- Otolaryngology, Audiology and Phoniatric Operative, Department of Surgical Pathology, Medical, Molecular and Critical Area, Azienda Ospedaliero-Universitaria Pisana, University of Pisa, Pisa, Italy
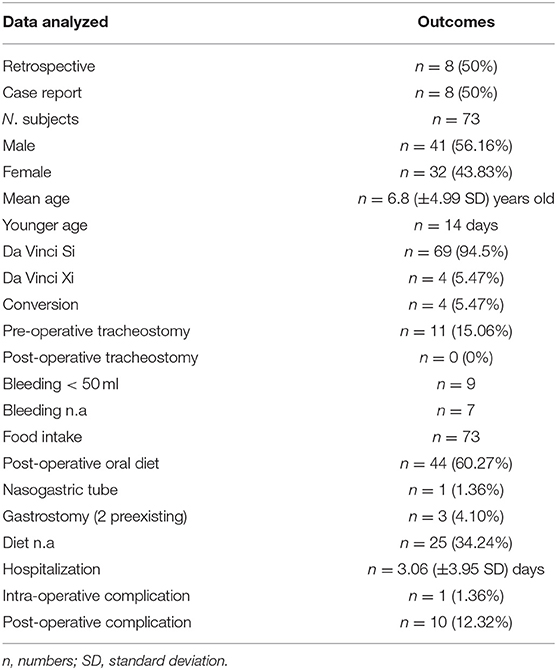
Pediatric transoral robotic surgery (TORS) has improved from 2007 to 2020, widening its indications and feasibility. This article aims to systematically analyze the procedures performed from the first use until the current year, observing their evolution over time. A systematic literature review was performed using PubMed, Scopus, Web of Science, and Cochrane databases between March 1, 2000, and April 1, 2020. We selected studies that were written only in English and were performed in live human subjects. About 16 studies were found with a total of 73 subjects treated, among them 41 were men and 32 were women with an average age of 6.8 ± 4.99 years. There have been four (5.47%) conversions. Both functional and benign-malignant diseases have been treated in the series. Eleven (15.06%) pre-operative tracheostomy and zero post-operative tracheostomy were performed. The bleeding data was only reported in 9 studies and was <50 ml. Only one (1.36%) intra-operative complication and 10 (12.32%) postoperative complications were reported. We consider the TORS procedures in pediatric subjects safe, feasible and with good surgical outcomes up to the laryngeal region.
Introduction
Since 2000, when the Da Vinci robotic system (Intuitive Surgical Inc., Sunnyvale, CA, USA) was approved for laparoscopic surgery by the Food and Drug Administration (FDA), robotic surgery has been progressing not only in terms of technology but also in terms of possibilities for application.
In the beginning, the system was mainly used in abdominal surgery for urological and gynecological procedures. Successively, it was applied in other anatomical districts with exponential growth in the population of pediatrics. In 2009, the FDA approved the Da Vinci system for transoral procedures.
The purpose of this study is to systematically analyze the transoral robotic surgery (TORS) procedures performed in pediatric subjects, from the first cases reported (1), up until today, to observe the evolution of the procedure in terms of feasibility and prevalence of the anatomical sites treated.
