
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 02 November 2022
Sec. Neurosurgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.1002744
This article is part of the Research Topic Novel techniques and technologies in Spine Surgery: New approaches for the traumatic, oncologic, and aging Spine. View all 6 articles
 Guanzhang Mu1,†
Guanzhang Mu1,† Hao Chen2,†
Hao Chen2,† Haoyong Fu1
Haoyong Fu1 Shijun Wang1
Shijun Wang1 Hailin Lu1
Hailin Lu1 Xiaodong Yi1
Xiaodong Yi1 Chunde Li1
Chunde Li1 Lei Yue1
Lei Yue1 Haolin Sun1*
Haolin Sun1*
Objective: To assess the mid-long-term clinical and radiological outcomes of zero-profile (ZP) compared with stand-alone (ST) cages for two-level anterior cervical discectomy and fusion (ACDF).
Methods: We included 77 patients (39 women and 38 men) who underwent two-level ACDF between May 5, 2016, and May 5, 2020, and who were followed up for at least 1 year. The subjects were divided into the ST (n = 38) and ZP (n = 39) group. For the evaluation of functional status, Japanese Orthopedic Association (JOA), Neck Disability Index (NDI), and Visual Analogue Scale (VAS) scores were used. Additionally, radiological outcomes and procedure complications were observed at final follow-up.
Results: Both groups had excellent clinical outcomes at the final follow-up. There were no significant intergroup (ZP vs. ST) differences in the fusion rate (91.02% vs. 90.79%, P > 0.05) and postoperative dysphagia (15.4% vs. 2.6%, P = 0.108). However, the disc height at the final follow-up in the ZP group was higher than that in the ST group (6.86 ± 0.84 vs. 6.17 ± 1.03, P = 0.002). The ZP group accomplished a lower loss of cervical lordosis (18.46 ± 4.78 vs. 16.55 ± 4.36, P = 0.071), but without reaching statistical significance.
Conclusion: ACDF with either ZP or ST cages turns out to be a dependable strategy for two-level ACDF in terms of clinical results. However, compared with the ST, the ZP cage may achieve a significantly lower loss of disc height.
Anterior cervical discectomy and fusion (ACDF) decompresses compressed spinal cord and nerve root, recovers physiological lordosis, and provides stability and anatomical height of the intervertebral disc. The technique was initially developed for treating cervical spondylosis, and the efficacy and safety of using ACDF for treating patients with radiculopathy and myelopathy are excellent (1–3). Anterior cervical plate technique has been reported to increase the operation time and the risk of postoperative dysphagia (4). In contrast, non-plate interbody implants, the stand-alone (ST) cage and zero-profile (ZP) cage have been widely used for ACDF surgeries. The ST cage in ACDF has positive effects in terms of recovery of physiological disc height, rapid improvement of the cervical lordosis, and facilitation of joint fusion (1, 5). However, ST cages have been reported to cause complications like cage migration, subsidence, and revision surgery (6, 7). By contrast, immediate postoperative stabilization the core advantage of a ZP cage and an ACP system (8). Unlike the latter, the ZP cage has an additional anchoring function, which ensures less protrusion in front of the vertebral body, thereby placing less compression on the esophagus and ultimately decreasing the risk of postoperative dysphagia (9, 10). Due to the ability to overcome these disadvantages of the ST cage and ACP construct, the use of zero-profile cages in ACDF is gradually increasing.
For one-level ACDF, the ZP cage contributes to the improvements in neurological function and cervical lordosis, similar to those of the ST cage but with lower risk of implant failure (1, 10, 11). However, the number of current clinical articles comparing multi-level ACDF using ZP with that using ST is rare. Here, we aimed to explore comprehensive radiological and clinical outcomes in patients who had undergone two-level consecutive ACDF using ZP cages compared with those in whom ST cages were used.
This retrospective cohort study was conducted at Peking University First Hospital and received an approval from the local ethics committee (No. 2021133). Between May 5, 2016, and May 5, 2020, 166 patients were screened, of whom 77 (66.2% women and 33.8% men) were eligible. Intervertebral disc degeneration screening prior to surgery involved x-ray radiography, computed tomography (CT), and magnetic resonance imaging (MRI). We retrospectively collected patients aged at least 18 years with two-level consecutive ACDF between C3 and C7. ALL patients reported an intractable radiculopathy or myelopathy that lasted at least 6 weeks and was refractory to nonsurgical therapies, including physical therapy and anti-inflammatory drugs. Participants were excluded if they experienced nerve compression as a result of an acute trauma, tumor, infection, or other reason. Participants were also excluded if they had a history of cervical surgery or revision surgery. Depending on the device used for ACDF, the subjects were divided into the stand-alone cage (ST) group (n = 38) or the zero-profile (ZP) group (n = 39).
