- 1The School of Clinical Medicine, The Third Clinical Medical College, Fujian Medical University, China
- 2Department of Orthopedics, The First Affiliated Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China
- 3Division of Neurosurgery, Department of Surgery, Changhua Christian Hospital, Changhua, Taiwan
- 4Department of Leisure Industry Management, National Chin-Yi University of Technology, Taichung, Taiwan
- 5College of Nursing and Health Sciences, Dayeh University, Taiwan
- 6Department of Neurosurgery, The First Affiliated Hospital of Xiamen University, School of Medicine, Xiamen University, Xiamen, China
- 7Department of Breast Surgery, The First Affiliated Hospital of Hainan Medical University, Haikou, China
Purpose: In the past decade, the field of pre-psoas oblique lumbar interbody fusion (OLIF) has developed rapidly, and with it, the literature on OLIF has grown considerably. This study was designed to analyze the top 50 articles in terms of the number of citations through bibliometric research to demonstrate the research characteristics and hotspots of OLIF.
Method: Searching the Web of Science database yielded the 50 most cited publications in the OLIF field as of July 10, 2022. The publications were ranked according to the number of citations. The following sources were evaluated: the year of publications, the number of citations, authors, countries, institutions, journals, research topics, and keyword hotspots.
Results: The most productive period was from 2017 to 2020, with 41 articles. The number of citations varied from 10 to 140, with an average of 35.52, and 1,776 citations were found. World Neurosurgery published the most articles (12), China produced the most articles (16), and the Catholic University of Korea produced the most studies (6). The corresponding author who produced the most articles was J.S. Kim (5), and the first author who produced the most publications was S. Orita (3). The main research topics were anatomical morphology, surgical techniques, indications, outcomes, and complications. The top 10 most cited keywords were “complications,” “decompression,” “spine,” “surgery,” “outcomes,” “transpsoas approach,” “spondylolisthesis,” “anterior,” “disease,” and “injury.”
Conclusions: Certain articles can be distinguished from others using citation analysis as an accurate representation of their impact due to their long-term effectiveness and peer recognition. With these publications, researchers are provided with research priorities and hotspots through influential literature in the field of OLIF.
Introduction
The anterior retroperitoneal approach, which was initially introduced by Mayer in 1997 and evolved through time, was termed oblique lateral lumbar interbody fusion (OLIF) by Silvestre et al. (1) in 2012 and has since become a popular and commonly used approach of lumbar interbody fusion (2). The OLIF procedure is distinguished by the fact that it does not require access to the abdominal cavity or incision of the psoas major muscle, thereby, preserving normal anatomy and allowing the placement of large interbody cages to fully restore disk height, achieve indirect decompression, and correct imbalances (3–5). Compared with the typical anterior approach technique, OLIF does not require extensive dissection or traction of the peritoneum, retroperitoneal arteries, and nerves, lowering the risk of vascular, visceral, and nerve injuries (6). The OLIF procedure, as opposed to direct/extreme lateral lumbar interbody fusion (D/XLIF), does not require crossing the lumbar major muscle, protecting it and avoiding the lumbar plexus nerve, resulting in a significantly lower incidence of lumbar plexus nerve injury and eliminating the need for intraoperative nerve monitoring (7, 8). Furthermore, compared with the posterior/transforaminal approach, OLIF does not destroy the muscles, ligament complexes, and bony structures of the posterior lumbar spine, which is more conducive to preserving the stability of the posterior lumbar column and generally does not cause damage to the spinal cord and nerve roots (9, 10). Therefore, annually, numerous experts and researchers endeavor to provide new insights into OLIF, and numerous articles on OLIF are published, proving its safety and effectiveness in the form of case reports, surgical technique descriptions, reviews, and clinical studies.
Citation analysis involves ranking articles based on the number of citations they receive, evaluating them and identifying influential studies in the field, and further applying a bibliometric analysis to these studies (11). While citation analysis studies remain somewhat controversial, proponents point to this method as an objective way in which the importance of an article or journal can be determined.
Citation analysis has been adopted in numerous medical fields to determine influential publications in their respective fields (12–14). However, so far, no citation analysis studies have been conducted focusing on OLIF. Given this situation, this study was designed to analyze the top 50 influential articles through citation analysis to visually present the research characteristics and hotspots of OLIF.
Method
The data for this study were obtained from the Web of Science (WoS) core collection on July 10, 2022. The WoS is a critical database for worldwide access to academic content that is commonly used in citation analysis or bibliometric research (15–17). Furthermore, we used PubMed to identify supplementary data connected to the research.
The following search keywords were used: ((((TS = (oblique)) or TS = (anterior to psoas)) or TS = (anterior retroperitoneal)) or TS = (prepsoas)) and TS = (interbody fusion). From January 1982 to July 10, 2022, all English articles were limited to OLIF. Only original articles and reviews were included. Two independent reviewers confirmed their relevance to the OLIF publications according to their titles and abstracts. Any disagreements were resolved through discussion or by consulting a third reviewer until consensus was reached.
The top 50 OLIF-related articles with the most citations were obtained and reviewed. The title, author names, journal, year of publication, number of citations, and citations per year were documented. The region and institution of each article's author/s were recorded. If an article has more than one region or institution, the region and institution of the last corresponding author are recorded. The keywords were further visualized using the package bibliometrix through RStudio and VOSviewer (18).
