
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg., 28 June 2021
Sec. Genitourinary Surgery and Interventions
Volume 8 - 2021 | https://doi.org/10.3389/fsurg.2021.689782
Objective: To identify the effect of music on outpatient-based cystoscopy.
Methods: We systematically reviewed the effect of music on all reported outpatient for cystoscopy and extracted data from randomized trials from inception to February 3, 2021, with no language restrictions. The analysis was completed via STATA version 14.2.
Results: A total of 27 studies were initially identified, and 6 articles containing 639 patients were included in the final analysis. In terms of post-procedural pain perception, a pooled analysis of 6 articles containing 639 patients showed that music seems to improve discomfort in patients who undergo cystoscopy (WMD: −1.72; 95%CI: −2.37 to −1.07). This improvement remained consistent in patients undergoing flexible cystoscopy (FC) (WMD: −1.18; 95% CI: −1.39 to −0.98) and rigid cystoscopy (RC) (WMD: −2.56; 95% CI: −3.64 to −1.48). The music group also had less post-procedural anxiety than those in no music group during cystoscopy (WMD: −13.33; 95% CI: −21.61 to −5.06), which was in accordance with the result of FC (WMD: −4.82; 95% CI: −6.38 to −3.26) than RC (WMD: −26.05; 95% CI: −56.13 to 4.04). Besides, we detected a significantly lower post-procedural heart rate (HR) in the music group than no music group during cystoscopy (WMD: −4.04; 95% CI: −5.38 to −2.71), which is similar to the results of subgroup analysis for FC (WMD: −3.77; 95% CI: −5.84 to −1.70) and RC (WMD: −4.24; 95% CI: −5.98 to −2.50). A pooled analysis of three trials indicated that patients in the music group had significantly higher post-operative satisfaction visual analog scale (VAS) scores than those in the no-music group during RC. However, there was no significant difference between the music group and no music group regarding post-procedural systolic pressures (SPs) during cystoscopy (WMD: −3.08; 95% CI: −8.64 to 2.49). For male patients undergoing cystoscopy, the music seemed to exert a similar effect on decreasing anxiety and pain, and it might serve as a useful adjunct to increase procedural satisfaction.
Conclusions: These findings indicate that listening to music contributes to the improvement of pain perception, HR, and anxiety feeling during cystoscopy, especially for male patients undergoing RC. Music might serve as a simple, inexpensive, and effective adjunct to sedation during cystoscopy.
Cystoscopy is well-recognized as one of the most frequent procedures in outpatient urology, which is almost performed under local anesthesia. Urologists usually recommend their patients for a cystoscopy to figure out the etiology of lower urinary tract symptoms, such as hematuria, suspicious bladder tumor, and recurrent urinary tract infections (1, 2). However, the feelings of pain and anxiety discourage many patients from undergoing this clinical examination (2). For the past decades, clinical practitioners have tried various methods to alleviate the suffering of patients, such as parenteral agents (3), inhalational agents (4), intraurethral lidocaine (5), watching relaxing video (6, 7), bag squeeze (8), and flexible cystoscopy (FC) (9), but it can be difficult to achieve complete pain relief during cystoscopy under local anesthesia.
Music therapy was established as an adjuvant treatment to be beneficial in a variety of clinical settings including dental extractions, coronary heart disease, during colonoscopy, and prostate biopsies (10–13). Currently, an increasing number of original articles have been developed to explore its potentiality in cystoscopy. Despite two previous reviews (14, 15) showing a beneficial effect of music on urologic outpatient cystoscopy, the evidence remains underpowered. The present study aimed to evaluate the efficacy of music as an adjunct to routine local anesthesia in reducing pain and anxiety in patients undergoing cystoscopy.
In accordance with the preferred reporting items for systematic review and meta-analysis (PRISMA) guidelines (16), we conducted a systematic literature search by using PubMed, the Cochrane Library, and Embase using the search terms of “music” and “cystoscopy” before February 3, 2021, without any language limitations to identify possible studies.