To expose the surgical segments, the right transversal incision was made in the supine posture of the patient. In most cases, the right transversal incision is sufficient. A distractor was utilized to access the lesioned intervertebral space after fluoroscopy had revealed that the area required decompression. During the process of decompression, nucleus pulposus and osteophytes were removed until we got satisfied decompression. When all the foregoing procedures were finished, ZP or ST cages were implanted. Intraoperative x-ray was used to verify that disc height and cervical alignment were restored, and to check all implants were in good position. For about 8 weeks after surgery, the patients were required to wear a cervical collar.
We collected the data regarding the surgical levels, operative time, blood loss, and patient's weight and height from the anesthesia records. All the participants had been instructed to fill out evaluations at the time of surgery, at 3-month intervals, and at the final follow-up. For the evaluation of functional status, Japanese Orthopedic Association (JOA), Neck Disability Index (NDI) (12), and the neck Visual Analogue Scale (VAS) pain scores were used. The prevalence of dysphagia was determined by utilizing the Bazaz system (Table 1) (13).
Cervical curvature, disc height, and subsidence were investigated based on the lateral cervical x-ray radiographs. The imaging examinations were completed after the operation (within 4 days), at postoperative 3 months, and every 6 months thereafter until the final follow-up. The Cobb angle of C2–C7 (between the lower endplate of C2 and the lower endplate of C7) was used to examine the cervical lordosis (14). The disc height (DHI) was defined as the distance between the highest section of the cephalad vertebra's lower endplate and the closest region of the caudal vertebra's upper endplate (14). Subsidence was defined as an intervertebral height reduction of more than 2 mm relative to that immediately after surgery (14). A solid fusion was present if the following features were observed: the lateral x-ray observation of cervical hyperextension curve showed that there was no abnormal activity between the fusion segment and the spinous process; x-ray images of cervical vertebra showed that the two ends of the fusion cage were tightly combined with the upper and lower contact surfaces of the vertebral body without transparent band; and bone connection and trabecular formation appeared on x-ray and CT. The presence of any two of the above conditions was marked as interbody fusion (15). To compensate for discrepancies in radiological measures, three qualified investigators separately examined radiological outcomes at least three times.
SPSS statistical software version 20.0 (IBM corp., Armonk, NY) was used for all analyses and calculations. In cases of continuous variables, the mean and standard deviation (SD) were used. Chi-square tests or Fisher's exact tests were used to compare categorical variables. To assess intergroup differences in numerical variables, the Student t test or Mann-Whitney U test was employed depending on compliance with a normal distribution or not. We utilized paired t tests to investigate the differences within the same group between different time points. Statistical significance level was set at P < 0.05.
A total of 77 patients (66.2% women and 33.8% men) were eventually included in this study. There were 39 patients (78 segments) in the ZP group and 38 patients (76 segments) in the ST group, of the 154 analyzed segments for which at least 1 year follow-up (mean 17.2 months, range 12–26 months) was completed. Sex, age, BMI, surgical levels, operative time, and intraoperative blood loss were not significantly different between the two groups (Table 2).
The descriptive statistics illustrating the clinical outcomes of the included patients are listed in Table 3. The two groups had a fairly equivalent neurologic enhancement and pain alleviation according to VAS, NDI, and JOA at all time points. However, compared with preoperative state, these indicators improved markedly at any time point following surgery (P < 0.05), both in the ZP group and in the ST group.
The descriptive statistics illustrating the radiological outcomes of the patients are listed in Table 4. The C2–C7 Cobb angle was used to measure cervical curvature. Although the Cobb angle of the ST and ZP groups declined with time, the C2–C7 Cobb angle in all patients was substantially improved at any point after treatment (P < 0.05, Table 4). At 3 months following surgery, the C2–C7 Cobb angle exhibited various degrees of decrease when compared to that immediately after the treatment. Figures 1, 2 depict the changes in C2–C7 Cobb angle over time. However, there were neither significant differences between various follow-up time points within the same group nor significant differences between the two groups at the same follow-up time points (Figure 3).
