
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 06 January 2023
Sec. Otorhinolaryngology - Head and Neck Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1014649
Pulsatile tinnitus (PT) caused by enlarged oblique occipital sinus (OOS) and resultant diverticulum/dehiscence of the sigmoid-jugular wall has not been described in previous literature. This study recruits one case of PT induced by ipsilateral enlarged OOS and sigmoid-jugular wall diverticulum (case 1) alongside one case of PT induced by ipsilateral enlarged OOS and sigmoid-jugular wall dehiscence (case 2). Various radiologic and computational techniques including computed tomography (CT), magnetic resonance (MR) imaging, Doppler ultrasound, and computational fluid dynamics (CFD) simulation were implemented. Transmastoid sinus wall reconstruction was performed on case 1 with a large sigmoid-jugular diverticulum potentially traumatizing the facial nerve canal. Contrast-enhanced CT or MR venogram images coupling with three-dimensional reconstructed are advantageous in revealing the covert route of OOS that runs under the cerebellum and drains directly into jugular bulb (JB) region. PT in case 1 was successfully eliminated after transmastoid sinus wall reconstruction surgery. Tinnitus handicap inventory score in case 1 reduced from 70 to 0. The ipsilateral jugular outflow mean velocity (Vmn) and flow volume (FVOL) were 42.5 cm/s and 25.9 g/s (case 1 prior to surgery) and 56.6 cm/s and 41.2 g/s (case 2), respectively. Based on CFD simulation, the peak flow velocity in OOS was 1.85 m/s and 2.1 m/s, the wall pressure of the diverticular dome and dehiscence area of the SS-JB wall was 1724.7 Pa and 369.8 Pa in case 1 and 2, respectively. Enlarged OOS caries greater flow kinetic energy that possibly induces sigmoid-jugular wall diverticulum/dehiscence; transmastoid surgical method is safe and therapeutically effective against PT induced by enlarged OOS.
Vascular pulsatile tinnitus (PT) or pulse-synchronous tinnitus is the auditory perception of vascular sounds in line with the cardiac rhythm (1). The most common type of vascular PT is venous PT (2), which is characterized by the reduction or elimination of PT sound when the ipsilateral internal jugular vein (IJV) is compressed (3).
Venous PT requires prudent examination of venous vasculature and the surrounding osseous structure near the hearing apparatus. The causes of venous PT include sigmoid sinus (SS) wall anomalies, high-riding jugular bulb (JB) dehiscence/diverticulum, transverse-SS enlargement, and mastoid emissary vein (4, 5). The symptomology and radiologic signs in patients with venous PT overlap with those in patients with idiopathic intracranial hypertension, a clinical entity characterized by increased intracranial pressure with unknown cause (4). Hypothesized mechanisms of the cause of PT relate to (1) osseous defects surrounding the pulsating vessel that produce vibroacoustic noises, and (2) increased flow kinetic energy that engenders hydroacoustic vascular sounds (6). The produced mechanical sound is transmitted predominantly through the air-conduction pathway to the inner ear, resulting in the perception of PT (5–7).
The occipital sinus is a small venous channel found in 64.5%–95% of cadaveric specimens and normal subjects (8). The length and inner diameter of an occipital sinus measure between 15 and 70 mm and 0.33–7.06 mm, respectively, and age-related regression may occur (9). It is usually positioned underneath the torcular herophili at the midline near the attachment of the falx cerebelli or deviates on the left or right side with two or more cranial or caudal divisions. In a large case series, Kobayashi et al. found that 11.9% of the occipital sinus communicates with or branches into the SS (10). This type of occipital sinus is called oblique occipital sinus (OOS). However, despite previous reports, the epidemiology of a large OOS that runs directly into the SS or the JB remains unknown.
This study reports unprecedented causes of venous PT caused by ipsilateral OOS and sigmoid-jugular wall anomalies (SJWAs) invading the mastoid cavity and sheds light on the mechanism of this newly discovered phenotype of venous PT.
