
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 18 June 2021
Sec. Orthopedic Surgery
Volume 8 - 2021 | https://doi.org/10.3389/fsurg.2021.603589
This article is part of the Research Topic Innovations and New Technology in Spine Surgery View all 16 articles
 Fei-Long Wei1†
Fei-Long Wei1† Ming-Rui Du1†
Ming-Rui Du1† Tian Li2†
Tian Li2† Kai-Long Zhu1†
Kai-Long Zhu1† Yi-Li Zhu2
Yi-Li Zhu2 Xiao-Dong Yan1
Xiao-Dong Yan1 Yi-Fang Yuan1
Yi-Fang Yuan1 Sheng-Da Wu1
Sheng-Da Wu1 Bo An1
Bo An1 Hao-Ran Gao1*
Hao-Ran Gao1* Ji-Xian Qian1*
Ji-Xian Qian1* Cheng-Pei Zhou1*
Cheng-Pei Zhou1*Background: Percutaneous endoscopic decompression (PED) is a minimally invasive surgical technique that is now used for not only disc herniation but also lumbar spinal stenosis (LSS). However, few studies have reported endoscopic surgery for LSS. Therefore, we conducted this study to evaluate the outcomes and safety of large channel endoscopic decompression.
Methods: Forty-one patients diagnosed with LSS who underwent PED surgery were included in the study. The estimated blood loss, operative time, length of hospital stay, hospital costs, reoperations, complications, visual analogue scale (VAS) score, Oswestry Disability Index (ODI) score, Japanese Orthopaedic Association (JOA) score and SF-36 physical-component summary scores were assessed. Preoperative and postoperative continuous data were compared through paired-samples t-tests. The significance level for all analyses was defined as p < 0.05.
Results: A total of 41 consecutive patients underwent PED, including 21 (51.2%) males and 20 (48.8%) females. The VAS and ODI scores decreased from preoperatively to postoperatively, but the JOA and SF-36 physical component summary scores significantly increased. The VAS (lumbar) score decreased from 5.05 ± 2.33 to 0.45 ± 0.71 (P = 0.000); the VAS (leg) score decreased from 5.51 ± 2.82 to 0.53 ± 0.72 (P = 0.000); the ODI score decreased from 52.80 ± 20.41 to 4.84 ± 3.98 (P = 0.000), and the JOA score increased from 11.73 ± 4.99 to 25.32 ± 2.12 (P = 0.000). Only 1 patient experienced an intraoperative complication (2.4%; dural tear), and 1 patient required reoperation (2.4%).
Conclusions: Surgical treatment for LSS is to sufficiently decompress and minimize the trauma and complications caused by surgery. This study did not reveal any obvious shortcomings of PED and suggested PED is a safe and effective treatment for LSS.
Degenerative lumbar spinal stenosis (LSS) is characterized by changes in the spinal structure (such as facet joints and ligaments) due to aging, resulting in a reduction in the diameter of the spinal canal (1). LSS is the most common spinal pathology in the elderly population, and the number of patients who need to undergo surgery for the disease has increased (2–4). In the United States, the prevalence of relatively narrow LSS (i.e., 12 mm tube diameter) is as high as 22.5% in the general population, and that of absolute stenosis (i.e., 10 mm tube diameter) is as high as 7.3% (5). These figures increase sharply with age, reaching 47.2 and 19.4%, respectively, among people aged 60 years or older (6). LSS greatly reduces patient quality of life (7).
Minimally invasive surgery techniques are becoming increasingly important in spinal surgery to protect the multifidus muscle, a stabilizer for the spine and locomotor actions (2, 8, 9). At present, endoscopic surgery, a minimally invasive surgery technique, is considered to be an extension of alternative to spinal surgery (10). The surgical indications for endoscopic spine surgery are still increasing due to the release of practical and reliable clinical results (11, 12). Spinal endoscopy is now used to treat not only disc herniation but also LSS (13). Previously, a key obstacle was the need to remove enough bone and the ligamentum flavum under continuous visualization to achieve decompression (14). Advances in technology have made it possible to treat LSS with percutaneous endoscopic decompression (PED) (14, 15).
