- 1Department of Urology, Affiliated Hospital of Qingdao University, Qingdao, China
- 2Department of Urology, Beijing TianTan Hospital, Capital Medical University, Beijing, China
- 3Department of Urology, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, China
- 4Department of Urology, Shandong Cancer Hospital and Institute, Shandong First Medical University and Shandong Academy of Medical Sciences, Jinan, China
Background: Bipolar and monopolar transurethral resections have a stable status for non-muscle invasive bladder cancer (NMIBC). We conducted a meta-analysis to analyze the outcomes and complications of bipolar vs. monopolar energy for transurethral resection of bladder tumors (TURB).
Methods: The Preferred Reporting Items for Systematic Reviews and Meta-analyses was followed. Based on the Population, Intervention, Comparator, Outcomes, and Study Designs (PICOS) strategy, randomized controlled trials were searched in MEDLINE, EMBASE, and the Cochrane Controlled Trials Register. The reference lists of the associated articles were also retrieved. The data were calculated by Rev Man v5.3.0.
Results: Eleven publications containing an amount of 2, 099 patients were involved in the study. Two groups did not show a significant difference in the mean age and the number of bladder tumors. The results showed that m-TURB had a greater decrease in postoperative hemoglobin level [mean difference (MD) −0.26, 95% confidence interval (CI) −0.48 to −0.04, P = 0.02] and sodium level (MD −0.36, 95% CI −0.62 to −0.10, P = 0.007) compared with b-TURB. B-TURB spent relatively little in hospitalization time (MD −0.52, 95% CI −0.88 to −0.15, P = 0.005) than m-TURB with the exception of operation time (P = 0.47) and catheterization time (P = 0.19). B-TURB did not show a significant difference in the incidence rate of obturator reflex (P = 0.10), bladder perforation (P = 0.32), postoperative blood transfusion (P = 0.28), and clot retention (P = 0.21) compared with the b-TURB group. Besides, there were no significant difference in terms of muscle tissue sampling (P = 0.43), recurrence-free survival at 6 months (P = 0.68) and 12 months (P = 0.78).
Conclusions: B-TURB was more effective than m-TURB in minimizing intraoperative or postoperative bleeding with the smaller loss of hemoglobin and the shorter hospitalization time for patients with NMIBC.
Introduction
Bladder cancer is one of the most common malignancies in the United States, and its incidence rate is about 80,470 new cases and 17,670 deaths in 2019 (1, 2). In new cases, non-muscle invasive bladder cancer (NMIBC) accounts for ~80%, and urothelial carcinoma is the main type of histologic classification (3, 4).
Transurethral resection (TUR) is the basis of staging and treatment of bladder tumors (5). Transurethral resection of bladder tumors (TURB) aims to achieve a definitive diagnosis and remove visible pathological tissue including muscle tissue (6). Monopolar activated current, as a source of energy for the cutting loop, is the gold standard for the treatment of NMIBC, which is simultaneously correlated with some adverse events including blood loss and disorder of electrolyte balance (7). Recently, bipolar resection with the use of physiological saline solution has proven to be a beneficial choice in the prevention of possible complications (8–10). However, there were few sufficient evidence-based medical studies focusing on analyzing the advantages and disadvantages of the two technologies for bladder tumors.
We conducted a meta-analysis of randomized controlled trial (RCTs) to evaluate the outcomes and complications of bipolar vs. monopolar TURB.
Materials and Methods
Study Protocol
This systematic review was implemented by following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (11). Only RCTs were included in the study. Observational studies, editorials, commentaries, and review articles were excluded. Abstracts of conferences were also excluded. If a group of patients was included in two or more studies, each of the studies may have been analyzed in the present study.
Information Sources and Literature Search
Based on databases including MEDLINE (1996 to May 2020), EMBASE (1999 to May 2020), and the Cochrane Controlled Trials Register, two reviewers did a comprehensive retrieval to analyze the outcomes and complications of b-TURB vs. m-TURB. The following search terms were used: “bipolar, monopolar, TURB, and NMIBC.” The study only included published literature with restriction on English language. If necessary, authors were contacted to provide more accurate data for their research. Meanwhile, reviewers also searched for published systematic reviews and other key references. Two reviewers screened independently titles and abstracts to identify studies that met the inclusion criteria, and if there were any objections, it was referred to the third person for examination. When abstracts were insufficient to determine whether the study met the inclusion criteria, full text would be required.