A 43-year-old female patient with persistent right sided PT for 1 year as the solitary symptom presented to our facility in June 2022. Her PT was abolished when the ipsilateral IJV was compressed. Endoscopic examination revealed a normal tympanic membrane in both ears. Pure-tone audiometry showed no hearing loss on either side. Computed tomography (CT) revealed a right-sided SS-jugular diverticulum invading the lower mastoid cavity, potentially traumatizing the facial nerve and nearly exiting the mastoid apex (Figure 1). The closest distance between the dome of the diverticular and facial nerve canal was 3 mm. Magnetic resonance (MR) images revealed an enlarged OOS running into the lower curve of the right-side SS, with ipsilateral intrinsic transverse sinus stenosis and contralateral transverse sinus hypoplasia. A diverticulum had formed between the lower curve of the SS and JB. Fundus examination showed presence of bilateral papilledema. The tinnitus handicap score was 70. Computational fluid dynamics (CFD) was performed to analyze sinus flow hemodynamics (see Supplementary Digital Content S1 for CFD methodology). Transmastoid surgical resurfacing of SJWAs was performed to resolve the PT (see Figure 2 for a detailed description of the surgical procedures).
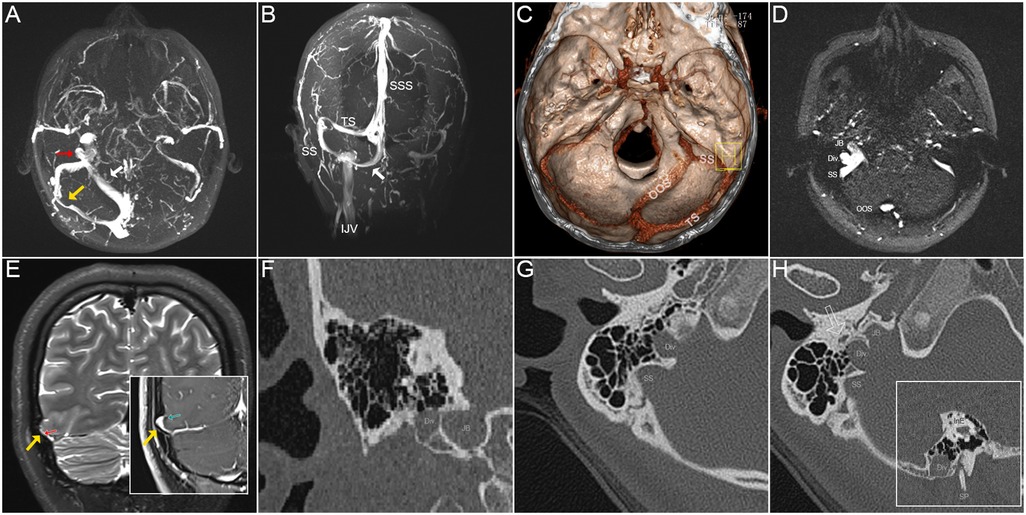
Figure 1. Radiological imaging and signs of case 1 of right-sided pulsatile tinnitus. (A) The maximum intensity projection (MIP) reconstruction of axial 2D-time-of-flight (TOF) magnetic resonance (MR) images showing an enlarged oblique occipital sinus (OOS, white arrow) anastomosing with the lower curve sigmoid sinus (SS), forming a diverticulum (red arrow) in between the SS and jugular bulb (JB). Note the abrupt transverse sinus stenosis at the middle segment. (B) Coronal MIP reconstruction of 2D-TOF MR images. The white arrow indicates the enlarged OOS. (C) Volume rendering technique reconstructed using postoperative contrast-enhanced CT images demonstrating an enlarged OOS running above the occipital bone and underneath the cerebellum to directly anastomose with SS. (D) An axial 2D-TOF MR slice showing the SS, diverticulum (Div.), JB, and OOS. (E) Coronal T2-weighted MR and T1-weighted 2D FLASH images showing the brain herniation into arachnoid granulation [(cerebrospinal fluid signal hyperintense on T2 (red arrow) and hypointense on T1 (green arrow)] that compress into the transverse sinus lumen (yellow arrow), which should be suspected of increased intracranial pressure. (F) Coronal CT image showing the relative location of the diverticulum and JB. (G) Axial CT image exhibiting a seemingly right-sided high-riding JB dehiscence/diverticulum (pseudo-JB anomalies sign) invading the mastoid cavity. The bulging vascular wall emerging at the lower SS was a diverticulum (Div.) but not JB. (H) Axial CT slice showing the SS, diverticulum (Div.), and JB. The hollow arrow indicates the facial nerve canal. The reconstructed sagittal CT slice shows the diverticulum (Div.) nearly exited the mastoid apex. SP and InE indicate the styloid process and inner ear, respectively.