Although many surgical techniques are available for the treatment of lumbar spinal stenosis, there is little evidence to support this rapidly developing surgical technique, and clinicians often rely on their own opinions and experience (16–18). Few studies have investigated endoscopic surgery for LSS, and their evaluation indicators were relatively simple (19–21). Therefore, we conducted this study to evaluate the efficacy and safety of endoscopic surgery for LSS. In addition, this is the first study to systematically evaluate the application of large channel endoscopy in LSS.
This was a retrospective study. The study protocol was approved by the hospital ethics committee and performed according to the Declaration of Helsinki. Between January 2012 and December 2018, 41 patients diagnosed with LSS who underwent PED were included in the study. The inclusion criteria were as follows: (1) patients with LSS due to neurogenic claudication; (2) Central stenosis or lateral stenosis who need surgery; (3) Low-grade (Meyerding grade 1 or 2) isthmic spondylolisthesis or degenerative spondylolisthesis; (4) patients with imaging findings consistent with the symptoms. The exclusion criteria included trauma, active infection, malignant tumors, spinal deformity, previous lumbar fusion, multi-segment fusion, multi-level, high-grade (Meyerding grade 3 or 4) isthmic spondylolisthesis or degenerative spondylolisthesis; obvious lumbar instability in the surgical segment (the change of cobb angle in hyperextension and flexion is >11° or displacement is >3 mm). A representative case is shown in Figure 1.
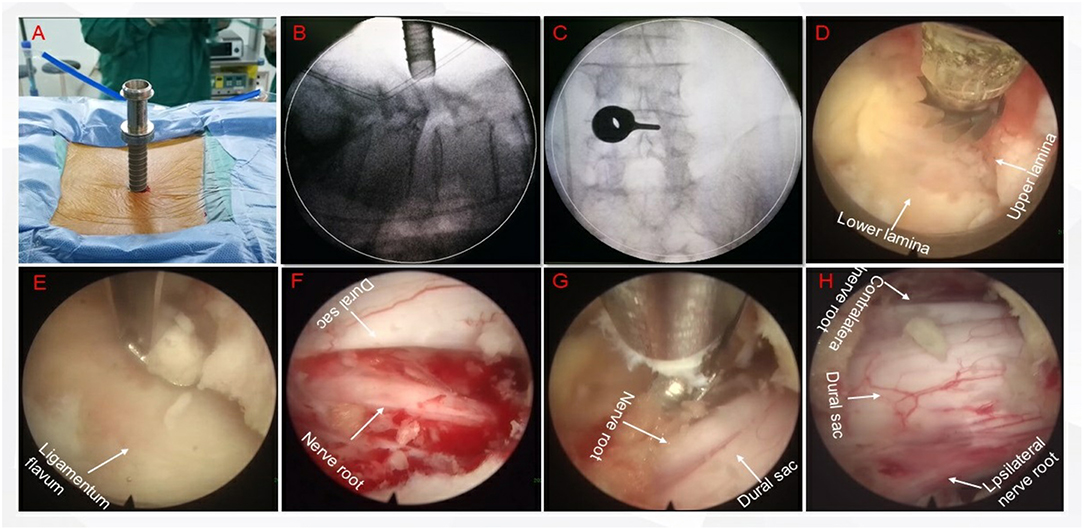
Figure 1. A representative case. (A) Place the working channel; (B) Lateral X-ray fluoroscopy confirms that the channel is facing the intervertebral space; (C) Positive X-ray fluoroscopy confirms that the channel is located inside the facet joint; (D) Clean up the soft tissue on the surface of the lamina, confirm the lamina space and upper and lower lamina; E. Remove the lamina and expose the ligamentum flavum; (F) Decompression of the nerve root on the same side, ranging from the initial segment of the nerve root, down to the inner edge of the pedicle, explore the Ipsilateral nerve root canal to achieve at least 270° decompression of the nerve root canal; (G) Decompression of the contralateral nerve root; (H) After the decompression, the dural sac and bilateral nerve roots are visible.
