
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 06 January 2023
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1006167
Background: Os odontoideum is a rare abnormality of the upper cervical spine, and os odontoideum associated with a retro-odontoid cyst has been described as a marker of local instability.
Case description: This paper reports a case of a 52-year-old female patient who was diagnosed with os odontoideum associated with a retro-odontoid cyst. The patient underwent posterior C1–C3 fixation without surgical removal of the cyst. Magnetic resonance imaging (MRI) two days later revealed that the retro-odontoid cyst was still present and that there were no significant changes to it when compared with the preoperative MRI.
Conclusion: Retro-odontoid cysts associated with unstable os odontoideum can lead to symptomatic spinal cord compression. Posterior C1–C3 fixation can restore atlantoaxial stability by allowing the gradual resorption of the cyst and ensuring spinal cord decompression. Fixation can also avoid the surgical risk associated with a high-riding vertebral artery.
Os odontoideum is a rare malformation of the upper cervical spine, and its combination with a retro-odontoid cyst has been described as a marker of local instability. Different terms are associated with retro-odontoid structures involving spinal cord compression, including mass, cyst, pseudotumor, granuloma, and pannus. It is also thought that the atlantoaxial instability related to os odontoideum may prompt the appearance of a retro-odontoid cyst. The nonspecific symptomatic indications of the two together are erratic and vary from cervical pain to neurological disorders (1, 2).
This paper reports a case of os odontoideum associated with a retro-odontoid cyst that was treated with posterior C1–C3 fixation without surgical removal of the cyst. Using magnetic resonance imaging (MRI) that was performed immediately and three months after the fixation operation, it was found, for the first time, that the retro-odontoid cyst did not disappear immediately but was gradually resorbed.
A 52-year-old female patient had displayed numbness (paresthesia) and weakness in her limbs for 3 months. No hemodynamic or respiratory complications were observed during her initial care, and a neurological examination indicated a AIS was D (American Spinal Injury Association Impairment Scale) (3) and no pyramidal syndrome. Cervical flexion and extension radiographs suggested atlantoaxial instability (Figure 1), and a cervical computed tomography (CT) scan demonstrated the existence of a bony continuity that had not been displaced within the odontoid process (Figure 2). These findings, along with the existence of corticalized edges, led to a diagnosis of os odontoideum.
To evaluate the existence of any recent neurological disorders, a cervical MRI was performed, which led to the discovery of a retro-odontoid cyst with T2 hyperintensity and T1 hypointensity. The cyst was exerting pressure on the spinal cord, and the intramedullary T2 hyperintensity signified a spinal cord disorder (Figure 3). Figure 4 indicates the presence of a high left carotid artery span in the patient.
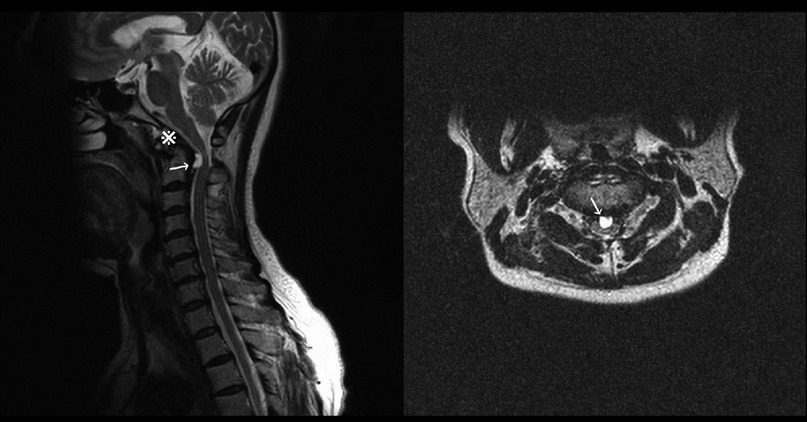
Figure 3. Sagittal and axial preoperative magnetic resonance imaging showing os odontoideum (※) and a compressive retro-odontoid cyst (arrows) with a hyperintense medullary signal.