Results
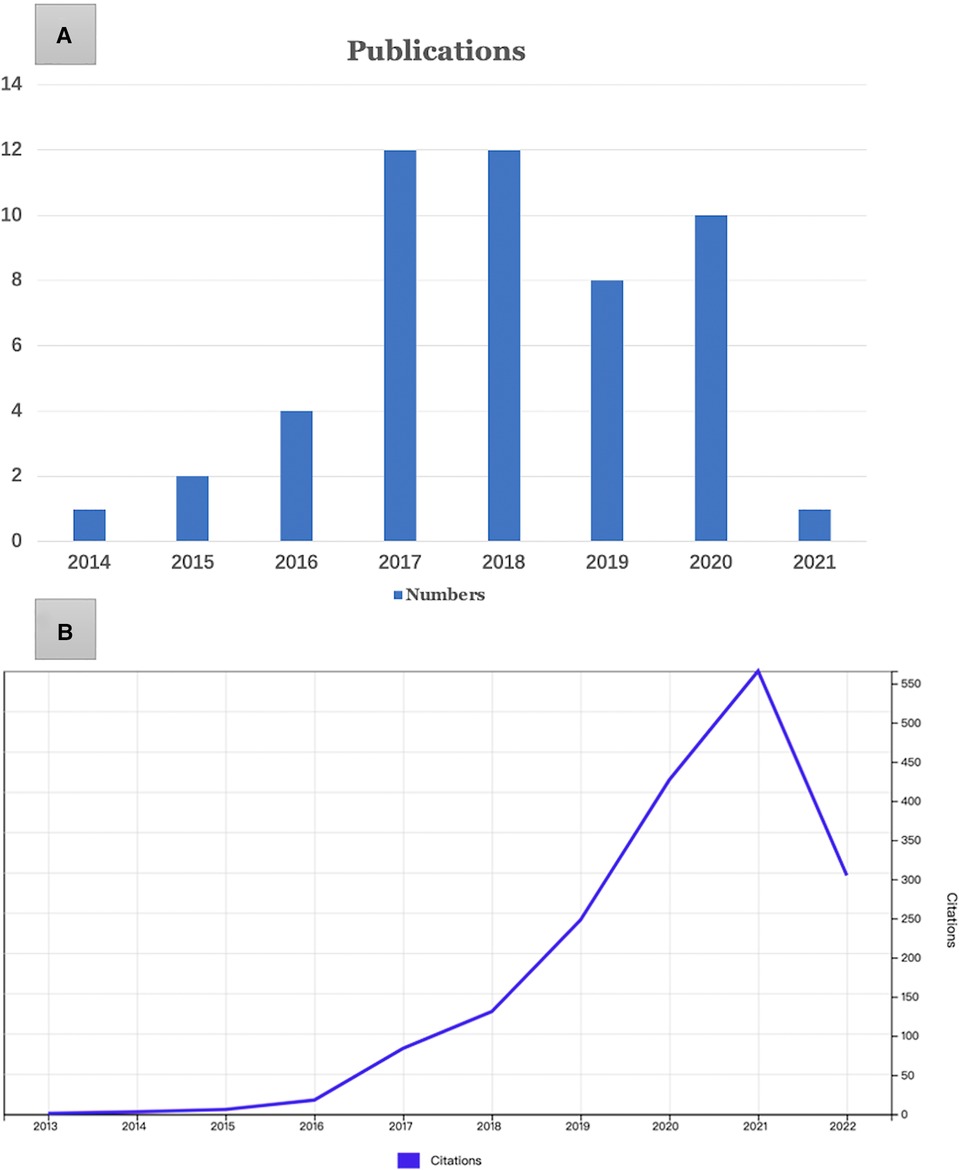
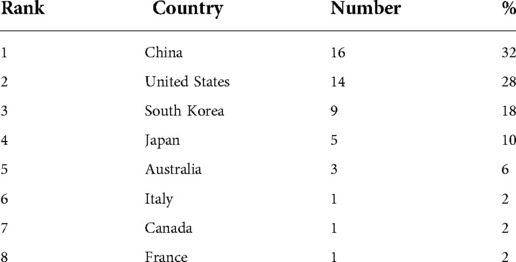
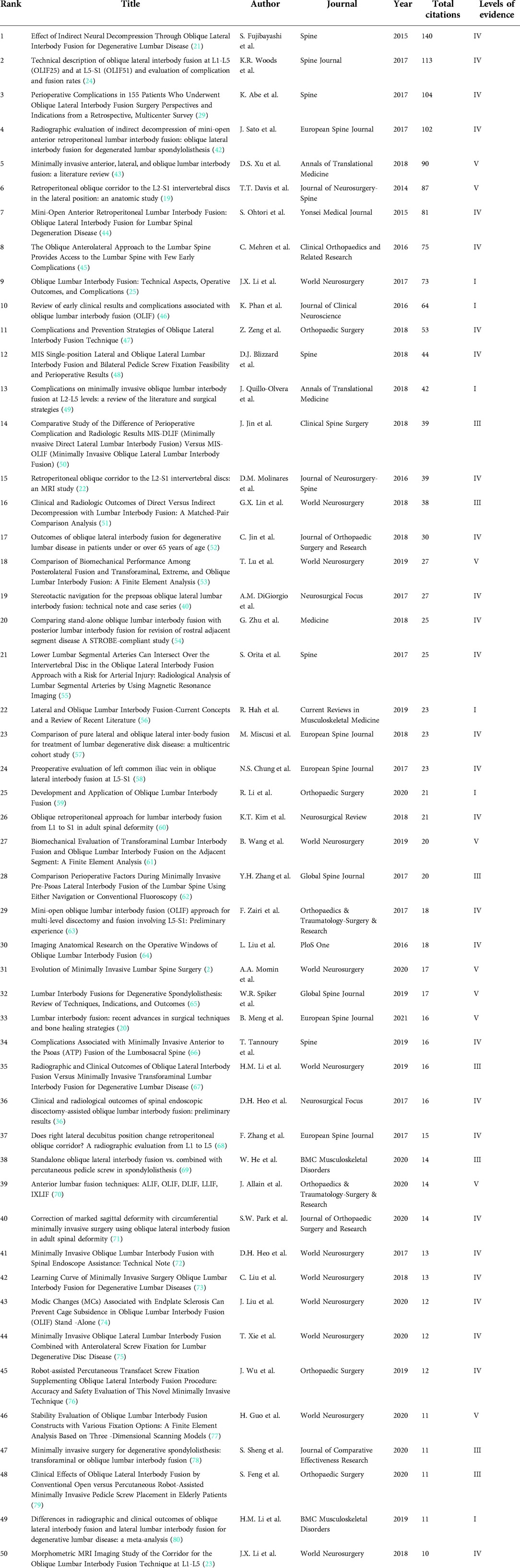
Initially, 629 papers were searched, and after careful screening, 236 of them were related to OLIF, and finally the 50 most cited OLIF-related publications were identified. All 50 most cited articles were published between 2014 and 2021 (Figure 1). The most productive period was from 2017 to 2020, with 41 articles. Of these articles, the oldest was published by T.T. Davis et al. (19), and the most recent was published by B. Meng et al. (20). The number of citations varied from 10 to 140, with an average of 35.52, and 1,776 citations were found. Among them, four articles had more than 100 citations. Among these publications, the most cited paper was the study by S. Fujibayashi et al. (21), entitled “Effect of Indirect Neural Decompression Through Oblique Lateral Interbody Fusion for Degenerative Lumbar Disease.” Table 1 shows the 50 most cited papers based on the number of citations to better present the details to the investigators.
The 50 most cited articles were published in 22 journals (Table 2), with World Neurosurgery contributing the most publications (n = 12), followed by European Spine Journal (n = 5), Spine (n = 5), and Orthopaedic Surgery (n = 4).

Table 2. Contributing institution of the 50 most cited articles on pre-psoas oblique lumbar interbody fusion.
Eight countries contributed to the 50 most cited papers in the OLIF field (Table 3). China was the primary contributor (n = 16), followed by the United States (n = 14), South Korea (n = 9), Japan (n = 5), Australia (n = 3), and France, Italy, and Australia (n = 1 for each). No shortage of multinational collaborative papers was observed.
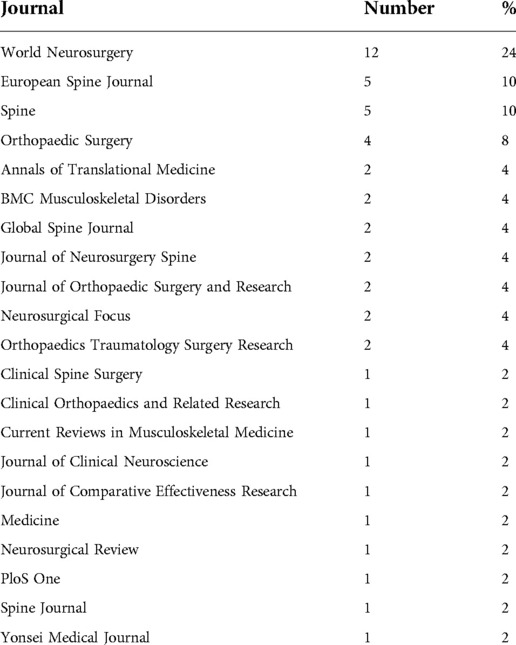
Table 3. Journal distribution of the 50 top cited articles on pre-psoas oblique lumbar interbody fusion.
