- Department of Orthopedics, The First Affiliated Hospital of Nanchang University, Artificial Joints Engineering and Technology Research Center of Jiangxi Province, Nanchang, China
Objective: The purpose of this study was to analyze the risk factors for limb fracture non-union in order to improve non-union prevention and early detection.
Methods: A total of 223 patients with non-union after surgery for limb fractures performed at our institution from January 2005 to June 2017 were included as the case group, while a computer-generated random list was created to select 446 patients with successful bone healing after surgery for limb fractures who were treated during the same period as the control group, thus achieving a ratio of 1:2. The medical records of these patients were reviewed retrospectively. Age, sex, body mass index, obesity, smoking, alcohol, diabetes, hypertension, osteoporosis, fracture type, multiple fractures, non-steroidal anti-inflammatory drugs (NSAIDs) use, delayed weight bearing, internal fixation failure, and infection data were analyzed and compared between the two groups. A multivariate logistic regression model was constructed to determine relevant factors associated with non-union.
Results: After comparison between two groups by univariate analysis and multivariate logistic regression, we found some risk factors associated that osteoporosis (odds ratio [OR] = 3.16, 95% confidence interval [CI]: 2.05–4.89, p < 0.001), open fracture (OR = 2.71, 95%CI: 1.72–4.27, p < 0.001), NSAIDs use (OR = 2.04, 95%CI: 1.24–3.37, p = 0.005), delayed weight bearing (OR = 1.72, 95%CI: 1.08–2.74, p = 0.023), failed internal fixation (OR = 5.93, 95%CI: 2.85–12.36, p < 0.001), and infection (OR = 6.77, 95%CI: 2.92–15.69, p < 0.001) were independent risk factors for non-union after surgery for limb fractures.
Conclusions: Osteoporosis, open fracture type, NSAIDs use, delayed weight bearing, failed internal fixation, and infection were found to be the main causes of bone non-union; clinicians should, therefore, take targeted measures to intervene in high-risk groups early.
Introduction
Recently, the number of patients with successful callus formation after fracture surgical management has decreased, with 5–10% of non-union cases leading to worrying outcomes (1, 2). The loss of productivity caused by a long healing process affects patients, healthcare systems, and the economy (3). It is estimated that 100,000 fracture cases show non-union in the United States each year, with the cost of non-union complications being close to $12,000 per patient (4, 5). In addition, in the United Kingdom, the cost of treating non-union is estimated at £7,000 to £79,000, but these figures relate only to the cost of hospitalization (6, 7), which indicates that a large amount of medical resources are consumed each year in non-union cases.
Risk factors can determine which patients may benefit from more active interventions among those who tend to develop non-union, and a clear idea of the risk of non-union may help to choose between competing treatment options (8). Identifying these factors will enable surgeons to identify high-risk cases before surgery in order to implement measures to promote healing, such as more comprehensive metabolic examinations, medical interventions, early bone grafting, and the use of osteoinductive agents and bone stimulants (9). Furthermore, these findings will help surgeons consult on the anticipated outcomes of such patients. Bone non-union is a multifactorial disease, and it is considered that the coexistence of different risk factors is crucial to its occurrence. A series of factors have been considered to be the causes of non-union, which can be divided into two main categories: (1) patient-related factors (8), including age and sex, body mass index (BMI), obesity, smoking, alcohol, and medical history of diabetes, hypertension, and osteoporosis; and (2) injury characteristics and treatment-related factors (10), including fracture type, use of non-steroidal anti-inflammatory drugs (NSAIDs), delayed weight bearing, mechanical instability resulting in internal fixation failure, and infection.
Until now, although a large number of studies have been conducted to analyze the multiple risk factors involved in the development of fracture non-union, they are limited by small sample sizes and incomplete potential risk factors (11–14). Moreover, clinical trials have shown that changes in the rate of non-union are related to different surgical treatments (15, 16). However, the above factors cannot fully explain the occurrence of non-union. Most of these studies reported fractures at specific sites, such as the humerus, femur, or tibia, or were limited to one type of non-union, such as that caused only by biological or treatment-related factors, without a systematic and global analysis that is required for limb fractures.