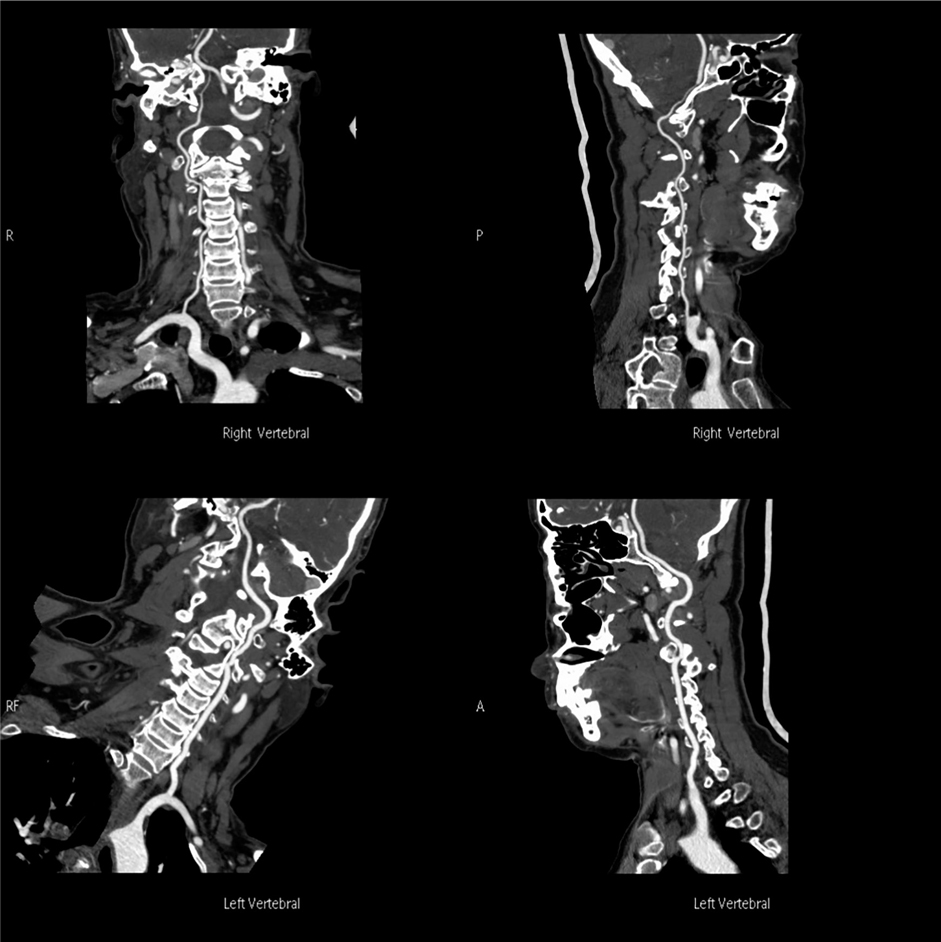
Figure 4. Preoperative carotid CTA indicated the presence of a high left carotid artery span in the patient.
It was decided to perform a C1–C3 fixation (Figure 5), and, two days after the operation, the MRI results showed that the retro-odontoid cyst was still present and had not changed significantly compared with the preoperative MRI results (Figure 6). However, the patient's clinical progress was rapid and favorable, with the paresthesia regressing and motor recovery reaching grade 4 out of 5 by MRC (Medical Research Council) Scale for Muscle Strength (4). She was discharged one week after the surgery with no scarring and no longer presenting paresthesia in the right upper limb, and her ASIA was E. At 3 months, a complete neurological recovery was confirmed. Some cervical pain was reported, 2/10 on the VAS (Visual Analog Scale) (5), without it being debilitating. The follow-up MRI also showed the complete disappearance of the retro-odontoid cyst and no signs of persistent spinal cord involvement (Figure 7).