Materials and Methods
Literature Review and Research Strategy
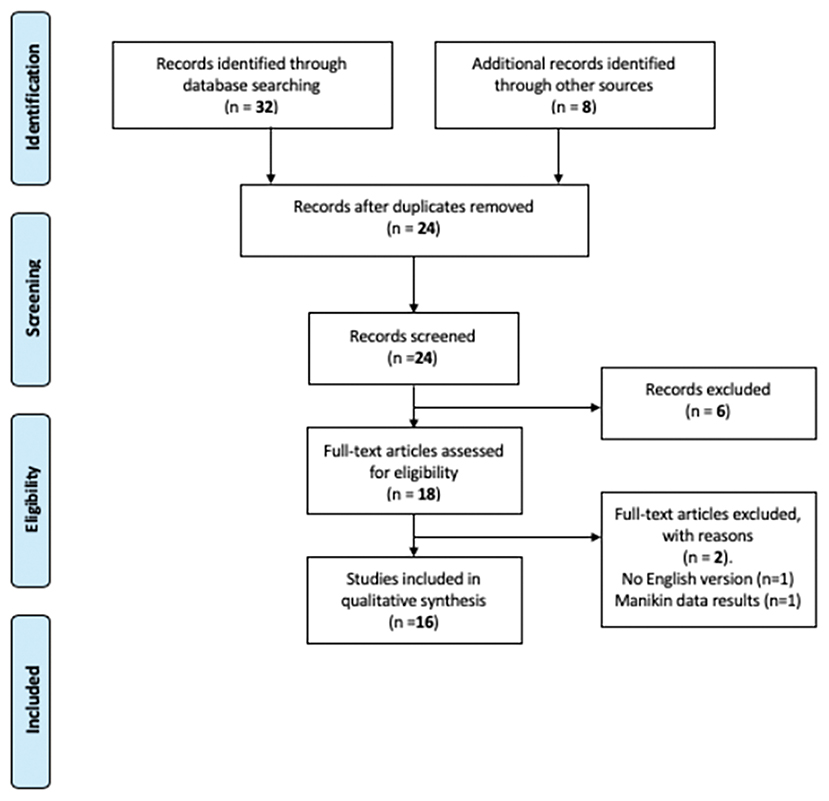
A systematic literature review was conducted using PubMed, Scopus, Web of Science, and Cochrane databases, according to the PRISMA guidelines (2), by combining the following keywords: robotic, robotic surgery, pediatric tors, children head and neck, Da Vinci, pediatric transoral robotic surgery, pediatric robot ENT, pediatric robot otolaryngology, tors infant, tors children; between March 1, 2007, and April 1, 2020.
Eligibility Criteria
We included studies according to the following criteria: studies on TORS pediatric procedures; retrospective and prospective studies that are peer-reviewed; English-written studies; studies performed in live human subjects (cadaver dissections were excluded). The pediatric subject included was up to 16 years of age.
Study Selection and Data Extraction
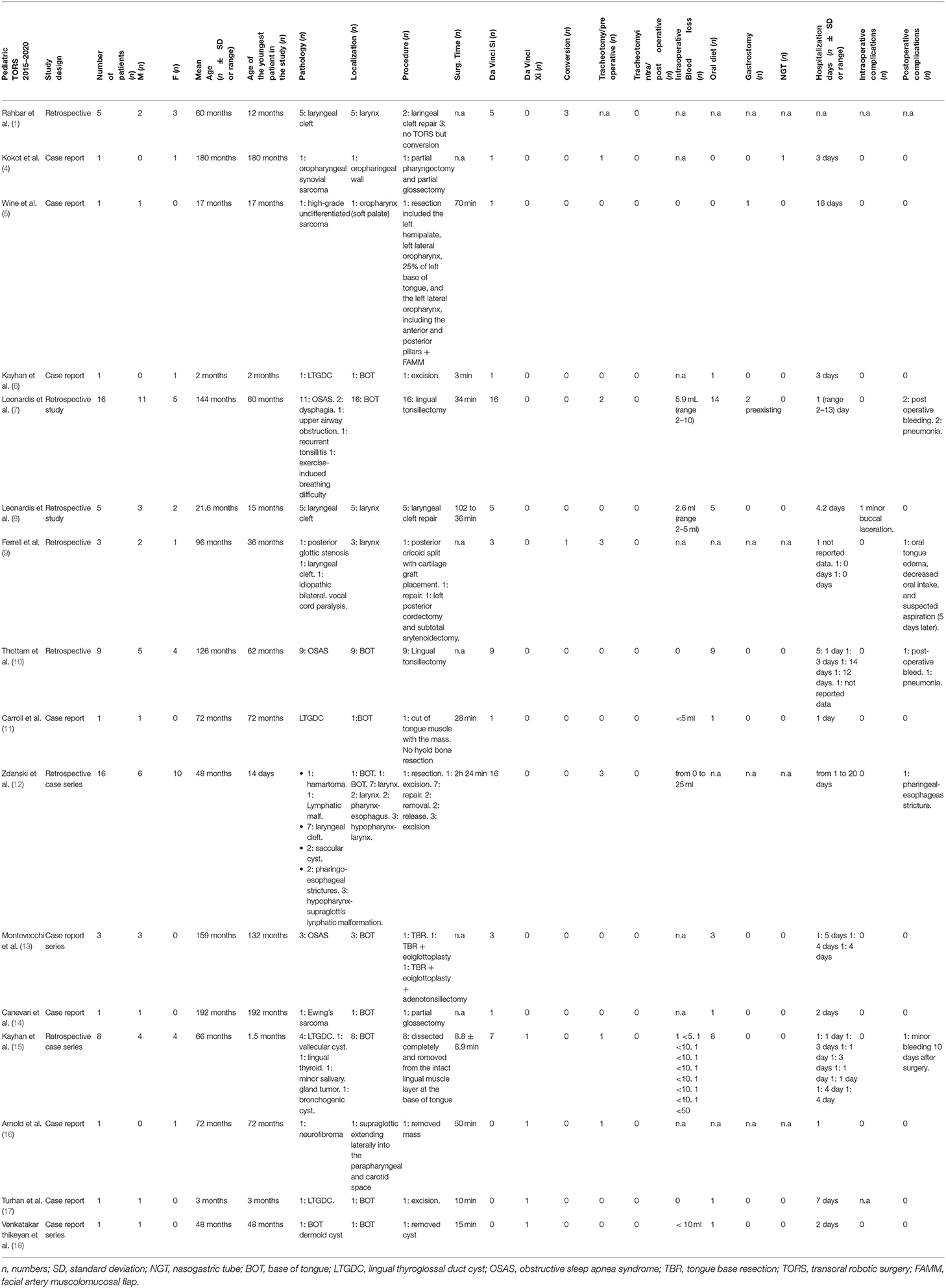
Two of the authors (MV and GF) independently screened the retrieved studies based on the title, keywords, and abstracts to exclude irrelevant and non-English written studies. Duplicates were removed and the full-text of the remaining papers were analyzed when uncertainty existed in the abstract evaluation. A manual search in the reference lists of these articles was performed to identify potentially relevant papers missed during the database search. Differing opinions were solved by consensus between the two authors. Data extracted and analyzed for the study included the following criteria: the demographic data, the number of procedures performed, the number and type of pathology, the typology of the robot used, site and sub-site of the procedure, surgical time (ST) of the procedures, number of conversions and/or abortions, the number of intra- and post-operative complications, times of hospitalization, intraoperative blood loss, ways for food intake, and the number of intra- and post-operative tracheostomy.
