- 1Department of Cardiology, Langfang People Hospital, Langfang, China
- 2Department of Orthopedics, Langfang People Hospital, Langfang, China
Background: This study compares the efficacy of two elastic bandages in treating forearm hematoma after transradial coronary intervention.
Methods: A total of 60 patients with moderate or severe forearm hematoma following transradial coronary intervention were enrolled in this study. They were randomly divided into two groups, as follows: an Idealast-haft elastic bandage group (the observation group) and a control group. The patients in the Idealast-haft elastic bandage group received compression bandaging with Idealast-haft elastic bandages and the patients in the control group received compression bandaging with Nylexorgrip elastic bandages. Observation indexes related to, for example, forearm pain, arterial pulsation, blistering, skin color, and hemostasis time were compared between the two groups.
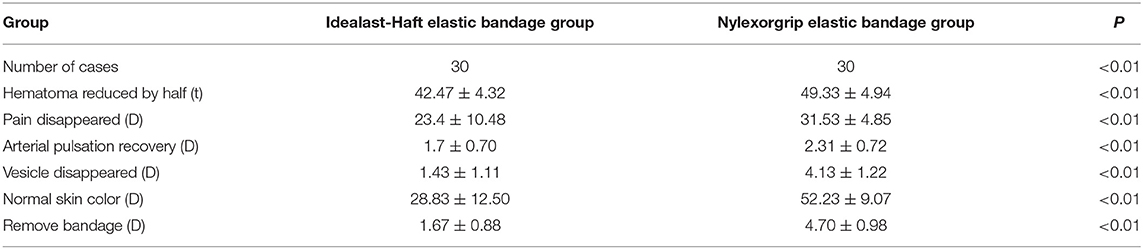
Results: The results revealed that the times taken for pain disappearance, arterial pulse recovery, blister disappearance, skin color recovery, and compression hemostasis were significantly shorter in the Idealast-haft elastic bandage group than in the control group, and the differences were statistically significant (P < 0.05). The hematoma range and the arm circumference at the severest part of the hematoma decreased faster in the observation group than in the control group, and the differences were statistically significant (P < 0.05).
Conclusion: The Idealast-haft elastic bandage is more effective than the Nylexorgrip elastic bandage in patients with forearm hematoma following transradial coronary intervention and should therefore be used in such cases.
Background
Transradial coronary intervention for diagnosis and treatment is a milestone in the history of interventional cardiology (1, 2). The radial artery approach is superficial and easily compressed and fixed; in addition, it forms a double blood supply with the ulnar artery. The many advantages of transradial intervention include the following: few complications, small trauma of the puncture site, no need for long-term bed rest, improved patient comfort, slight postoperative nursing workload, and short hospital stay (3, 4). The promotion of this technology over the last 10 years has given it global popularity. In 2017, the total number of coronary intervention cases in China exceeded 750,000. The transradial technique currently accounts for more than 80% of interventions in many medical centers in China. Although the radial artery approach has many advantages, the popularity of this technique means that the associated complications cannot be ignored (5, 6).
As the proportion of patients who undergo transradial coronary intervention has increased, postoperative complications have become more common. Forearm hematoma is the most common complication following transradial intervention, with an incidence of ~1–2%. Early detection and the use of appropriate procedures are key to preventing serious adverse events (7–9).
Methods
General Data
This study included patients with coronary heart disease who were admitted to our department from March 2016 to January 2018. All patients had moderate to severe forearm hematoma after coronary intervention (see Table 1). They were randomly divided into two groups, an Idealast-haft elastic bandage group (the observation group) and a control group. The patients in the Idealast-haft elastic bandage group received compression bandaging with Idealast-haft elastic bandages and the patients in the control group received compression bandaging with Nylexorgrip elastic bandages. The study was approved by the Ethics Committee of our hospital, and all patients provided signed informed consent.
Inclusion and Exclusion Criteria
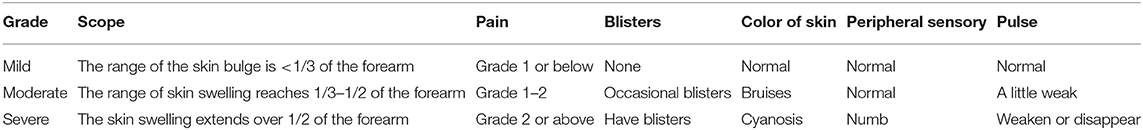
The inclusion criteria for patients were as follows: (1) transradial coronary intervention by the same operator; (2) moderate or severe forearm hematoma (as defined in Table 1) after the operation; and (3) an age of ≥18 years. The exclusion criteria for patients were as follows: (1) negative Allen's test result; (2) history of radial artery puncture within half a year; and (3) complicated degeneration of the vein bridge.