The purpose of this study was, therefore, to investigate the association between the occurrence of non-union after surgery for limb fractures and patient-, injury-, and treatment-related factors. A thorough understanding of these factors and their relative impact may provide better insight into the causes of non-union and the required treatment. Modifiable factors, such as use of NSAIDs and delayed weight bearing, should be strictly evaluated to optimize the patient prognosis.
Materials and Methods
Research Data
We retrospectively analyzed 223 patients with bone non-union after surgery for limb fractures in our institution from January 2005 to June 2017 (case group), and created a computer-generated random list to select 446 patients with successful bone healing after surgery for limb fractures (control group), thus achieving a case-control ratio of 1:2. Both groups of patients were treated during the same period. The present study was approved by the Ethics Committee of the First Affiliated Hospital of Nanchang University.
Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (i) meeting the diagnostic criteria for bone non-union for the case group: fracture not completely healed within 9 months after injury and showing no progression toward healing on radiographs for 3 consecutive months; (ii) a clear history of trauma and (iii) fracture of the humerus, ulna, radius, femur, tibia, or fibula. The exclusion criteria were as follows: (i) comorbid severe loss of other major organs, severe malnutrition, or malignant disease; (ii) severe bone defect requiring bone grafting and (iii) incomplete clinical data.
Criteria of Related Risk Factors and Data Collection
All cases of limb fractures were treated surgically by experienced doctors in our institution. Postsurgically, the use of NSAIDs such as flurbiprofen and celecoxib was decided according to the patients' pain. Delayed weight bearing was defined as starting weight bearing more than 12 weeks after surgery, and failure of internal fixation was defined as screw loosening, screw fracture, plate fracture, intramedullary nail fracture, and internal fixation rejection. Additionally, all patients were followed up at least 9 months after surgery, which included clinical data and X-ray examinations to observe wound healing, internal fixation, fracture healing, and joint function. The collected patient-related data included age, sex, BMI, obesity, smoking, alcohol, diabetes, hypertension, osteoporosis, fracture type, multiple fractures, use of NSAIDs, delayed weight bearing, failed internal fixation, and infection to further analyze risk factors for non-union.
Statistical Analyses
Continuous variable data are presented as mean ± standard deviation, and discrete variable data are presented as frequencies. The Shapiro-Wilk test was used to test the normality of continuous variables, and the independent-samples t-test was used to compare differences in age and BMI between the case and the control groups. The chi-square test and Spearman correlation coefficient were used to test and analyze differences in other data. The most significant risk factors for bone non-union were analyzed by univariate analysis, and then the risk factors with P < 0.05 were analyzed by Logistic regression analysis. All the above analyses were carried out using SPSS 26.0 statistical software (IBM Corp., Armonk, NY, USA). P < 0.05 were considered statistically significant.