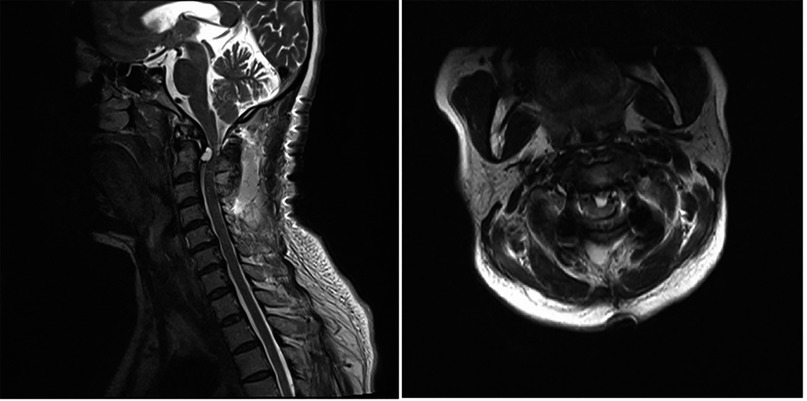
Figure 6. Sagittal and axial immediate postoperative magnetic resonance imaging showing the continued presence of the retro-odontoid cyst.
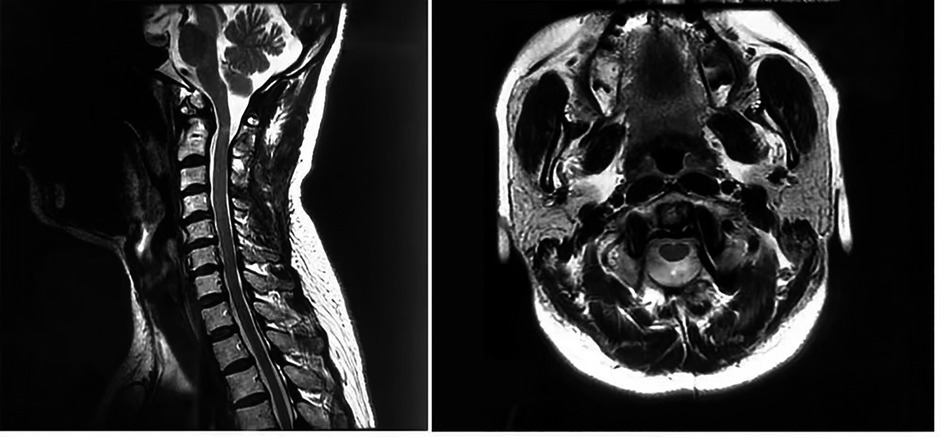
Figure 7. Sagittal and axial 3-month postoperative magnetic resonance imaging showing the complete disappearance of the retro-odontoid cyst.
Os odontoideum was first described by Giacomini in 1886. This abnormality is an anatomical variation of the C2 odontoid process and defined as a small bone of varying size with a smooth margin of the surrounding cortex, separated from the axis.
The etiology of os odontoideum remains controversial but is focused on congenital and acquired causes. With respect to the former, the disorder is often associated with congenital malformations such as Klippel–Feil syndrome, trisomy 21 syndrome, Morquio syndrome, or neurofibromatosis. In terms of the latter, an insufficient arterial blood supply and unrecognized or repeated minor trauma, resulting in transverse ligament contracture, have been found to result in secondary odontoid base contraction (6, 7).
A synovial cyst is a cystic mass lined with pseudo-lamellar columnar cells and containing clear or yellow fluid. Although synovial cysts often occur in the lumbar spine, they rarely occur in the inferior cervical axis and rarely involve the odontoid process. The cause of posterior odontoid cysts is unknown, but previous studies have suggested that these cysts are associated with growth of synovial rests, pluripotent stromal cell proliferation, atlantoaxial instability, and trauma (8). The association of os odontoideum with a posterior odontoid cyst has been described as a marker of local instability, and atlantoaxial instability associated with the odontoid bone may also suggest a retro-odontoid cyst.
Computed tomography and MRI are of great significance in the diagnosis of this type of cyst, which produces a low T1 signal and a high T2 signal. Cysts may also appear black on T2-weighted MRI, possibly due to bleeding and blood products. Peripheral angiographic enhancement is also common, which may be linked to the adjacent epidural plexus. However, cervical synovial cysts cannot be accurately distinguished from other lesions by MRI features, and in many cases, accurate diagnosis can only be made after surgery (1, 2, 8–32).