We used the PICOS method to define the inclusion criteria. Patients (P): patients undergoing FC or rigid cystoscopy (RC); intervention (I): listening to music during cystoscopy; comparison (C) of publications to compare music with no music; outcomes (O): post-procedural pain perception measured by visual analog scale (VAS) ranging from 0 to 10 (17). High scores on the scale indicate that pain intensity is high. Post-procedural anxiety levels were measured by the State-Trait Anxiety Inventory (STAI) questionnaire (18), which consists of 20 questions. STAI scores range from 20 to 80, and a higher score indicated a greater anxiety level. Post-procedural satisfaction was assessed by VAS, and a higher VAS score represented a greater satisfaction level. Post-procedural heart rate (HR) or the pulse and systolic pressure (SP) were also measured. Study design (S): The included studies were all randomized controlled trials (RCTs). Exclusion criteria included the following items: (1) meeting abstracts and reviews including meta-analysis; (2) no systemic sedation or analgesia before cystoscopy; (3) current urinary infection; (4) presence of current pain in the pelvic region (e.g., a bladder pain syndrome or interstitial cystitis); (5) pregnancy; (6) prior urethral surgery; (7) cystoscopy with other interventions; and (8) data not available. Figure 1 shows the flowchart of the selection process of the study.
Two authors were independently involved to screen the search results in the following order to remove duplicates, title, abstract, and finally full text according to prespecified standardized criteria. Disagreements were resolved by discussion. Two independent reviewers used the preformulated tables to extract data. The following data were extracted: the name of the first author, year of publication, country, period, age, sample size, music type, local anesthesia, and cystoscopy type.
Two independent authors evaluated the methodological quality of the studies according to the Cochrane Collaboration's risk of bias (RoB) tool in Review Manager software (19). This tool primarily evaluates 7 domains: random sequence generation (selection bias); allocation concealment (selection bias); blinding of participants and personnel (performance bias); blinding of outcome assessment (detection bias); incomplete outcome data (attrition bias); selective reporting (reporting bias); and other bias (such as funding sources). In addition, two reviewers independently rated the level of evidence (LoE) of the included articles through the Oxford Centre for Evidence-Based Medicine criteria (20); This scale graded studies from strongest (level 1) to weakest (level 5) strength of evidence according to the study design and data quality.
Figure 2 shows the RoB summary of the six RCTs (21–26). Overall, included studies had a low risk of selection bias, attrition bias, and reporting bias. However, the risk of performance bias was high. The risk of detection bias was unclear due to the absence of related descriptions.
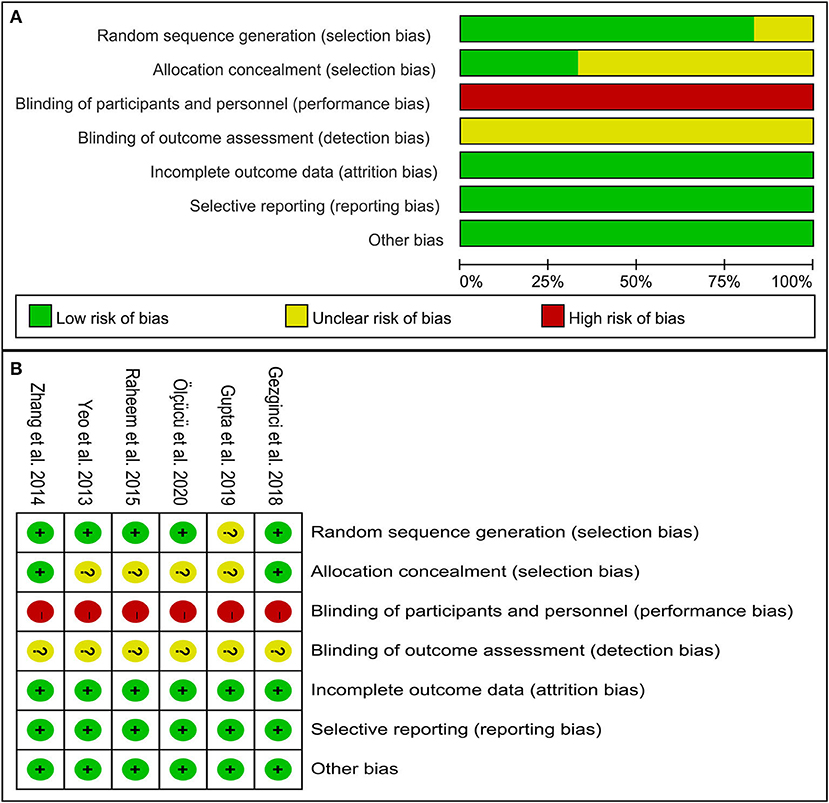
Figure 2. The methodological quality of studies included in this study. (A) Risk of bias graph. (B) Risk of bias summary.