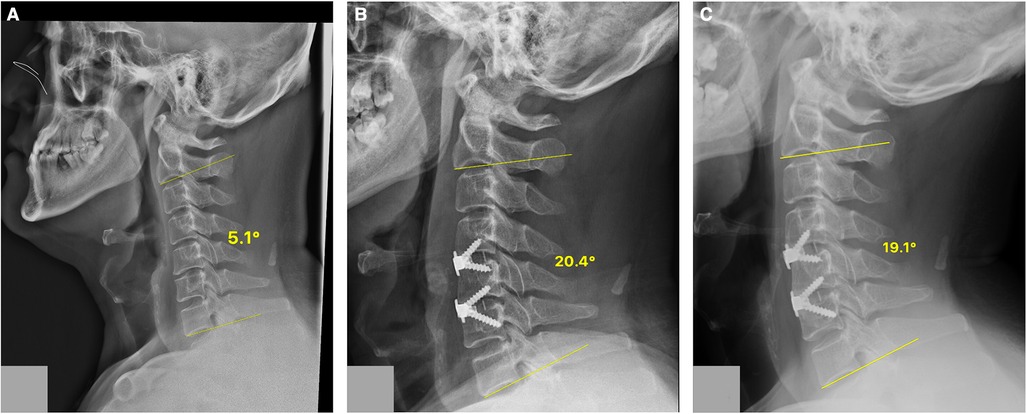
Figure 1. A case of the ZP group. Cervical lateral radiographs of a 47-year-old woman from the ZP cage group showing the C2–C7 Cobb angle at different time points. (A) 5.1° preoperatively; (B) 20.4° postoperatively; (C) 19.1° at the final follow-up. ZP, zero-profile cage.
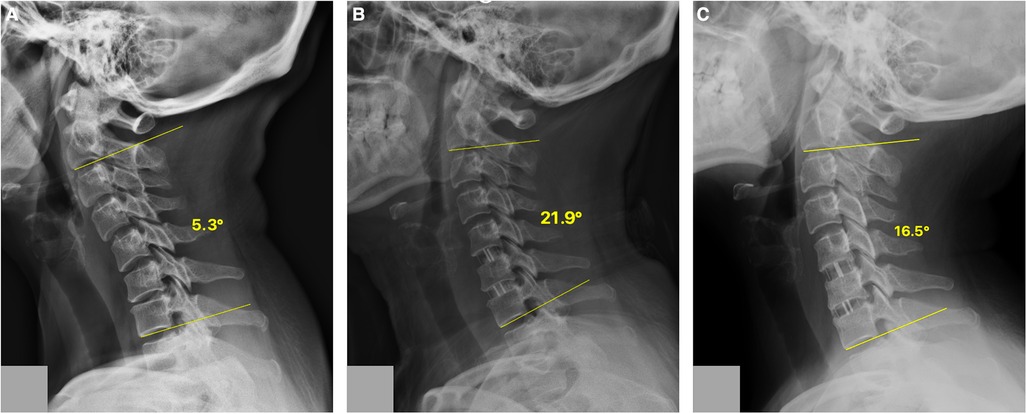
Figure 2. A case of the ST group. Cervical lateral radiographs of a 56-year-old woman from the ST group showing the C2–C7 Cobb angle at different time points. (A) 5.3° preoperatively; (B) 21.9° postoperatively; (C) 16.5° at the final follow-up. ST, stand-alone cage.

Figure 3. Variation of C2–C7 Cobb angle during the follow-up for ZP group and SC group. ZP, zero-P cage; ST, stand-alone cage; Preop, preoperative; Postop, postoperative. *P < 0.05, compared with preoperative value.
The descriptive statistics illustrating the DHI are listed in Table 4. After the procedure, the DHI of the treated segments recovered considerably, and there was a significant difference between the two groups at the last follow-up (Table 4). The average DHI declined steadily in both groups after surgery, but it dropped more rapidly and dramatically in the ST group, resulting in a significant difference in DHI at the last follow-up (P = 0.002) (Figure 4).