Hypoplasia of the odontoid associated with an independent oval ossicle, with smooth margins widely separated from the C2 vertebra and well above the superior facets of the axis, is termed os odontoideum. It is a rare condition with a controversial pathogenesis and poorly understood natural history. The neurological manifestations of os odontoideum arise from bulbospinal compression both at rest and during motion due to craniovertebral junction (CVJ) instability. Consequently, the surgical management of os odontoideum should aim at achieving both neural decompression and stabilization of the CVJ (33).
With regard to anterior decompressive procedures, in particular, it has been widely reported that alternative transoral decompressive strategies have been improved with the introduction of endoscopy, neuronavigation, exoscopy, and intraoperative neuroradiological assessment such as the O-arm CT scan. All these approaches contribute to reducing the invasiveness of decompressive procedures and increasing their effectiveness (34–37). In addition, although the transnasal approach seems a more promising minimally invasive alternative to the transoral approach, it can lead to some adverse effects that deserve consideration, including cerebrospinal fluid leakage, infections, and velopalatal dysfunction (38–41). For these reasons, posterior atlantoaxial fixation seems to be a more promising and less invasive form of treatment, but it should only be used for bioptical procedures. In 2004, Goel reported two patients with Atlantoaxial instability and retroodontoid mass. Following atlantoaxial fixation, both patients showed remarkable and sustained neurological improvement. These cases provide further evidence that retroodontoid ligamentous hypertrophic mass lesion could be secondary to instability of the atlantoaxial region (42). Goel (43) also reported an experience with 190 cases of os odontoideum over 20 years. He thought the segmental atlantoaxial fixation is a reliable form of surgical treatment. Bone decompression is not necessary. Inclusion of occipital bone and subaxial vertebrae in the fixation construct is not necessary.
In 2021, Goel (44) searched 63 patients with retro-odontoid pseudotumor, pannus, and/or cyst (RPC) treated by atlantoaxial fixation from January 2000 to March 2020. After atlantoaxial stabilization, the RPC spontaneously regressed or disappeared. Direct resection of the RPC was neither performed nor was necessary in any case. In our case, due to the presence of a high-riding vertebral artery in the patient's preoperative CT examination and to avoid injury to it during screw placement in the C2 vertebra, relatively short screws were used, and posterior C1–C3 fixation was performed to ensure the stability of the fixation. The procedure reconfirmed that retro-odontoid cysts can be treated by posterior spinal fixation and that there is no need to remove the cyst directly by surgery.
In the case reported here, the immediate postoperative MRI showed that the retro-odontoid cyst was still present and had not changed significantly from that of the preoperative MRI findings. However, at the 3-month postoperative follow-up, the MRI confirmed the complete disappearance of the retro-odontoid cyst and the decompression of the spinal cord. This demonstrated, for the first time, that the retro-odontoid cyst did not disappear immediately after surgery but was gradually resorbed.
Retro-odontoid cysts associated with unstable os odontoideum can lead to symptomatic spinal cord compression, but posterior C1–C3 fixation can restore atlantoaxial stability. This approach will allow for the gradual resorption of the cyst postoperatively and ensure spinal cord decompression, and it can also avoid the inherent risks of an operation to remove a cyst when the vertebral artery is high-riding.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The study was conducted in accordance with the Declaration of Helsinki (as was revised in 2013). The study was approved by Ethics Committee of the Beijing Tongren Hospital of Capital Medical University. A written, informed consent was obtained from the participant for the publication of this case report. Written informed consent was obtained from the relevant individual for the publication of any potentially identifiable images or data included in this article.
Conception and design of the research: BXB, JGT: Acquisition of data: BXB, JGT: Analysis and interpretation of the data: HY: Statistical analysis: HY, JGT: Obtaining financing: None: Writing of the manuscript: HY, JGT: Critical revision of the manuscript for intellectual content: BXB, JGT: All authors contributed to the article and approved the submitted version.