The patients were treated with large-channel endoscopic decompression. The PED operation was performed with bilateral decompression through a unilateral approach. After general anesthesia, each patient was placed in the prone position, and then, the operating table was adjusted to expand the lumbar lamina space. The positioning point was located at the midpoint of the interlaminar space of the facet joint under X-ray. Then, a 15 mm incision was made at the positioning point; the skin and fascia were cut, and they were expanded step by step with a 3rd grade cannula. The depth of the expansion cannula was confirmed under fluoroscopy without breaking the ligament flavum. After the position of the cannula was confirmed to be satisfactory, the working cannula was inserted, and the expansion cannula was removed; the spinal endoscope was connected and inserted. First, the soft tissues on the lamina and ligamentum flavum were cleaned endoscopically. Bony decompression was performed using a high-speed drill under direct endoscopic vision, and then, the ligamentum flavum was removed, completing ipsilateral decompression. Then, the cannula was tilted to remove the contralateral ligamentum flavum and part of the medial bone of the upper articular process to complete contralateral decompression. After the exploration step showed that the extent of decompression was sufficient, the working sleeve was pulled out, and finally, the wound was sutured.
The blood loss, operative time, length of hospital stay, costs, reoperation rate and complications were assessed. We recorded the visual analogue scale (VAS), Oswestry Disability Index (ODI), Japanese Orthopaedic Association (JOA) and SF-36 physical component summary scores of the patients before surgery and at 2 and 3 years after surgery.
The statistical analyses were performed by SPSS (version 23.0; IBM, Chicago, IL). Preoperative and postoperative continuous data were compared through paired-samples t-tests. The significance level for all analyses was defined as p < 0.05.
Forty-one patients were included in this study, including 21 (51.2%) males and 20 (48.8%) females. The mean age was 56.76 ± 13.35 years. The patients had a mean body mass index of 25.34 ± 3.10 kg/m2. The most common surgical segment in both groups was L4/5. The mean operative time was 113.41 ± 28.69 min (60–150 min); the volume of intraoperative blood loss was 121.78 ± 82.03 mL (10–300 mL); the length of hospital stay was 10.34 ± 2.84 days (6–23 days); and the total cost was 3.57 ± 0.45 ten thousand yuan (2.89–4.62 ten thousand yuan) (Table 1).
As shown in Figures 2, 3, the VAS and ODI scores significantly decreased from pre- to postoperatively, and the JOA and SF-36 physical component summary scores increased significantly (P < 0.05). Comparing the 2-year data, the VAS (lumbar), VAS (leg) and ODI scores increased slightly with significant differences (P < 0.05).
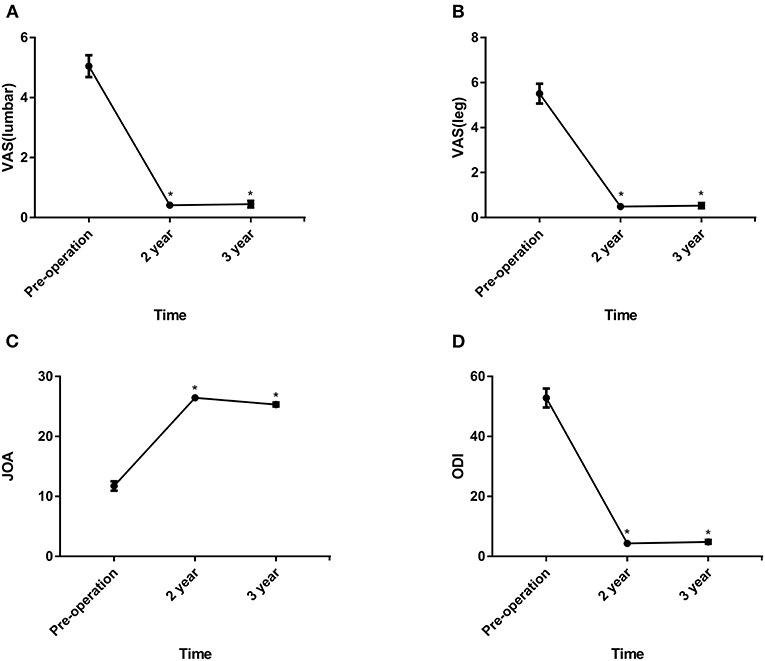
Figure 2. (A–D) The VAS (lumbar), VAS (leg), JOA and ODI scores before surgery and at 24 and 36 months postoperatively. VAS, visual analogue scale; JOA, japanese orthopaedic association; ODI, oswestry disability index. *P < 0.01, within-group comparisons between at baseline, 24 and 36 months.
