
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 06 January 2023
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1016707
 Peizhi Yuwen1
Peizhi Yuwen1 Weiyi Sun1
Weiyi Sun1 Jialiang Guo1
Jialiang Guo1 Wenli Chang2
Wenli Chang2 Ning Wei3
Ning Wei3 Haicheng Wang1
Haicheng Wang1 Kai Ding1
Kai Ding1 Wei Chen1,4,5,6
Wei Chen1,4,5,6 Yingze Zhang1,4,5,6*
Yingze Zhang1,4,5,6*
Objectives: This study aims to quantitatively evaluate the femoral–tibial contact pressure on the knee under certain malrotaional degrees.
Methods: Femoral–tibial contact pressure was carried out on 14 fixed rotational knee models under 200/400/600 N vertical load using ultra-low-pressure sensitive film technology, rotation angles including neutral position (0°, anatomically reduced), 5°, 10°, and 15° internally and externally. Data were collected and analyzed with SPSS software.
Results: There are significant statistical differences between the medial contact pressure among rotational deformities (including neutral position) (P < 0.01), the increase in the degree of fixed internal malrotation of the femur resulted in a linear increase in the medial femoral–tibial contact pressures (P < 0.05) under 200/400/600 N vertical load, while increase in the degree of fixed external malrotation resulted in a linear decrease (P < 0.05). Except the 200 N compression, we can't find significant differences in lateral contact pressures (P > 0.05). In the comparison of medial to lateral contact pressures, no statistically significant differences were found in neutral and 5° internal rotation under 200/400 N, neutral, 5° internal rotation, and 15° external rotation under 600 N. In contrast, medial contact pressures were higher than lateral at other angles (P < 0.05).
Conclusion: Obvious contact pressure changes were observed in rotatory femur. Doctors should detect rotational deformity as much as possible during operation and perform anatomical reduction. For patients with residual rotational deformities, indication of osteotomy should not be too broad.
Rotational deformity is one of the most significant complications of femoral shaft fractures, and many studies have mentioned its high incidence (1–4). More than 15° torsion deformity alters gait mechanics and efficiency (5–8), as it completely disrupts the biomechanical relationship of hip and knee joint or both and changes the stroke and direction of related muscles. Patients might develop degenerative arthritis of the knee (KOA) and obvious local symptoms in the long term (9–14).
Femur osteotomy is a well-established surgical treatment for femoral torsion (6). Generally, a malrotation <10° is reckoned as a normal alteration, >15° is a true torsional deformity (1, 15, 16), and between 10° and 14° is considered a “gray area” (15–17). However, this conclusion comes from a large number of clinical observations, patient's subjective feelings, and different conclusions in the literature, so robust evidence is needed for surgical indications. We, therefore, bring this biomechanical study to understand the changes of the medial and lateral femoral–tibial contact pressures under different rotation angles and compressions and to provide theoretical support for the cutting angle of femoral osteotomy.
This study has been approved by the Institutional Review Board (IRB) of the Third Hospital of Hebei Medical University (2017-003-1). All cadavers were voluntarily donated and provided by the Department of Human Anatomy, Hebei Medical University. Consent for the storage and use of the bodies for research purposes was given by all body donors before death or by their next of kin.
Specimen preparation: Fourteen fresh-frozen cadaveric lower limbs with intact soft tissue were autopsied; the mean height of the donors was 171 cm (range, 163–181 cm), and average age was 55 years (range, 42–65 years). No history of surgery and gross knee deformities, i.e., hyperflexion, hyperextension, varus, and valgus were observed of all specimens. The passive joint motion was freely achieved. Subsequently x-ray examination showed that all inner structures were intact.
The muscular tissues are carefully excised, and the intact joint capsule and surrounding overlying ligaments are observed (Figure 1). A horizontal incision approximately 3–4 cm long is made along the level of the joint space on either side of the patellar ligament, close to the inferior border of the patella. The subcutaneous fat and capsule are separated and the joint space is exposed. Particular attention needs to be paid to checking the integrity of the anterior and posterior cruciate ligaments and meniscus, as the meniscus is a load-bearing structure that buffers pressure and affects the expansion (18). The lower limb mechanical force line is marked prior to the experiment (17).