Table 4 shows the institutions with >2 publications among the 50 most cited publications in the field of OLIF. The Catholic University of Korea (South Korea) produced the most publications (n = 6), followed by Chiba University (Japan) (n = 4), Beijing Jishuitan Hospital (n = 3), and University of New South Wales (n = 3).
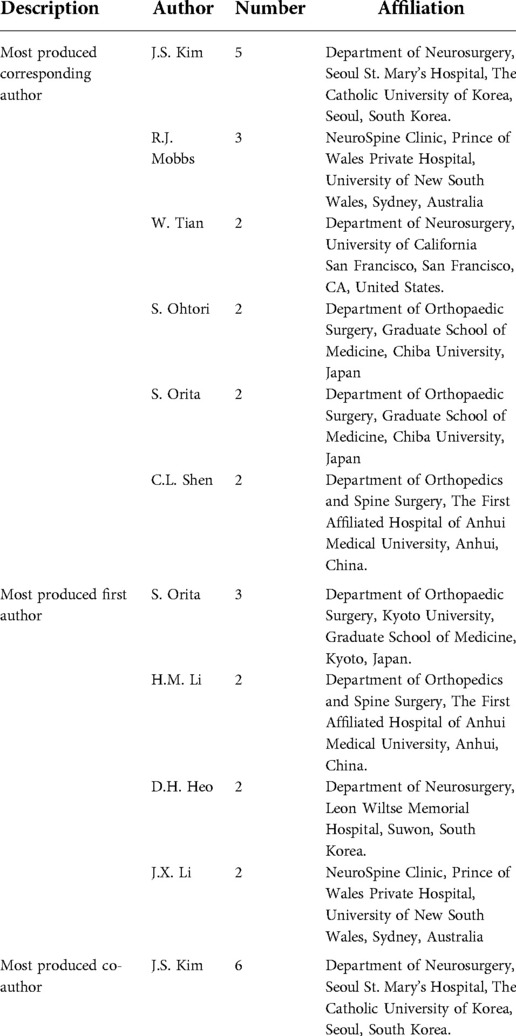
Table 4. Authors with multiple publications in the field of pre-psoas oblique lumbar interbody fusion.
Moreover, 272 authors contributed to the 50 most cited articles. Table 5 presents the first, last, and co-authors of the most cited articles. The corresponding author who produced the most publications was J.S. Kim (South Korea) (n = 5), and the first author who produced the most publications was S. Orita (Japan) (n = 3).
These articles were further classified according to the study design; 39 were original papers, and 11 were review studies. Furthermore, of these 39 original papers, 29 were research articles, seven were anatomical studies, and the remaining three were biomechanical studies.
The top 10 most cited keywords were (Figure 2A): “complications,” “decompression,” “spine,” “surgery,” “outcomes,” “transpsoas approach,” “spondylolisthesis,” “anterior,” “disease,” and “injury.” “Complications” is a recent research hotspot and emphasis (Figure 2B). As shown in the keyword density visualization (Figure 3), we could identify perioperative and postoperative complications, as well as clinical and radiological outcomes as the main research hotspots in this field.
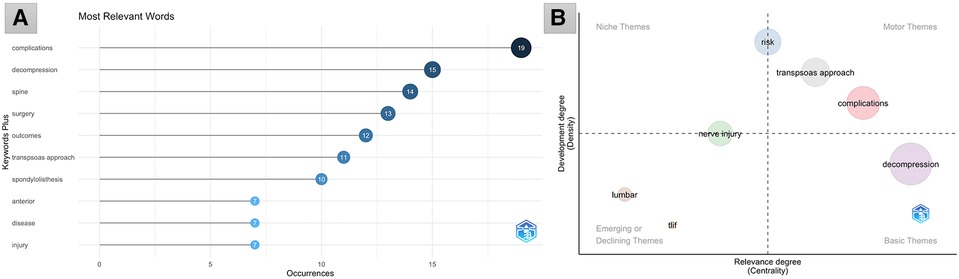
Figure 2. (A) The top 10 most cited keywords in the field of pre-psoas oblique lumbar interbody fusion. (B) Thematic map. Bottom right is the basic themes, top right is the motor themes, top left is the niche themes, bottom left is the emerging or declining themes.
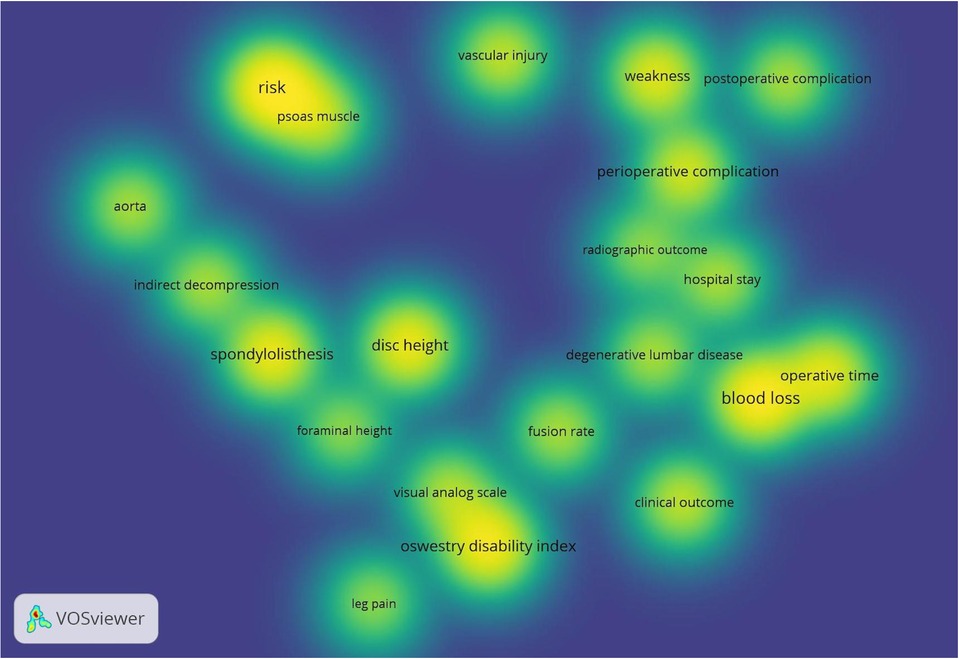
Figure 3. Density visualization map of keywords. The density magnitude depends on the number of elements in the surrounding area and the importance of those elements. The higher the density, the brighter the color; conversely, the lower the density, the lighter the color.
Discussion
The field of OLIF has greatly evolved in recent decades, and this study highlights the 50 most cited articles in this field. Considering the rapid growth of the publications in this day and age, the current screening of the 50 most cited papers in the field of OLIF is valuable for surgeons and researchers to keep them abreast of the most relevant articles, which helps better place the hotspots of this study and helps guide further research efforts in this field.
