mumps and its complications among anesthesiologists, surgeons, and postoperative caregivers.
Introduction
Transient inflammation and swelling of the salivary glands is a rare complication after general or epidural anesthesia and is defined as anesthesia mumps (1). It is usually benign and can develop during surgery or, more commonly, a few hours postoperatively, and usually resolves without sequelae within few days. In rare cases, it can lead to severe symptoms that require emergency intervention (2). Anesthesia mumps has been reported after various surgical procedures (2–22) (Table 1). Herein, we report a case of anesthesia mumps, which involved the left parotid gland and caused severe facial edema and airway stenosis, after laparoscopic radical nephrectomy in the urology department.
Case report
A 58-year-old man underwent laparoscopic radical nephrectomy for a right renal tumor in the urology department. The patient had a history of hypertension for 3 years and type 2 diabetes for 17 years, and his blood pressure and glucose levels were well controlled. The patient's body mass index (BMI) was 32.1.
In the 2nd day after admission, the patient underwent laparoscopic radical right nephrectomy under general anesthesia. Anesthesia was induced using propofol (2 mg/kg) and fentanyl (1 µg/kg). Endotracheal intubation (internal diameter 8 mm) was performed after muscle relaxation with vecuronium (0.1 mg/kg), and sevoflurane (1MAC) was used for anesthesia maintenance. The patient was placed in the left lateral position with his head on a soft gel pad, and with the waist as the fulcrum, the patient's lower limbs and head were lowered by 20° each. The surgical time was 5 h and 47 min.
Shortly after the patient was shifted to the anesthesia recovery room, a swelling of approximately 5 × 4 cm was observed in the left parotid region, while the body temperature remained normal. The facial swelling was further aggravated at 3 h postoperatively; swelling was found on the left eyelid and forehead (Figure 1A), and the overlying skin of the left parotid gland area was mildly hyperemic and tender. However, no crepitation on palpation was detected. Enhanced computed tomography (CT) of the head and neck showed obvious swelling of the soft tissue from the left periorbital area to the left submandibular region. The swelling involved the left parapharyngeal space, uvula, oropharynx, epiglottis, and laryngopharyngeal airway (Figures 1B,C). Electronic laryngoscopy showed edema in the left lateral pharyngeal wall, epiglottis, and supraglottic tissue, and the glottis was partially obscured. The patient developed shortness of breath 5 h postoperatively. Considering upper airway obstruction, emergency endotracheal intubation was performed, and the patient was transferred to the intensive care unit for monitoring and treatment.
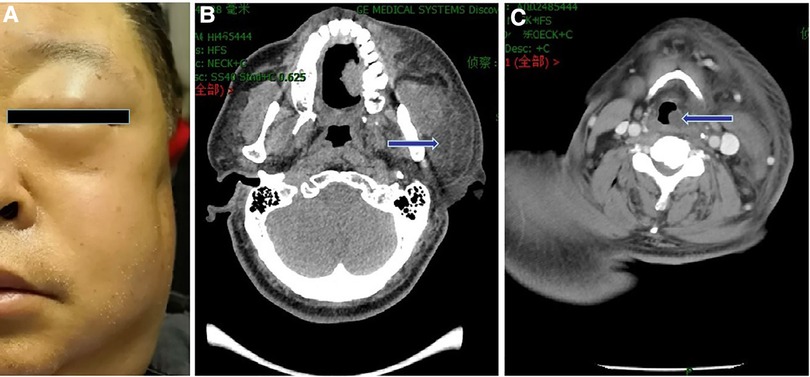
Figure 1. Clinical appearance and imaging findings of the patient. (A) Photograph of the patient showing swelling of the left eyelid and parotid gland area. (B) Enhanced CT image showing significant enlargement of the left submandibular soft tissue and parotid gland (arrow). (C) Enhanced CT image showing the involvement of the left parapharyngeal space and airway stenosis (arrow).
Laboratory examination revealed a normal white blood cell count; C-reactive protein, serum amylase, and lipase levels were normal; glycosylated hemoglobin level was 6.8%; salivary culture of Stensen's duct was negative; and the pathological diagnosis of the tumor specimens was renal cell carcinoma.