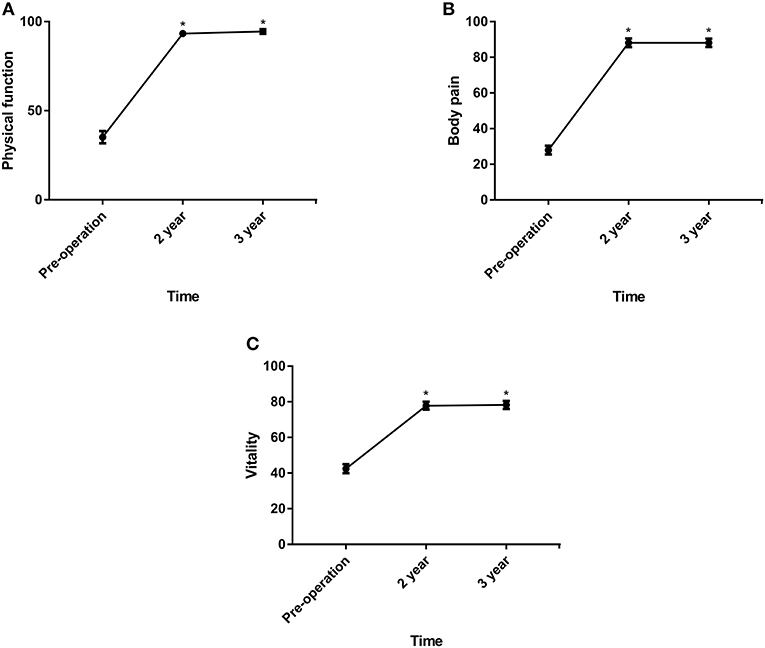
Figure 3. (A–C) The SF-36 physical component summary scores (physical function, body pain and vitality) before surgery and at 24 and 36 months postoperatively. *P < 0.01, within-group comparisons between at baseline, 24 and 36 months.
Only 1 patient experienced intra-complications (2.4%; dural tear). After 1 week of conservative treatment, the patient exhibited satisfactory recovery. No patients experienced postoperative complications, and 1 patient required reoperation (2.4%) (Table 2).
LSS is a common disease that is increasing in frequency in the elderly population worldwide, but it is also common in adults (older than 35–40 years) who commonly perform manual labor and excessively load their spine with heavy loads (22). Conventional laminectomy decompression is a surgical method commonly used for the treatment of LSS (2, 23, 24). The posterior column structure is severely damaged during laminectomy and related facet joint resection, and postoperative complications such as lumbar instability can occur (25, 26). Lumbar interbody fusion is a common treatment for LSS and can prevent lumbar spine instability (27). The resection of joint and soft-tissue structures is also required for the decompression of LSS. With the development of endoscopic technology, it is possible to achieve decompression without destroying these structures (8, 28). However, there is little evidence to support this rapidly developing surgical technique. Therefore, we conducted this study to evaluate the outcomes of PED surgery for LSS. This retrospective trial included 41 patients with LSS, including patients with or without degenerative spondylolisthesis.