Among the 50 most cited papers, 29 were clinical research articles, seven were anatomical studies, three were biomechanical studies, and 11 were review articles. Of these 29 clinical studies, six were comparative studies between different techniques, such as two studies comparing OLIF with D/XLIF, three studies comparing OLIF with transforaminal lumbar interbody fusion (TLIF), and one study comparing OLIF with posterior lumbar interbody fusion. The remaining 23 research articles analyzed the clinical outcomes, radiological results, and complications of the OLIF technique. The other 11 review articles were non-meta-analyses in nature, and the authors collected and integrated a large amount of information and addressed it in these reviews, focusing on history, techniques, indications, outcomes, and complications.
Anatomical and radiological study of the feasibility of the OLIF access
Cadaveric study
In one study (19), anatomical data on the OLIF surgical window at L2–S1 were collected from 20 adult cadaveric specimens. The widths of the oblique corridor of the L2–S1 levels were measured in the lateral position, both at rest and with mild distraction of the psoas major muscle. At the L2–L5 level, in the static state, the oblique corridor was the narrowest at 15 mm in L4–L5 and the widest at 19.25 mm in L3–L4; in the mild distraction state, the access corridor increased in all levels, with the highest increase of 59.60% in L2–L3 and the least increase of 43.96% in L3–L4. The L5-S1 disk space is regularly accessible from an oblique angle with gentle iliac vascular retraction.
Radiological study
One researcher (22) conducted a magnetic resonance imaging (MRI) study of the width of the L2–S1 OLIF surgical window, which was measured on 100 adult MRI images. The measurements were taken in the static state, and the average width of the surgical window (left side) for each level from L2 to L5 was 16.04 mm for L2–L3, 14.21 mm for L3–L4, and 10.28 mm for L4–L5, and 10 mm for the L5–S1 lateral horizontal width and 10.13 mm for the longitudinal vertical width of the surgical window. Moreover, aortic bifurcation was found to mostly occur in the plane of the L4 vertebral body (43%), followed by the L4–L5 intervertebral disk (11%), the L5 vertebral body (9%), the L3–L4 intervertebral disk (5%), and the L3 vertebral body (2%). Furthermore, a low level of iliac vessel confluence was also found, with 45.9% confluence in the L4 vertebral plane, 19.4% in the L4–L5 intervertebral space, and 34.7% in the L5 vertebral body. In another paper (23), the authors measured the OLIF corridor on the right and left sides in 200 patients. The authors found that the right-side OLIF corridor was much narrower than the left-side one at the same level, indicating that a right-sided approach was less likely to be effective for OLIF.
Anatomical and radiological studies have confirmed the feasibility of the OLIF access; however, a few patients may have a narrow access corridor or anatomical variants; thus, a detailed preoperative examination and careful planning for each patient are required.
Indications and contraindications
The indications of OLIF have been reported in the literature, which included the following: diskogenic low back pain, lumbar spinal stenosis, lumbar segmental instability, spondylolisthesis, adjacent segmental disease, scoliosis, revision, disk space infection, trauma, and tumors. OLIF can be used for the fusion procedure in the L1–S1 levels; however, this procedure has been available for a short time, and few relevant studies are available, and its indications still need more clinical studies.
There are few reported contraindications to OLIF, which mainly included a history of abdominal surgery, severe obesity, and a narrow OLIF corridor. Furthermore, additional posterior decompression or osteotomy should be combined appropriately in patients with severe nerve root compression, severe spinal stenosis, moderate to severe spinal slippage, bony stenosis of the lateral recess, and moderate to severe rotational spinal deformity.
Clinical and radiological outcomes
Numerous previous studies and meta-analyses have affirmed OLIF surgical outcomes, such as intraoperative parameters (i.e., operating time, estimated blood loss, and hospital stay), clinical scores (i.e., visual analog scale [VAS] and Oswestry Disability Index [ODI]), and radiographic findings (i.e., restoration of disk height and foraminal height, correction of sagittal and coronal alignment, subsidence, and fusion rate). Woods et al. (24) reported that 137 patients underwent OLIF with an average intraoperative blood loss of 83.2 ml (range, 10–300 ml), and the fusion rate was 97.9% on computed tomography examination after 6 months. A recent meta-analysis included 16 studies (25), which resulted in a mean blood loss of 109.9 ml, a mean operative time of 95.2 min, a mean postoperative hospital stay of 6.3 days, and a postoperative fusion rate of 93%. We retrospectively analyzed the clinical results of 47 patients (62 levels) who underwent OLIF and found significant decreases in the mean VAS scores for back and leg pain, from 6.0 preoperatively to 2.3 postoperatively and from 6.9 preoperatively to 2.2 postoperatively, respectively (26). Simultaneously, the mean ODI decreased from 49.1 preoperatively to 26.5 postoperatively, with a 46.0% improvement (26). Furthermore, according to a recent meta-analysis (27), OLIF effectively corrects sagittal and coronal deformities, in the absence of posterior columnar osteotomy, with a significant difference in VAS and ODI between the preoperative and postoperative periods. Furthermore, the OLIF procedure for treating single-level spinal tuberculosis is more effective than anterior surgery alone, with less trauma and a lower complication rate (28). This may be because the OLIF procedure allows for the direct and complete removal of infectious pathologies from the anterior column and anterior column reconstruction, while using a minimally invasive surgical technique that lowers surgical morbidity.
Complications
A study (29) reported complications in 155 patients undergoing OLIF, of whom 75 (48.3%) had complications. The most common complications reported were endplate fracture and subsidence and transient low back weakness and thigh numbness at 18.7% and 13.5%, respectively. Other less frequent complications were segmental arterial injury, infection, and revision surgery. Another recent meta-analysis (25) reported intraoperative (1.5%) and postoperative complications (9.9%); the most common complications were transient thigh pain and/or numbness and hip flexion weakness (3.0% and 1.2%, respectively). Although OLIF via the prepsoas route is regarded as a generally safe technique, various perioperative and postoperative complications are unavoidable and should require special attention by the surgeon. Possible intraoperative complications of OLIF include the following: vascular injury, nerve injury, sympathetic chain injury, peritoneal and ureteral injury, poor cage position, and endplate violation (30). Possible postoperative complications include the following: buttock and/or thigh pain and/or weakness, superior mesenteric artery syndrome, postoperative ileus, intestinal obstruction, incisional hernia, surgical site or retroperitoneal infection, cage subsidence, and pseudarthrosis (31).
Vascular injury (abdominal vessels and segmental arteries)
It is the most serious intraoperative complication of OLIF surgery, and if it occurs, the consequences are unimaginable. Our recommendations are that preoperative imaging determines whether there is an adequate surgical window (OLIF corridor) and that the presence of anatomical variants in the great vessels should be assessed in the surgical area. Moreover, the breakthrough point should not be too far in front of the vertebral body when breaking through the contralateral annule ring. Furthermore, intraoperative hemostasis and neuroprotective measures are required. Regarding the corridor distance, some researchers suggest that this corridor is riskier in patients with a width < 1 cm; others consider that a slight dissection of the psoas major muscle is necessary to obtain a sufficient space for access placement, and overly demanding the width of the corridor is unnecessary.
Segmental arteries are also important vessels susceptible to injury. We recommend that the fixation nail of the OLIF spacer should be inserted as closely as possible to the proximal inferior endplate of the intervertebral space and that the segmental artery alignment area often overlaps with the inferior retraction baffle placement area; thus, placing the stabilizing nail in the superior retraction baffle only is safer. Furthermore, being gentle when installing the spacer and implanting the fixation nail under direct vision are important to ensure the safety of the segmental artery; after the fusion is implanted, the fixation nail and spacer should be withdrawn slowly to confirm that there is no obvious active bleeding.