Eligibility Criteria
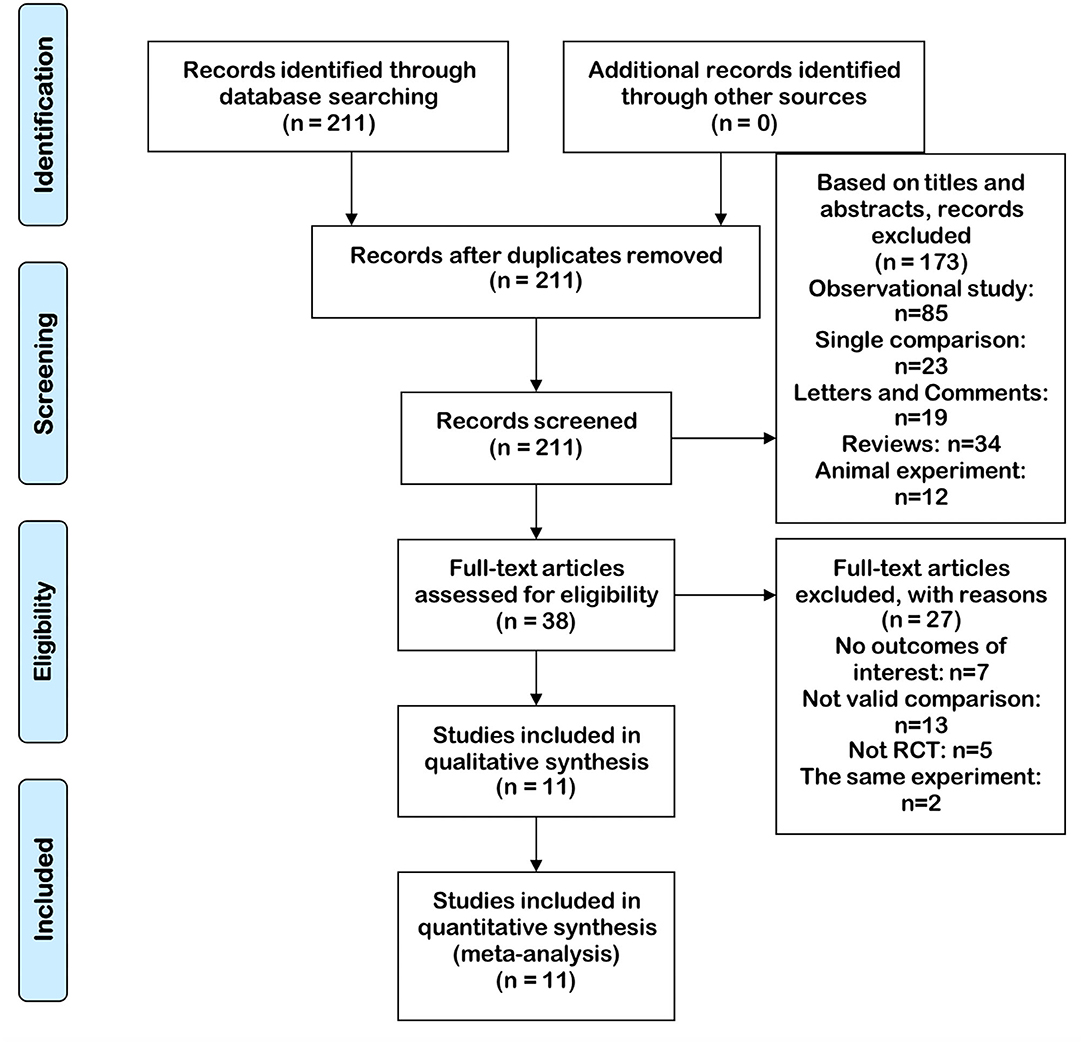
(1) B-TURB vs. m-TURB was involved. (2) Full-text could be acquired. (3) The data provided by the article were valid and valuable, mainly involving the number of cases and valuable results of each indicator. (4) The method of article was RCT. The search strategy according to the focused PICOS question is presented in Table 1. The PRISMA diagram of selection is shown in Figure 1.