Evidence Quality Appraisal
All studies were assessed for their methodological quality using the National Institute for Health and Care Excellence (NICE) methodology checklist (3) for quality assessment of case series.
Statistical Analysis
The data from each study were transcribed in tabular forms and these were summarized using descriptive statistics. Dichotomous variables were reported as numbers and percentages, while continuous variables were reported as mean ± SD, or median ± interquartile range (IQR) if the values were not normally distributed.
Results
General data about included studies and subjects are shown in Table 1. Sixteen studies (Table 2) met our inclusion criteria (Figure 1).
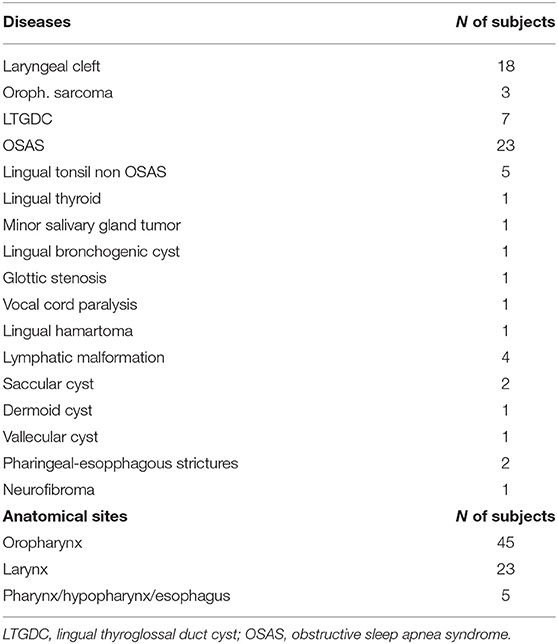
The most frequent pathology observed was obstructive sleep apnea syndrome (OSAS): 20 subjects were treated with lingual tonsillectomy, 2 subjects were treated with lingual tonsillectomy plus epiglottoplastic, and 1 subject was treated with lingual tonsillectomy plus epiglottoplastic plus adenotonsillectomy (13). Five subjects underwent lingual tonsillectomy for non-OSAS diseases (7). The second most performed surgery was laryngeal cleft repair treating 18 subjects (1, 8, 9, 12). The third most common intervention (7 subjects) was the exeresis of lingual thyroglossal duct cyst (6, 11, 15, 17). Neoplastic pathology was treated in six subjects (8, 21%), four of these with malignant disease of the base-tongue: three sarcomas (4, 5, 14) and one minor salivary gland tumor (15). The remaining two subjects were affected by a benign pathology: one hamartoma (12) of the base tongue and the other neurofibroma of the larynx (16). Lymphatic malformation (12) was identified in 4 subjects, one in the base-tongue and three in the hypopharynx-larynx site. The numbers and anatomical distribution relating to the rest of the TORS procedures are shown in Table 3.