Nerve injury (genitofemoral nerve, sympathetic chain, and lumbar plexus nerve)
Unlike traditional surgery, which requires the decompression of the spinal and nerve root canals and is prone to nerve damage, OLIF requires the stretching of the psoas major muscle, which can easily damage the lumbar plexus nerve, genitofemoral nerve and sympathetic nerve chain, resulting in symptoms, such as radicular pain and abnormal sensation in the lower extremities, numbness and weakness of the psoas major muscle and groin area, and even retrograde ejaculation. On the one hand, postoperative nerve injury symptoms are related to ischemic injury to the lumbar major psoas muscle and lumbar plexus nerves caused by the long duration of surgery and stretching. On the other hand, it can be caused by postoperative hematoma irritation. Generally, no specific treatment is needed, and postoperative recovery can be gradual.
Peritoneal and ureteral injury
Peritoneal injury is also one of the complications of OLIF because the peritoneum must be pulled forward when placing the tube. If the peritoneum is not pulled forward enough during the operation and the blunt tissue separation is not sufficient, the peritoneum will be embedded in the gap of the tube and the peritoneum will be torn.
The ureter is located posterior to the peritoneum and descends vertically into the pelvis along the anterior aspect of the medial lumbar major psoas muscle. Its ventral segment is anterior to the vertebral body or anterior to the psoas major muscle, and the ureter can be injured intraoperatively by traction or instrumentation. Ureteral injury can have serious consequences, such as hematuria and urinary extravasation. Therefore, when we establish the channel intraoperatively, we must not operate through the fat; otherwise, the ureter can be easily damaged later in the operation. The extraperitoneal fat must be pushed to the ventral side, and if some of the fat is left under the channel, it will increase the risk of ureteral injury. If ureteral injury occurs, surgical intervention must be performed immediately.
Cage subsidence
Mild cage subsidence is a process in which the cage and the upper and lower endplates adhere to each other. When the patient stands up after surgery, the cage is stressed by the endplate and settles to a certain extent so that the cage can make better contact with the upper and lower endplates, and this process results in a partial loss of disk height. Subsidence usually ends when the interface heals and is unlikely to cause serious consequences unless it leads to foraminal narrowing and nerve root compression. According to the previous studies (32–34), elderly, osteoporosis, severe multifidus muscle fatty degeneration, low Hounsfield units, concave endplate morphology, and higher cage height were all risk factors for OLIF subsidence. To avoid cage subsidence, we should choose a fusion device of the appropriate size; avoid intraoperative damage to the bony endplate; choose the appropriate indications; improve osteoporosis; and avoid premature weight-bearing. For patients with severe osteoporosis and significant lumbar instability, a combination of posterior percutaneous arch nail–rod system is required.
Nonunion
During OLIF surgery, the imperfect instrumentation of disk tissue removal can easily lead to the incomplete removal of disk tissue. Moreover, osteoporosis can accelerate bone graft resorption, inhibit and reduce new bone formation, and is harmful to bone fusion (20). Furthermore, cage subsidence is also a risk factor for nonunion (35).
Recent progress
OLIF is an indirect decompression procedure, and to overcome the indirect decompression effect of OLIF, some scholars have attempted to perform disk removal and endplate preparation under spinal endoscopic assistance, and the position of the interbody fusion cage can be assessed under direct vision, which also reduces radiation. Heo et al. (36) published the preliminary results of the OLIF technique with spinal endoscopic assistance (14; 18 segments) and showed that the average time for a single-level procedure is 120 min and that a significant postoperative improvement in preoperative VAS and ODI scores was observed, with the restoration of disk height and foraminal height and an increment of segmental lordosis and whole lumbar lordosis. Another recent article (37) reported the results of their full-endoscopic OLIF, showing significant relief of back and leg pain in all patients (20 patients; 22 levels) and complete interbody fusion in all segments after 1 year.
Recently, intraoperative navigation systems and robotic assistance have been increasingly used in OLIF, and there is also evidence that using these technologies can increase surgical precision and patient outcomes while lowering radiation exposure for surgeons and surgical personnel (38–41).
Limitations
Citation analysis is a popular bibliometric approach for analyzing scientific publications; however, it has numerous drawbacks. First, we only analyzed papers from journals indexed by the WoS; therefore, some novel papers related to OLIF may have been ignored and excluded from this study. Second, because papers were classified based on the number of citations, certain recent noteworthy papers in the area did not have enough opportunity to be referenced through other writers. As a result, some of the authors' innovative strategies and ideas may be overlooked. Third, only published articles were analyzed in this study. Other studies, such as recommendations, conferences, clinical guidelines, and case reports, may also provide useful insights in this area. Fourth, the self-citation phenomenon is also a factor in analyzing the drawbacks of literature research based on the number of citations. Finally, we included some studies involving few cases (at least 12 cases) in this study. However, these articles are also indispensable, as our goal is to provide a global and exhaustive analytical study of the literature in the field of OLIF.
Conclusions
This study spotlights the top 50 most cited articles in the OLIF field, which were subjected to a comprehensive bibliometric analysis, including the number of publications per year, number of citations, authors, journals, countries, and research topics. Clinical studies comprised the majority of the studies reviewed, followed by review articles and anatomical studies, and a few were biomechanical studies. Similar to most surgical procedures, the main research topics in the field of OLIF are focused on anatomical morphology, surgical techniques, indications, outcomes, and complications. Research has concentrated on complications, clinical outcomes and radiological outcomes. Complications are a recent research hotspot and focus. Despite the inherent limitations of bibliometric studies based on citation count, with the results of this review, we provide spine surgeons with research priorities and hotspots in the field of OLIF.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
GXL performed drafted the work; CMC performed methodology; SWJ performed the investigation and data curation; MTZ conceptualized or designed of the work; PL performed software; BSH helped with manuscript revisions;. All authors read and approved the final manuscript.
Funding
This research was funded by the Natural Science Foundation of Fujian Province, grant number 2021J05282; funded by the “Xiamen Health System Discipline Leaders and their Backup Candidates, Senior Management Talent Training Candidates Training Program”.