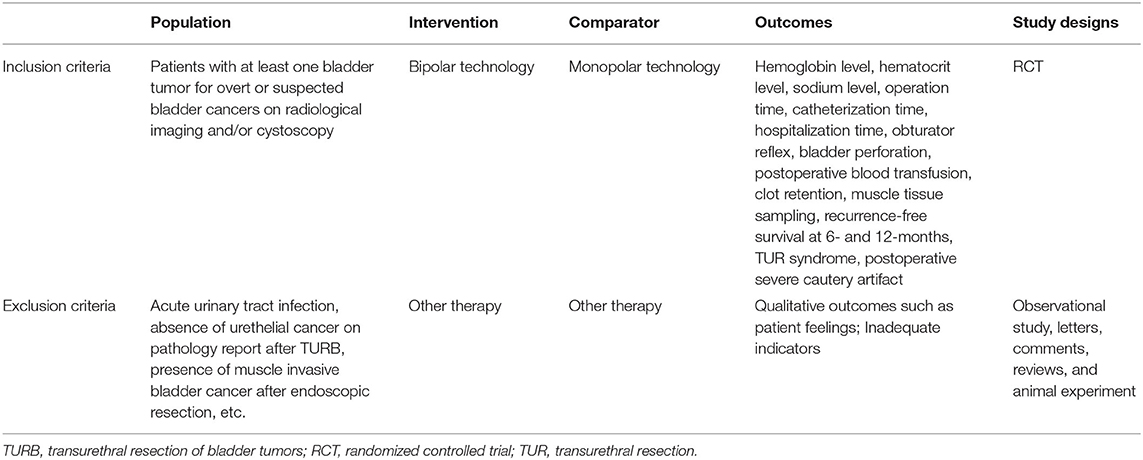
Table 1. Criteria for considering studies for the review based on the Population, Intervention, Comparator, Outcomes, and Study Designs (PICOS) Structure.
Quality Assessment Methods
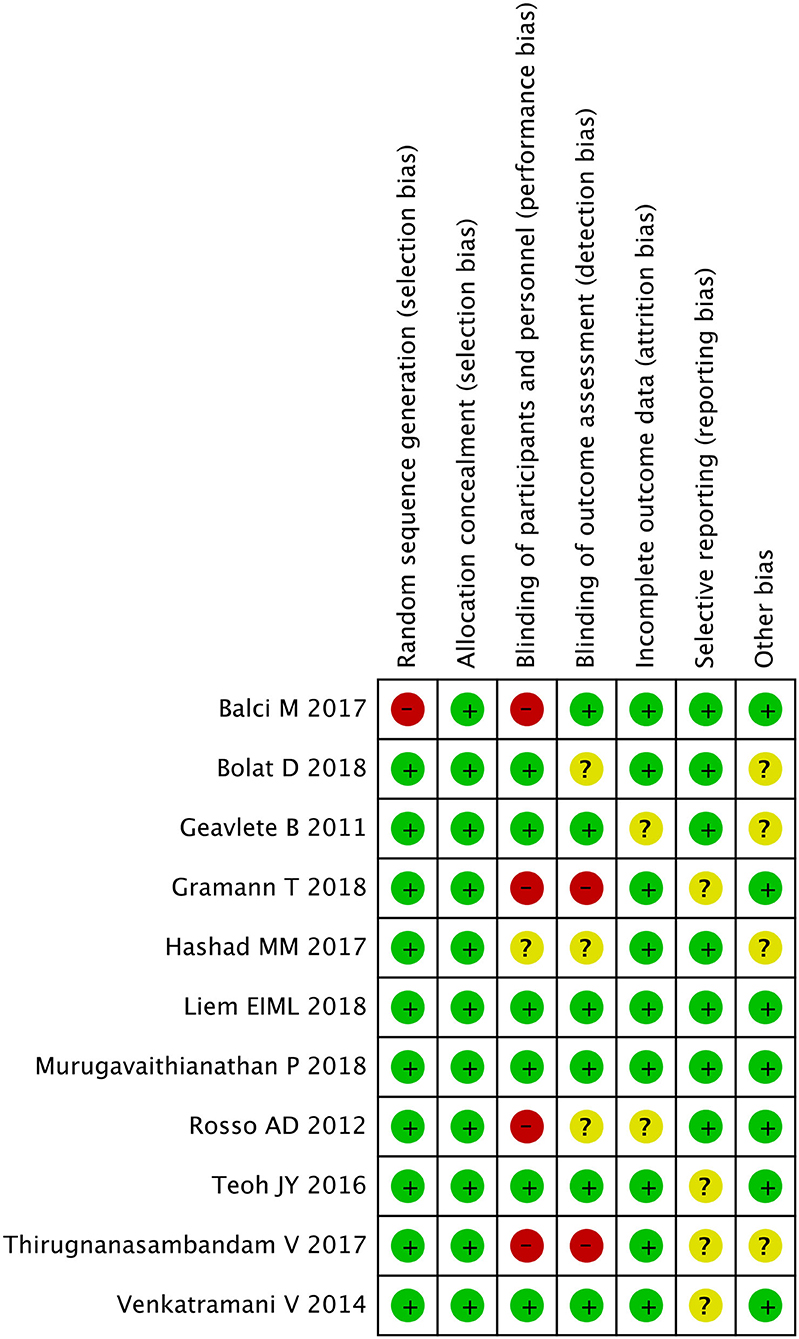
Each study was classified by the Jadad scale (12). Studies were graded in line with the principles, which are derived from the Cochrane Handbook for Systematic Reviews of Interventions v5.30 (13). Each RCT was allotted according to the following quality classification standards: (+) low potential of bias, (?) secondary probability of bias, and (–) high possibility of bias. All authors participated in the assessment of each RCT, and eventually, everyone agreed with the results. All reviewers independently assessed whether the study fitted into the criteria. Any discrepancies were recorded, discussed, and settled in a negotiated manner.