The continuous variables were described as means ± SD. Median and range were used to estimate mean and SD (27). The percentiles, 25th, and 75th percentiles as well as 5th and 95th percentiles, were transformed to SD by using the following formula: SD ≈ Norm IQR = (P75−P25) × 0.7413 (IQR: inter-quartile range, P75: 75th percentile, P25: 25th percentile) (28). Mean difference (MD) was pooled for continuous variables. The fixed-effects model was used unless there exists heterogeneity (I2 > 50%, p < 0.1), and the level of significance was set at p < 0.05. Additionally, we performed a subgroup analysis based on gender. Besides, we conducted subgroup analyses for types of cystoscopy and male patients. This meta-analysis was completed by STATA version 14.2.
A total of 27 studies were initially identified, and 6 articles (21–26) containing 639 patients were included in the final analyses. The participants in this meta-analysis were from China, the USA, Turkey, Korea, and India. Four of six studies (21, 23–25) enrolled only male patients, and three of six studies (21–23) used FC. Five of six studies (21–25) followed intraurethral administration of 2% lidocaine jelly prior to cystoscopy, and only one study (26) made use of 2% xylocaine jelly before RC to conduct local anesthesia. Table 1 shows the main characteristics of studies included in this meta-analysis.
In terms of post-procedural pain perception, a pooled analysis of six articles (21–26) containing 639 patients showed that patients listening to music experienced less significant discomfort than their counterparts during cystoscopy (WMD: −1.72; 95% CI: −2.37 to −1.07). This improvement remained consistent in patients undergoing FC (WMD: −1.18; 95% CI: −1.39 to −0.98) and RC (WMD: −2.56; 95% CI: −3.64 to −1.48). Patients in the music group also had less post-procedural anxiety feeling than those in no music group during cystoscopy (WMD: −13.33; 95% CI: −21.61 to −5.06), which was in accordance with the result of FC (WMD: −4.82; 95% CI: −6.38 to −3.26) than RC (WMD: −26.05; 95% CI: −56.13 to 4.04). Besides, we detected a significantly lower post-procedural HR in the music group than no music group during cystoscopy (WMD: −4.04; 95% CI: −5.38 to −2.71), which is similar to the results of subgroup analysis for FC (WMD: −3.77; 95% CI: −5.84 to −1.70) and RC (WMD: −4.24; 95% CI: −5.98 to −2.50). A pooled analysis of three trials (24–26) indicated that patients in the music group had significantly higher post-operative satisfaction VAS scores than those in the no music group during RC. However, there was no significant difference between the music group and the no music group regarding post-procedural SP during cystoscopy (WMD: −3.08; 95% CI: −8.64 to 2.49). Figure 3 presents the meta-analysis results of estimated outcomes.
A pooled analysis of four articles (21, 23–25) including 402 male participants showed that there was significantly less post-procedural pain perception for patients in the music group than those in the no music group (WMD: −1.48; 95% CI: −2.26 to −0.70). These results were coincidentally stratified by FC (WMD: −0.92; 95% CI: −1.29 to −0.54) and RC (WMD: −2.29; 95% CI: −3.95 to −0.63). Four articles (21, 23–25) reported post-procedural anxiety. Meta-analysis showed that patients listening to music had significantly less anxiety feeling compared with the control group (CG) (WMD: −14.96; 95% CI: −24.70 to 5.22), but no difference was identified between the two groups of patients undergoing RC (WMD: −26.05; 95% CI: −56.13 to 4.04). A pooled analysis of three articles (21, 24, 25) showed that lower post-procedural HR was identified in the music group compared with the no music group during cystoscopy (WMD: −3.96; 95% CI: −5.67 to −2.25), as well as during RC (WMD: −4.17; 95% CI: −6.75 to −1.59). Besides, a pooled analysis of two studies (24, 25) showed that patients in the music group experienced significantly higher post-operative satisfaction VAS scores (WMD: 3.29; 95% CI: 1.78 to 4.81) and lower post-procedural SPs (WMD: −7.96; 95% CI: −13.57 to −2.34) compared with those in the no music group. Figure 4 presents the results of subgroup analysis of male patients.