The presence of degenerative spondylolisthesis is generally considered a sign of instability, although there is no consensus on the definition of the term (29). Some studies have shown that patients with degenerative spondylolisthesis may be at risk of iatrogenic spondylolisthesis or an increased degree of spondylolisthesis after decompression surgery (30). However, the clinical consequences of spondylolisthesis have been controversial for decades (31). In addition, few studies support the widespread use of fusion surgery in patients with lumbar spinal stenosis, regardless of whether there is spondylolisthesis (32). Despite the lack of a consensus on the definition of instability, surgeons often use decompression and fusion surgery as a means to prevent postoperative instability (29). Two studies have provided the main basis for this fusion surgery (33, 34), but its validity has been questioned (32). The results of a previous study revealed that the clinical efficacy of PED was reliable during a follow-up. A recent study showed that there were no substantial benefits of additionally performing fusion surgery for LSS, even in the presence of spondylolisthesis (29).
Although some studies have reported good clinical outcomes and a low complication rate for endoscopic lumbar decompression, its effect on LSS has not yet been proven. Our study showed that PED also has a satisfactory effect on LSS. In addition, advantages have been reported for PED over traditional surgery, for example, better clinical outcomes, a lower complication rate, a shorter hospital stay, and faster rehabilitation (35, 36). The slow deterioration of surgical results over time has been described, and a similar situation was found in our study at the third-year follow-up (37, 38). Overall, the patients achieved satisfactory results over an average of 3 years of follow-up. Since minimally invasive surgery eliminates the need for the removal of spinal canal structures or reduces the extent of resection, this method seems to reduce the consequences of surgery (39, 40). Postoperative ODI and VAS were significantly improved compared with preoperative values which was similar with previous study (19, 20). Our study showed that 1 patient had dural tear (complication rate of 2.4%). Dural injuries have been reported in the literature to occur at a rate ranging from 0% to ~5% (41–44). In addition, 1 patient required reoperation (2.4%) for incomplete decompression. The reoperation rate is much lower than previous study (16.7%) (20).
To date, it is still difficult to determine well-defined parameters based on evidence-based medicine standards that require fusion in addition to decompression. Some experts have pointed out that patients with predominantly leg symptoms and no signs of segmental instability or deformities should use stability-preserving decompression techniques to avoid fusion (38). Our study revealed that all patients, with or without mild degenerative spondylolisthesis, exhibited satisfactory results. The results were consistent with those of previous studies (23, 29).
This study had some limitations. In this study, the follow-up time was short, and the long-term efficacy of the PED treatment could not be evaluated. Endoscopic techniques have not been used for the treatment of LSS for very long, so the technique is not well-established. Endoscopic decompression still needs to be improved further, and the operation time can be shortened.
In conclusion, the purpose of surgical treatment for LSS is to sufficiently decompress and minimize the trauma and complications caused by surgery. In general, this study did not reveal any obvious shortcomings of PED. Therefore, we recommend PED for LSS. However, prospective randomized controlled trials are needed to verify these results. The cases that require fusion as well as decompression need to be urgently identified.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Clinical Research Ethics Committee of the Tangdu Hospital. The patients/participants provided their written informed consent to participate in this study.
F-LW, J-XQ, H-RG, TL, K-LZ, and C-PZ contributed to the revised the work critically. All authors have approved the final version to be published and have agreed to be accountable for all aspects of the work. All authors contributed substantially to the conception and design of the work, acquisition and interpretation of data, and the drafted work.
This work was supported by grants from the National Natural Science Foundation of China (No. 81871818). Sponsors were not involved in study design or implementation plans.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We would like to thank the National Natural Science Foundation of China for making this research possible.