Data Extraction
Based on predetermined criteria, three reviewers independently extracted the following data from each study: (A) published time; (B) first author's name; (C) country of study; (D) the type of trial; (E) technique received; (F) number of participants; (G) mean age; (H) tumor number (single/multiple); and (I) hemoglobin level, hematocrit level, sodium level, operation time, catheterization time, hospitalization time, obturator reflex, bladder perforation, postoperative blood transfusion, clot retention, muscle tissue sampling, and recurrence-free survival at 6 and 12 months. Because these indicators had a remarkable impact on patient, they were regarded as an important aspect. No ethical approval was required for our study.
The main primary outcomes were operative time, catheterization time, and hospitalization time. The secondary outcomes were postoperative complications, tumor muscle tissue sampling, and recurrence-free survival at 6 and 12 months.
Statistical Analyses
Reman version 5.3.0 (Cochrane Collaboration, Oxford, UK) (13) was used in the analysis of data. Mean difference (MD) was applied to analyze continuous data, and the odds ratio (OR) was calculated for dichotomous results with the corresponding 95% confidence interval (CI) (14). The results of analysis showed that if the P > 0.05 for the I2 statistic, the study was considered to be homogeneous, and the fixed-effects model was used for the analysis. When heterogeneity is high, sensitivity analysis and subgroup analysis would