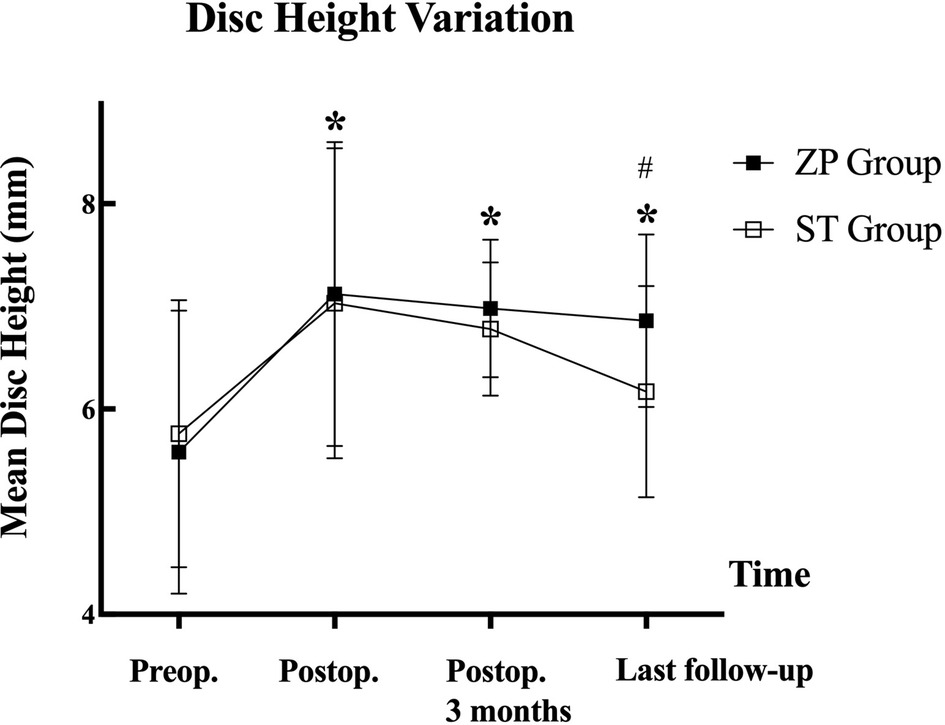
Figure 4. Changes of mean cervical disc height during the follow-up for ZP group and ST group. ZP, zero-P cage; ST, stand-alone cage; Preop, preoperative; Postop, postoperative. *P < 0.05, compared with preoperative value; #P < 0.05 significant difference between the two groups.
The fusion rates were 71/78 (91.02%) in the ZP group, and 69/76 (90.79%) in the ST group at the final follow-up (P > 0.05) (Table 4).
The descriptive statistics illustrating other complications are listed in Table 5. Dysphagia (n = 1), axial cervical discomfort (n = 1), and subsidence (n = 7) occurred in the ST group, while dysphagia (n = 6), axial cervical discomfort (n = 1), and subsidence (n = 6) occurred in the ZP group. Although postoperative consequences were comparable between the ZP and ST groups, we detected a substantial difference in transitory postoperative dysphagia (<3 months) (P = 0.108) (15.4% vs. 2.6%, respectively). Just one individual in the ZP group reported symptoms of dysphagia that lasted longer than 3 months, but the symptoms were mild.
ACDF, a gold standard for patients’ refractory to non-operative treatment, has shown efficacy to treat degenerative spine conditions (16, 17). Moreover, the ZP cage and ST cage are emphatic devices, with efficacy in disc reconstruction (15). Despite being technically easier and probably evading the risk factors of ACP, the use of ST and ZP cages in two-level ACDF has been associated with multiple intraoperative and postoperative complications. For example, decreased rigidity in extension, an increased risk of vertebral subsidence, and pseudoarthrosis have been reported (1, 15, 18). We documented the clinical and radiographic findings in two-level ACDF using the ZP and ST cages. Furthermore, we compared ZP and ST cages to clarify whether the ZP cage could achieve solid fusion and keep postsurgical clinical outcomes. Our results indicated that both groups had substantial improvements in VAS, NDI, and JOA ratings in the postoperative period, suggesting that ZP and ST could contribute to equal recovery of functional status, which is in accordance with previous evidence (19).
Cervical curvature is known to contribute to excellent clinical outcomes (10). After surgery, subsidence and the size of the cage may all have an impact on cervical curvature. A larger cage increases the intervertebral pressure and provides better axial stability of the cage, thus affecting the postoperative Cobb angle (20, 21). Nakanishi et al. (16) suggested that subsidence of the spacer affected the focal angle but did not alter the C2–C7 angle or the tilt angle. In our study, the ST and ZP groups both showed a substantial increase in the degree of cervical lordosis at the final follow-up, while both groups had substantial improvements in VAS, NDI, and JOA ratings in the postoperative period. In addition, a biomechanical study showed that cages with fixation provided greater structural strength than ST spacers for two and three levels, whereas single-level fixation provided equal stiffness (19, 22, 23). This may be the reason why there were variations in radiological measurements between single-level and mixed-level with ZP and ST cages.
The better clinical recovery was substantially more obvious in solid fusion, a condition that avoids delayed kyphotic deformity. For one-segment ACDF, several studies have found similar clinical outcomes in neurological recovery and fusion regardless of whether a ZP or ST cage was used (5, 24, 25). For two-segment ACDF, nine clinical studies included in a meta-analysis revealed that the usage of a ZP cage was associated with a 90% fusion rate after 36 months of follow-up (26). According to Sun et al. (10), radiological fusion was detected in 92.59% of the cases in the ZP group after a year, and all patients of the ZP group had complete fusion after 5 years. According to multi-level research by Li et al. (5), the usage of a ST cage resulted in a fusion rate of 91.7%. In our research, the ZP group had a higher fusion rate than the ST group, but the variations between the groups were too minor to be practically meaningful.