The patient was diagnosed as anesthesia mumps and treated with endotracheal intubation and a ventilator to maintain his breathing, along with anti-infection treatment, an expectorant, and blood glucose control. Repeat CT 4 days postoperatively showed resolution of the swelling in left temporal, facial, and cervical soft tissue and parapharyngeal space. Laryngoscopy confirmed the absence of redness or swelling of the nasopharynx, oropharynx, laryngopharynx, or epiglottis, and no airway obstruction was observed. The swelling left parotid gland gradually resolved without recurrence within 7 days postoperatively, and the patient was extubated without incident.
Discussion
The etiology of parotid gland enlargement is complex and varied (1). Anesthesia mumps is an acute swelling of the unilateral or bilateral parotid glands after surgery (7), which was first described in 1960, and its incidence has been reported to be 0.16%–0.2% (23). The exact pathophysiology of anesthesia mumps is not clear, and many factors are thought to play a role. First, the loss of muscle tone caused by muscle relaxants and positive pressure mask ventilation during anesthesia is considered a factor. During recovery from general anesthesia, the significant increase in positive pressure in the mouth due to nervousness, coughing, and sneezing while the patient is still receiving positive pressure ventilation facilitates the retrograde passage of air through Stenson's ducts into the parotid gland (1). Second, the perioperative use of anticholinergics, phenothiazines, antihistamines, barbiturates, beta-blockers, and preoperative dehydration may be inducing factors. This can lead to obstruction of the salivary ducts by reducing salivary secretion and increasing the viscosity of secretions (19). Third, Mandel and Surattanont believed that activation of the pharyngeal reflex stimulates the parasympathetic nervous system, which in turn leads to vasodilation and hyperemia in the parotid gland (24). Another possible explanation is that the patient's parotid canal becomes blocked due to overrotation of the head and compression of the parotid gland during long periods of surgery (7). In addition, some medical conditions, such as diabetes, hypothyroidism, hepatorenal failure, Sjogren's syndrome, depression, and malnutrition, also increase the risk of anesthesia mumps (25).
In our patient, transient parotid secretion obstruction due to dehydration was not considered a possible cause of swelling as good intraoperative hydration was ensured. Moreover, the patient had no history of parotid or salivary calculi, or neck masses, and excretory duct obstruction was ruled out as CT confirmed the absence of calculi, air, or duct dilation. Bacterial parotitis was excluded due to normal infection indicators, and no purulent discharge was observed from Stenson's duct orifice. Adverse drug reactions were also less likely as the patient's body temperature and eosinophil count were normal, and no skin rash was observed. Furthermore, drugs related to parotid swelling were not administered during anesthesia. Therefore, this condition may have occurred due to the compression of vessels owing to the short, thick neck of the obese patient, which affected perfusion of the area supplied, leading to anesthesia mumps. The involved salivary gland was on the side of the face that was pressed against the operating table, and the swelling may be associated with prolonged surgery. In obese patients, the lateral decubitus position may cause venous congestion due to twisting of veins and/or gland ischemia due to compression of the arteries. Venous congestion can explain immediate facial swelling after surgery, and ischemic salivary glands usually present with unilateral swelling and pain. Depending on the degree of swelling, pain can vary from mild and bearable to unbearable (26). In this case, the use of a head ring and extreme neck extension may be the reasons for the development of anesthesia mumps.
Previous reports have shown that in the majority of cases, anesthesia mumps resolved spontaneously in the short term. In many patients, undetected anesthesia mumps resolved without any treatment, while in some cases, hydration and symptomatic treatment were sufficient to treat mumps (24). However, our patient developed severe airway obstruction, and tracheal intubation was performed. No case of anesthesia mumps with airway stenosis has been previously reported following urological surgery. Emergency tracheostomy may be an option if intubation is difficult (27); however, it is difficult to identify the location of tracheostomy in obese patients with a short neck or neck swelling.
Several measures have been proposed to prevent the occurrence of anesthesia mumps, include reducing or avoiding the use of anticholinergic drugs prior to surgery, smoothing intubation and extubation to avoid mechanical irritation, and maintaining optimal hydration during surgery (8). In the present case, a properly shaped soft pad to avoid direct compression of the parotid gland and ducts, and a tension-free head and neck position to maintain normal blood circulation might have prevented the development of anesthesia mumps.