be used to analyze the source of heterogeneity if necessary, which may understand the potential confounders that might be significantly associated with the outcomes of interest (i.e., tumor features, patient features, etc.). Otherwise, a random-effects model would be used in the study when the results showed p < 0.05. For the main evidence from RCTs, we rated our confidence in the estimates of effect for the outcome as strength of evidence (SOE) as high, moderate, low, or insufficient (15).
Results
Study Selection Process, Search Results, and Characteristics of the Trials
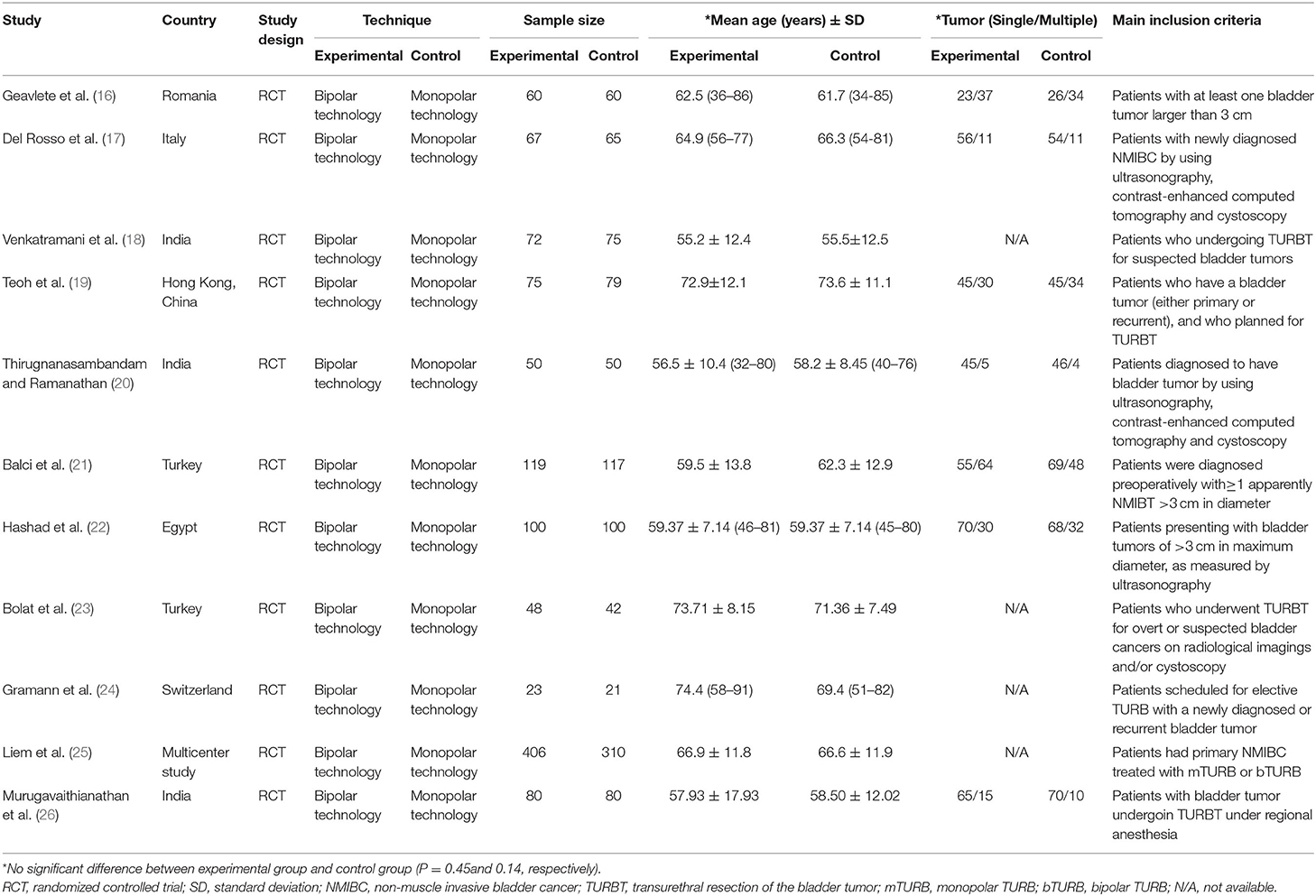
Our search found 211 articles by retrieving three databases. In screening abstracts and titles, 173 articles were excluded. For the remaining 38 articles, 25 articles were excluded due to lack of available data, and two articles were excluded because of the same trial. Finally, 11 articles containing 11 RCTs (16–26) were included to evaluate the outcomes and complications of b-TURB vs. m-TURB. The details of 11 articles are listed in Table 2. Two groups did not show a significant difference in the mean age and the number of bladder tumors. Patients with NMIBC included in each study showed a similar evaluation index.
Risk of Bias
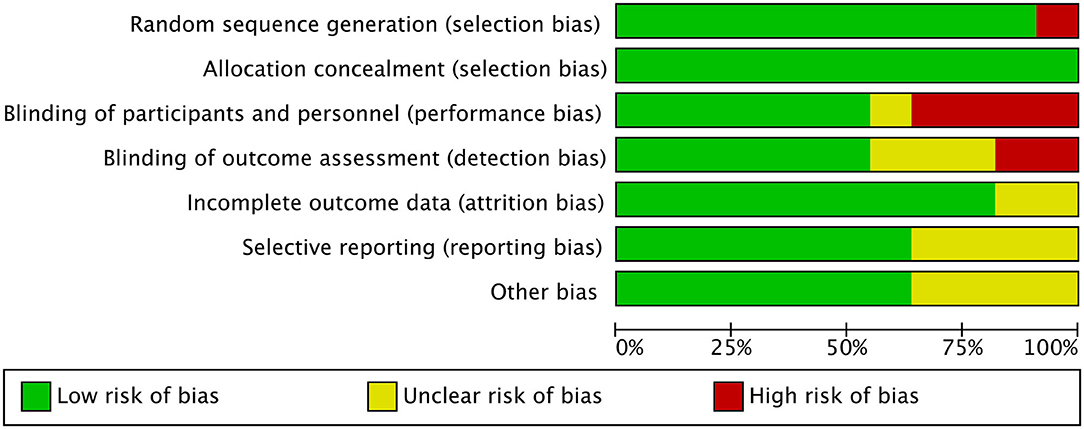
All studies included in the meta-analysis were RCT. The plot showed that 11 circles were contained in the large triangle, and no evidence of bias was found (Figure 2). The risk of bias summary and graph are shown in Figures 3, 4.