There was only one intra-operative complication (1.36%): a small buccal laceration that required a suture in a laryngeal cleft repair surgery (8). There were a total of nine postoperative complications (12.32%) worthy of note, including four pneumonia (7, 12, 19), one of which with septic shock (12), 4 bleedings (7, 10, 15), and 1 edema of the tongue, which did not allow correct oral nutrition (9). There were four conversions (5.47%): three for oral exposure difficulties (1) and one subject was affected by posterior glottic stenosis. For the latter subject, a robotic-assisted posterior cricoid split with cartilage graft placement was attempted [but required conversion to an open surgical technique (9)].
Only nine studies reported operating times but due to the heterogeneity of the pathologies treated, we did not perform any statistical analysis.
On intraoperative blood losses, only eight studies reported these data (5, 7, 8, 10–12, 15, 18), and in all cases, it was <25 ml, except one subject <50 ml (15).
The results of the NICE methodology checklist for quality assessment for the case series are shown in Table 4. Data quality of 13 studies (81.25%) was classified as moderate and 3 as high (18.75%).
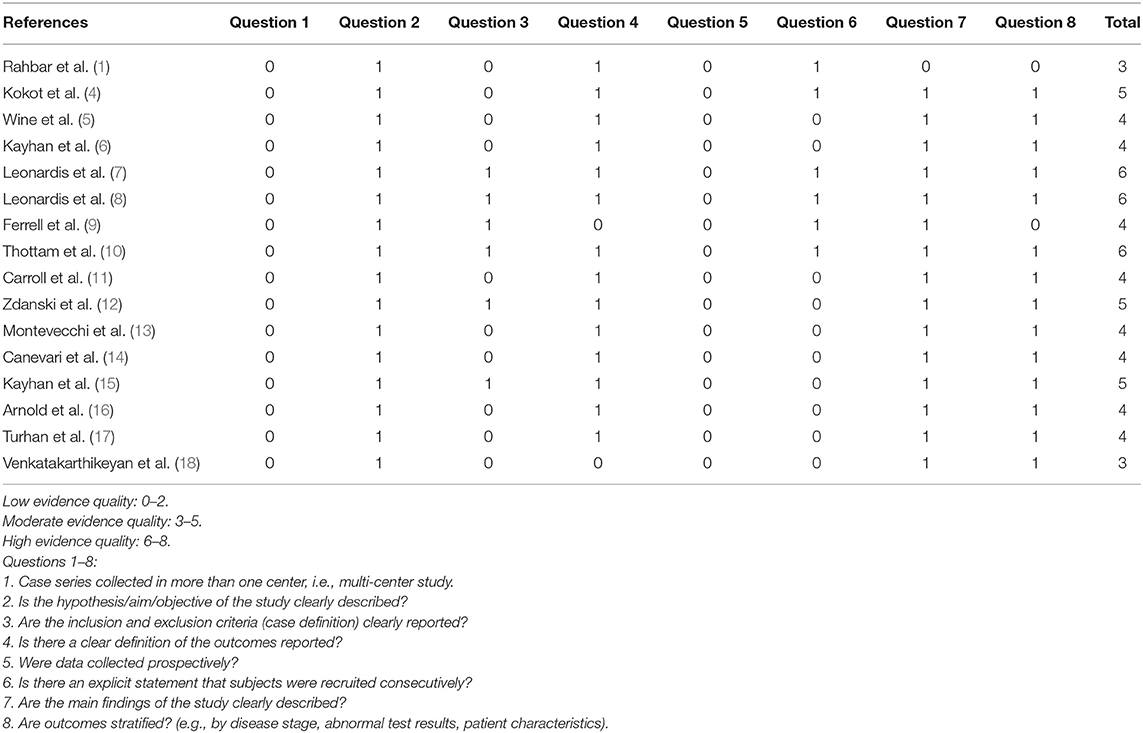
Table 4. National Institute for Health and Care Excellence (NICE) methodology checklist for quality assessment of case series.