Establishment of rotatory fixation models: The femoral shaft was sawn transversely at the distal one-third, rotated at a specific angle, and then both femoral stumps were fixed with plates and screws. Specific angles included neutral (0°, anatomically reduced), 5°, 10°, and 15° internal and external rotation. To facilitate retrofitting to the biomechanical machine, the distal femur and the proximal tibia and fibula were each retained at 25 cm.
An ultra-low-pressure sensitive film (LLW type, Fujifilm Investment Co. Ltd. Japan) was used to measure the intra-articular femoral–tibial contact pressures. The room humidity was set at 35% RH and the temperature was 20 °C to ensure its sensitivity. Fuji films (0.5–2.5 MPa) were trimmed to fit the joint lacuna, in order to prevent contamination; then, they were wrapped and sealed with a thin polyethylene sheet (total thickness, approximately 250 pm). After finishing, two wrapped Fuji films were carefully inserted into the space beneath the medial and lateral meniscus through the anterior incision, ensuring that they were fully accessed, suturing the capsule tightly; any leaking, bent, or broken seal pocket meant failure (19) (Figure 2). Before insertion, indentations are made with a hemostat to distinguish the anterior and posterior side of the Fuji films.
Assembling models: The models were rigidly clamped in a self-made iron square trough in anatomic position, and two ends were embedded in a mixture of denture base resin (type II self-setting denture base powder) and denture base resin liquid (type II self-setting denture base water) (Figures 3, 4). The completed fixed model was then transferred and assembled into the biomechanical test machine (Electroforce 3520-AT, Bose company, United States).
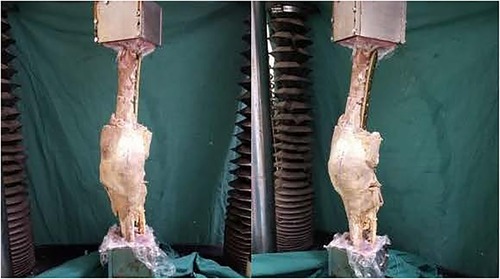
Figure 3. Model of external rotatory deformity. The specimens were assembled to the BOSE Electroforce 3520-AT biomechanical testing machine.
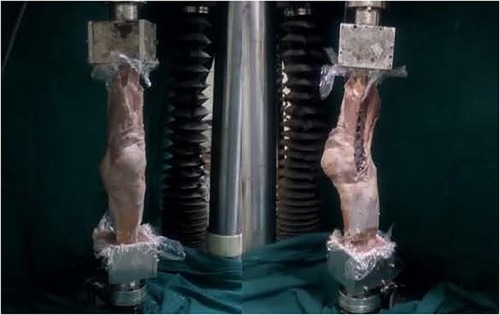
Figure 4. Model of internal rotatory deformity. The specimens were assembled to the BOSE Electroforce 3520-AT biomechanical testing machine.
To eliminate creep, biomechanical machine was started and the test bench was loaded with a pressure up 200 N at a speed of 10N/s. After stabilization, axial compression up to 400 N was applied to each knee and upheld for 2 min; the Fuji films were took out and unloaded. Pressure values were read through the FPD-305E density meter and the FPD-306E pressure converter. Experiments were carried out as above with 200 and 600 N.
Measurements were repeated three times for each specimen to eliminate interobserver variation. Saline was continuously sprayed on the specimens during the experiment to prevent drying from affecting the accuracy of the experimental data.
Experimental data were collated and calculated using SPSS 21.0 software (SPSS, Chicago, IL, United States). Normality was verified using the Shapiro–Wilk test and expressed as . We used t-tests for two independent samples to obtain differences between the medial and lateral groups, and the Student–Newman–Keuls test was used for pairwise comparisons between multiple sample measures. The Levene test was used to test for consistency of variance, and analysis of variance (ANOVA) was performed on randomized groups of zones. Data that did not conform to normality were expressed as median (quartiles), and the Mann–Whitney U test was used to obtain differences between the inner and outer groups. The Kruskal–Wallis H-test was used for the random block group; P < 0.05 indicated significance.
Tables 1, 2 show the calculated contact pressures in neutral position (0°, anatomically reduced)5°, 10°, and 15° of internal and external rotation under 200, 400, and 600 N vertical compressions (Figure 5).
The contact pressures in neutral position are the lowest on both medial and lateral sides compared to other angles under any compressions.
