- Department of Gastroenterology Surgery, Affiliated Hospital of Qingdao University, Qingdao, China
Groin hernioplasty is the most performed intervention in the adults worldwide, the minimally invasive inguinal hernia repair techniques widely used by surgeons today are transabdominal preperitoneal patch plasty (TAPP) and total extraperitoneal patch plasty (TEP). We report a 62-year-old man with bowel obstruction caused by the use of self-anchoring barbed suture to close the peritoneum 3 days after TAPP. Surgeons using the barbed suture should be alert to this possibility when encountering this complication of intestinal obstruction, so as to avoid more serious consequences.
Introduction
Since the 1990s, laparoscopic inguinal hernioplasty has been performed more frequently worldwide. The laparoscopic approach can be either transperitoneal or retroperitoneal. Transabdominal preperitoneal (TAPP) repair is commonly performed because of its advantages as a minimally invasive approach, resulting in less postoperative discomfort, better cosmesis, and a shorter hospital stay (1). TAPP inguinal hernia repair involves dissection of the preperitoneal space, mesh repair of the hernia defect, and closure of the peritoneum (2). A barbed suture is often applied to facilitate closure of the peritoneum. One of these novel sutures is V-Loc™ (Covidien, Mansfield, MA, USA), which consists of a unidirectional barbed absorbable thread equipped with a surgical needle at one end and a loop at the opposite end to secure the suture. However, as demonstrated in several case reports (3, 4), a potential drawback to the use of barbed suture is that exposed suture barbs may catch on the adjacent small bowel, mesentery, or omentum and cause serosal injury, obstruction, or volvulus. We herein present a case of postoperative small bowel obstruction (SBO) after TAPP repair that was directly related to the use of barbed suture.
Case Report
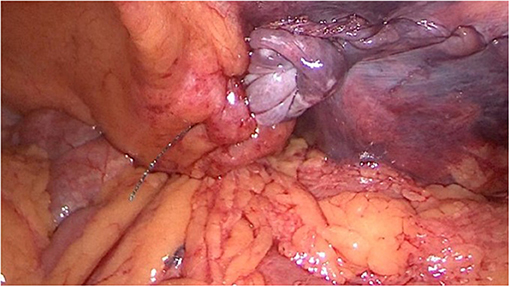
A 62-year-old man with a body mass index of 18.5 kg/m2 presented with symptomatic bilateral inguinal hernias. The bilateral inguinal hernias were evident on clinical and ultrasound examinations. TAPP repair was performed by an experienced surgeon at the Department of Gastroenterology Surgery, Affiliated Hospital of Qingdao University. After stripping the right hernia sac, a 15- ×10-cm partially absorbable mesh (Ultrapro UMM1, Johnson & Johnson Medical, USA) was fixed at multiple points with 2 mL of medical glue (Compont® Beijing Compont Medical Devices Co., Ltd., Beijing, China) using a laparoscopic sprayer. V-loc™ absorbable barbed suture was used to close the peritoneum, leaving about 2 cm of exposed suture in the abdominal cavity (Figure 1). The patient was in stable condition after surgery and was discharged on postoperative day 1.
The patient presented to the emergency room on postoperative day 2 with severe abdominal pain and no flatulence or defecation for 2 days. Abdominal computed tomography showed mild small intestinal dilation and the “whirlpool sign,” consistent with intestinal volvulus (Figure 2). Considering these imaging findings combined with clinical signs consistent with intestinal volvulus, emergency laparoscopy, was performed. The small intestinal membrane was found to be stuck in the lower right quadrant by the reverse hook of the V-loc™ suture that had previously been used to close the peritoneum, and the surrounding intestines exhibited significant congestive edema (Figure 3). After cutting the V-loc™ suture and performing derotation, good reperfusion was obtained. The patient recovered well and was discharged on postoperative day 2. Upon hospital discharge, physical examination revealed no abdominal softness or pressure pain, and he was able to tolerate food and perform bowel movements.
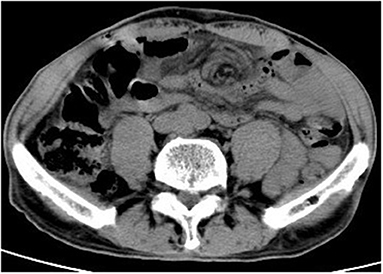
Figure 2. CT of the abdomen on re-admission, the red arrow indicates the “vortex sign” that marks volvulus.
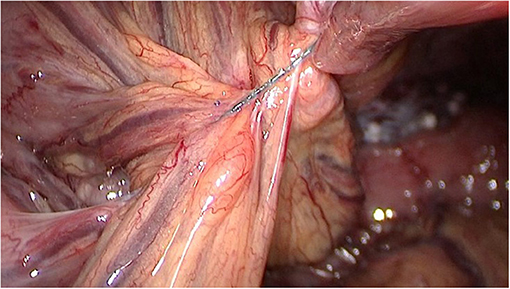
Figure 3. Emergency laparoscopy revealed that the barbed sutures were firmly entangled with the mesenteric.