Subsidence occurs when the measured height at any of the two-disc heights decreases by more than 2 mm. Recent statistics reveal that postsurgical subsidence occurs most frequently within the first 3 months after the treatment (27, 28). The gap under the disc surface might decline due to natural or pathological processes during the fusing process. In general, the estimated range of the percentage of patients with subsidence following ACDF is between 0% and 40% (2, 29, 30). Bartels et al. (27) reported a subsidence rate of 19.1% after the usage of ZP cage. Wu et al. (18) reported a subsidence rate of up to 29.2% after utilizing ST cages. Even when the cage subsided, Opsenak et al. (28) showed that subsidence had no serious influence on the clinical outcome. A number of additional trials have shown comparable results (2, 30, 31). In our study, the incidence of interbody fusion cage subsidence in the ZP and ST groups was 7.7% and 9.5%, respectively. A higher rate of subsidence may explain the differential disc height loss in the ST group. Although the loss of disc height significantly differed between the groups, the patients’ mid-long-term clinical outcomes were, surprisingly, still rather excellent in both groups. Additionally, the disc height in patients with subsidence was substantially higher than before. Progressive subsidence of the cage might be caused by surgery, such as cervical fusion, as well as by the movement caused by the natural procedure itself, and poor bone mineral density.
Dysphagia is a frequently reported complaint of patients after ACDF; however, it is often temporary and self-limiting (10). Persistent and chronic dysphagia poses substantial medical nutritional concerns and may increase mortality. In recent studies (32, 33), it has been shown that dysphagia was more common in the ZP group than in the ST group. The frequency of post-ACDF dysphagia varies from 0% to 76% (34, 35), likely depending on how thoroughly investigators check for dysphagia following surgery. According to a prior study, there is a notable incidence of postoperative dysphagia (40.7%) and chronic dysphagia (3.7%) after ACDF with a ZP cage (10). The occurrence of dysphagia in our study is similar to that reported in the literature (2, 36, 37). The ST group showed a lower incidence of dysphagia both in the early postoperative period (<3 months) and at the final follow-up than the ZP group. It may becasuse the removal of the anterior plating in ST group reduces the irritation to the anterior cervical tissue and esophagus. It has been proved that the thickness of the cervical plate is related to dysphagia. Therefore, the ZP cage might not be a strategy to diminish dysphagia, which agrees with the reports by Albanese and Scholz. According to Albanese et al. (32), the prevalence of dysphagia was 20.8%; likewise, according to Scholz et al. (33), among patients with a ZP cage, 15% (3/20) reported a history of mild dysphagia. When compared with the documented occurrence of chronic dysphagia following placement of the ZP cage (33, 36), our occurrence of this condition was somewhat low. A variety of variables have been implicated in the development of dysphagia following ACDF, but the exact reasons remain unknown. According to prior research, dysphagia is more common with older age (3, 38), unfavorable postoperative C2–C7 angle (39), pre-pneumonectomy (40), two-level surgery (9, 41), long operation time (36), and greater prevertebral soft tissue swelling (9, 42). Further research on dysphagia mechanisms and techniques for reducing the occurrence of dysphagia are necessary.
The current study is limited by its retrospective nature and small sample size. Besides, the follow-up time was not long enough to demonstrate the mid-long-term impact of the ZP and ST cages for cervical degenerative disc disease. However, given there are few papers describing outcomes after ZP and ST cages for two-level ACDF, we believe this study provides helpful information about surgical intervention for cervical radiculopathy and myelopathy. To overcome the limitations and identify whether the ZP cage is better than the ST cage for ACDF, larger and prospective, randomized studies with long-term follow-up periods are needed.
ACDF with ZP cages is an effective and safe procedure for two-level cervical spondylosis. Compared with ST cages, ZP cages generate less disc height loss and fewer negative issues associated with cervical curvature.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
HS: design of the study, supervision, critically revising the article, acquisition of data. GM and HC: design of the study, investigation, acquisition of data, statistical analysis, writing—original draft. HF and SW: acquisition of data. SW, HL, XY, CL, HS, LY: operation. All authors: reviewed submitted version of manuscript. All authors contributed to the article and approved the submitted version.