Acknowledgments
The author Guang-Xun Lin would like to give thanks for the “Xiamen Health High-Level Talent Training Program”.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. (2012) 6(2):89–97. doi: 10.4184/asj.2012.6.2.89
2. Momin AA, Steinmetz MP. Evolution of minimally invasive lumbar spine surgery. World Neurosurg. (2020) 140:622–6. doi: 10.1016/j.wneu.2020.05.071
3. Kai W, Cheng C, Yao Q, Zhang C, Jian F, Wu H. Oblique lumbar interbody fusion using a stand-alone construct for the treatment of adjacent-segment lumbar degenerative disease. Front Surg. (2022) 9:850099. doi: 10.3389/fsurg.2022.850099
4. Shao X, Li R, Zhang L, Jiang W. Enhanced recovery after surgery protocol for oblique lumbar interbody fusion. Indian J Orthop. (2022) 56(6):1073–82. doi: 10.1007/s43465-022-00641-4
5. Akbary K, Quillo-Olvera J, Lin GX, Jo HJ, Kim JS. Outcomes of minimally invasive oblique lumbar interbody fusion in patients with lumbar degenerative disease with rheumatoid arthritis. J Neurol Surg A Cent Eur Neurosurg. (2019) 80(3):162–8. doi: 10.1055/s-0038-1676301
6. Chung HW, Lee HD, Jeon CH, Chung NS. Comparison of surgical outcomes between oblique lateral interbody fusion (OLIF) and anterior lumbar interbody fusion (ALIF). Clin Neurol Neurosurg. (2021) 209:106901. doi: 10.1016/j.clineuro.2021.106901
7. Limthongkul W, Chantharakomen R, Tanasansomboon T, Yingsakmongkol W, Yoong-Leong Oh J, Kotheeranurak V, et al. Comparison of unremoved intervertebral disc location between 2 lateral lumbar interbody fusion (LLIF) techniques. World Neurosurg. (2022) 160:e322–e7. doi: 10.1016/j.wneu.2022.01.011
8. Walker CT, Farber SH, Cole TS, Xu DS, Godzik J, Whiting AC, et al. Complications for minimally invasive lateral interbody arthrodesis: a systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J Neurosurg Spine. (2019) 25:1–15. doi: 10.3171/2018.9.SPINE18800
9. Zhu HF, Fang XQ, Zhao FD, Zhang JF, Zhao X, Hu ZJ, et al. Comparison of oblique lateral interbody fusion (OLIF) and minimally invasive transforaminal lumbar interbody fusion (MI-TLIF) for treatment of lumbar degeneration disease: a prospective cohort study. Spine. (2022) 47(6):E233–E42. doi: 10.1097/BRS.0000000000004303
10. Shimizu T, Fujibayashi S, Otsuki B, Murata K, Matsuda S. Indirect decompression via oblique lateral interbody fusion for severe degenerative lumbar spinal stenosis: a comparative study with direct decompression transforaminal/posterior lumbar interbody fusion. Spine J. (2021) 21(6):963–71. doi: 10.1016/j.spinee.2021.01.025
11. Gan P, Fan W, Zhang H, Zhong C, Xia H, Lu M, et al. The top-cited articles with a focus on Barrett's Esophagus: a bibliometric analysis. Front Surg. (2022) 9:743274. doi: 10.3389/fsurg.2022.743274
12. Chen K, Zhao J, Yang Y, Wei X, Chen Z, Li M, et al. Global research trends of adult degenerative scoliosis in this decade (2010–2019): a bibliometric study. Eur Spine J. (2020) 29(12):2970–9. doi: 10.1007/s00586-020-06574-6
13. Tang K, Wan M, Zhang H, Zhang Q, Yang Q, Chen K, et al. The top 100 most-cited articles citing human brain banking from 1970 to 2020: a bibliometric analysis. Cell Tissue Bank. (2020) 21(4):685–97. doi: 10.1007/s10561-020-09849-w
14. Yin M, Xu C, Mo W. The 100 most cited articles on lumbar spinal stenosis: a bibliometric analysis. Global Spine J. (2022) 12(3):381–91. doi: 10.1177/2192568220952074
15. Wu H, Sun Z, Tong L, Wang Y, Yan H, Sun Z. Bibliometric analysis of global research trends on male osteoporosis: a neglected field deserves more attention. Arch Osteoporos. (2021) 16(1):154. doi: 10.1007/s11657-021-01016-2
16. Wu H, Cheng K, Tong L, Wang Y, Yang W, Sun Z. Knowledge structure and emerging trends on osteonecrosis of the femoral head: a bibliometric and visualized study. J Orthop Surg Res. (2022) 17(1):194. doi: 10.1186/s13018-022-03068-7
17. Lyu PF, Li JT, Deng T, Lin GX, Fan PM, Cao XC. Research trends and hotspots of breast cancer management during the COVID-19 pandemic: a bibliometric analysis. Front Oncol. (2022) 12:918349. doi: 10.3389/fonc.2022.918349
18. Bragg KM, Marchand GC, Hilpert JC, Cummings JL. Using bibliometrics to evaluate outcomes and influence of translational biomedical research centers. J Clin Transl Sci. (2022) 6(1):e72. doi: 10.1017/cts.2021.863
19. Davis TT, Hynes RA, Fung DA, Spann SW, MacMillan M, Kwon B, et al. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine. (2014) 21(5):785–93. doi: 10.3171/2014.7.SPINE13564
20. Meng B, Bunch J, Burton D, Wang J. Lumbar interbody fusion: recent advances in surgical techniques and bone healing strategies. Eur Spine J. (2021) 30(1):22–33. doi: 10.1007/s00586-020-06596-0
21. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine. (2015) 40(3):E175–82. doi: 10.1097/BRS.0000000000000703
22. Molinares DM, Davis TT, Fung DA. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs: an MRI study. J Neurosurg Spine. (2016) 24(2):248–55. doi: 10.3171/2015.3.SPINE13976
23. Julian Li JX, Mobbs RJ, Phan K. Morphometric MRI imaging study of the corridor for the oblique lumbar interbody fusion technique at L1-L5. World Neurosurg. (2018) 111:e678–e85. doi: 10.1016/j.wneu.2017.12.136
24. Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. (2017) 17(4):545–53. doi: 10.1016/j.spinee.2016.10.026
25. Li JX, Phan K, Mobbs R. Oblique lumbar interbody fusion: technical aspects, operative outcomes, and complications. World Neurosurg. (2017) 98:113–23. doi: 10.1016/j.wneu.2016.10.074
26. Lin GX, Rui G, Sharma S, Mahatthanatrakul A, Kim JS. The correlation of intraoperative distraction of intervertebral disc with the postoperative canal and foramen expansion following oblique lumbar interbody fusion. Eur Spine J. (2021) 30(1):151–63. doi: 10.1007/s00586-020-06604-3
27. Zhu L, Wang JW, Zhang L, Feng XM. Outcomes of oblique lateral interbody fusion for adult spinal deformity: a systematic review and meta-analysis. Global Spine J. (2022) 12(1):142–54. doi: 10.1177/2192568220979145
28. Zhuang QK, Li W, Chen Y, Bai L, Meng Y, Li Y, et al. Application of oblique lateral interbody fusion in treatment of lumbar spinal Tuberculosis in adults. Orthop Surg. (2021) 13(4):1299–308. doi: 10.1111/os.12955
29. Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine. (2017) 42(1):55–62. doi: 10.1097/BRS.0000000000001650
30. Zhang QY, Tan J, Huang K, Xie HQ. Minimally invasive transforaminal lumbar interbody fusion versus oblique lateral interbody fusion for lumbar degenerative disease: a meta-analysis. BMC Musculoskelet Disord. (2021) 22(1):802. doi: 10.1186/s12891-021-04687-7