Discussion
The overall complication rate of TAPP repair is low because of technological advances. Statistical data indicate that the incidence of SBO after TAPP repair ranges from 0.2% to 0.5% (5) and is usually attributed to inadequate peritoneal closure, trocar site herniation, or adhesion (6). We identified other case reports similar to ours, in which a self-anchoring barbed suture remained after TAPP repair and caused SBO (7, 8). Although such cases are rare, they provide many clinical learning points.
Complete closure of the peritoneum during TAPP repair is a very important step. On one hand, it prevents intestinal adhesion and obstruction caused by mesh exposure. On the other hand, it can prevent the intestine from entering the preperitoneal space (2, 9). Closure can be achieved with staples, tacks, running suture, or glue. Among these options, application of running suture is more time-consuming to perform but less painful to the patient (9). In recent years, self-anchoring barbed suture such as V-loc™ has eliminated the need for knot tying and has thus been welcomed by clinicians (10). The efficacy and suitability of barbed sutures have been reported in the fields of gynecologic surgery (11, 12), plastic surgery (13), urology, orthopedic surgery (14, 15), and general surgery (16).
The use of self-anchoring barbed suture saves time but is also associated with several risks. In the present case, the free suture in the abdominal cavity was firmly fixed to the mesentery of the small bowel, forming a rivet point. The mesentery and small intestine became entangled at this point during peristalsis, causing intestinal volvulus. If surgery is not performed in a timely manner in such cases, more serious ischemic intestinal obstruction will occur and intestinal necrosis may even develop. Sartori et al. (17) reported a case of SBO after TAPP hernia repair using a barbed suture. The patient returned 3 days postoperatively with typical signs of bowel obstruction. Additionally, Lee and Wong (18) reported a case of SBO caused by barbed sutures 6 weeks after laparoscopic myomectomy. Api et al. (19) established a rat model and found that barbed suture material might be associated with adhesion formation when used intra-abdominally and that these adhesions could not be prevented by peritonization. Notably, these clinical cases and animal models had a common feature: the barbed suture was left in the abdominal cavity and directly contacted the intestine or mesentery.
Conclusions
Self-anchoring barbed suture has a wide range of indications and good performance. More importantly, however, it must be used correctly to reduce the risk of complications. The cases discussed herein emphasize that although barbed sutures can be applied more rapidly and conveniently under laparoscopy, the free end of the barbed suture remaining in the abdominal cavity may adhere to the intestine or mesentery, resulting in an intestinal obstruction. This complication can be avoided by either preventing exposure of excess suture in the abdominal cavity or using conventional absorbable sutures for peritoneal closure. A high degree of suspicion for this complication is warranted in patients who show typical signs after surgery. Early diagnosis and treatment should be ensured to avoid adverse consequences such as intestinal necrosis, which will seriously affect the prognosis.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Affiliated Hospital of Qingdao University School of Medicine. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
LZ and XY draft the manuscript. SW, HL, and JH edited the manuscript. All authors were involved in the clinical care of the patient and approved the final version of the manuscript at time of submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Angela Morben, DVM, ELS, from Liwen Bianji, Edanz Editing China (www.liwenbianji.cn/ac), for editing the English text of a draft of this manuscript.
References
1. Kockerling F, Jacob DA, Lomanto D, Chowbey P. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia. Surg Endosc. (2012) 26:2394–5. doi: 10.1007/s00464-012-2191-x
2. McKay R. Preperitoneal herniation and bowel obstruction post laparoscopic inguinal hernia repair: case report and review of the literature. Hernia. (2008) 12:535–7. doi: 10.1007/s10029-008-0341-9
3. Filser J, Reibetanz J, Krajinovic K, Germer CT, Dietz UA, Seyfried F. Small bowel volvulus after transabdominal preperitoneal hernia repair due to improper use of V-Loc barbed absorbable wire - do we always “read the instructions first”? Int J Surg Case Rep. (2015) 8C:193–5. doi: 10.1016/j.ijscr.2015.02.020