Results
General Characteristics
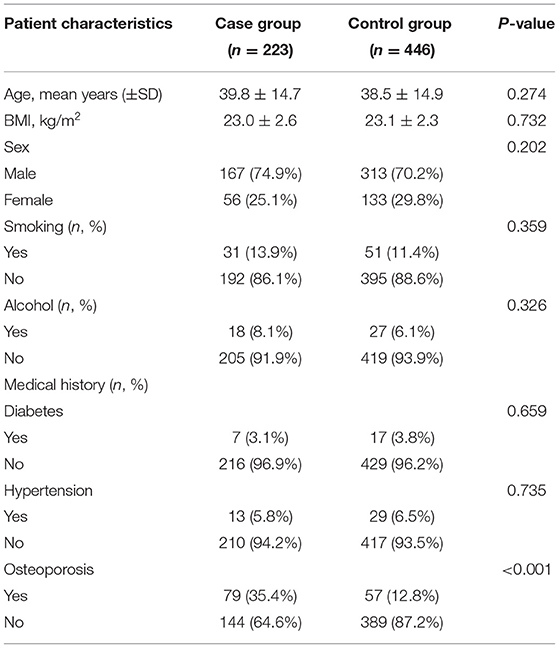
As shown in Table 1, there were 223 patients in the case group with an average age of 39.8 ± 14.7 years (167 males and 56 females) and 446 patients in the control group with an average age of 38.5 ± 14.9 years (313 males and 133 females). There was no significant difference in average age and sex ratio between the two groups. The average BMI of patients in the case group was higher than that of patients in the control group (23.0 ± 2.6 kg/m2 vs. 23.1 ± 2.3 kg/m2), but this difference was not significant (P = 0.732). There were also no significant differences in smoking, alcohol, diabetes, and hypertension between the two groups (Table 1). Conversely, the proportion of patients with a history of osteoporosis was significantly higher in the case group than in the control group [35.4% (79/223) vs. 12.8% (57/446); P < 0.001].
Follow-Up Results
All patients were followed up for at least 9 months after surgery, including clinical data, especially x-ray examinations to observe whether the fracture has healed. As shown in Figures 1–3, the typical imaging follow-up data of three typical non-union and union after surgery for limb fractures.
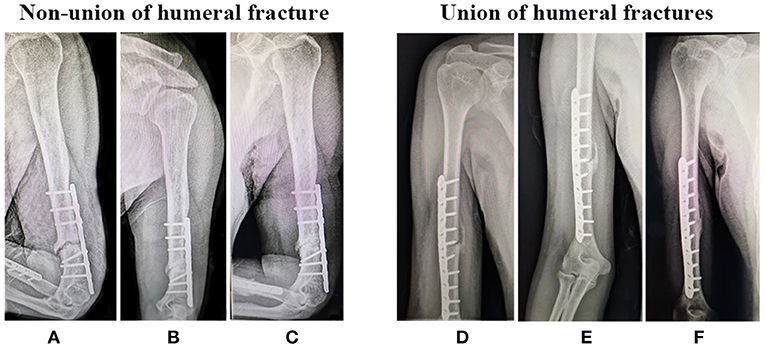
Figure 1. Non-union and Union of humeral fractures after surgery, respectively. X-ray examination (A,D) 1 month, (B,E) 3 month, and (C,F) 9 month after surgery.

Figure 2. Non-union and Union of radius fracture after surgery. X-ray examination (A,D) 1 month, (B,E) 3 month, and (C,F) 9 month after surgery.
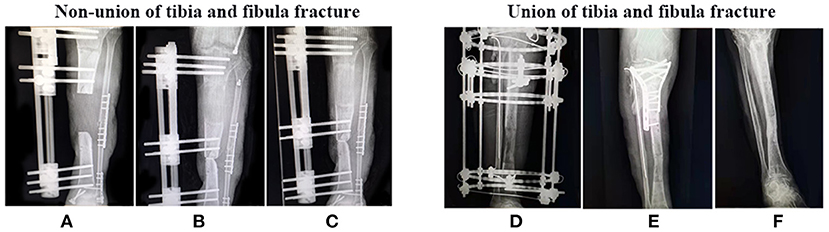
Figure 3. Non-union and Union of tibia and fibula fracture after surgery. X-ray examination (A,D) 1 month, (B,E) 3 month, and (C,F) 9 month after surgery.