In many urological institutions, an intraurethral instillation of 2% lidocaine gel is often required to provide local anesthesia and to reduce pain before cystoscopy (5, 29). However, cystoscopy is invasive and might lead to increased pain perception and anxiety levels, despite local anesthesia. Patients having high anxiety levels usually experience longer pain and require more analgesics (30, 31), because anxiety is frequently related to increased pain perception (32, 33). In the present study, we found that music intervention was significantly associated with decreased pain perception, anxiety, and HR levels. Furthermore, this improvement was more pronounced for patients undergoing RC, which was consistent with previous studies (9, 34, 35). They observed that FC was more tolerable than RC, especially in male patients (9, 35). Besides, patients in the music group had higher satisfaction VAS scores than those in the CG during RC.
It is well-known that there are anatomical gender differences with respect to urethra (36). Males have prostate, tight sphincter, and longer urethra (23, 36). Thus, male patients suffer more painful experiences than females (21, 23). Given this, we also conducted a subgroup analysis for male patients undergoing cystoscopy. We demonstrated a beneficial effect of music on pain perception, anxiety levels, HR, and SP. Furthermore, male patients undergoing RC seem to benefit more and are more satisfied with music intervention as well. Compared to other systematic reviews, the present review performed a subgroup analysis of gender and added three new studies updating the evidence level.
The present study does have some limitations. First, the limited number of studies, sample sizes, the study population, the experience of the surgeon, and the definition of outcome measures make it difficult to emphatically confirm the advantage of music intervention. Besides, the ethnic differences in penis and diameters of FC might affect the results. Second, the surgeons were not blinded during the procedure, so it is potentially possible that patients in the music group could get more careful manipulation than those in the CG. Finally, VAS and STAI scores are self-reported outcomes of patients, which are partly subjective. We still need to develop more objective parameters and multicenter trials with a large number of patients to yield better results.
These findings indicate that listening to music contributes to the improvement of pain perception, HR, and anxiety feeling during cystoscopy, especially for male patients undergoing RC. Besides, music might increase procedural satisfaction for male patients undergoing RC as well. Music might serve as a simple, inexpensive, and effective adjunct to sedation during cystoscopy.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
LY: conception and design. CT and GC: administrative support. YuhL, GC, and YueL: provision of study materials or patients. YD and YueL: collection and assembly of data. YuhL and GC: data analysis and interpretation. GC: manuscript drafting. All authors: final approval of manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Burke DM, Shackley DC, O'Reilly PH. The community-based morbidity of flexible cystoscopy. BJU international. (2002) 89:347–9. doi: 10.1046/j.1464-4096.2001.01899.x
2. Greenstein A, Greenstein I, Senderovich S, Mabjeesh NJ. Is diagnostic cystoscopy painful? Analysis of 1,320 consecutive procedures. Int Braz J Urol. (2014) 40:533–8. doi: 10.1590/S1677-5538.IBJU.2014.04.13