4. Chen H, Hong MK, Ding DC. Acute small bowel obstruction caused by barbed suture on the second day after laparoscopic hysterosacropexy: a case report and literature review. Taiwan J Obstet Gynecol. (2017) 56:247–9. doi: 10.1016/j.tjog.2016.03.008
5. Fitzgerald HL, Orenstein SB, Novitsky YW. Small bowel obstruction owing to displaced spiral tack after laparoscopic TAPP inguinal hernia repair. Surg Laparosc Endosc Percutan Tech. (2010) 20:e132–5. doi: 10.1097/SLE.0b013e3181dfbc05
6. Kapiris SA, Brough WA, Royston CM, O'Boyle C, Sedman PC. Laparoscopic transabdominal preperitoneal (TAPP) hernia repair. A 7-year two-center experience in 3017patients. Surg Endosc. (2001) 15:972–5. doi: 10.1007/s004640080090
7. Kohler G, Mayer F, Lechner M, Bittner R. Small bowel obstruction after TAPP repair caused by a self-anchoring barbed suture device for peritoneal closure: case report and review of the literature. Hernia. (2015) 19:389–94. doi: 10.1007/s10029-014-1301-1
8. Tagliaferri EM, Wong TS, Abad DJJ, Bergmann H, Hammans S, Seidlmayer CM. Small bowel obstruction SBO after TAPP repair caused by a self-anchoring barbed suture device for peritoneal closure: case report. J Surg Case Rep. (2018) 2018:y165. doi: 10.1093/jscr/rjy165
9. Bittner R, Arregui ME, Bisgaard T, Dudai M, Ferzli GS, Fitzgibbons RJ, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia [International Endohernia Society (IEHS)]. Surg Endosc. (2011) 25:2773–843. doi: 10.1007/s00464-011-1799-6
10. Takayama S, Nakai N, Shiozaki M, Ogawa R, Sakamoto M, Takeyama H. Use of barbed suture for peritoneal closure in transabdominal preperitoneal hernia repair. World J Gastrointest Surg. (2012) 4:177–9. doi: 10.4240/wjgs.v4.i7.177
11. Einarsson JI, Chavan NR, Suzuki Y, Jonsdottir G, Vellinga TT, Greenberg JA. Use of bidirectional barbed suture in laparoscopic myomectomy: evaluation of perioperative outcomes, safety, and efficacy. J Minim Invasive Gynecol. (2011) 18:92–5. doi: 10.1016/j.jmig.2010.10.003
12. Naki MM, Api O, Acioglu HC, Ozkan S, Kars B, Unal O. Comparative study of a barbed suture, poliglecaprone and stapler in Pfannenstiel incisions performed for benign gynecological procedures: a randomized trial. Acta Obstet Gynecol Scand. (2010) 89:1473–7. doi: 10.3109/00016349.2010.516815
13. Warner JP, Gutowski KA. Abdominoplasty with progressive tension closure using a barbed suture technique. Aesthet Surg J. (2009) 29:221–5. doi: 10.1016/j.asj.2009.01.009
14. Williams SB, Alemozaffar M, Lei Y, Hevelone N, Lipsitz SR, Plaster BA, et al. Randomized controlled trial of barbed polyglyconate versus polyglactin suture for robot-assisted laparoscopic prostatectomy anastomosis: technique and outcomes. Eur Urol. (2010) 58:875–81. doi: 10.1016/j.eururo.2010.07.021
15. Tewari AK, Srivastava A, Sooriakumaran P, Slevin A, Grover S, Waldman O, et al. Use of a novel absorbable barbed plastic surgical suture enables a “self-cinching” technique of vesicourethral anastomosis during robot-assisted prostatectomy and improves anastomotic times. J Endourol. (2010) 24:1645–50. doi: 10.1089/end.2010.0316
16. Milone M, Di Minno MN, Galloro G, Maietta P, Bianco P, Milone F, et al. Safety and efficacy of barbed suture for gastrointestinal suture: a prospective and randomized study on obese patients undergoing gastric bypass. J Laparoendosc Adv Surg Tech A. (2013) 23:756–9. doi: 10.1089/lap.2013.0030
17. Sartori A, De Luca M, Clemente N, De Luca A, Scaffidi G, Piatto G, et al. Small bowel occlusion after trans-abdominal preperitoneal hernia approach caused by barbed suture: case report and review of literature. G Chir. (2019) 40:322–4.
18. Lee ET, Wong FW. Small bowel obstruction from barbed suture following laparoscopic myomectomy-A case report. Int J Surg Case Rep. (2015) 16:146–9. doi: 10.1016/j.ijscr.2015.09.039
Keywords: inguinal hernia, TAPP, small bowel, obstruction, postoperative
Citation: Zheng L, Yin X, Liu H, Wang S and Hu J (2021) Case Report: Small Bowel Obstruction Owing to Self-Anchoring Barbed Suture Device After TAPP Repair. Front. Surg. 8:646091. doi: 10.3389/fsurg.2021.646091
Received: 25 December 2020; Accepted: 21 January 2021;
Published: 11 February 2021.
Edited by:
René H. Fortelny, Wilhelminenspital, AustriaReviewed by:
Franz Mayer, University Hospital Salzburg, AustriaJan Frank Kukleta, Independent researcher, Zurich, Switzerland
Copyright © 2021 Zheng, Yin, Liu, Wang and Hu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jilin Hu, Y2FybGh1NjImI3gwMDA0MDsxMjYuY29t
 Longbo Zheng
Longbo Zheng Xiangyi Yin
Xiangyi Yin Huasheng Liu
Huasheng Liu