1. Wei F-L, Liu Y, Zhou C-P, Sun S-G, Zhu K-L, Du M-R, et al. Management for lumbar spinal stenosis: protocol for a network meta-analysis and systematic review. J Ortho Surg. (2020) 28:1–6. doi: 10.1177/2309499020975212
2. Haddadi K, Ganjeh Qazvini HR. Outcome after surgery of lumbar spinal stenosis: a randomized comparison of bilateral laminotomy, trumpet laminectomy, and conventional laminectomy. Front Surg. (2016) 3:19. doi: 10.3389/fsurg.2016.00019
3. Ma X-L, Zhao X-W, Ma J-X, Li F, Wang Y, Lu B. Effectiveness of surgery versus conservative treatment for lumbar spinal stenosis: a system review and meta-analysis of randomized controlled trials. Int J Surg. (2017) 44:329–38. doi: 10.1016/j.ijsu.2017.07.032
4. Wei FL, Zhou CP, Liu R, Zhu KL, Du MR, Gao HR, et al. Management for lumbar spinal stenosis: a network meta-analysis and systematic review. Int J Surg. (2020) 85:19–28. doi: 10.1016/j.ijsu.2020.11.014
5. Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT, Toton JF, et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J. (2013) 13:734–43. doi: 10.1016/j.spinee.2012.11.059
6. Kalichman L, Cole R, Kim DH, Li L, Suri P, Guermazi A, et al. Spinal stenosis prevalence and association with symptoms: the framingham study. Spine J. (2009) 9:545–50. doi: 10.1016/j.spinee.2009.03.005
7. Katz JN, Harris MB. Clinical practice. Lumb Spinal Steno N Eng J Med. (2008) 358:818–25. doi: 10.1056/NEJMcp0708097
8. Guiot BH, Khoo LT, Fessler RG. A minimally invasive technique for decompression of the lumbar spine. Spine. (2002) 27:432–8. doi: 10.1097/00007632-200202150-00021
9. Choi CM, Chung JT, Lee SJ, Choi DJ. How I do it? Biportal endoscopic spinal surgery (BESS) for treatment of lumbar spinal stenosis. Acta Neurochir. (2016) 158:459–63. doi: 10.1007/s00701-015-2670-7
10. Lee C-H, Choi M, Ryu DS, Choi I, Kim CH, Kim HS, et al. Efficacy and safety of full-endoscopic decompression via interlaminar approach for central or lateral recess spinal stenosis of the lumbar Spine: a meta-analysis. Spine. (2018) 43:1756–64. doi: 10.1097/BRS.0000000000002708
11. Ahn Y. Endoscopic spine discectomy: indications and outcomes. Int Ortho. (2019) 43:909–16. doi: 10.1007/s00264-018-04283-w
12. Wei FL, Gao H, Yan X, Yuan Y, Qian S, Gao Q, et al. Comparison of postoperative outcomes between patients with positive and negative straight leg raising tests who underwent full-endoscopic transforaminal lumbar discectomy. Sci Rep. (2020) 10:16516. doi: 10.1038/s41598-020-73357-w
13. Ahn Y. Percutaneous endoscopic decompression for lumbar spinal stenosis. Exp Rev Med Dev. (2014) 11:605–16. doi: 10.1586/17434440.2014.940314
14. Torudom Y, Dilokhuttakarn T. Two portal percutaneous endoscopic decompression for lumbar spinal stenosis: preliminary study. Asian Spine J. (2016) 10:335–42. doi: 10.4184/asj.2016.10.2.335
15. Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study. J Neuro Spine. (2009) 10:476–85. doi: 10.3171/2008.7.17634
16. Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochr Datab Syst Rev. (2016) CD 2016:010264. doi: 10.1002/14651858.CD010264.pub2
17. Chang W, Yuwen P, Zhu Y, Wei N, Feng C, Zhang Y, et al. Effectiveness of decompression alone versus decompression plus fusion for lumbar spinal stenosis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. (2017) 137:637–50. doi: 10.1007/s00402-017-2685-z
18. Yavin D, Casha S, Wiebe S, Feasby TE, Clark C, Isaacs A, et al. Lumbar fusion for degenerative disease: a systematic review and meta-analysis. Neurosurgery. (2017) 80:701–15. doi: 10.1093/neuros/nyw,162
19. Hwa Eum J, Hwa Heo D, Son SK, Park CK. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neuro Spine. (2016) 24:602–7. doi: 10.3171/2015.7.SPINE15304
20. Eun SS, Eum JH, Lee SH, Sabal LA. Biportal endoscopic lumbar decompression for lumbar disk herniation and spinal canal stenosis: a technical note. J Neuro Surg Cent Eur Neuro. (2017) 78:390–6. doi: 10.1055/s-0036-1592157
21. Kim HS, Paudel B, Jang JS, Oh SH, Lee S, Park JE, et al. Percutaneous full endoscopic bilateral lumbar decompression of spinal stenosis through uniportal-contralateral approach: techniques and preliminary results. World Neuro. (2017) 103:201–9. doi: 10.1016/j.wneu.2017.03.130
22. Usman M, Ali M, Khanzada K, Ishaq M, Naeemul H, Aman R, et al. Unilateral approach for bilateral decompression of lumbar spinal stenosis: a minimal invasive surgery. J Coll Phys Surg Pakistan. (2013) 23:852–6.