3. Song YS, Song ES, Kim KJ, Park YH, Ku JH. Midazolam anesthesia during rigid and fexible cystoscopy. Urol Res. (2007) 35:139–42. doi: 10.1007/s00240-007-0091-7
4. Calleary JG, Masood J, Van-Mallaerts R, Barua JM. Nitrous oxide inhalation to improve patient acceptance and reduce procedure related pain of fexible cystoscopy for men younger than 55 years. J Urol. (2007) 178:184–8. doi: 10.1016/j.juro.2007.03.036
5. Raskolnikov D, Brown B, Holt SK, Ball AL, Lotan Y, Strope S, et al. Reduction of pain during flexible cystoscopy: a systematic review and meta-analysis. J Urol. (2019) 202:1136–42. doi: 10.1097/JU.0000000000000399
6. Patel AR, Jones JS, Angie S, Babineau D. Office based flexible cystoscopy may be less painful for men allowed to view the procedure. J Urol. (2007) 177:1843–5. doi: 10.1016/j.juro.2007.01.070
7. Gezginci E, Bedir S, Ozcan C, Iyigun E. Does watching a relaxing video during cystoscopy affect pain and anxiety levels of female patients? A randomized controlled trial. Pain Manag Nurs. (2021) 22:214–9. doi: 10.1016/j.pmn.2020.08.005
8. Berajoui MB, Aditya I, Herrera-Caceres J, Qaoud Y, Lajkosz K, Ajib K, et al. A prospective randomized controlled trial of irrigation “Bag Squeeze” to manage pain for patients undergoing flexible cystoscopy. J Urol. (2020) 204:1012–8. doi: 10.1097/JU.0000000000001139
9. Krajewski W, Kościelska-Kasprzak K, Rymaszewska J, Zdrojowy R. How different cystoscopy methods influence patient sexual satisfaction, anxiety, and depression levels: a randomized prospective trial. Qual Life Res. (2017) 26:625–34. doi: 10.1007/s11136-016-1493-1
10. López-Cepero Andrada JM, Amaya Vidal A, Castro Aguilar-Tablada T, García Reina I, Silva L, Ruiz Guinaldo A, et al. Anxiety during the performance of colonoscopies: modifcation using music therapy. Eur J Gastroenterol Hepatol. (2004) 16:1381–6. doi: 10.1097/00042737-200412000-00024
11. Bradt J, Dileo C, Potvin N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database Syst Rev. (2013) 12:CD006577. doi: 10.1002/14651858.CD006577.pub3
12. Packyanathan JS, Lakshmanan R, Jayashri P. Effect of music therapy on anxiety levels on patient undergoing dental extractions. J Family Med Prim Care. (2019) 8:3854–60. doi: 10.4103/jfmpc.jfmpc_789_19
13. Song M, Li N, Zhang X, Shang Y, Yan L, Chu J, et al. Music for reducing the anxiety and pain of patients undergoing a biopsy: a meta-analysis. J Adv Nurs. (2018) 74:1016–29. doi: 10.1111/jan.13509
14. García-Perdomo HA, Montealegre Cardona LM, Cordoba-Wagner MJ, Zapata-Copete JA. Music to reduce pain and anxiety in cystoscopy: a systematic review and meta-analysis. J Complement Integr Med. (2018). 16:/j/jcim.2019.16.issue-3/jcim-2018-0095/jcim-2018-0095.xml. doi: 10.1515/jcim-2018-0095
15. Kyriakides R, Jones P, Geraghty R, Skolarikos A, Liatsikos E, Traxer O, et al. Effect of music on outpatient urological procedures: a systematic review and meta-analysis from the European association of urology section of uro-technology. J Urol. (2018) 199:1319–27. doi: 10.1016/j.juro.2017.11.117
16. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
17. Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. (1997) 72:95–97. doi: 10.1016/S0304-3959(97)00005-5
18. Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press (1983).
19. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0. The Cochrane Collaboration. (2013).