We are particularly grateful to all the people who have given us help on our article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Le Pape S, Gauthé R, Latrobe C, Leroux J, Roussignol X, Ould-Slimane M. Cervical myelopathy involving os odontoideum and retro-odontoid cyst treated with Harms C1–C2 arthrodesis. Orthop Traumatol Surg Res. (2016) 102:817–20. doi: 10.1016/j.otsr.2016.06.008
2. Ogata T, Kawatani Y, Morino T, Yamamoto H. Resolution of intraspinal retro-odontoid cyst associated with os odontoideum after posterior fixation. J Spinal Disord Tech. (2009) 22:58–61. doi: 10.1097/BSD.0b013e31815e6d3c
3. Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. (2011) 34(6):535–46. doi: 10.1179/204577211X13207446293695
4. Van Allen M W. Aids to the examination of the peripheral nervous system. Arch Neurol. (1977) 34(1):61–61. doi: 10.1001/archneur.1977.00500130081027
5. Flynn D, Van Schaik P, Van Wersch A. A comparison of multi-item Likert and visual analogue scales for the assessment of transactionally defined coping function. Eur J Psychol Assess. (2004) 20(1):49. doi: 10.1027/1015-5759.20.1.49
6. Giacomini C. Sull' esistenza dell' “osodontoideum: nell” uomo. Gior dr Accaddi med Torino. (1986) 49:24–8.
7. Wang Q, Dong S, Wang F. Os odontoideum: diagnosis and role of imaging. Surg Radiol Anat. (2020) 42:155–60. doi: 10.1007/s00276-019-02351-3
8. Delavari N, Geh N, Hervey-Jumper SL, McKean EL, Sullivan SE. Transnasal and transoral approaches to atlantoaxial synovial cysts: report of 3 cases and review of the literature. World Neurosurg. (2019) 132:258–64. doi: 10.1016/j.wneu.2019.08.248
9. Cecchi PC, Peltz MT, Rizzo P, Musumeci A, Pinna G, Schwarz A. Conservative treatment of an atlantoaxial degenerative articular cyst: case report. Spine J. (2008) 8:687–90. doi: 10.1016/j.spinee.2007.01.006
10. Sagiuchi T, Shimizu S, Tanaka R, Tachibana S, Fujii K. Regression of an atlantoaxial degenerative articular cyst associated with subluxation during conservative treatment. J Neurosurg Spine. (2006) 5:161–4. doi: 10.3171/spi.2006.5.2.161
11. Oushy S, Carlstrom LP, Krauss WE. Spontaneous regression of a retroodontoid transverse ligament cyst: a case report. Neurosurgery. (2019) 84:E112–5. doi: 10.1093/neuros/nyy036
12. D’Aliberti GA, Talamonti G, Villa FG, Crisà FM. A rare case of cervical junction ligamentous cyst. Acta Neurochir. (2019) 16:1385–8. doi: 10.1007/s00701-019-03942-0
13. Zorzon M, Skrap M, Diodato S, Nasuelli D, Lucci B. Cysts of the atlantoaxial joint: excellent long-term outcome after posterolateral surgical decompression. J Neurosurg. (2001) 95:111–4. doi: 10.3171/jns.2001.95.1.0111
14. Ohnishi Y, Iwatsuki K, Taketsuna S, Ninomiya K, Yoshimine T. Retro-odontoid synovial cyst resected via an anterolateral approach without fusion. Eur Spine J. (2015) 24:S508–513. doi: 10.1007/s00586-014-3578-2
15. Colasanti R, Lamki T, Tailor AR, Ammirati M. Recurrent atlantoaxial synovial cyst resection via a navigation-guided, endoscope-assisted posterior approach. Surg Neurol Int. (2014) 5:S567–9. doi: 10.4103/2152-7806.148048
16. Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg. (2000) 93:199–204. doi: 10.3171/jns.2000.93.3.0513
17. Velán O, Rabadán A, Paganini L, Langhi L. Atlantoaxial joint synovial cyst: diagnosis and percutaneous treatment. Cardiovasc Intervent Radiol. (2008) 31:1219–21. doi: 10.1007/s00270-008-9347-z