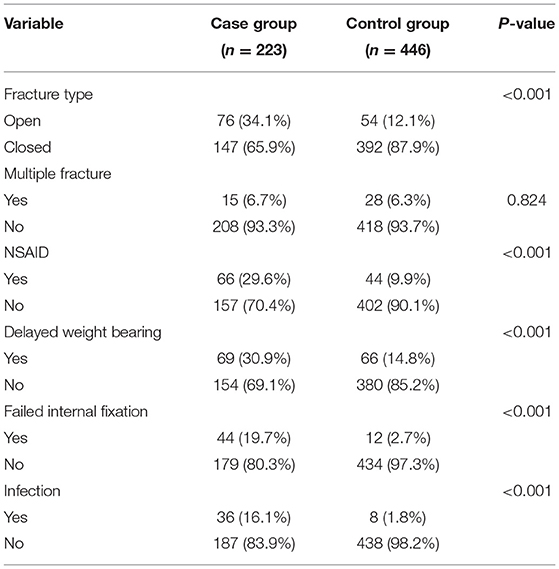
Outcome of Univariate Analysis
A univariate comparison between the case group and the control group found that fracture type (P < 0.001), NSAIDs use (P < 0.001), delayed weight bearing (P < 0.001), failed internal fixation (P < 0.001), and infection (P < 0.001) demonstrated a statistically significant difference (Table 2). There was no statistically significant difference only in multiple fracture (P = 0.824, Table 2).
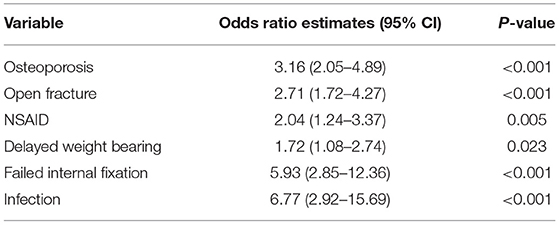
Outcome of Multivariate Logistic Regression Analysis
Furthermore, the variables P < 0.05 in univariate analysis were selected for further Logistic regression analysis. The results of multivariate analysis indicated that osteoporosis (odds ratio [OR] = 3.16, 95% confidence interval [CI]: 2.05–4.89, p < 0.001), open fracture (OR = 2.71, 95%CI: 1.72–4.27, p < 0.001), NSAIDs use (OR =2.04, 95%CI:1.24–3.37, p = 0.005), delayed weight bearing (OR = 1.72, 95%CI: 1.08–2.74, p = 0.023), failed internal fixation (OR = 5.93, 95%CI: 2.85–12.36, p < 0.001), and infection (OR = 6.77, 95%CI: 2.92–15.69, p < 0.001) were independent risk factors for non-union after surgery for limb fractures (Table 3).
Discussion
In this study, we found six predictors of non-union after surgery for limb fractures: osteoporosis, open fracture, NSAIDs use, delayed weight bearing, failed internal fixation, and infection. Other patient- and injury-related factors, such as age, sex, BMI, obesity, smoking, alcohol, hypertension, diabetes, closed fracture, and multiple fractures, were not significant risk factors.
Risk Factors
Without controlling for potential confounding factors, it is not clear whether age and sex itself are risk factors for bone non-union. Although the number of patients included in this study is relatively large, it is not sufficient to control the confounding effect of age and sex. Some studies have reported that age and sex are positively correlated with the risk of non-union (17, 18), while other reports show that there is no significant correlation (19, 20). It is worth noting that the average age of the population in this study is only ~40 years old, and the results may not apply to older patients. This may also explain why age-related factors such as obesity, smoking, alcohol, hypertension, and diabetes have not been identified as statistically significant risk factors in this study, despite being suggested as possible causes of bone non-union in previous studies (21–25). In addition, the study by Solomon et al. showed that there was a significant positive correlation between osteoporosis and the risk of non-union (26). However, another case-control study evaluated 1,498 patients and failed to find such an association (27). Our results indicated that the osteoporosis (OR = 3.16, 95%CI: 2.05–4.89) is associated with non-union, which is in support of the findings of Solomon et al.