Conclusion
In summary, anesthesia mumps is a rare complication following urological surgery. It is usually noticed in the recovery room, and surgeons, anesthesiologists, and postoperative caregivers should be aware of this complication. It is important to pay attention to patients with predisposing conditions, such as obesity and diabetes, placed in the lateral or prone positions during long surgeries. Particular attention should be paid to the endotracheal tube insertion and removal and rehydration therapy. When anesthesia mumps with airway obstruction occurs, it is necessary to inform the patient of the condition and take appropriate treatment measures in a timely manner.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZD and XL conceived the paper's objective and collected the patient's data. ZL and LZ analyzed the data and performed reference search. WL and LY drafted and revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hans P, Demoitié J, Collignon L, Bex V, Bonhomme V. Acute bilateral submandibular swelling following surgery in prone position. Eur J Anaesthesiol. (2006) 23:83–4. doi: 10.1017/S0265021505231824
2. Hamaguchi T, Suzuki N, Kondo I. A case of anesthesia mumps that required postoperative re-intubation. JA Clin Rep. (2018) 4:22. doi: 10.1186/s40981-018-0159-0
3. Cozzaglio L, Pizzocaro A, Cancellieri F. Anesthesia mumps after thyroidectomy. J Endocrinol Invest. (2017) 40:335–6. doi: 10.1007/s40618-016-0598-2.28000179
4. Jan R, Alshuaibi KM, Rehman IU, Bithal PK. Acute transient sialadenitis—“anesthesia mumps:” case report and review of literature. Anesth Essays Res. (2020) 14:352–4. doi: 10.4103/aer.AER_80_20
5. Bayir H, Yildiz I, Sereflican M, Yoldas H, Demirhan A, Kurt AD. A pediatric case of anesthesia mumps after general anesthesia. J Res Med Sci. (2015) 20:1123–4. doi: 10.4103/1735-1995.172851
6. Özyurt E, Ekin Sarı GE, Doğan S. Acute unilateral swelling of parotid gland after general anesthesia: anesthesia mumps. Balk Med J. (2019) 36:363. doi: 10.4274/balkanmedj.galenos.2019.2019.6.103
7. Kwon SY, Kang YJ, Seo KH, Kim Y. Acute unilateral anesthesia mumps after hysteroscopic surgery under general anesthesia: a case report. Korean J Anesthesiol. (2015) 68:300–3. doi: 10.4097/kjae.2015.68.3.300
8. Ghatak T, Gurjar M, Samanta S, Baronia AK. A case of “anesthesia mumps” from ICU. Saudi J Anaesth. (2013) 7:222–3. doi: 10.4103/1658-354X.114067
9. Erkiliç E, Kesimci E, Yüngül A, Alaybeyoğlu F, Aksoy M. A complication after percutaneous nephrolithotomy: anesthesia mumps. Anesth Essays Res. (2017) 11:794–6. doi: 10.4103/0259-1162.204203
10. Katz RB, Helgeson L, Ostroff R. A case of anesthesia mumps with electroconvulsive therapy. J ECT. (2017) 33:e6. doi: 10.1097/YCT.0000000000000370
11. Asghar A, Karam K, Rashid S. A case of anesthesia mumps after sacral laminectomy under general anesthesia. Saudi J Anaesth. (2015) 9:332–3. doi: 10.4103/1658-354X.154743
12. Akçaboy EY, Akçaboy ZN, Alkan H, Gogus N. “Anesthesia mumps” after electroconvulsive therapy anesthesia. J ECT. (2011) 27:e21–2. doi: 10.1097/YCT.0b013e3181df4ed0
13. Quinn ME, Quinn TDM, Mian AZ, Sakai O. Imaging findings of “anesthesia mumps” (acute postoperative sialadenitis) after general anesthesia. J Comput Assist Tomogr. (2012) 36:745–8. doi: 10.1097/RCT.0b013e318268ec47