18. Kenéz J, Turóczy L, Barsi P, Veres R. Retro-odontoid “ghost” pseudotumours in atlanto-axial instability caused by rheumatoid arthritis. Neuroradiology. (1993) 35:367–9. doi: 10.1007/BF00588372
19. Marbacher S, Lukes A, Vajtai I, Ozdoba C. Surgical approach for synovial cyst of the atlantoaxial joint: a case report and review of the literature. Spine. (2009) 34:E528–33. doi: 10.1097/BRS.0b013e3181ab22c3
20. Lyons MK, Birch B. Transoral surgical approach for treatment of symptomatic atlantoaxial cervical synovial cysts. Turk Neurosurg. (2011) 21:483–8. doi: 10.5137/1019-5149.JTN.4288-11.1
21. Lee CY, Lai HY, Lee ST. Ganglion cyst of the cruciate ligament with atlantoaxial subluxation. Acta Neurochir. (2013) 155:1917–21. doi: 10.1007/s00701-013-1803-0
22. Okamoto K, Doita M, Yoshikawa M, Manabe M, Sha N, Yoshiya S. Synovial cyst at the C1–C2 junction in a patient with atlantoaxial subluxation. J Spinal Disord Tech. (2004) 17:535–8. doi: 10.1097/01.bsd.0000117546.88865.62
23. Theodotou CB, Urakov TM, Vanni S. Atlantoaxial synovial cyst: case report and literature review. World Neurosurg. (2016) 92:588.e7–588.e15. doi: 10.1016/j.wneu.2016.04.036
24. Lin D, Ding Z, Guo Y, Lian K. Retro-odontoid cystic mass treated by laminectomy and C1–C2 fixation. Indian J Orthop. (2014) 48:621–4. doi: 10.4103/0019-5413.144239
25. Ito T, Hayashi M, Ogino T. Retrodental synovial cyst which disappeared after posterior C1–C2 fusion: a case report. J Orthop Surg. (2000) 8:83–7. doi: 10.1177/230949900000800115
26. Puffer RC, Van Gompel JJ, Morris JM, Krauss WE. Resolution of cystic deterioration of the C1–2 articulation with posterior fusion: treatment implications for asymptomatic patients. World Neurosurg. (2013) 79:773–8. doi: 10.1016/j.wneu.2012.03.035
27. Tangviriyapaiboon T. Complete spontaneous regression of the intraspinal synovial cyst at the C1–C2 junction following with atlantoaxial fusion of non-union odontoid fracture: a case report. J Med Assoc Thai. (2016) 99:S120–5. PMID: 2990135629901356
28. Klimo P Jr, Kan P, Rao G, Apfelbaum R, Brockmeyer D. Os odontoideum: presentation, diagnosis, and treatment in a series of 78 patients. J Neurosurg Spine. (2008) 9:332–42. doi: 10.3171/SPI.2008.9.10.332
29. Shah A, Jain S, Kaswa A, Goel A. Immediate postoperative disappearance of retro-odontoid “pseudotumor”. World Neurosurg. (2016) 91:419–23. doi: 10.1016/j.wneu.2016.04.050
30. Chang H, Park JB, Kim KW. Synovial cyst of the transverse ligament of the atlas in a patient with os odontoideum and atlantoaxial instability. Spine. (2000) 25:741–4. doi: 10.1097/00007632-200003150-00016
31. Wang X, Fan CY, Liu ZH. The single transoral approach for os odontoideum with irreducible atlantoaxial dislocation. Eur Spine J. (2010) 19:S91–5. doi: 10.1007/s00586-009-1088-4
32. Chang A, Zhao H. Representation of specific diagnosis for low back pain using the 11th revision of international classification of diseases and related health problems: perspectives of conventional medicine and traditional medicine. World J Tradit Chin Med. (2021) 7:234–9. doi: 10.4103/wjtcm.wjtcm_17_21
33. Visocchi M, Di Rocco C. Os odontoideum syndrome: pathogenesis, clinical patterns and indication for surgical strategies in childhood. Adv Tech Stand Neurosurg. (2014) 40:273–93. doi: 10.1007/978-3-319-01065-6_9