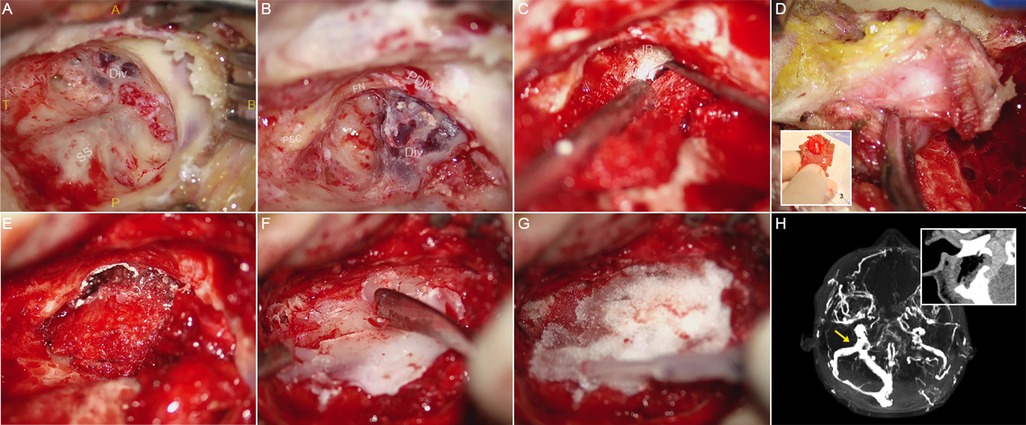
Figure 2. Intraoperative photographs and detailed description of the transmastoid surgery of case 1. (A) Localizing the SS-JB diverticulum by adopting a lower mastoid bone incision site with the upper and lower bonds leveling with the base of the external canal and the mastoid apex, respectively. Note the absence of osseous wall and dura mater covering the surface of the diverticulum upon initial exposure. SS, sigmoid sinus; Div., diverticulum; A, anterior; P, posterior; T, top; B, bottom. (B) Skeletonization of the posterior semi-circular canal (PSC), facial nerve (FN), and the diverticulum (Div.) in sequential order. Notably, the diverticulum abuts the posterior digastric muscle (PDM) and nearly exits the mastoid apex. (C) A 45-degree knife curette was used to separate the diverticular wall from the surrounding osseous walls. To prevent excessive hemorrhage, a ribbon gauze was placed topically over the diverticulum to protect its fragile surface. (D) Rupture of the diverticular wall can be inevitable during the separation procedure, which the high blood flow velocity and pressure render the process of hemostasis arduous. Therefore, we harvested and customized the hemostatic material (a robust yet pliable artificial dura mater-temporalis fascia complex) that also serves as the sinus wall repairing material. (1) Topical fixation of a tough solidified artificial dura mater smeared with surgical glue to compress and reduce the diverticulum. (2) Robust yet pliable hardened/dried temporalis fascia providing a petticoat-like supporting structure to fit and laminate with the surrounding osseous structures. (3) Prior to holistic and surgical glue fixation of the repairing materials, the suture was sewn at the caudal portion of the temporalis fascia to prevent suction of the operative filler into the vascular laceration and into the sigmoid sinus. (E) Surgical glue fixation of the repairing materials covering the diverticulum. The thickness of repairing materials should be prudently controlled to avoid total collapse of the sigmoid sinus wall. (F) and (G) Bone wax-solidified gelatin sponge complex is applied topically to reconstruct the sound-proof barrier. (H) Postoperative contrast-enhanced CT and magnetic-resonance venogram demonstrating complete reduction of the diverticulum. The yellow arrow exhibiting the befitted extraluminal compression over the sigmoid sinus.