20. Centre for Evidence-Based Medicine. Oxford Centre for Evidence-Based Medicine: Levels of Evidence. (2009). Available online at: http://www.cebm.net/oxfordcentreevidence-based-medicine-levels-evidencemarch-2009/
21. Zhang ZS, Wang XL, Xu CL, Zhang C, Cao Z, Xu WD, et al. Music reduces panic: an initial study of listening to preferred music improves male patient discomfort and anxiety during flexible cystoscopy. J Endourol. (2014) 28:739–44. doi: 10.1089/end.2013.0705
22. Raheem OA, Mirheydar HS, Lee HJ, Patel ND, Godebu E, Sakamoto K. Does listening to music during office-based flexible cystoscopy decrease anxiety in patients: a prospective randomized trial. J Endourol. (2015) 29:791–6. doi: 10.1089/end.2015.0029
23. Ölçücü MT, Yilmaz K, Karamik K, Okuducu Y, Özsoy Ç, Aktaş Y, et al. Effects of listening to binaural beats on anxiety levels and pain scores in male patients undergoing cystoscopy and ureteral stent removal: a randomized placebo-controlled trial. J Endourol. (2020) 35:54–61. doi: 10.1089/end.2020.0353
24. Yeo JK, Cho DY, Oh MM, Park SS, Park MG. Listening to music during cystoscopy decreases anxiety, pain, and dissatisfaction in patients: a pilot randomized controlled trial. J Endourol. (2013) 27:459–62. doi: 10.1089/end.2012.0222
25. Gezginci E, Iyigun E, Kibar Y, Bedir S. Three distraction methods for pain reduction during cystoscopy: a randomized controlled trial evaluating the effects on pain, anxiety, and satisfaction. J Endourol. (2018) 32:1078–84. doi: 10.1089/end.2018.0491
26. Gupta S, Das SK, Jana D, Pal DK. Distraction during cystoscopy to reduce pain and increase satisfaction: randomized control study between real-time visualization versus listening to music versus combined music and real-time visualization. Urol Ann. (2019) 11:33–8. doi: 10.4103/UA.UA_191_17
27. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) 5:13. doi: 10.1186/1471-2288-5-13
28. Yang L, Wang G, Du Y, Ji B, Zheng Z. Remote ischemic preconditioning reduces cardiac troponin I release in cardiac surgery: a meta-analysis. J Cardiothorac Vasc Anesth. (2014) 28:682–9. doi: 10.1053/j.jvca.2013.05.035
29. Aaronson DS, Walsh TJ, Smith JF, Davies BJ, Hsieh MH, Konety BR. Meta-analysis: does lidocaine gel before flexible cystoscopy provide pain relief? BJU international. (2009) 104:506–10. doi: 10.1111/j.1464-410X.2009.08417.x
30. Vaughn F, Wichowski H, Bosworth G. Does preoperative anxiety level predict postoperative pain? AORN J. (2007) 85:589–604. doi: 10.1016/S0001-2092(07)60130-6
31. Taenzer P, Melzack R, Jeans ME. Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain. (1986) 24:331–42. doi: 10.1016/0304-3959(86)90119-3
32. Jones A, Spindler H, Jørgensen MM, Zachariae R. The effect of situation-evoked anxiety and gender on pain report using the cold pressor test. Scand J Psychol. (2002) 43:307–13. doi: 10.1111/1467-9450.00299
33. Michaelides A, Zis P. Depression, anxiety and acute pain: links and management challenges. Postgrad Med. (2019) 131:438–44. doi: 10.1080/00325481.2019.1663705
34. Casteleijn NF, Vriesema JL, Stomps SP, van Balen OL, Cornel EB. The effect of office based flexible and rigid cystoscopy on pain experience in female patients. Investig Clin Urol. (2017) 58:48–53. doi: 10.4111/icu.2017.58.1.48
35. Seklehner S, Remzi M, Fajkovic H, Saratlija-Novakovic Z, Skopek M, Resch I, et al. Prospective multi-institutional study analyzing pain perception of flexible and rigid cystoscopy in men. Urology. (2015) 85:737–41. doi: 10.1016/j.urology.2015.01.007
Keywords: anxiety, cystoscopy, music, pain, effect
Citation: Chen G, Tang C, Liu Y, Liu Y, Dai Y and Yang L (2021) Does Listening to Music Improve Pain Perception and Anxiety in Patients Undergoing Cystoscopy: A Meta-Analysis. Front. Surg. 8:689782. doi: 10.3389/fsurg.2021.689782
Received: 13 April 2021; Accepted: 31 May 2021;
Published: 28 June 2021.
Edited by:
Christian P. Meyer, University Medical Center Hamburg-Eppendorf, GermanyReviewed by:
Julia Kaulfuss, Klinik für Urologie, Charité Universitätsmedizin Berlin, GermanyCopyright © 2021 Chen, Tang, Liu, Liu, Dai and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luo Yang, eWFuZ2x1bzUzMUBxcS5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.