Therapeutic Methods
After the interventional therapy, the skin around the radial artery puncture point was sterilized and dried, the sheath tube was withdrawn, and local compression hemostasis was performed with a pressure apparatus. Patients with forearm hematoma during and after the operation were selected. With the local bleeding site as the midpoint, compression hemostasis with elastic bandages was performed at two sites, ~2 cm from the proximal and distal ends of the hematoma. Patients in the Idealast-haft elastic bandage group were treated with Idealast-haft elastic bandages, and patients in the control group were treated with Nylexorgrip elastic bandages. The pressure of the elastic bandages was maintained within the levels in which the pulsation of the radial artery of the affected limb could be felt, and the patients were monitored for the presence of ischemic symptoms. The elastic bandaging was relaxed every 2 h according to the condition of the subcutaneous hematoma and the chief complaint and symptoms of the patient; this adjustment continued until the bandages were removed.
The Main Observation Indexes
In the present study, the main observation indexes included: (a) the speed of reduction of the hematoma range; (b) the speed of reduction of the arm circumference at the severest part of the hematoma; (c) the time taken for the pain to disappear; (d) the time taken for the arterial pulse to recover; (e) the time taken for the blisters to disappear; (f) the time taken for the skin color to return to normal; and (g) the time before bandage removal.
Subcutaneous hematomas were graded according to hematoma range, pain, blistering, and skin pulse, as follows: mild skin swelling with range less than one third of the forearm = level 1 or below (mild to normal); moderate skin swelling with range from one third to half of the forearm = level 1–2, occasionally with blistering and/or bruising (normal to moderate); and severe skin swelling with range greater than half of the forearm = level 2, or above if blistering, cyanosis, numbness, and weakness occur (severe).
Statistical Analysis
Data in the present study were analyzed using statistical software SPSS 15.0. Measurement data were expressed as mean ± standard deviation (x ± SD). Count data were expressed as percentages (%). A test of normality was conducted using the W-test, and homogeneity of variance was tested using the F-test. An intergroup comparison was conducted using a t-test. Non-normally distributed means of multiple samples or normally distributed means of multiple samples with heterogeneity of variance were compared using a non-parametric test. Counting data were compared using a Chi-square test. The correlation was tested using logistic and Cox regression analysis, and a survival analysis curve was drawn. P < 0.05 was considered statistically significant.
Results
General Data
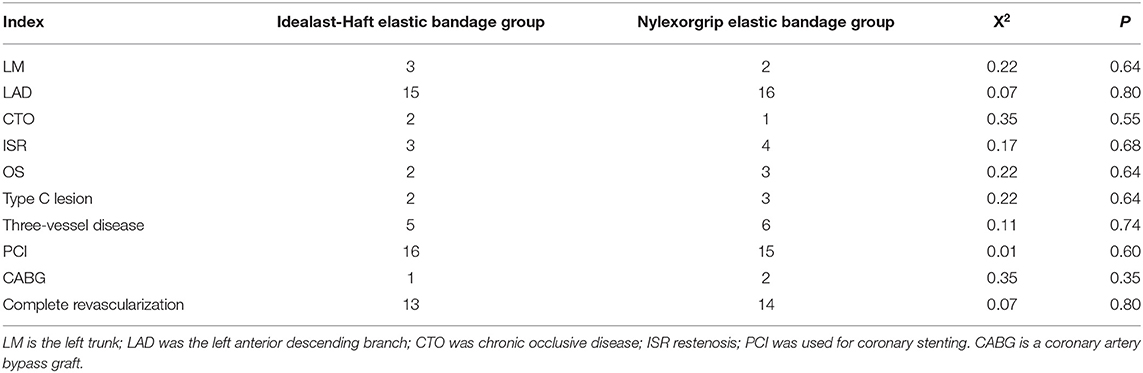
A total of 60 patients with moderate or severe forearm hematoma following transradial coronary intervention were enrolled in this study and randomly divided into two groups, namely, an Idealast-haft elastic bandage group and a control group (for each group, n = 30). The differences in general data, including age, gender, height, weight, smoking history, hypertension, diabetes, red blood cell count, hemoglobin level, platelet count, activated partial thromboplastin time, activated clotting time, levels of epidermal growth factor receptor, aspartate aminotransferase, alanine aminotransferase, antiplatelet drugs, and intraoperative heparin dosage between the two groups were not statistically significant (P > 0.05), as shown in Tables 2–4.