Discussion
The use of the robot in the pediatric transoral robotic procedure has been more consistent over the years. The first work on the application of robotics in the pediatric population was conducted by Rahbar et al. (1). Since then, several studies have been published regarding pediatric TORS. The first and only article reviewing the literature on this topic was published in 2015 by Erkul et al. (19). They analyzed studies concerning 41 subjects and the surgical procedures carried out. Since then, 32 new pediatric subjects have been reported in the literature, approximately doubling the number of patients to be analyzed; however, the number of subjects included is quite low and there are lots of missing data in the selected articles. These aspects limit this work and prevent us from drawing any definitive conclusion.
The most surgically treated site was the oropharynx, especially the base of the tongue (Table 3). In this anatomical location, the applications for surgery have become broader and there has been an increase over the years of cases of treated Lingual Thyroglossal Duct Cyst (LTGDC) and the use of TORS for the malignant neoplastic pathology. Until 2017, information is only available for the surgical repair procedures of the laryngeal cleft, posterior glottic stenosis, and idiopathic bilateral cord paralysis. In the following years, 2 saccular cysts, 3 lymphatic malformations (12), and a neurofibroma involving the parapharyngeal space (16) were successfully removed.
Four conversions (5.47%) are identified: 3 for oral exposure difficulties, all in the first study of the series (1). The other case of conversion was because of the inability to have a good visual of the subglottis and difficulty with the placement of robotic arms in a subject with posterior glottic stenosis, following an inhalational burn injury (9). The learning curve provides the authors with a plausible reason behind the lack of other conversions in the series, other than the ones already described, despite more complex surgical interventions over the years. Only a minor buccal laceration is described for intraoperative complications.
We consider the data relating to post-operative bleeding and tracheostomies, to be interesting for its variations. Four among the 73 subjects (5.47%) were reported with postoperative bleeding. Hay et al. (20) reported in adult subjects an incidence of postoperative bleeding after TORS procedures of 16% and 6% among the subjects back to the operating rooms to manage the complication. In other large retrospective TORS series on adult subjects, the risk of postoperative hemorrhage ranged from 7 to 22% (21). Due to the low incidence of bleeding in pediatric subjects, we agree with Canevari et al. (14) that tracheostomy can only be justified in selected cases and no intra- or post-operative tracheostomies were reported in the selected studies. Only 11 subjects were subjected to this procedure due to a difficulty in breathing but before the surgery.
In terms of intraoperative blood loss, we have not noticed considerable data on the amount of milliliters. We hypothesize that it would have been of interest to conduct a comparison based on incidence percentages of the intraoperative blood losses. The comparison could have been made on data with adults or with non-robotic transoral procedures. Unfortunately, among the 16 studies of the series reported, only 8 had the available data, not enough to conduct a statistically relevant comparison; however, it must be taken into account that the experience on pediatric TORS procedures is derived from the experience of adult patients, limiting any serious comparison of data regarding intra- and post-operative complications.
The endotracheal tube does interfere with a good visualization (14) of the oropharynx, and, despite some surgeons prefer trans-nasal intubation to treat the base of the tongue (15), others reported that both oral or nasal intubation did not obstruct the necessary view of the oropharyngeal anatomy (8). In another significant study on subjects operated at the base of the tongue (15), these authors argue that compared to adult subjects, in pediatric subjects the limits are because the size of airways in children is smaller, mouth opening is inefficient, have large retractors and the available instruments today reduces exposition leading to incompatibility of robotic arms. These authors used different types of mouth opening devices, such as the Davis-Meyer mouth gag, Davis-Boyle mouth gag, Dingman retractor, McIvor retractor, and Feyh-Kastenbauer retractor, depending on age and mouth structure of the child; however, a laryngeal saccular cyst was removed in a 14-day-old patient successfully and with no complication.