This work was granted by Interdisciplinary clinical research project of Peking University First Hospital (identifier: 2021CR31).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ZP, zero-profile cage; ST, stand-alone cage; ACDF, anterior cervical discectomy and fusion; ACPS, anterior cervical plate; JOA, Japanese Orthopedic Association scores; NDI, Neck Disability Index; VAS, Visual Analogue Scale; CT, computed tomography; DHI, disc height; SD, standard deviation; BMI, body mass index
1. Li Z, Zhao Y, Tang J, Ren D, Guo J, Wang H, et al. A comparison of a new zero-profile, stand-alone fidji cervical cage and anterior cervical plate for single and multilevel ACDF: a minimum 2-year follow-up study. Eur Spine J. (2017) 26(4):1129–39. doi: 10.1007/s00586-016-4739-2
2. Lu Y, Bao W, Wang Z, Zhou Z, Zou F, Jiang J, Yang W, et al. Comparison of the clinical effects of zero-profile anchored spacer (ROI-C) and conventional cage-plate construct for the treatment of noncontiguous bilevel of cervical degenerative disc disease (CDDD): a minimum 2-year follow-up. Medicine. (2018) 97(5):e9808. doi: 10.1097/md.0000000000009808
3. Smith-Hammond CA, New KC, Pietrobon R, Curtis DJ, Scharver CH, Turner DA. Prospective analysis of incidence and risk factors of dysphagia in spine surgery patients: comparison of anterior cervical, posterior cervical, and lumbar procedures. Spine. (2004) 29(13):1441–6. doi: 10.1097/01.brs.0000129100.59913.ea
4. Vaishnav AS, Saville P, McAnany S, Patel D, Haws B, Khechen B, et al. Predictive factors of postoperative dysphagia in single-level anterior cervical discectomy and fusion. Spine. (2019) 44(7):E400–E07. doi: 10.1097/brs.0000000000002865
5. Li Z, Wang H, Li L, Tang J, Ren D, Hou S. A new zero-profile, stand-alone fidji cervical cage for the treatment of the single and multilevel cervical degenerative disc disease. J Clin Neurosci. (2017) 41:115–22. doi: 10.1016/j.jocn.2017.02.043
6. Fayed I, Conte AG, Keating G, Cobourn KD, Altshuler M, Makariou E, et al. Comparison of clinical and radiographic outcomes after standalone versus cage and plate constructs for anterior cervical discectomy and fusion. Int J Spine Surg. (2021) 15(3):403–12. doi: 10.14444/8060
7. Fujibayashi S, Neo M, Nakamura T. Stand-alone interbody cage versus anterior cervical plate for treatment of cervical disc herniation: sequential changes in cage subsidence. J Clin Neurosci. (2008) 15(9):1017–22. doi: 10.1016/j.jocn.2007.05.011
8. Li N, Wang R, Teng W, Yu J. Zero-profile versus cage-plate interbody fusion system in anterior cervical discectomy and fusion for the treatment of multilevel cervical spondylosis: a protocol of systematic review and meta-analysis. Medicine. (2020) 99(35):e22026. doi: 10.1097/md.0000000000022026
9. Huang C, Abudouaini H, Wang B, Ding C, Meng Y, Yang Y, et al. Comparison of patient-reported postoperative dysphagia in patients undergoing one-level versus two-level anterior cervical discectomy and fusion with the zero-P implant system. Dysphagia. (2021) 36(4):743–53. doi: 10.1007/s00455-020-10197-w
10. Sun B, Shi C, Wu H, Xu Z, Lin W, Shen X, et al. Application of zero-profile spacer in the treatment of three-level cervical spondylotic myelopathy: 5-year follow-up results. Spine. (2020) 45(8):504–11. doi: 10.1097/brs.0000000000003312
11. Virkar N, Bhilare P, Hadgaonkar S, Kothari A, Sancheti P, Aiyer S. Standalone cage versus anchored cage for anterior cervical discectomy and fusion: a comparative analysis of clinical and radiological outcomes. Int Orthop. (2022) 46(10):2339–45. doi: 10.1007/s00264-022-05493-z
12. Hoppenbrouwers M, Eckhardt MM, Verkerk K, Verhagen A. Reproducibility of the measurement of active and passive cervical range of motion. J Manipulative Physiol Ther. (2006) 29(5):363–7. doi: 10.1016/j.jmpt.2006.04.007
13. Sakai K, Yoshii T, Arai Y, Hirai T, Torigoe I, Inose H, et al. A prospective cohort study of dysphagia after subaxial cervical spine surgery. Spine. (2021) 46(8):492–98. doi: 10.1097/brs.0000000000003842