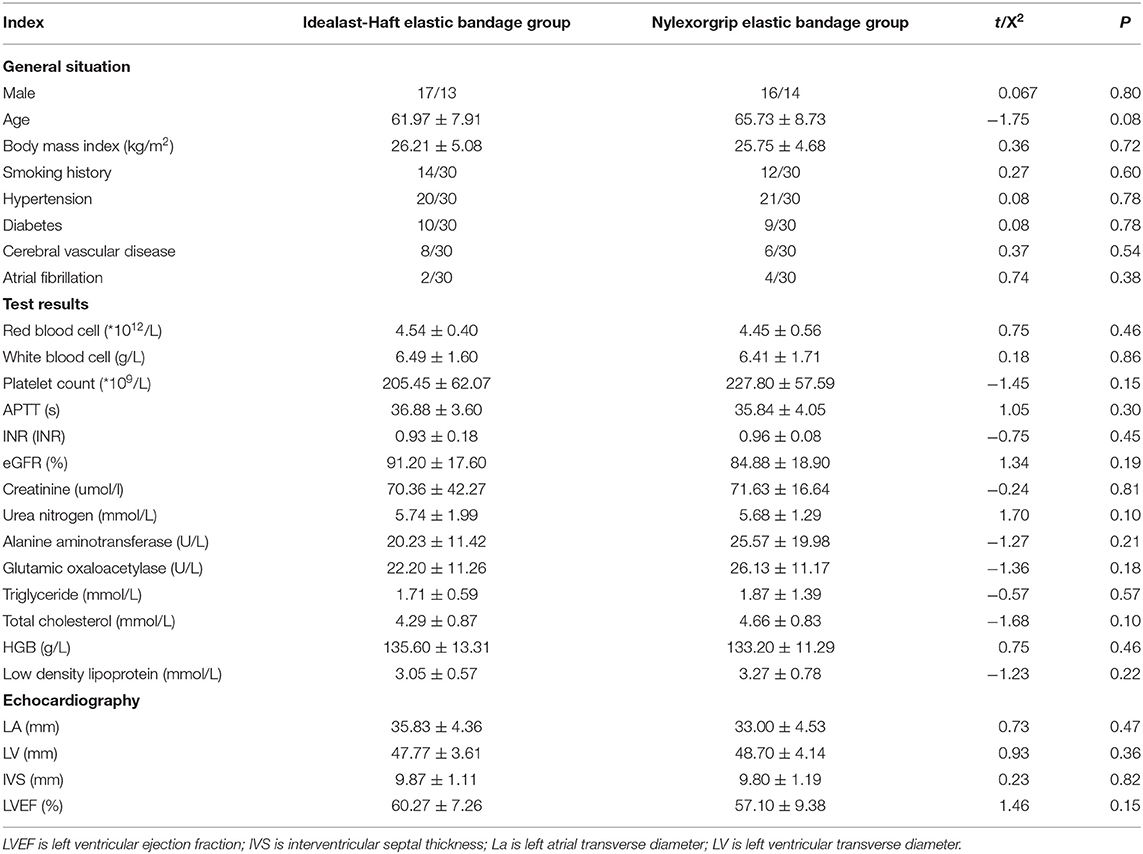
Table 2. Comparison of clinical baseline characteristics and laboratory test results between the two groups.
Improvement of Forearm Hematoma
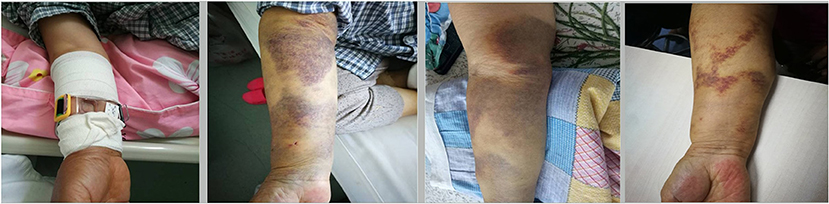
The status of the forearm hematoma (including the speed of reduction of the hematoma range, the speed of reduction of the arm circumference at the severest part of the hematoma, the time taken for pain to disappear, the time taken for the arterial pulse to recover, the time taken for blisters to disappear, the time taken for the skin color to return to normal, and the time before bandage removal) were significantly better in the Idealast-haft elastic bandage group than in the control group (P < 0.05). Brachial artery thrombosis with severe tension hematoma occurred in one patient in the control group after the discontinuation of antithrombotic drugs, and the patient was forced to undergo a surgical incision and thrombectomy, as shown in Figures 1–5. The details are presented in Table 5.