The use of the Da Vinci Xi system was made in four different studies and four consecutive years from 2017 until today (15–18). Its application has remained marginal, in part due to the non-FDA approval for TORS procedures, and in part because of the technical peculiarities that limit its applications for certain TORS procedures (22).
We agree with Zdanski et al. (12) that the plausible key elements that can lead to further evolution of TORS procedures in pediatric subjects are the following: securing the airway tract with the appropriate laser-safe endotracheal or tracheostomy tubes; identifying the appropriate exposure; surgical access with robotic arms for unrestricted mobility; the critical role of the bedside surgeon, in protecting the airway, the patient, and assisting the robotic surgeon. It will be necessary in the future to design appropriate instruments for pediatric airway TORS surgeries, without converting the general or urological instruments available today. The Da Vinci Robotic System was built to treat general and urological pathologies, and, nowadays, its instrumentation is adapted to TORS procedures (22). For that reason, most of the time patient selection is tailored to what can be done with the available technology and not vice versa.
Conclusion
The feasibility of the pediatric TORS procedures has been demonstrated up to the laryngeal region, with good outcomes in terms of successful surgeries. In addition to the evolution of the instruments, we hypothesize that surgeons who already currently practice this type of surgery in adult subjects can also upgrade their training and experience in a pediatric patient.
In relation to the low intraoperative blood loss, the lack of major intra- and post-operative complications, the low percentage of the minor ones, and the low percentage of conversions in open procedures, we can consider the TORS procedures in pediatric subjects safe and feasible.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
MV and GF: study conception and design. MV, GF, and GB: data acquisition. MV, GF, ID, and LB: analysis and data interpretation. MV, GF, and LB: drafting of the manuscript. LB: critical revision of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rahbar R, Ferrari LR, Borer JG, Peters CA. Robotic surgery in the pediatric airway: application and safety. Arch Otolaryngol Head Neck Surg. (2007) 133:46. doi: 10.1001/archotol.133.1.46
2. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. (2009) 6:e1000100. doi: 10.1371/journal.pmed.1000100
3. NICE. National Institute for Health and Care Excellence. Methods for the Development of NICE Public Health Guidance. National Institute for Health and Care Excellence (NICE), London (2012).
4. Kokot N, Mazhar K, O'Dell K, Huang N, Lin A, Sinha UK. Transoral robotic resection of oropharyngeal synovial sarcoma in a pediatric patient. Int J Pediatr Otorhinolaryngol. (2013) 77:1042–4. doi: 10.1016/j.ijporl.2013.03.022
5. Wine TM, Duvvuri U, Maurer SH, Mehta DK. Pediatric transoral robotic surgery for oropharyngeal malignancy: a case report. Int J Pediatr Otorhinolaryngol. (2013) 77:1222–6. doi: 10.1016/j.ijporl.2013.04.024
6. Kayhan FT, Kaya KH, Koc AK, Altintas A, Erdur O. Transoral surgery for an infant thyroglossal duct cyst. Int J Pediatr Otorhinolaryngol. (2013) 77:1620–3. doi: 10.1016/j.ijporl.2013.07.007
7. Leonardis RL, Duvvuri U, Mehta D. Transoral robotic-assisted lingual tonsillectomy in the pediatric population. JAMA Otolaryngol Head Neck Surg. (2013) 139:1032. doi: 10.1001/jamaoto.2013.4924
8. Leonardis RL, Duvvuri U, Mehta D. Transoral robotic-assisted laryngeal cleft repair in the pediatric patient. Laryngoscope. (2014) 124:2167–9. doi: 10.1002/lary.24680