14. Li Z, Yu S, Zhao Y, Hou S, Fu Q, Li F, et al. Clinical and radiologic comparison of dynamic cervical implant arthroplasty versus anterior cervical discectomy and fusion for the treatment of cervical degenerative disc disease. J Clin Neurosci. (2014) 21(6):942–8. doi: 10.1016/j.jocn.2013.09.007
15. Gerszten PC, Paschel E, Mashaly H, Sabry H, Jalalod’din H, Saoud K. Outcomes evaluation of zero-profile devices compared to stand-alone PEEK cages for the treatment of three- and four-level cervical disc disease. Cureus. (2016) 8(9):e775. doi: 10.7759/cureus.775
16. Nakanishi Y, Naito K, Yamagata T, Masaki Yoshimura, Shimokawa N, Nishikawa M, et al. Safety of anterior cervical discectomy and fusion using titanium-coated polyetheretherketone stand-alone cages: multicenter prospective study of incidence of cage subsidence. J Clin Neurosci. (2020) 74:47–54. doi: 10.1016/j.jocn.2020.01.056
17. Pereira EA, Chari A, Hempenstall J, Leach JC, Chandran H, Cadoux-Hudson TA. Anterior cervical discectomy plus intervertebral polyetheretherketone cage fusion over three and four levels without plating is safe and effective long-term. J Clin Neurosci. (2013) 20(9):1250–5. doi: 10.1016/j.jocn.2012.10.028
18. Wu WJ, Jiang LS, Liang Y, et al. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J. (2012) 21(7):1374–82. doi: 10.1007/s00586-011-2131-9
19. Scholz M, Schleicher P, Pabst S, Dai LY. A zero-profile anchored spacer in multilevel cervical anterior interbody fusion: biomechanical comparison to established fixation techniques. Spine. (2015) 40(7):E375–80. doi: 10.1097/brs.0000000000000768
20. Igarashi H, Hoshino M, Omori K, Matsuzaki H, Nemoto Y, Tsuruta T, et al. Factors influencing interbody cage subsidence following anterior cervical discectomy and fusion. Clin Spine Surg. (2019) 32(7):297–302. doi: 10.1097/bsd.0000000000000843
21. Shi S, Liu ZD, Li XF, Qian L, Zhong GB, Chen FJ, et al. Comparison of plate-cage construct and stand-alone anchored spacer in the surgical treatment of three-level cervical spondylotic myelopathy: a preliminary clinical study. Spine J. (2015) 15(9):1973–80. doi: 10.1016/j.spinee.2015.04.024
22. Kinon MD, Greeley SL, Harris JA, Gelfand Y, Yassari R, Nakhla J, et al. Biomechanical evaluation comparing zero-profile devices versus fixed profile systems in a cervical hybrid decompression model: a biomechanical in vitro study. Spine J. (2020) 20(4):657–64. doi: 10.1016/j.spinee.2019.10.004
23. Paik H, Kang DG, Lehman RA, Cardoso MJ, Gaume RE, Ambati DV, et al. Do stand-alone interbody spacers with integrated screws provide adequate segmental stability for multilevel cervical arthrodesis? Spine J 2014;14(8):1740–7. doi: 10.1016/j.spinee.2014.01.034
24. Li T, Yang JS, Wang XF, Meng CY, Wei JM, Wang YX, et al. Can zero-profile cage maintain the cervical curvature similar to plate-cage construct for single-level anterior cervical diskectomy and fusion? World Neurosurg. (2020) 135:e300–e06. doi: 10.1016/j.wneu.2019.11.153
25. Noh SH, Zhang HY. Comparison among Perfect-C®, Zero-P®, and plates with a cage in single-level cervical degenerative disc disease. BMC Musculoskelet Disord. (2018) 19(1):33. doi: 10.1186/s12891-018-1950-9
26. Lu VM, Mobbs RJ, Fang B, Phan K. Clinical outcomes of locking stand-alone cage versus anterior plate construct in two-level anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur Spine J. (2019) 28(1):199–208. doi: 10.1007/s00586-018-5811-x
27. Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. (2006) 58(3):502–8; discussion 2–8. doi: 10.1227/01.Neu.0000197258.30821.50
28. Opsenak R, Hanko M, Snopko P, Varga K, Kolarovszki B. Subsidence of anchored cage after anterior cervical discectomy. Bratisl Lek Listy. (2019) 120(5):356–61. doi: 10.4149/bll_2019_058
29. Lonjon N, Favreul E, Huppert J, Lioret E, Delhaye M, Mraidi R, et al. Clinical and radiological outcomes of a cervical cage with integrated fixation. Medicine. (2019) 98(3):e14097. doi: 10.1097/md.0000000000014097