In our study, no significant correlation was found between the presence of multiple fractures and non-union. On the contrary, a previous study showed that non-union seems to be associated with multiple fractures (28). This discrepancy may be related to the small proportion of non-union (n = 15, 6.7%) in patients with multiple fractures in our study; further studies with larger samples are needed to provide a more definitive understanding of the role of multiple fractures. However, a significant proportion of non-union cases occurred in patients with open fractures (n = 76, 34.1%), and the multiple regression analysis showed that patients with open fractures have a greater risk of non-union, which was consistent with the results of a previous study (29). Compared with closed fractures, open fractures are associated with relatively greater trauma, more serious destruction of soft tissue blood supply, higher probability of infection, and decreased blood supply, thus affecting bone healing (30). This also explains that patients with open fractures have a relatively high rate of healing disturbances.
Basic studies have shown that NSAIDs use affects bone healing, mainly due to their inhibiting effect on cyclooxygenase-2, which delays fracture healing (31). A recent retrospective clinical study of 1,900 patients with long bone fractures showed that the postoperative use of NSAIDs doubled the risk of healing complications (32). Moreover, Giannoudis et al. have demonstrated that there is a highly significant relationship between NSAIDs use and bone non-union (P < 0.001) (33). Our findings suggest that the NSAIDs use after surgery for limb fractures is associated with a 2.04-fold higher odds ratio of non-union, which is in line with the results of previous studies.
It is crucial to start weight bearing after a fracture since it helps maintain bone and muscle mass and helps restore the performance of activities of daily living. Additionally, weight bearing promotes bone healing through a process called mechanical transduction (34). Recently, a study demonstrated the safety of early weight bearing after fracture surgery (35). We identified a significant association (P < 0.001) between delayed weight bearing after surgery and the development of non-union, which is consistent with the results of the study by Westgeest et al. (36). Furthermore, delayed weight bearing was identified as an independent risk factor for the development of non-union in the multivariate analysis. This finding may be explained by a relationship between weight bearing and healing outcomes in the reverse direction. That is, bone non-union may cause more pain, resulting in delayed weight bearing, rather than delayed weight bearing causing non-union (37). Additionally, internal fixation failure is often considered as a reason to postpone the initial weight bearing. In this study, internal fixation failure (n = 44, 19.7%) accounted for a large proportion of bone non-union cases, which indicates that there is some association between failed internal fixation and delayed weight bearing. Indeed, our results showed that failed internal fixation (OR = 5.93, 95% CI: 2.85 to 12.36) significantly increases the risk of non-union.
Different opinions have been put forward on whether there is a connection between infection and non-union. Most scholars believe that infection does not increase the risk of non-union (38–40). However, a prospective cohort study evaluated 736 patients and showed that infection was significantly associated with non-union (36). The results of our analysis show that infection is an independent risk factor for non-union, with a 6.77-fold higher risk of non-union in patients with infection. There was also a significant correlation between infection and non-union. This may be due to the increased fracture end necrosis and vascular embolism, giving rise to poor local bone blood supply, so that the formation of bone is disturbed and healing is impaired, ultimately resulting in bone non-union (9).
Limitations of the Study
Despite these findings, this study has some limitations. First, although we designed a 1:2 matched case-control study to try to minimize the impact of the small sample size, our sample may not fully represent all postoperative patients with limb fractures and may also not be large enough to make our regression analysis conclusive. Second, multiple surgeons were involved in this retrospective study, each with a slightly different non-union definition and treatment. Finally, most patients in this study were middle-aged; thus, it is difficult to apply these findings to older patients. Therefore, further research in a wider age range is needed.
Conclusions
In summary, this study demonstrated that osteoporosis, open fractures, delayed weight bearing, NSAIDs use, failure of internal fixation, and infection are independent risk factors for non-union. Clinically, surgeons should understand these risk profiles in order to effectively guide patients and successfully set appropriate expectations.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the First Affiliated Hospital of Nanchang University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
KQ: methodology, investigation, and writing-original draft. QX: investigation and writing—original draft. MZ: formal analysis. XL: supervision, writing—review and editing, and conceptualization. MD: writing—review and editing, conceptualization, and funding acquisition. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation (No. 81860404).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BMI, body mass index; NSAIDs, non-steroidal anti-inflammatory drugs.