23. Ghogawala Z, Dziura J, Butler WE, Dai F, Terrin N, Magge SN, et al. Laminectomy plus fusion vs. laminectomy alone for lumbar spondylolisthesis. N Eng J Med. (2016) 374:1424–34. doi: 10.1056/NEJMoa1508788
24. Zhao X-W, Ma J-X, Ma X-L, Li F, He W-W, Jiang X, et al. Interspinous process devices(IPD) alone versus decompression surgery for lumbar spinal stenosis (LSS): a systematic review and meta-analysis of randomized controlled trials. Int J Surg. (2017) 39:57–64. doi: 10.1016/j.ijsu.2017.01.074
25. Haher TR, O'Brien M, Dryer JW, Nucci R, Zipnick R, Leone DJ. The role of the lumbar facet joints in spinal stability. Identification of alternative paths of loading. Spine. (1994) 19:2667–70. doi: 10.1097/00007632-199412000-00012
26. Jasper GP, Francisco GM, Telfeian AE. A retrospective evaluation of the clinical success of transforaminal endoscopic discectomy with foraminotomy in geriatric patients. Pain Phys. (2013) 16:225–9. doi: 10.36076/ppj.2013/16/225
27. Kaiser MG, Eck JC, Groff MW, Watters WC, Dailey AT, Resnick DK, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 1: introduction and methodology. J Neuro Spine. (2014) 21:2–6. doi: 10.3171/2014.4.SPINE14257
28. Khoo LT, Fessler RG. Microendoscopic decompressive laminotomy for the treatment of lumbar stenosis. Neurosurgery. (2002) 51:S146–54. doi: 10.1097/00006123-200211002-00020
29. Försth P, Ólafsson G, Carlsson T, Frost A, Borgström F, Fritzell P, et al. A randomized, controlled trial of fusion surgery for lumbar spinal stenosis. N Eng J Med. (2016) 374:1413–23. doi: 10.1056/NEJMoa1513721
30. Johnsson K, Redlund-Johnell I, Udén A, Willner S. Preoperative and postoperative instability in lumbar spinal stenosis. Spine. (1989) 14:591–3. doi: 10.1097/00007632-198906000-00008
31. Hasegawa K, Kitahara K, Shimoda H, Ishii K, Ono M, Homma T, et al. Lumbar degenerative spondylolisthesis is not always unstable: clinicobiomechanical evidence. Spine. (2014) 39:2127–35. doi: 10.1097/BRS.0000000000000621
32. Martin C, Gruszczynski A, Braunsfurth H, Fallatah S, O'Neil J, Wai E. The surgical management of degenerative lumbar spondylolisthesis: a systematic review. Spine. (2007) 32:1791–8. doi: 10.1097/BRS.0b013e3180bc219e
33. Herkowitz H, Kurz L. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. The Journal of bone and joint surgery. Am Vol. (1991) 73:802–8. doi: 10.2106/00004623-199173060-00002
34. Bridwell K, Sedgewick T, O'Brien M, Lenke L, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Dis. (1993) 6:461–72. doi: 10.1097/00002517-199306060-00001
35. Feng F, Xu Q, Yan F, Xie Y, Cai L. Comparison of 7 surgical interventions for lumbar disc herniation: a network meta-analysis. Pain Phys. (2017) 20:E863–71. doi: 10.36076/ppj.20.5.E863
36. Tu Z, Li YW, Wang B, Lu G, Li L, Kuang L, et al. Clinical outcome of full-endoscopic interlaminar discectomy for single-level lumbar disc herniation: a minimum of 5-year follow-up. Pain Phys. (2017) 20:E425–30. doi: 10.36076/ppj.2017.E430
37. Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE, et al. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine. (2005) 30:936–43. doi: 10.1097/01.brs.0000158953.57966.c0
38. Komp M, Hahn P, Oezdemir S, Giannakopoulos A, Heikenfeld R, Kasch R, et al. Bilateral spinal decompression of lumbar central stenosis with the full-endoscopic interlaminar versus microsurgical laminotomy technique: a prospective, randomized, controlled study. Pain Phys. (2015) 18:61–70. doi: 10.36076/ppj/2015.18.61
39. Iida YA, Kataoka OS, Sho TO, Sumi MA, Hirose TE, Bessho YA, et al. Postoperative lumbar spinal instability occurring or progressing secondary to laminectomy. Spine. (1990) 15:1186–9. doi: 10.1097/00007632-199011010-00018
40. Zander T, Rohlmann A, Klöckner C, Bergmann G. Influence of graded facetectomy and laminectomy on spinal biomechanics. Eur Spine J. (2003) 12:427–34. doi: 10.1007/s00586-003-0540-0
41. Ruetten S, Komp M, Merk H, Godolias G. Use of newly developed instruments and endoscopes: full-endoscopic resection of lumbar disc herniations via the interlaminar and lateral transforaminal approach. J Neuro Spine. (2007) 6:521–30. doi: 10.3171/spi.2007.6.6.2
42. Nie H, Zeng J, Song Y, Chen G, Wang X, Li Z, et al. Percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation via an interlaminar approach vs. a transforaminal approach: a prospective randomized controlled study with 2-year follow up. Spine. (2016) 41(Suppl. 19):B30–37. doi: 10.1097/B.R.S.0000000000001810
43. Song H, Hu W, Liu Z, Hao Y, Zhang X. Percutaneous endoscopic interlaminar discectomy of L5-S1 disc herniation: a comparison between intermittent endoscopy technique and full endoscopy technique. J Orthop Surg Res. (2017) 12:162. doi: 10.1186/s,13018-017-0662-4
44. Liu X, Yuan S, Tian Y, Wang L, Gong L, Zheng Y, et al. Comparison of percutaneous endoscopic transforaminal discectomy, microendoscopic discectomy, and microdiscectomy for symptomatic lumbar disc herniation: minimum 2-year follow-up results. J Neuro Spine. (2018) 28:317–25. doi: 10.3171/2017.6.S.P.I.N.E.172
Keywords: lumbar spinal stenosis, outcomes, safety, large channel, endoscopic decompression
Citation: Wei F-L, Du M-R, Li T, Zhu K-L, Zhu Y-L, Yan X-D, Yuan Y-F, Wu S-D, An B, Gao H-R, Qian J-X and Zhou C-P (2021) Therapeutic Effect of Large Channel Endoscopic Decompression in Lumbar Spinal Stenosis. Front. Surg. 8:603589. doi: 10.3389/fsurg.2021.603589
Received: 07 September 2020; Accepted: 26 May 2021;
Published: 18 June 2021.
Edited by:
Vassilios S. Nikolaou, National and Kapodistrian University of Athens, GreeceReviewed by:
Konstantinos Markatos, Salamina Medical Center, GreeceCopyright © 2021 Wei, Du, Li, Zhu, Zhu, Yan, Yuan, Wu, An, Gao, Qian and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cheng-Pei Zhou, emhvdWNwZWlAMTI2LmNvbQ==; Ji-Xian Qian, cGFzbWlzczIwMTJAMTYzLmNvbQ==; Hao-Ran Gao, eGhfZ2hyQHFxLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.