31. Cheng C, Wang K, Zhang C, Wu H, Jian F. Clinical results and complications associated with oblique lumbar interbody fusion technique. Ann Transl Med. (2021) 9(1):16. doi: 10.21037/atm-20-2159
32. Hu Z, He D, Gao J, Zeng Z, Jiang C, Ni W, et al. The influence of endplate morphology on cage subsidence in patients with stand-alone oblique lateral lumbar interbody fusion (OLIF). Global Spine J. (2021) 9:2192568221992098. doi: 10.1177/2192568221992098
33. Wu H, Cheung JPY, Zhang T, Shan Z, Zhang X, Liu J, et al. The role of hounsfield unit in intraoperative endplate violation and delayed cage subsidence with oblique lateral interbody fusion. Global Spine J. (2021) 4:21925682211052515. doi: 10.1177/21925682211052515
34. Kotheeranurak V, Jitpakdee K, Lin GX, Mahatthanatrakul A, Singhatanadgige W, Limthongkul W, et al. Subsidence of interbody cage following oblique lateral interbody fusion: an analysis and potential risk factors. Global Spine J. (2021) 17:21925682211067210. doi: 10.1177/21925682211067210
35. Lin GX, Kotheeranurak V, Zeng TH, Mahatthanatrakul A, Kim JS. A longitudinal investigation of the endplate cystic lesion effect on oblique lumbar interbody fusion. Clin Neurol Neurosurg. (2019) 184:105407. doi: 10.1016/j.clineuro.2019.105407
36. Heo DH, Kim JS. Clinical and radiological outcomes of spinal endoscopic discectomy-assisted oblique lumbar interbody fusion: preliminary results. Neurosurg Focus. (2017) 43(2):E13. doi: 10.3171/2017.5.FOCUS17196
37. Li ZZ, Wang JC, Cao Z, Zhao HL, Lewandrowski KU, Yeung A. Full-Endoscopic oblique lateral lumbar interbody fusion: a technical note with 1-year follow-up. Int J Spine Surg. (2021) 15(3):504–13. doi: 10.14444/8072
38. Sardhara J, Singh S, Mehrotra A, Bhaisora KS, Das KK, Srivastava AK, et al. Neuro-navigation assisted pre-psoas minimally invasive oblique lumbar interbody fusion (MI-OLIF): new roads and impediments. Neurol India. (2019) 67(3):803–12. doi: 10.4103/0028-3886.263262
39. Gennari A, Gavotto A, Almairac F, Pelletier Y, Paquis P, Litrico S. Transfacet screws using spinal navigation in addition to anterior or oblique lumbar interbody fusion: technical note and preliminary results. Eur J Orthop Surg Traumatol. (2021) 31(7):1523–8. doi: 10.1007/s00590-021-02878-5
40. DiGiorgio AM, Edwards CS, Virk MS, Mummaneni PV, Chou D. Stereotactic navigation for the prepsoas oblique lateral lumbar interbody fusion: technical note and case series. Neurosurg Focus. (2017) 43(2):E14. doi: 10.3171/2017.5.FOCUS17168
41. Xi Z, Chou D, Mummaneni PV, Burch S. The navigated oblique lumbar interbody fusion: accuracy rate, effect on surgical time, and complications. Neurospine. (2020) 17(1):260–7. doi: 10.14245/ns.1938358.179
42. Sato J, Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Radiographic evaluation of indirect decompression of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for degenerated lumbar spondylolisthesis. Eur Spine J. (2017) 26(3):671–8. doi: 10.1007/s00586-015-4170-0
43. Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS. Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med. (2018) 6(6):104. doi: 10.21037/atm.2018.03.24
44. Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, et al. Mini-Open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J. (2015) 56(4):1051–9. doi: 10.3349/ymj.2015.56.4.1051
45. Mehren C, Mayer HM, Zandanell C, Siepe CJ, Korge A. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res. (2016) 474(9):2020–7. doi: 10.1007/s11999-016-4883-3
46. Phan K, Maharaj M, Assem Y, Mobbs RJ. Review of early clinical results and complications associated with oblique lumbar interbody fusion (OLIF). J Clin Neurosci. (2016) 31:23–9. doi: 10.1016/j.jocn.2016.02.030
47. Zeng ZY, Xu ZW, He DW, Zhao X, Ma WH, Ni WF, et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg. (2018) 10(2):98–106. doi: 10.1111/os.12380
48. Blizzard DJ, Thomas JA. MIS Single-position lateral and oblique lateral lumbar interbody fusion and bilateral pedicle screw fixation: feasibility and perioperative results. Spine. (2018) 43(6):440–6. doi: 10.1097/BRS.0000000000002330
49. Quillo-Olvera J, Lin GX, Jo HJ, Kim JS. Complications on minimally invasive oblique lumbar interbody fusion at L2-L5 levels: a review of the literature and surgical strategies. Ann Transl Med. (2018) 6(6):101. doi: 10.21037/atm.2018.01.22
50. Jin J, Ryu KS, Hur JW, Seong JH, Kim JS, Cho HJ. Comparative study of the difference of perioperative complication and radiologic results: MIS-DLIF (minimally invasive direct lateral lumbar interbody fusion) versus MIS-OLIF (minimally invasive oblique lateral lumbar interbody fusion). Clin Spine Surg. (2018) 31(1):31–6. doi: 10.1097/BSD.0000000000000474
51. Lin GX, Akbary K, Kotheeranurak V, Quillo-Olvera J, Jo HJ, Yang XW, et al. Clinical and radiologic outcomes of direct versus indirect decompression with lumbar interbody fusion: a matched-pair comparison analysis. World Neurosurg. (2018) 119:e898–909. doi: 10.1016/j.wneu.2018.08.003
52. Jin C, Jaiswal MS, Jeun SS, Ryu KS, Hur JW, Kim JS. Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J Orthop Surg Res. (2018) 13(1):38. doi: 10.1186/s13018-018-0740-2
53. Lu T, Lu Y. Comparison of biomechanical performance among posterolateral fusion and transforaminal, extreme, and oblique lumbar interbody fusion: a finite element analysis. World Neurosurg. (2019) 129:e890–e9. doi: 10.1016/j.wneu.2019.06.074
54. Zhu G, Hao Y, Yu L, Cai Y, Yang X. Comparing stand-alone oblique lumbar interbody fusion with posterior lumbar interbody fusion for revision of rostral adjacent segment disease: a STROBE-compliant study. Medicine (Baltimore). (2018) 97(40):e12680. doi: 10.1097/MD.0000000000012680
55. Orita S, Inage K, Sainoh T, Fujimoto K, Sato J, Shiga Y, et al. Lower lumbar segmental arteries can intersect over the intervertebral disc in the oblique lateral interbody fusion approach with a risk for arterial injury: radiological analysis of lumbar segmental arteries by using magnetic resonance imaging. Spine. (2017) 42(3):135–42. doi: 10.1097/BRS.0000000000001700
56. Hah R, Kang HP. Lateral and oblique lumbar interbody fusion-current concepts and a review of recent literature. Curr Rev Musculoskelet Med. (2019) 12(3):305–10. doi: 10.1007/s12178-019-09562-6