References
1. Tzioupis C, Giannoudis PV. Prevalence of long-bone non-unions. Injury. (2007) 38(Suppl. 2):S3–9. doi: 10.1016/S0020-1383(07)80003-9
2. Calori GM, Mazza E, Colombo M, Ripamonti C, Tagliabue L. Treatment of long bone non-unions with polytherapy: indications and clinical results. Injury. (2011) 42:587–90. doi: 10.1016/j.injury.2011.03.046
3. Reahl GB, Gerstenfeld L, Kain M. Epidemiology, clinical assessments, and current treatments of nonunions. Curr Osteoporos Rep. (2020) 18:157–68. doi: 10.1007/s11914-020-00575-6
4. Brinker MR, Trivedi A, O'Connor DP. Debilitating effects of femoral nonunion on health-related quality of life. J Orthop Trauma. (2017) 31:e37–42. doi: 10.1097/BOT.0000000000000736
5. Hak DJ, Fitzpatrick D, Bishop JA, Marsh JL, Tilp S, Schnettler R, et al. Delayed union and nonunions: epidemiology, clinical issues, and financial aspects. Injury. (2014) 45(Suppl. 2):S3–7. doi: 10.1016/j.injury.2014.04.002
6. Mills LA, Simpson AH. The relative incidence of fracture non-union in the Scottish population (5.17 million): a 5-year epidemiological study. BMJ Open. (2013) 3:e002276. doi: 10.1136/bmjopen-2012-002276
7. Kanakaris NK, Giannoudis PV. The health economics of the treatment of long-bone non-unions. Injury. (2007) 38(Suppl. 2):S77–84. doi: 10.1016/S0020-1383(07)80012-X
8. Wildemann B, Ignatius A, Leung F, Taitsman LA, Smith RM, Pesántez R, et al. Non-union bone fractures. Nat Rev Dis Primers. (2021) 7:57. doi: 10.1038/s41572-021-00289-8
9. Rodriguez EK, Boulton C, Weaver MJ, Herder LM, Morgan JH, Chacko AT, et al. Predictive factors of distal femoral fracture nonunion after lateral locked plating: a retrospective multicenter case-control study of 283 fractures. Injury. (2014) 45:554–9. doi: 10.1016/j.injury.2013.10.042
10. Copuroglu C, Calori GM, Giannoudis PV. Fracture non-union: who is at risk? Injury. (2013) 44:1379–82. doi: 10.1016/j.injury.2013.08.003
11. Wiss DA, Garlich J, Sherman R. Healing the index tibial nonunion: risk factors for development of a recalcitrant nonunion in 222 patients. J Orthop Trauma. (2021) 35:e316–21. doi: 10.1097/BOT.0000000000002060
12. Drosos GI, Bishay M, Karnezis IA, Alegakis AK. Factors affecting fracture healing after intramedullary nailing of the tibial diaphysis for closed and grade I open fractures. J Bone Joint Surg Br. (2006) 88:227–31. doi: 10.1302/0301-620X.88B2.16456
13. Chahar HS, Gupta M, Kumar V, Yadav R, Patel J, Pal CP. Prospective evaluation of role of limb reconstruction system (rail external fixator) in open fractures and infected non-union of femur. J Orthopaed Case Rep. (2021) 11:5–11. doi: 10.13107/jocr.2021.v11.i01.1942
14. Ding L, He Z, Xiao H, Chai L, Xue F. Factors affecting the incidence of aseptic nonunion after surgical fixation of humeral diaphyseal fracture. J Orthop Sci. (2014) 19:973–7. doi: 10.1007/s00776-014-0640-1
15. Bhandari M, Tornetta P III, Sprague S, Najibi S, Petrisor B, Griffith L, et al. Predictors of reoperation following operative management of fractures of the tibial shaft. J Orthop Trauma. (2003) 17:353–61. doi: 10.1097/00005131-200305000-00006