34. Visocchi M, Della Pepa GM, Doglietto F, Esposito G, La Rocca G, Massimi L. Video-assisted microsurgical transoral approach to the craniovertebral junction: personal experience in childhood. Childs Nerv Syst. (2011) 27(5):825–31. doi: 10.1007/s00381-010-1386-5
35. Visocchi M, Doglietto F, Della Pepa GM, Esposito G, La Rocca G, Di Rocco C, et al. Endoscope-assisted microsurgical transoral approach to the anterior craniovertebral junction compressive pathologies. Eur Spine J. (2011) 20(9):1518–25. doi: 10.1007/s00586-011-1769-7
36. Visocchi M, Di Martino A, Maugeri R, González Valcárcel I, Grasso V, Paludetti G. Videoassisted anterior surgical approaches to the craniocervical junction: rationale and clinical results. Eur Spine J. (2015) 24(12):2713–23. doi: 10.1007/s00586-015-3873-6
37. Visocchi M, Mattogno PP, Ciappetta P, Barbagallo G, Signorelli F. Combined transoral exoscope and OArm-assisted approach for craniovertebral junction surgery: light and shadows in single-center experience with improving technologies. J Craniovertebr Junction Spine. (2020) 11(4):293–9. doi: 10.4103/jcvjs.JCVJS_176_20
38. Visocchi M. Considerations on “endoscopic endonasal approach to the craniocervical junction: the importance of anterior C1 arch preservation or its reconstruction”. Acta Otorhinolaryngol Ital. (2016) 36(3):228–30. doi: 10.14639/0392-100X-927
39. Visocchi M, Pappalardo G, Pileggi M, Signorelli F, Paludetti G, La Rocca G. Experimental endoscopic angular domains of transnasal and transoral routes to the craniovertebral junction: light and shade. Spine. (2016) 41(8):669–77. doi: 10.1097/BRS.0000000000001288
40. Visocchi M, Signorelli F, Liao C, Rigante M, Paludetti G, Barbagallo G, et al. Endoscopic endonasal approach for craniovertebral junction pathologic conditions: myth and truth in clinical series and personal experience. World Neurosurg. (2017) 101:122–9. doi: 10.1016/j.wneu.2017.01.099
41. Visocchi M, Signorelli F, Liao C, Rigante M, Paludetti G, Barbagallo G, et al. Transoral versus transnasal approach for craniovertebral junction pathologies: never say never. World Neurosurg. (2018) 110:592–603. doi: 10.1016/j.wneu.2017.05.125
42. Goel A, Phalke U, Cacciola F, Muzumdar D. Atlantoaxial instability and retroodontoid mass–two case reports. Neurol Med Chir. (2004) 44(11):603–6. doi: 10.2176/nmc.44.603
43. Goel A, Patil A, Shah A, Dandpat S, Rai S, Ranjan S. Os odontoideum: analysis of 190 surgically treated cases. World Neurosurg. (2020) 134:e512–23. doi: 10.1016/j.wneu.2019.10.107
Keywords: os odontoideum, retro-odontoid cyst, posterior c1-C3 fixation, atlantoaxial stability, gradual resorption of cyst
Citation: Bao B, Yan H and Tang J (2023) Os odontoideum associated with a retro-odontoid cyst treated with posterior C1–C3 fixation: A case report and literature review. Front. Surg. 9:1006167. doi: 10.3389/fsurg.2022.1006167
Received: 29 July 2022; Accepted: 21 October 2022;
Published: 6 January 2023.
Edited by:
Atul Goel, King Edward Memorial Hospital and Seth Gordhandas Sunderdas Medical College, IndiaReviewed by:
Paolo Di Russo, Mediterranean Neurological Institute Neuromed (IRCCS), Italy© 2023 Bao, Yan and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia-Guang Tang dGFuZ2ppYWd1YW5nX2RyMjNAMTYzLmNvbQ==
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.