14. Tekelioglu UY, Akkaya A, Apuhan T, Demirhan A, Bayır H, Kocoglu H. A case of anesthesia mumps after general anesthesia. J Anesth. (2012) 26:130–1. doi: 10.1007/s00540-011-1255-8
15. Özdek A, Bayır Ö, Işık ME, Tatar EÇ, Saylam G, Korkmaz H. Anesthesia mumps resulting in temporary facial nerve paralysis after the auditory brainstem implantation in a 3-year-old child. Int J Pediatr Otorhinolaryngol. (2014) 78:159–62. doi: 10.1016/j.ijporl.2013.09.030
16. Baykal M, Karapolat S. A case of anesthesia mumps after general anesthesia. Acta Anaesthesiol Scand. (2009) 53:138. doi: 10.1111/j.1399-6576.2008.01809.x
17. Serin S, Kaya S, Kara CO, Baser S. A case of anesthesia mumps. Anesth Analg. (2007) 104:1005. doi: 10.1213/01.ane.0000258824.59125.f8
18. Bahadur S, Fayyaz M, Mehboob S. Salivary gland swelling developing after endoscopy: “anesthesia mumps”. Gastrointest Endosc. (2006) 63:345–7. doi: 10.1016/j.gie.2005.09.008
19. Narang D, Trikha A, Chandralekha C. Anesthesia mumps and morbid obesity. Acta Anaesthesiol Belg. (2010) 61:83–5. PMID: 21155444
20. Cavaliere F, Conti G, Annetta MG, Greco A, Cina A, Proietti R. Massive facial edema and airway obstruction secondary to acute postoperative sialadenitis or “anesthesia mumps”: a case report. J Med Case Rep. (2009) 3:7073. doi: 10.1186/1752-1947-3-7073
21. Postaci A, Aytac I, Oztekin CV, Dikmen B. Acute unilateral parotid gland swelling after lateral decubitus position under general anesthesia. Saudi J Anaesth. (2012) 6:295–7. doi: 10.4103/1658-354X.101227
22. Liu FC, Liou JT, Li AH, Chiou H, Day YJ. Acute unilateral parotid glands enlargement following endotracheal general anesthesia: report of two cases. Chang Gung Med J. (2007) 30:453–7. PMID: 18062177
23. Rosique MJF, Rosique RG, Costa IR, Lara BR, Figueiredo JLF, Ribeiro DGB. Parotitis after epidural anesthesia in plastic surgery: report of three cases. Aesthet Plast Surg. (2013) 37:838–42. doi: 10.1007/s00266-013-0112-6
24. Mandel L, Surattanont F. Bilateral parotid swelling: a review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. (2002) 93:221–37. doi: 10.1067/moe.2002.121163
25. Raad II, Sabbagh MF, Caranasos GJ II. Acute bacterial sialadenitis: a study of 29 cases and review. Rev Infect Dis. (1990) 12:591–601. doi: 10.1093/clinids/12.4.591
26. Berker M, Sahin A, Aypar U, Ozgen T. Acute parotitis following sitting position neurosurgical procedures: review of five cases. J Neurosurg Anesthesiol. (2004) 16:29–31. doi: 10.1097/00008506-200401000-00007
Keywords: postoperative care, radical nephrectomy, sialadenitis, anesthesia mumps, airway obstruction
Citation: Li W, Liao Z, Yao L, Zhang L, Li X and Dong Z (2023) Anesthesia mumps with airway obstruction after radical nephrectomy: A case report and literature review. Front. Surg. 9:1039362. doi: 10.3389/fsurg.2022.1039362
Received: 8 September 2022; Accepted: 28 October 2022;
Published: 6 January 2023.
Edited by:
Maurizio Brausi, Hesperia Hospital, ItalyReviewed by:
Fanyue Qin, Third Affiliated Hospital of Zhengzhou University, ChinaSinan Hatipoglu, Adiyaman University, Turkey
© 2023 Li, Liao, Yao, Zhang, Li and Dong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wanqiang Li NjQ5NDI3ODE5QHFxLmNvbQ==
Specialty Section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
 Wanqiang Li
Wanqiang Li Zhengquan Liao2
Zhengquan Liao2