The increase in the degree of fixed internal malrotation of the femur resulted in a linear increase in the medial femoral–tibial contact pressures (P < 0.05) under any compressions, while an increase in the degree of fixed external malrotation resulted in a linear decrease (P < 0.05). There are significant statistical differences between the medial contact pressure among rotational deformities (including neutral position) (P < 0.01); comparisons in pairs were all significant (P < 0.05).
Except the 200 N compression, we could not find significant differences in lateral contact pressure among malrotaional angels (P > 0.05).
In the comparison of medial to lateral contact pressures, no statistically significant differences were found in neutral and 5° internal rotation under 200/400 N, and neutral, 5° internal rotation, and 15° external rotation under 600 N. In contrast, medial contact pressures were higher than lateral at other angles (P < 0.05) (Tables 3–5).
Residual rotational misalignment of the femur remains a Gordian knot (20, 21). Winquist et al. (3) conducted a study on 520 femoral shaft fractures and noticed that 8% of patients had postoperative external rotation deformities of more than 10°. Bråten et al. (1) in 1993 found that 19% of patients had more than 15° malalignment after intramedullary nailing nailing of femoral fractures. Sennerich et al. (2) reported that 40% patients had more than 10° of rotational malalignment and 16% had more than 20°. Hufner et al. (22) documented that 22% of 82 patients had a rotation deformity more than 15° after intramedullary nails. Others (5, 23, 24) reported an even higher incidence.
In our biomechanical study, the contact pressures in neutral position are the lowest on both medial and lateral sides compared to other angles under any compressions. Indicating that any rotation deformity will result into the contact pressure increasing, which is consistent with the conclusion of the study by Thorp et al. (25), the contact pressure on the medial compartment was significantly higher in patients with knee osteoarthritis than normal ones during walking. It is not difficult to conclude that rotation deformity is one of the risk factors of knee arthritis. Changes in intra-articular pressures and asymmetric weight-bearing during movement exceed the elastic potential capacity of the cartilage and subchondral bone. In addition, preexisting axial pressures are partially converted into shear forces due to rotational deformities, causing a local biomechanical chain reaction (26, 27).
We also found that the medial contact pressure is close to the lateral side at 0° and 5° internal rotation; a possible explanation is that the human body has certain adaptability, trying to balance the increased pressure. While exceeding 5°, the medial contact pressures were higher than the lateral side, the human body begins to lose balance and the medial compartment bears the brunt. Our findings coincide with those of Foroughi et al. (28) that changes in the medial compartment are the most pronounced in degenerative arthritis, occurring 10 times more frequently than the lateral compartment.
Poor reduction and postoperative malalignment is the main cause of rotational deformities. Early detection during operation can help surgeons to improve the quality of fracture reduction, but once rotational deformity is identified postoperatively, osteotomy is inevitable. However, the indications are still unclear. Lee et al. (29) argue that as long as the deformity is obvious, it can be corrected by osteotomy. Piper et al. (30) believed that internal rotation exceeding 10° can be corrected by osteotomy. Citak et al. (31) found that indication could be relaxed to 15°, as hideously torsion can severely affect activities and even lower limb function abnormalities. Other authors (2, 32) have concluded that torsional deformity of less than 20° is not usually a barrier. We found that contact pressure on the medial side decreased with the aggravation of external rotation and increased with the aggravation of internal rotation, but both were higher than the neutral position. There is no significant difference in lateral contact pressure at all malrotaional angels. Therefore, we recommend that doctors should give more attention to internal rotation than external rotation. From our point of view, the indications for osteotomy should not be too broad, although some patients can tolerate certain degree of torsional alignment.
Certain limitations are evident in this study. First, this was an in vitro study, which is not fully representative of the muscle dynamics of a normal human being. Second, our study fixed the models along the anatomical axis, which may increase the femoral–tibial contact pressure on the medial side. Third, vertical compression is definitely small to simulate human beings in walking or running activities, and in future, lager pressure experiments are expected.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) of the Third Hospital of Hebei Medical University. The patients/participants provided their written informed consent to participate in this study.
PY and WS designed the study. JG, WC, and NW made substantial contributions to collect and judge all data. PY and WC analyzed data and performed statistical analysis. PY and WS drafted the manuscript. HW, KD, and YZ give specific suggestions about the writing. All authors contributed to the article and approved the submitted version.