57. Miscusi M, Ramieri A, Forcato S, Giuffre M, Trungu S, Cimatti M, et al. Comparison of pure lateral and oblique lateral inter-body fusion for treatment of lumbar degenerative disk disease: a multicentric cohort study. Eur Spine J. (2018) 27(Suppl 2):222–8. doi: 10.1007/s00586-018-5596-y
58. Chung NS, Jeon CH, Lee HD, Kweon HJ. Preoperative evaluation of left common iliac vein in oblique lateral interbody fusion at L5-S1. Eur Spine J. (2017) 26(11):2797–803. doi: 10.1007/s00586-017-5176-6
59. Li R, Li X, Zhou H, Jiang W. Development and application of oblique lumbar interbody fusion. Orthop Surg. (2020) 12(2):355–65. doi: 10.1111/os.12625
60. Kim KT, Jo DJ, Lee SH, Seo EM. Oblique retroperitoneal approach for lumbar interbody fusion from L1 to S1 in adult spinal deformity. Neurosurg Rev. (2018) 41(1):355–63. doi: 10.1007/s10143-017-0927-8
61. Wang B, Hua W, Ke W, Lu S, Li X, Zeng X, et al. Biomechanical evaluation of transforaminal lumbar interbody fusion and oblique lumbar interbody fusion on the adjacent segment: a finite element analysis. World Neurosurg. (2019) 126:e819–e24. doi: 10.1016/j.wneu.2019.02.164
62. Zhang YH, White I, Potts E, Mobasser JP, Chou D. Comparison perioperative factors during minimally invasive Pre-psoas lateral interbody fusion of the lumbar spine using either navigation or conventional fluoroscopy. Global Spine J. (2017) 7(7):657–63. doi: 10.1177/2192568217716149
63. Zairi F, Sunna TP, Westwick HJ, Weil AG, Wang Z, Boubez G, et al. Mini-open oblique lumbar interbody fusion (OLIF) approach for multi-level discectomy and fusion involving L5-S1: preliminary experience. Orthop Traumatol Surg Res. (2017) 103(2):295–9. doi: 10.1016/j.otsr.2016.11.016
64. Liu L, Liang Y, Zhang H, Wang H, Guo C, Pu X, et al. Imaging anatomical research on the operative windows of oblique lumbar interbody fusion. PLoS One. (2016) 11(9):e0163452. doi: 10.1371/journal.pone.0163452
65. Spiker WR, Goz V, Brodke DS. Lumbar interbody fusions for degenerative spondylolisthesis: review of techniques, indications, and outcomes. Global Spine J. (2019) 9(1):77–84. doi: 10.1177/2192568217712494
66. Tannoury T, Kempegowda H, Haddadi K, Tannoury C. Complications associated with minimally invasive anterior to the psoas (ATP) fusion of the lumbosacral spine. Spine. (2019) 44(19):E1122–E9. doi: 10.1097/BRS.0000000000003071
67. Li HM, Zhang RJ, Shen CL. Radiographic and clinical outcomes of oblique lateral interbody fusion versus minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar disease. World Neurosurg. (2019) 122:e627–e38. doi: 10.1016/j.wneu.2018.10.115
68. Zhang F, Xu H, Yin B, Tao H, Yang S, Sun C, et al. Does right lateral decubitus position change retroperitoneal oblique corridor? A radiographic evaluation from L1 to L5. Eur Spine J. (2017) 26(3):646–50. doi: 10.1007/s00586-016-4645-7
69. He W, He D, Sun Y, Xing Y, Wen J, Wang W, et al. Standalone oblique lateral interbody fusion vs. Combined with percutaneous pedicle screw in spondylolisthesis. BMC Musculoskelet Disord. (2020) 21(1):184. doi: 10.1186/s12891-020-03192-7
70. Allain J, Dufour T. Anterior lumbar fusion techniques: aLIF, OLIF, DLIF, LLIF, IXLIF. Orthop Traumatol Surg Res. (2020) 106(1S):S149–S57. doi: 10.1016/j.otsr.2019.05.024
71. Park SW, Ko MJ, Kim YB, Le Huec JC. Correction of marked sagittal deformity with circumferential minimally invasive surgery using oblique lateral interbody fusion in adult spinal deformity. J Orthop Surg Res. (2020) 15(1):13. doi: 10.1186/s13018-020-1545-7
72. Heo DH, Choi WS, Park CK, Kim JS. Minimally invasive oblique lumbar interbody fusion with spinal endoscope assistance: technical note. World Neurosurg. (2016) 96:530–6. doi: 10.1016/j.wneu.2016.09.033
73. Liu C, Wang J. Learning curve of minimally invasive surgery oblique lumbar interbody fusion for degenerative lumbar diseases. World Neurosurg. (2018) 120:e88–93. doi: 10.1016/j.wneu.2018.07.167
74. Liu J, Ding W, Yang D, Wu H, Hao L, Hu Z, et al. Modic changes (MCs) associated with endplate sclerosis can prevent cage subsidence in oblique lumbar interbody fusion (OLIF) stand-alone. World Neurosurg. (2020) 138:e160–e8. doi: 10.1016/j.wneu.2020.02.047
75. Xie T, Wang C, Yang Z, Xiu P, Yang X, Wang X, et al. Minimally invasive oblique lateral lumbar interbody fusion combined with anterolateral screw fixation for lumbar degenerative disc disease. World Neurosurg. (2020) 135:e671–e8. doi: 10.1016/j.wneu.2019.12.105
76. Wu JY, Yuan Q, Liu YJ, Sun YQ, Zhang Y, Tian W. Robot-assisted percutaneous transfacet screw fixation supplementing oblique lateral interbody fusion procedure: accuracy and safety evaluation of this novel minimally invasive technique. Orthop Surg. (2019) 11(1):25–33. doi: 10.1111/os.12428
77. Guo HZ, Tang YC, Guo DQ, Luo PJ, Li YX, Mo GY, et al. Stability evaluation of oblique lumbar interbody fusion constructs with Various fixation options: a finite element analysis based on three-dimensional scanning models. World Neurosurg. (2020) 138:e530–e8. doi: 10.1016/j.wneu.2020.02.180
78. Sheng SR, Geng YB, Zhou KL, Wu AM, Wang XY, Ni WF. Minimally invasive surgery for degenerative spondylolisthesis: transforaminal or oblique lumbar interbody fusion. J Comp Eff Res. (2020) 9(1):45–51. doi: 10.2217/cer-2019-0055
79. Feng S, Tian W, Wei Y. Clinical effects of oblique lateral interbody fusion by conventional open versus percutaneous robot-assisted minimally invasive pedicle screw placement in elderly patients. Orthop Surg. (2020) 12(1):86–93. doi: 10.1111/os.12587
Keywords: anterior to psoas, citation analysis, most cited, oblique lumbar interbody fusion, prepsoas, OLIF
Citation: Lin G-X, Chen C-M, Jhang S-W, Zhu M-T, Lyu P and Hu B-S (2022) Characteristics and hotspots of the 50 most cited articles in the field of pre-psoas oblique lumbar interbody fusion. Front. Surg. 9:1004839. doi: 10.3389/fsurg.2022.1004839
Received: 27 July 2022; Accepted: 23 September 2022;
Published: 12 October 2022.
Edited by:
Gabriel Tender, Louisiana State University, United StatesReviewed by:
Tianwei Sun, Nankai University, ChinaAnthony DiGiorgio, University of California, United States
© 2022 Lin, Chen, Jhang, Zhu, Lyu and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bao-Shan Hu eG1oYnNAMjFjbi5jb20= Ming-Tao Zhu em10ZHl5eUAxNjMuY29t Pengfei Lyu c2t5MTI1NTg1MTE3QDE2My5jb20=
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Guang-Xun Lin
Guang-Xun Lin Chien-Min Chen
Chien-Min Chen Ming-Tao Zhu6*
Ming-Tao Zhu6* Pengfei Lyu
Pengfei Lyu