9. Ferrell JK, Roy S, Karni RJ, Yuksel S. Applications for transoral robotic surgery in the pediatric airway: TORS and the pediatric airway. Laryngoscope. (2014) 124:2630–5. doi: 10.1002/lary.24753
10. Thottam PJ, Govil N, Duvvuri U, Mehta D. Transoral robotic surgery for sleep apnea in children: is it effective? Int J Pediatr Otorhinolaryngol. (2015) 79:2234–7. doi: 10.1016/j.ijporl.2015.10.010
11. Carroll DJ, Byrd JK, Harris GF. The feasibility of pediatric TORS for lingual thyroglossal duct cyst. Int J Pediatr Otorhinolaryngol. (2016) 88:109–12. doi: 10.1016/j.ijporl.2016.06.038
12. Zdanski CJ, Austin GK, Walsh JM, Drake AF, Rose AS, Hackman TG, et al. Transoral robotic surgery for upper airway pathology in the pediatric population: TORS in pediatric population. Laryngoscope. (2017) 127:247–51. doi: 10.1002/lary.26101
13. Montevecchi F, Bellini C, Meccariello G, Hoff PT, Dinelli E, Dallan I, et al. Transoral robotic-assisted tongue base resection in pediatric obstructive sleep apnea syndrome: case presentation, clinical and technical consideration. Eur Arch Otorhinolaryngol. (2017) 274:1161–6. doi: 10.1007/s00405-016-4269-x
14. Canevari FR, Montevecchi F, Galla S, Sorrentino R, Vicini C, Sireci F. Trans-Oral Robotic Surgery for a Ewing's sarcoma of tongue in a pediatric patient: a case report. Braz J Otorhinolaryngol. (2017) 86(Suppl 1):26–9. doi: 10.1016/j.bjorl.2017.04.001
15. Kayhan FT, Yigider AP, Koc AK, Kaya KH, Erdim I. Treatment of tongue base masses in children by transoral robotic surgery. Eur Arch Otorhinolaryngol. (2017) 274:3457–63. doi: 10.1007/s00405-017-4646-0
16. Arnold MA, Mortelliti AJ, Marzouk MF. Transoral resection of extensive pediatric supraglottic neurofibroma: pediatric TOS. Laryngoscope. (2018) 128:2525–8. doi: 10.1002/lary.27186
17. Turhan M, Bostanci A. Robotic resection of lingual thyroglossal duct cyst in an infant. J Robotic Surg. (2019) 13:331–4. doi: 10.1007/s11701-018-0841-2
18. Venkatakarthikeyan C, Nair S, Gowrishankar M, Rao S. Robotic surgery in head and neck in pediatric population: our experience. Indian J Otolaryngol Head Neck Surg. (2020) 72:98–103. doi: 10.1007/s12070-019-01768-x
19. Erkul E, Duvvuri U, Mehta D, Aydil U. Transoral robotic surgery for the pediatric head and neck surgeries. Eur Arch Otorhinolaryngol. (2017) 274:1747–50. doi: 10.1007/s00405-016-4425-3
20. Hay A, Migliacci J, Karassawa Zanoni D, Boyle JO, Singh B, Wong RJ, et al. Haemorrhage following transoral robotic surgery. Clin Otolaryngol. (2018) 43:638–44. doi: 10.1111/coa.13041
21. Zenga J, Suko J, Kallogjeri D, Pipkorn P, Nussenbaum B, Jackson RS. Postoperative hemorrhage and hospital revisit after transoral robotic surgery. Laryngoscope. (2017) 127:2287–92. doi: 10.1002/lary.26626
Keywords: pediatric surgery, pediatric trans-oral robotic surgery, pediatric TORS, pediatric Da Vinci, trans-oral robotic surgery
Citation: Vianini M, Fiacchini G, Benettini G, Dallan I and Bruschini L (2021) Experience in Transoral Robotic Surgery in Pediatric Subjects: A Systematic Literature Review. Front. Surg. 8:726739. doi: 10.3389/fsurg.2021.726739
Received: 17 June 2021; Accepted: 19 July 2021;
Published: 12 August 2021.
Edited by:
Alberto Deganello, University of Brescia, ItalyReviewed by:
Giuseppe Meccariello, Azienda Unità Sanitaria Locale (AUSL) della Romagna, ItalyVittorio Rampinelli, University of Brescia, Italy
Copyright © 2021 Vianini, Fiacchini, Benettini, Dallan and Bruschini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Giacomo Fiacchini, Zy5maWFjY2hpbmlAZ21haWwuY29t
†These authors have contributed equally to this work
 Matteo Vianini
Matteo Vianini Giacomo Fiacchini
Giacomo Fiacchini Giacomo Benettini
Giacomo Benettini Iacopo Dallan
Iacopo Dallan Luca Bruschini
Luca Bruschini