The study was supported by the Non-profit Central Research Institute Fund of the Chinese Academy of Medical Sciences (2019PT320001) and the Major Research Plan of National Natural Science Foundation of China (91949203).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bråten M, Terjesen T, Rossvoll I. Torsional deformity after intramedullary nailing of femoral shaft fractures: measurement of femoral anteversion in 110 patients. J Bone Joint Surg Br. (1993) 75:799–803. doi: 10.1302/0301-620X.75B5.8376444
2. Sennerich T, Sutter P, Ritter G, Zapf S. Computerized tomography follow-up of the ante-torsion angle after femoral shaft fractures in the adult. Unfallchirurg. (1992) 95(6):301–5. PMID: 16361111636111
3. Winquist RA, Hanson ST Jr., Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. (1984) 66(4):529–39. doi: 10.2106/00004623-198466040-00006
4. Yang KH, Han DY, Jahng JS, Shin DE, Park JH. Prevention of malrotation deformity in femoral shaft fracture. J Orthop Trauma. (1998) 12(8):558–62. doi: 10.1097/00005131-199811000-00005
5. Karaman O, Ayhan E, Kesmezacar H, Seker A, Unlu MC, Aydingoz O. Rotational malalignment after closed intramedullary nailing of femoral shaft fractures and its influence on daily life. Eur J Orthop Surg Traumatol. (2014) 24(7):1243–7. doi: 10.1007/s00590-013-1289-8
6. Middleton S, Walker RW, Norton M. Decortication and osteotomy for the correction of multiplanar deformity in the treatment of malunion in adult diaphyseal femoral deformity: a case series and technique description. Eur J Orthop Surg Traumatol. (2018) 28(1):117–20. doi: 10.1007/s00590-017-2008-7
7. Palmu SA, Lohman M, Paukku RT, Peltonen JI, Nietosvaara Y. Childhood femoral fracture can lead to premature knee-joint arthritis. Acta Orthop. (2013) 84(1):71–5. doi: 10.3109/17453674.2013.765621
8. McErlain DD, Milner JS, Ivanov TG, Jencikova-Celerin L, Pollmann SI, Holdsworth DW. Subchondral cysts create increased intra-osseous stress in early knee OA: a finite element analysis using simulated lesions. Bone. (2011) 48(3):639–46. doi: 10.1016/j.bone.2010.11.010
9. Eckhoff DG, Kramer RC, Alongi CA, VanGerven DP. Femoral anteversion and arthritis of the knee. J Pediatr Orthop. (1994) 14(5):608–10. doi: 10.1097/01241398-199409000-00010
10. Tönnis D, Heinecke A. Diminished femoral antetorsion syndrome: a cause of pain and osteoarthritis. J Pediatr Orthop. (1991) 11:419–31. doi: 10.1097/01241398-199107000-00001
11. Kumar A, Whittle AP. Treatment of complex (Schatzker type VI) fractures of the tibial plateau with circular wire external fixation: retrospective case review. J Orthop Trauma. (2000) 14(5):339–44. doi: 10.1097/00005131-200006000-00006
12. Greenwood DC, Muir KR, Doherty M, Milner SA, Stevens M, Davis TR. Conservatively managed tibial shaft fractures in Nottingham, UK: are pain, osteoarthritis, and disability long-term complications? J Epidemiol Community Health. (1997) 51(6):701–4. doi: 10.1136/jech.51.6.701
13. Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury. (2006) 37(6):475–84. doi: 10.1016/j.injury.2005.06.035
14. Kettelkamp DB, Hillberry BM, Murrish DE, Heck DA. Degenerative arthritis of the knee secondary to fracture malunion. Clin Orthop Relat Res. (1988) 234:159–69. doi: 10.1097/00003086-198809000-00029
15. Jaarsma RL, Pakvis DF, Verdonschot N, Biert J, van Kampen A. Rotational malalignment after intramedullary nailing of femoral fractures. J Orthop Trauma. (2004) 18(7):403–9. doi: 10.1097/00005131-200408000-00002
16. Brouwer KJ, Molenaar JC, van Linge B. Rotational deformities after femoral shaft fractures in childhood: a retrospective study 27–32 years after the accident. Acta Orthop Scand. (1981) 52:81–9. doi: 10.3109/17453678108991764
17. Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. (1987) 69(5):745–9. doi: 10.2106/00004623-198769050-00016
18. Fukubayashi T, Kurosawa H. The contact area and pressure distribution pattern of the knee. A study of normal and osteoarthrotic knee joints. Acta Orthop Scand. (1980) 51(6):871. doi: 10.3109/17453678008990887
19. Bedi A, Kelly NH, Baad M, Fox AJ, Brophy RH, Warren RF, et al. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. (2010) 92(6):1398–408. doi: 10.2106/JBJS.I.00539
20. Rippstein J. Zur bestimmung der antetorsion des schenkelhalses mittels zweier röntgenaufnahmen. Z Orthop. (1955) 86:345–60. PMID: 1325751813257518
21. Bråten M, Terjesen T, Rossvoll I. Femoral anteversion in normal adults: ultrasound measurements in 50 men and 50 women. Acta Orthop Scand. (1992) 63:29–32. doi: 10.3109/17453679209154844
22. Hufner T, Citak M, Suero EM, Miller B, Kendoff D, Krettek C, et al. Femoral malrotation after unreamed intramedullary nailing: an evaluation of influencing operative factors. J Orthop Trauma. (2011) 25(4):224–7. doi: 10.1097/BOT.0b013e3181e47e3b
23. Thoresen BO, Alho A, Ekeland A, Strømsøe K, Follerås G, Haukebø A. Interlocking intramedullary nailing in femoral shaft fractures. A report of forty-eight cases. J Bone Joint Surg Am. (1985) 67(9):1313–20. doi: 10.2106/00004623-198567090-00002
24. Bellabarba C, Ricci WM, Bolhofner BR. Indirect reduction and plating of distal femoral nonunions. J Orthop Trauma. (2002) 16:287–96. doi: 10.1097/00005131-200205000-00001
25. Thorp LE, Sumner DR, Wimmer MA, Block JA. Relationship between pain and medial knee joint loading in mild radiographic knee osteoarthritis. Arthritis Care Res. (2007) 57(7):1254–60. doi: 10.1002/art.22991
26. Chew MW, Henderson B, Edwards JC. Antigen-induced arthritis in the rabbit: ultrastructural changes at the chondrosynovial junction. Int J Exp Pathol. (1990) 71(6):879. PMID: 22788282278828
27. Hamerman D. The biology of osteoarthritis. N Engl J Med. (1989) 320(20):1322. doi: 10.1056/NEJM198905183202006
28. Foroughi N, Smith R, Vanwanseele B. The association of external knee adduction moment with biomechanical variables in osteoarthritis: a systematic review. Knee. (2009) 16(5):303. doi: 10.1016/j.knee.2008.12.007
29. Lee SY, Jeong J, Lee K, Chung CY, Lee KM, Kwon SS, et al. Unexpected angular or rotational deformity after corrective osteotomy. BMC Musculoskelet Disord. (2014) 15:175. doi: 10.1186/1471-2474-15-175
30. Piper K, Chia M, Graham E. Correcting rotational deformity following femoral nailing. Injury. (2009) 40(6):660–2. doi: 10.1016/j.injury.2008.10.034
31. Citak M, Kendoff D, Gardner MJ, Oszwald M, O'Loughlin PF, Olivier LC, et al. Rotational stability of femoral osteosynthesis in femoral fractures—navigated measurements. Technol Health Care. (2009) 17(1):25–32. doi: 10.3233/THC-2009-0529
32. Yokozeki K. A study on alignment of comminuted femoral fractures treated by interlocking cylinder nailing. Kitasato Med. (1992) 22:20–8. Available at: https://xueshu.baidu.com/usercenter/paper/show?paperid=96534604c0b9f9e5da5ed9191499e593&site=xueshu_se
Keywords: biomechanics, contact pressure, knee, fracture, internal rotation, external rotation
Citation: Yuwen P, Sun W, Guo J, Chang W, Wei N, Wang H, Ding K, Chen W and Zhang Y (2023) Femoral–tibial contact stresses on fixed rotational femur models. Front. Surg. 9:1016707. doi: 10.3389/fsurg.2022.1016707
Received: 11 August 2022; Accepted: 28 October 2022;
Published: 6 January 2023.
Edited by:
Hengxing Zhou, Tianjin Medical University General Hospital, China© 2023 Yuwen, Sun, Guo, Chang, Wei, Wang, Ding, Chen and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yingze Zhang eXpsaW5nX2xpdUAxNjMuY29t
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.