16. Yang JJ, Lin LC, Chao KH, Chuang SY, Wu CC, Yeh TT, et al. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration. J Bone Joint Surg Am. (2013) 95:61–9. doi: 10.2106/JBJS.K.01081
17. Zura R, Braid-Forbes MJ, Jeray K, Mehta S, Einhorn TA, Watson JT, et al. Bone fracture nonunion rate decreases with increasing age: a prospective inception cohort study. Bone. (2017) 95:26–32. doi: 10.1016/j.bone.2016.11.006
18. Zura R, Watson JT, Einhorn T, Mehta S, Della Rocca GJ, Xiong Z, et al. An inception cohort analysis to predict nonunion in tibia and 17 other fracture locations. Injury. (2017) 48:1194–203. doi: 10.1016/j.injury.2017.03.036
19. Ali A, Douglas H, Stanley D. Revision surgery for nonunion after early failure of fixation of fractures of the distal humerus. J Bone Joint Surg Br. (2005) 87:1107–10. doi: 10.1302/0301-620X.87B8.15610
20. Mills LA, Aitken SA, Simpson A. The risk of non-union per fracture: current myths and revised figures from a population of over 4 million adults. Acta Orthop. (2017) 88:434–9. doi: 10.1080/17453674.2017.1321351
21. Meidinger G, Imhoff AB, Paul J, Kirchhoff C, Sauerschnig M, Hinterwimmer S. May smokers and overweight patients be treated with a medial open-wedge HTO? Risk factors for non-union. Knee Surg Sports Traumatol Arthrosc. (2011) 19:333–9. doi: 10.1007/s00167-010-1335-6
22. Ziran B, Cheung S, Smith W, Westerheide K. Comparative efficacy of 2 different demineralized bone matrix allografts in treating long-bone nonunions in heavy tobacco smokers. Am J Orthop. (2005) 34:329–32.
23. Duckworth AD, Bennet SJ, Aderinto J, Keating JF. Fixation of intracapsular fractures of the femoral neck in young patients: risk factors for failure. J Bone Joint Surg Br. (2011) 93:811–6. doi: 10.1302/0301-620X.93B6.26432
24. Cappuccio FP, Meilahn E, Zmuda JM, Cauley JA. High blood pressure and bone-mineral loss in elderly white women: a prospective study. Study of Osteoporotic Fractures Research Group. Lancet. (1999) 354:971–5. doi: 10.1016/S0140-6736(99)01437-3
25. Hernandez RK, Do TP, Critchlow CW, Dent RE, Jick SS. Patient-related risk factors for fracture-healing complications in the United Kingdom General Practice Research Database. Acta Orthop. (2012) 83:653–60. doi: 10.3109/17453674.2012.747054
26. Solomon DH, Hochberg MC, Mogun H, Schneeweiss S. The relation between bisphosphonate use and non-union of fractures of the humerus in older adults. Osteoporos Int. (2009) 20:895–901. doi: 10.1007/s00198-008-0759-z
27. van Wunnik BP, Weijers PH, van Helden SH, Brink PR, Poeze M. Osteoporosis is not a risk factor for the development of nonunion: a cohort nested case-control study. Injury. (2011) 42:1491–4. doi: 10.1016/j.injury.2011.08.019
28. Calori GM, Albisetti W, Agus A, Iori S, Tagliabue L. Risk factors contributing to fracture non-unions. Injury. (2007) 38(Suppl. 2):S11–8. doi: 10.1016/S0020-1383(07)80004-0
29. Zura R, Xiong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ, et al. Epidemiology of fracture nonunion in 18 human bones. JAMA Surg. (2016) 151:e162775. doi: 10.1001/jamasurg.2016.2775