A 35-year-old female patient complained of persistent right-sided PT for a duration of 1.5 years visited our clinic in October 2019. Her PT was silenced during ipsilateral IJV compression. Pure-tone audiometry revealed no hearing loss in either ear. Endoscopic examination revealed insignificant findings on both sides. CT images showed discontinuity and absence of bone structure in the SS-JB wall (Figure 3). MR resonance imaging revealed an enlarged OOS anastomosed with the JB and bilateral transverse sinus hypoplasia. Fundus examination results were normal. The tinnitus handicap index score was 22. CFD simulation was performed. Since the patient chose not to undergo surgical treatment, an annual radiologic follow-up was advised, and continuous online medical consultation was provided.
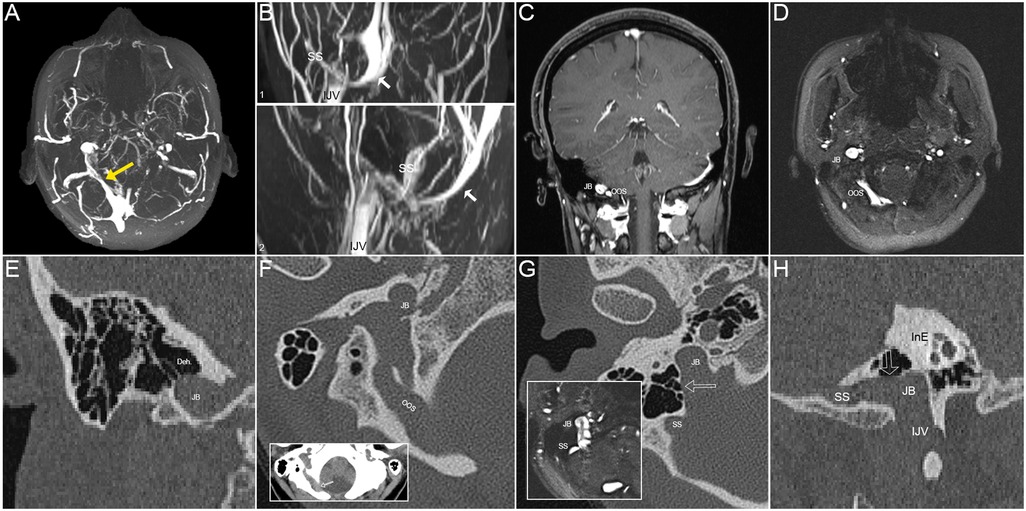
Figure 3. Radiological images of the patient in case 2 of right-sided pulsatile tinnitus (PT). (A) The maximum intensity projection (MIP) reconstruction of axial 2D-time-of-flight (TOF) magnetic resonance (MR) images showing an enlarged oblique occipital sinus (OOS) with distal stenosis (yellow arrow) anastomosing with the ipsilateral jugular bulb (JB). (B) (1) Coronal and (2) sagittal maximum intensity projection (MIP) reconstruction of 2D-time-of-flight (TOF) magnetic resonance (MR) images demonstrating the enlarged OOS (white arrows) running under the cerebellum. SS, sigmoid sinus; IJV, internal jugular vein. (C) Coronal contrast-enhanced T1-weighted gradient echo (2D FLASH) MR slice showing the relative locations of OOS and JB. (D) An axial 2D-TOF MR slice showing the SS, diverticulum (Div.), JB, and OOS. (E) Coronal CT image demonstrating dehiscence at the top of the SS-JB wall. (F) The notch of the OOS cuts through the edge of the foramen magnum of the occipital bone (red arrow). (G) Axial CT image showing SS-JB wall dehiscence and intrasinus flow pattern exhibited using the corresponding 2D-time-of-flight (TOF) magnetic resonance slice. (H) Reconstructed sagittal CT image exhibiting SS-JB wall dehiscence and locations of the SS, JB, and inner ear (InE).