Discussion
We found that the time taken for pain disappearance, arterial pulse recovery, blister disappearance, skin color recovery, and compression hemostasis were significantly shorter in the Idealast-haft elastic bandage group than in the control group, and the differences were statistically significant (P < 0.05). The hematoma range and arm circumference at the severest part of the hematoma decreased more rapidly in the observation group than in the control group; again, the differences were statistically significant (P < 0.05). The Idealast-haft elastic bandage should therefore be used for patients with forearm hematoma following transradial coronary intervention as it is more effective than the Nylexorgrip elastic bandage.
For forearm hematoma, prevention is more important than treatment. The intent of our center is to focus on prevention through the following means. (1) Preoperative prevention: The modified Allen's test is the most convenient preoperative evaluation method, and is routine in most centers. A finger oxygen saturation test and B ultrasound can also be chosen to monitor radial artery blood flow. (2) Intraoperative prevention: The occurrence of forearm hematoma is affected by the skill of the operator, the condition of the brachial artery, and the use of antithrombotic drugs before and during the operation. During the operation, the number of punctures should be minimized, and the operation should be gentle; when the guidewire is difficult to ascend, radial arteriography should be performed immediately, and a smooth guidewire with hydrophilic coating should be used. (3) Postoperative prevention: If the puncture site is not properly compressed after the operation, blood can leak into the subcutaneous tissue of the forearm. The presence and the condition of the hematoma in the position of the pressure apparatus and the forearm should be observed, particularly at three time points, namely, by the surgeon when the operation is completed and when the instruments are removed, by the assistant after the surgeon steps down, and by the nurse after the patient returns to the ward. Meanwhile, attention should be paid to the aggravation of ischemia symptoms such as pain, numbness, and abnormal activity, and the pressure of the elastic bandaging should be reduced every 2 h. Elastic bandaging that is too tight will lead to venous blood reflux obstruction; if this continues over a long period of time, it may slow the blood flow in the hand, and the nerve endings may become dull due to the lack of oxygen, leading to numbness (10–12). Pain at the compression site is mainly due to compression of the nerve (13). If the above situation occurs, the bandage should be released immediately to aid decompression (14). The Idealast-haft elastic bandage comprises of polyester fiber (45%), cotton (42%), and fiber adhesive (13%), with an adhesive coating made of natural rubber. The main materials of the Nylexorgrip elastic bandage are fiber adhesive (46%), face glue (42%), and elastic fiber (9%); it is covered with latex particles. These two types of elastic bandage differ somewhat in their materials, and the respective manufacturer of each has its peculiar craft.
Cold compression with an ice bag at the swelling area can shrink blood vessels and slow down blood flow, thereby relieving pain, bleeding, and hematoma. In a study involving a total of 38 patients with forearm hematoma following coronary intervention, Berner et al. compared the results of injecting dehydrating agents in the hand dorsal vein between the affected and the non-affected sides. They found that injection in the hand dorsal vein of the affected side could relieve pain faster, promote better edema regression, and reduce the occurrence of tension blisters (15). Jonker et al. compared the curative effects of tension hematoma on the anterior wall following coronary intervention of hand compression, elastic bandage compression alone, and bandage compression combined with dehydration. The results revealed that bandage compression combined with dehydration had a better clinical effect (16). When the patient has numbness, inactivity, and finger dyskinesia, clinicians should be alert to osteofascial compartment syndrome and, if necessary, puncture or surgical incision and drainage should be performed. Sphygmomanometer cuff compression is relatively convenient and simple to use, and is therefore a method worthy of tentative clinical application. Many centers currently use this method (17, 18).
The current treatment in most medical centers is local compression hemostasis using a pressure apparatus and an elastic bandage. When the radial artery is punctured, the puncture needle is inserted at 30°-45° to the skin. Therefore, when a forearm hematoma occurs in our center, first, the position of the pressure apparatus is checked and adjusted to ensure that it is 0.5 cm above the subcutaneous entry point (near the heart end), which is the center point for local compression hemostasis. However, sometimes blood spreads to the surrounding area along the tissue gap, resulting in subcutaneous bleeding and forearm hematoma. In such cases, our center mostly uses elastic bandages to wholly wrap the hematoma site and moderately compress it. The pressure of the elastic bandage should be maintained within the levels in which the pulsation of the radial artery of the affected limb can be felt, and patients should be monitored for the presence of pain, numbness, abnormal activity, and other ischemic symptoms. If these occur, the bandage should be released and the pressure should be reduced (19). At present, widely used elastic bandages include the German Idealast-haft bandage and the French Nylexorgrip bandage. The hemostatic effect will differ between bandages due to the different materials used, the manufacturing processes, tension, and other factors. The results of our study suggest that the Idealast-haft bandage has better curative effects in treating forearm hematomas than the Nylexorgrip bandage.