30. Ng EP, Yip AS, Wan KH, Tse MS, Wong KK, Kwok TK, et al. Stand-alone cervical cages in 2-level anterior interbody fusion in cervical spondylotic myelopathy: results from a minimum 2-year follow-up. Asian Spine J. (2019) 13(2):225–32. doi: 10.31616/asj.2018.0193
31. Shiban E, Nies M, Kogler J, Kogler L, da Cunha PR, Meyer B, et al. No correlation between radiological and clinical outcome 1 year following cervical arthrodesis. Acta Neurochir. (2018) 160(4):845–53. doi: 10.1007/s00701-018-3495-y
32. Albanese V, Certo F, Visocchi M, Barbagallo G. Multilevel anterior cervical diskectomy and fusion with zero-profile devices: analysis of safety and feasibility, with focus on sagittal alignment and impact on clinical outcome: single-institution experience and review of literature. World Neurosurg. (2017) 106:724–35. doi: 10.1016/j.wneu.2017.06.051
33. Scholz M, Onal B, Schleicher P, Pingel A, Hoffmann C, Kandziora F, et al. Two-level ACDF with a zero-profile stand-alone spacer compared to conventional plating: a prospective randomized single-center study. Eur Spine J. (2020) 29(11):2814–22. doi: 10.1007/s00586-020-06454-z
34. Hofstetter CP, Kesavabhotla K, Boockvar JA. Zero-profile anchored spacer reduces rate of dysphagia compared with ACDF with anterior plating. J Spinal Disord Tech. (2015) 28(5):E284–90. doi: 10.1097/BSD.0b013e31828873ed
35. Yang Y, Ma L, Liu H, Xu M. A meta-analysis of the incidence of patient-reported dysphagia after anterior cervical decompression and fusion with the zero-profile implant system. Dysphagia. (2016) 31(2):134–45. doi: 10.1007/s00455-015-9681-7
36. Lu Y, Fang Y, Shen X, Lu D, Zhou L, Gan M, Zhu X. Does zero-profile anchored cage accompanied by a higher postoperative subsidence compared with cage-plate construct? A meta-analysis. J Orthop Surg Res. (2020) 15(1):189. doi: 10.1186/s13018-020-01711-9
37. Zhu D, Zhang D, Liu B, Li C, Zhu J. Can self-locking cages offer the same clinical outcomes as anterior cage-with-plate fixation for 3-level anterior cervical discectomy and fusion (ACDF) in mid-term follow-up? Med Sci Monit. (2019) 25:547–57. doi: 10.12659/msm.911234
38. Yang Y, Ma L, Liu H, Liu Y, Hong Y, Wang B, et al. Comparison of the incidence of patient-reported post-operative dysphagia between ACDF with a traditional anterior plate and artificial cervical disc replacement. Clin Neurol Neurosurg. (2016) 148:72–8. doi: 10.1016/j.clineuro.2016.07.020
39. Huang CY, Meng Y, Wang BY, Yu J, Ding C, Yang Y, et al. The effect of the difference in C(2-7) angle on the occurrence of dysphagia after anterior cervical discectomy and fusion with the zero-P implant system. BMC Musculoskelet Disord. (2020) 21(1):649. doi: 10.1186/s12891-020-03691-7
40. Fisahn C, Schmidt C, Rustagi T, Moisi M, Iwanaga J, Norvell DC, et al. Comparison of chronic dysphagia in standalone versus conventional plate and cage fusion. World Neurosurg. (2018) 109:e382–e88. doi: 10.1016/j.wneu.2017.09.188
41. Fengbin Y, Xinwei W, Haisong Y, et al. Dysphagia after anterior cervical discectomy and fusion: a prospective study comparing two anterior surgical approaches. Eur Spine J. (2013) 22(5):1147–51. doi: 10.1007/s00586-012-2620-5
Keywords: anterior cervical discectomy and fusion (ACDF) surgery, cervical spine, disc herniation, outcome, stand-alone cage, zero-profile cage, two-level cervical spondylosis
Citation: Mu G, Chen H, Fu H, Wang S, Lu H, Yi X, Li C, Yue L and Sun H (2022) Anterior cervical discectomy and fusion with zero-profile versus stand-alone cages for two-level cervical spondylosis: A retrospective cohort study. Front. Surg. 9:1002744. doi: 10.3389/fsurg.2022.1002744
Received: 25 July 2022; Accepted: 13 October 2022;
Published: 2 November 2022.
Edited by:
Alessandro Pesce, Hospital Santa Maria Goretti, ItalyReviewed by:
Ahmed Khalifa, South Valley University, Egypt© 2022 Mu, Chen, Fu, Wang, Lu, Yi, Li, Yue and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Haolin Sun c3VuaGFvbGluQHZpcC4xNjMuY29t
†These authors share first authorship
Specialty Section: This article was submitted to Neurosurgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.