The ipsilateral jugular outflow mean velocity (Vmn) and flow volume (FVOL) were 42.5 cm/s and 25.9 g/s (case 1) and 56.6 cm/s and 41.2 g/s (case 2), respectively. The postoperative ipsilateral Vmn and FVOL of case 1 were 44.1 cm/s and 26.9 g/s. CFD analysis found that the peak velocity in the enlarged OOS was 1.85 m/s and 2.1 m/s, the wall pressure of the diverticular dome and SS-JB wall was 1724.7 Pa and 369.8 Pa in case 1 and 2, respectively (Figure 4).
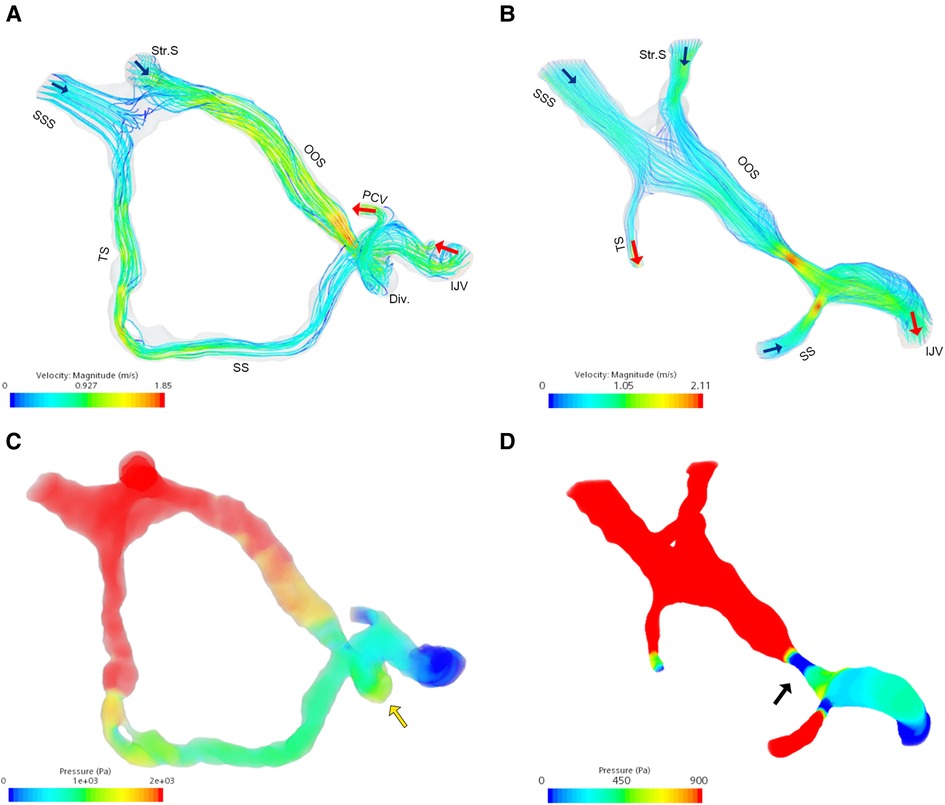
Figure 4. Flow field analysis of the enlarged oblique occipital sinus. (A) Velocity flow field in case 1. (B) Velocity flow field in case 2. (C) Flow pressure field of case 1. Note the pressure increase at the diverticular dome (yellow arrow). (D) Flow pressure field of case 2. Note the large trans-stenotic pressure gradient caused by OOS stenosis. Blue and red arrows indicate flow inlet and outlet, respectively. SSS, superior sagittal sinus; Str.S, straight sinus; TS, transverse sinus; OOS, oblique occipital sinus; SS, sigmoid sinus; Div., diverticulum; PCV, posterior condylar vein; IJV, internal jugular vein.
PT was eliminated after surgery in case 1. The cross-sectional diameter of the diverticular and SS lumen was reduced from 1.49 to 5.4 mm, rendering a smooth SS silhouette. The postoperative tinnitus handicap index score was 0. The patient had ear numbness and a plugged ear after surgery. There was no recurrence of PT or symptoms related to increased intracranial pressure during the 6-week follow-up.