30. Metsemakers WJ, Handojo K, Reynders P, Sermon A, Vanderschot P, Nijs S. Individual risk factors for deep infection and compromised fracture healing after intramedullary nailing of tibial shaft fractures: a single centre experience of 480 patients. Injury. (2015) 46:740–5. doi: 10.1016/j.injury.2014.12.018
31. Simon AM, O'Connor JP. Dose and time-dependent effects of cyclooxygenase-2 inhibition on fracture-healing. J Bone Joint Surg Am. (2007) 89:500–11. doi: 10.2106/JBJS.F.00127
32. Jeffcoach DR, Sams VG, Lawson CM, Enderson BL, Smith ST, Kline H, et al. Nonsteroidal anti-inflammatory drugs' impact on nonunion and infection rates in long-bone fractures. J Trauma Acute Care Surg. (2014) 76:779–83. doi: 10.1097/TA.0b013e3182aafe0d
33. Giannoudis PV, MacDonald DA, Matthews SJ, Smith RM, Furlong AJ, De Boer P. Nonunion of the femoral diaphysis. The influence of reaming and non-steroidal anti-inflammatory drugs. J Bone Joint Surg Br. (2000) 82:655–8. doi: 10.1302/0301-620X.82B5.0820655
34. Goodship AE, Cunningham JL, Kenwright J. Strain rate and timing of stimulation in mechanical modulation of fracture healing. Clin Orthop Relat Res. (1998) 355 (Suppl.):S105–15. doi: 10.1097/00003086-199810001-00012
35. Bailón-Plaza A, van der Meulen MC. Beneficial effects of moderate, early loading and adverse effects of delayed or excessive loading on bone healing. J Biomech. (2003) 36:1069–77. doi: 10.1016/S0021-9290(03)00117-9
36. Westgeest J, Weber D, Dulai SK, Bergman JW, Buckley R, Beaupre LA. Factors associated with development of nonunion or delayed healing after an open long bone fracture: a prospective cohort study of 736 subjects. J Orthop Trauma. (2016) 30:149–55. doi: 10.1097/BOT.0000000000000488
37. Houben IB, Raaben M, Van Basten Batenburg M, Blokhuis TJ. Delay in weight bearing in surgically treated tibial shaft fractures is associated with impaired healing: a cohort analysis of 166 tibial fractures. Eur J Orthop Surg Traumatol. (2018) 28:1429–36. doi: 10.1007/s00590-018-2190-2
38. Schemitsch EH, Bhandari M, Guyatt G, Sanders DW, Swiontkowski M, Tornetta P, et al. Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Joint Surg Am. (2012) 94:1786–93. doi: 10.2106/JBJS.J.01418
39. Audigé L, Griffin D, Bhandari M, Kellam J, Rüedi TP. Path analysis of factors for delayed healing and nonunion in 416 operatively treated tibial shaft fractures. Clin Orthop Relat Res. (2005) 438:221–32. doi: 10.1097/01.blo.0000163836.66906.74
Keywords: limb fractures, bone non-union, fracture healing, risk factors, multivariate logistic regression
Citation: Quan K, Xu Q, Zhu M, Liu X and Dai M (2021) Analysis of Risk Factors for Non-union After Surgery for Limb Fractures: A Case-Control Study of 669 Subjects. Front. Surg. 8:754150. doi: 10.3389/fsurg.2021.754150
Received: 06 August 2021; Accepted: 22 November 2021;
Published: 14 December 2021.
Edited by:
Ingo Marzi, Goethe University Frankfurt, GermanyReviewed by:
Junlin Zhou, Capital Medical University, ChinaXiuguo Han, Shanghai Jiaotong University, China
Copyright © 2021 Quan, Xu, Zhu, Liu and Dai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuqiang Liu, c2hsaXV4dXFpYW5nQDE2My5jb20=; Min Dai, ZGFpbWluQG1lZG1haWwuY29tLmNu
 Kun Quan
Kun Quan Qiang Xu
Qiang Xu Xuqiang Liu
Xuqiang Liu Min Dai
Min Dai