In this study, severe tension hematoma of the forearm occurred in one patient following the interventional operation, necessitating the use of general antithrombotic drugs, embolization of the brachial artery of the right upper limb, surgical incision, and embolectomy. The reason may be that the subcutaneous hematoma was found late and could not be treated in time; in addition, once it was discovered, we overemphasized compression with elastic bandaging at the hematoma and ignored timely hemostasis at the puncture point. In other words, although elastic bandage tension has the effect of local compression hemostasis, it must be carried out on the local puncture point. The discontinuation of antithrombotic drugs also indirectly induced brachial artery embolism. Therefore, the decision of whether to discontinue antithrombotic drugs should be individualized, and the risk of bleeding and thrombosis in the upper limbs and coronary artery should be weighed repeatedly (20).
There are some limitations to this study. First, although this was a randomized controlled trial, it was not blinded; therefore, a risk of bias remains. Second, this was a single-center clinical trial and the sample size is small. A multicenter clinical trial with a larger sample size is needed.
Conclusion
Although prevention is more important than treatment for forearm hematoma, the results of this study suggest that, when a forearm hematoma occurs, the Idealast-haft elastic bandage has a better compressive effect than the Nylexorgrip bandage and is, therefore, worthy of clinical popularization.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Langfang people hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Author Contributions
LA and W-lD conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. LA, X-NY, and C-YZ collected data, carried out the initial analyses, and reviewed and revised the manuscript. Z-MX coordinated, supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by Scientific Research project of Langfang Science and Technology Bureau in 2016 (project number: 2016013019). The funding body had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors are particularly grateful to all the people who have given them help on their article.
References
1. Anjum I, Khan MA, Aadil M, Faraz A, Farooqui M, Hashmi A. Transradial vs. Transfemoral approach in cardiac catheterization: a literature review. Cureus. (2017) 9:e1309. doi: 10.7759/cureus.1309
2. Aamir S, Mohammed S, Sudhir R. Transradial approach for coronary procedures in the elderly population. J Geriatr Cardiol. (2016) 13:798–806. doi: 10.11909/j.issn.1671-5411.2016.09.002
3. Erdil A, Akbulut N, Altan A, Demirsoy MS. Comparison of the effect of therapeutic elastic bandage, submucosal dexamethasone, or dexketoprofen trometamol on inflammatory symptoms and quality of life following third molar surgery: a randomized clinical trial. Clin Oral Investig. (2020) 25:1849–57. doi: 10.1007/s00784-020-03487-y
4. Borra V, Berry DC, Zideman D, Singletary E, De Buck E. Compression wrapping for acute closed extremity joint injuries: a systematic review. J Athl Train. (2020) 55:789–800. doi: 10.4085/1062-6050-0093.20
5. Allende-Carrera R, Viana-Rojas JA, Saldierna-Galván A, López-Quijano JM, Rivera-Arellano JJ, Leiva-Pons JL, et al. Feasibility of single catheter intervention for multivessel coronary artery disease using transradial approach. Arch Cardiol Mex. (2019) 89:160–6. doi: 10.24875/ACME.M19000037
6. Garg N, Umamaheswar KL, Kapoor A, Tewari S, Khanna R, Kumar S, et al. Incidence and predictors of forearm hematoma during the transradial approach for percutaneous coronary interventions. Indian Heart J. (2019) 71:136–42. doi: 10.1016/j.ihj.2019.04.014
7. Cesaro A, Moscarella E, Gragnano F, Perrotta R, Diana V, Pariggiano I, et al. Transradial access versus transfemoral access: a comparison of outcomes and efficacy in reducing hemorrhagic events. Expert Rev Cardiovasc Ther. (2019) 17:435–47. doi: 10.1080/14779072.2019.1627873