To the best of our knowledge, PT related to SJWAs caused by an enlarged OOS has not been described in the literature. An enlarged OOS can be overlooked owing to its covert route underneath the cerebellum and direct drainage into the SS or JB. In this study, OOS dominated over the ipsilateral or bilateral hypoplastic transverse sinus and carried excessive flow kinetic energy that exerted flow pressure onto the lower curve of the SS wall. The onset of PT in these two cases likely resulted from the formation of SJWAs, since the presence of OOS is congenital (8, 9). This inference is akin to the mechanism of PT caused by SS wall anomalies, which frequently occur on the dominant side of the transverse-sigmoid sinus junction. Additionally, the Venturi effect was also evidenced by the middle to distal stenosis of the OOS, producing a jet flow effect similar to that observed in transverse sinus stenosis (5). A more severe degree of osseous wall erosion and vascular wall protrusion was observed in these two cases, which is conceivably related to the high flow kinetic energy carried by the enlarged OOS.
According to the jugular Doppler measurement, the ipsilateral FVOL of subjects with enlarged OOS was 1.5∼2.5 times larger than those with venous PT caused by SS wall anomalies (7). Additionally, CFD indicates that the vortex generated at the intersection of the OOS and SS increased the regional flow pressure gradient. Given the impaired flow condition, patients with an enlarged OOS should be suspected of having increased intracranial pressure, especially when bilateral hypoplastic transverse sinus is present. Therefore, surgical attempts to occlude the OOS lumen or significantly reduce the venous pool volume may be unwise, whereas the stenting of OOS stenosis has been shown therapeutically effective, although the presence of SJWAs was not evaluated in that study (11).
PT secondary to SJWAs induced by an enlarged OOS can be treated with transtemporal sinus wall reconstruction surgery. Unlike transverse-SS junction diverticulum or dehiscence, SJWAs caused by an enlarged OOS can be more strenuous to operate on because of its location adjacent to vital anatomical structures. Owing to the fragile diverticulum surface, separating the diverticular and osseous walls (typically the medial portion) most likely lacerates the vascular surface and causes considerable hemorrhage. Because SJWAs are located at the lower curve of the SS, we tailored the repair material and inserted it into the epidural space to stanch bleeding during the reduction of the diverticulum. To avoid sinus overcompression or the entrance of hemostat debris into SS, haemostatic materials should be customized with certain malleability, robustness, and retractability; in our case, this was a large piece of temporalis muscle with the solidified artificial dura mater fixated on the muscular edge sewn with suture. Lastly, regarding strong OOS flow impaction, we reduced the diverticulum and applied multilayer materials to prevent further invasion of the diverticular wall into other anatomical structures and preclude the hydroacoustic/vibroacoustic sound transmission in the mastoid cavity.
Enlarged OOS caries greater flow kinetic energy (with 1.5∼2.5 times larger FVOL compared to those with venous PT without the afferent enlarged OOS) that possibly induces SJWAs. Although the presence of enlarged OOS is rare, this study reveals that the transmastoid surgical method safe and therapeutically effective against PT induced by enlarged OOS and resultant diverticulum/dehiscence of the sigmoid-jugular wall.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethical Committees of the Eye, Ear, Nose, and Throat Hospital in Shanghai, China. The patients/participants provided their written informed consent to participate in this study.
Y-LH designed the study, drafted the manuscript, and performed the computational analyses in this study. SW performed radiologic examinations and post-analysis of radiologic data. WW is the lead surgeon who discovered the pathology, performed the operation, and supervised this study. All authors contributed to the article and approved the submitted version.
This study was supported by Science and Technology Innovation Plan of Shanghai Science and Technology Commission (no. 22Y11902200).
Y-L H would like to thank WQW for sharing his discovery and constantly being attentive to this phenotype of venous PT.
The reviewer [SL] declared a shared parent affiliation with the authors to the handling editor at the time of review. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.1014649/full#supplementary-material.