8. Lee L, Kern J, Bair J, Rosenberg J, Lee M, Nathan S. Clinical determinants of radial artery caliber assessed at the time of transradial cardiac catheterization using routine prospective radiobrachial angiography. Cardiovasc Revasc Med. (2018) 19:939–43. doi: 10.1016/j.carrev.2018.08.025
9. Stajic Z, Romanovic R, Tavciovski D. Forearm approach for percutaneous coronary procedures. Acta Inform Med. (2013) 21:283–7. doi: 10.5455/aim.2013.21.283-287
10. Sugimoto A, Iwamoto J, Tsumuraya N, Nagaoka M, Ikari Y. Acute compartment syndrome occurring in forearm with relatively small amount of hematoma following transradial coronary intervention. Cardiovasc Interv Ther. (2016) 31:147–50. doi: 10.1007/s12928-015-0328-2
11. Andrews E, Lezotte J, Ackerman AM. Lingual compression for acute macroglossia in a COVID-19 positive patient. BMJ Case Rep. (2020) 13:e237108. doi: 10.1136/bcr-2020-237108
12. Gong S, Dong Y, Gunderson TM, Andrijasevic NM, Kashani KB. Elastic bandage vs hypertonic albumin for diuretic-resistant volume-overloaded patients in intensive care unit: a propensity-match study. Mayo Clin Proc. (2020) 95:1660–70. doi: 10.1016/j.mayocp.2020.03.029
13. Torres-Lacomba M, Navarro-Brazález B, Prieto-Gómez V, Ferrandez JC, Bouchet JY, Romay-Barrero H. Effectiveness of four types of bandages and kinesio-tape for treating breast-cancer-related lymphoedema: a randomized, single-blind, clinical trial. Clin Rehabil. (2020) 34:1230–41. doi: 10.1177/0269215520935943
14. Conde Montero E, Serra Perrucho N, de la Cueva Dobao P. Theory and practice of compression therapy for treating and preventing venous ulcers. Actas Dermosifiliogr. (2020) 111:829–34. doi: 10.1016/j.adengl.2020.10.022
15. Berner JE, Will P, Geoghegan L, Troisi L, Nanchahal J, Jain A. Safety and effectiveness of early compression of free flaps following lower limb reconstruction: a systematic review. J Plast Reconstr Aesthet Surg. (2020) 73:1604–11. doi: 10.1016/j.bjps.2020.05.011
16. Jonker L, Todhunter J, Robinson L, Fisher S. Open-label, randomised, multicentre crossover trial assessing two-layer compression bandaging for chronic venous insufficiency: results of the APRICOT trial. Br J Community Nurs. (2020) 25:S6–13. doi: 10.12968/bjcn.2020.25.Sup6.S6
17. Shalhoub J, Lawton R, Hudson J, Baker C, Bradbury A, Dhillon K, et al. Graduated compression stockings as adjuvant to pharmaco-thromboprophylaxis in elective surgical patients (GAPS study): randomised controlled trial. BMJ. (2020) 369:m1309. doi: 10.1136/bmj.m1309
18. Phillips CJ, Humphreys I, Thayer D, Elmessary M, Collins H, Roberts C, et al. Cost of managing patients with venous leg ulcers. Int Wound J. (2020) 17:1074–82. doi: 10.1111/iwj.13366
19. Rademakers LM, Laarman GJ. Critical hand ischaemia after transradial cardiac catheterisation: an uncommon complication of a common procedure. Neth Heart J. (2012) 20:372–5. doi: 10.1007/s12471-012-0276-8
Keywords: transradial coronary intervention, subcutaneous hematoma, elastic bandage, thrombosis, nylexorgrip elastic bandage
Citation: An L, Du W-l, Yang X-N, Zhang C-Y and Xue Z-M (2021) Comparison of the Efficacy of Two Elastic Bandages for Forearm Hematoma After Transradial Coronary Intervention. Front. Surg. 8:709489. doi: 10.3389/fsurg.2021.709489
Received: 14 May 2021; Accepted: 05 August 2021;
Published: 16 September 2021.
Edited by:
Pradeep Narayan, Rabindranath Tagore International Institute of Cardiac Sciences (RTIICS), IndiaReviewed by:
Sufina Shales, Rabindranath Tagore International Institute of Cardiac Sciences (RTIICS), IndiaPietro Cefali', ASST Papa Giovanni XXIII, Italy
Biswarup Purkayastha, Calcutta Medical Research Institute, India
Copyright © 2021 An, Du, Yang, Zhang and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zeng-Ming Xue, eHVlemVuZ21pbmcwOUAxNjMuY29t
 Lei An1
Lei An1 Zeng-Ming Xue
Zeng-Ming Xue