1. Song JJ, An GS, Choi I, De Ridder D, Kim SY, Choi HS, et al. Objectification and differential diagnosis of vascular pulsatile tinnitus by transcanal sound recording and spectrotemporal analysis: a preliminary study. Otol Neurotol. (2016) 37(6):613–20. doi: 10.1097/MAO.0000000000001005
2. Mattox DE, Hudgins P. Algorithm for evaluation of pulsatile tinnitus. Acta Otolaryngol. (2008) 128(4):427–31. doi: 10.1080/00016480701840106
3. Gao XL, Hsieh YL, Wang X, Wang WQ. Retroauricular/transcranial color-coded Doppler ultrasound approach in junction with ipsilateral neck compression on real-time hydroacoustic variation of venous pulsatile tinnitus. Front Hum Neurosci. (2022) 16:862420. doi: 10.3389/fnhum.2022.862420
4. Harvey RS, Hertzano R, Kelman SE, Eisenman DJ. Pulse-synchronous tinnitus and sigmoid sinus wall anomalies: descriptive epidemiology and the idiopathic intracranial hypertension patient population. Otol Neurotol. (2014) 35(1):7–15. doi: 10.1097/MAO.0b013e3182a4756c
5. Eisenman DJ, Raghavan P, Hertzano R, Morales R. Evaluation and treatment of pulsatile tinnitus associated with sigmoid sinus wall anomalies. Laryngoscope. (2018) 128(Suppl 2):S1–S13. doi: 10.1002/lary.27218
6. Hsieh YL, Gao XL, Wang X, Hsiang FC, Sun XB, Wang WQ. Therapeutic validation of venous pulsatile tinnitus and biomaterial applications for temporal bone reconstruction surgery using multi-sensing platforms and coupled computational techniques. Front Bioeng Biotechnol. (2022) 9:777648. doi: 10.3389/fbioe.2021.777648
7. Hsieh YL, Xu XB, Wu YZ, Wang WQ. Evidence of air-conduction transmission pathway and strategized transtemporal operative techniques for venous pulsatile tinnitus: combining water occlusion test and operative sensing applications. Laryngoscope Investig Otolaryngol. (2021) 6(6):1436–48. doi: 10.1002/lio2.699
8. Tubbs RS, Bosmia AN, Shoja MM, Loukas M, Curé JK, Cohen-Gadol AA. The oblique occipital sinus: a review of anatomy and imaging characteristics. Surg Radiol Anat. (2011) 33(9):747–9. doi: 10.1007/s00276-011-0831-9
9. Balak N, Ersoy G, Uslu Ü, Tanriöver N, Tapul L, Çetin G, et al. Microsurgical and histomorphometric study of the occipital sinus: quantitative measurements using a novel approach of stereology. Clin Anat. (2010) 23(4):386–93. doi: 10.1002/ca.20947
10. Kobayashi K, Suzuki M, Ueda F, Matsui O. Anatomical study of the occipital sinus using contrast-enhanced magnetic resonance venography. Neuroradiology. (2006) 48(6):373–9. doi: 10.1007/s00234-006-0087-y
Keywords: pulsatile tinnitus, occipital sinus, oblique occipital sinus, diverticulum, dehiscence
Citation: Hsieh Y, Wang S and Wang W (2023) Case Report: Venous pulsatile tinnitus induced by enlarged oblique occipital sinus and resultant diverticulum/dehiscence of the sigmoid-jugular wall. Front. Surg. 9:1014649. doi: 10.3389/fsurg.2022.1014649
Received: 8 August 2022; Accepted: 1 November 2022;
Published: 6 January 2023.
Edited by:
Han Lv, Capital Medical University, ChinaReviewed by:
Jae-Jin Song, Seoul National University Bundang Hospital, South Korea© 2023 Hsieh, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wuqing Wang d3d1cWluZ0BlZW50LnNobXUuZWR1LmNu
†These authors share first authorship
Specialty Section: This article was submitted to Otorhinolaryngology - Head and Neck Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.