Primary Outcomes
Hemoglobin Level
Seven RCTs gathering a total of 1,038 patients contributed to access a decrease in hemoglobin level. The forest plot demonstrated that m-TURB had a greater decrease in postoperative hemoglobin level (MD −0.26, 95% CI −0.48 to −0.04, P = 0.02; Figure 5A) compared with b-TURB. This result suggested that b-TURB was more effective than m-TURB in terms of minimizing bleeding during the procedure.
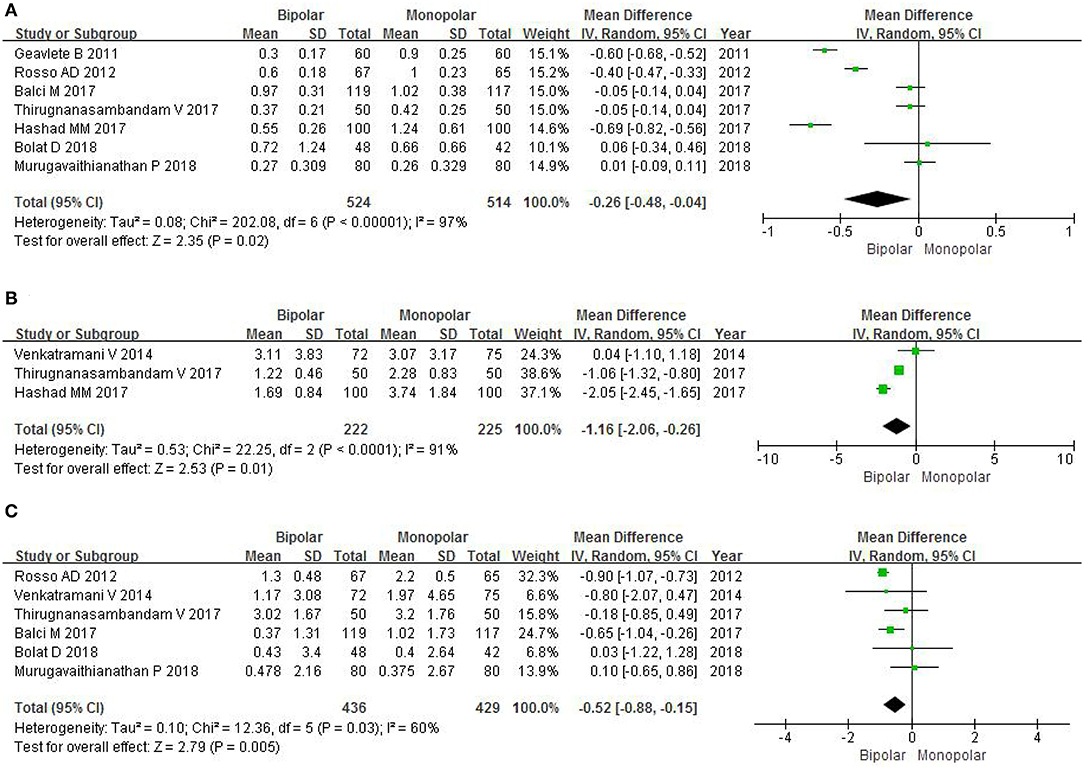
Figure 5. Forest plots showing changes in (A) hemoglobin level; (B) hematocrit level; (C) sodium level. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Hematocrit Level
To evaluate the decrease in hematocrit level, three RCTs had a sample of 447 patients. The random effect estimate of MD was −1.16, and the 95% CI was −2.06 to −0.26 (P = 0.01; Figure 5B). This result indicated that b-TURB was more effective in reducing the amount of bleeding compared with m-TURB.
Sodium Level
Six RCTs with an amount of 865 patients included data on the change of sodium level. The forest plots showed that m-TURB had a significant decrease in postoperative sodium level compared with b-TURB (MD −0.36, 95% CI −0.62 to −0.10, P = 0.007; Figure 5C).
Operation Time
Eleven RCTs enrolling 2,099 patients contained the data of operation time. The forest plots showed an MD of −1.73 and 95% CI of −6.38 to 2.92 (P = 0.47; Figure 6A). We found no statistical significance between b-TURB and m-TURB in the duration of the surgery.
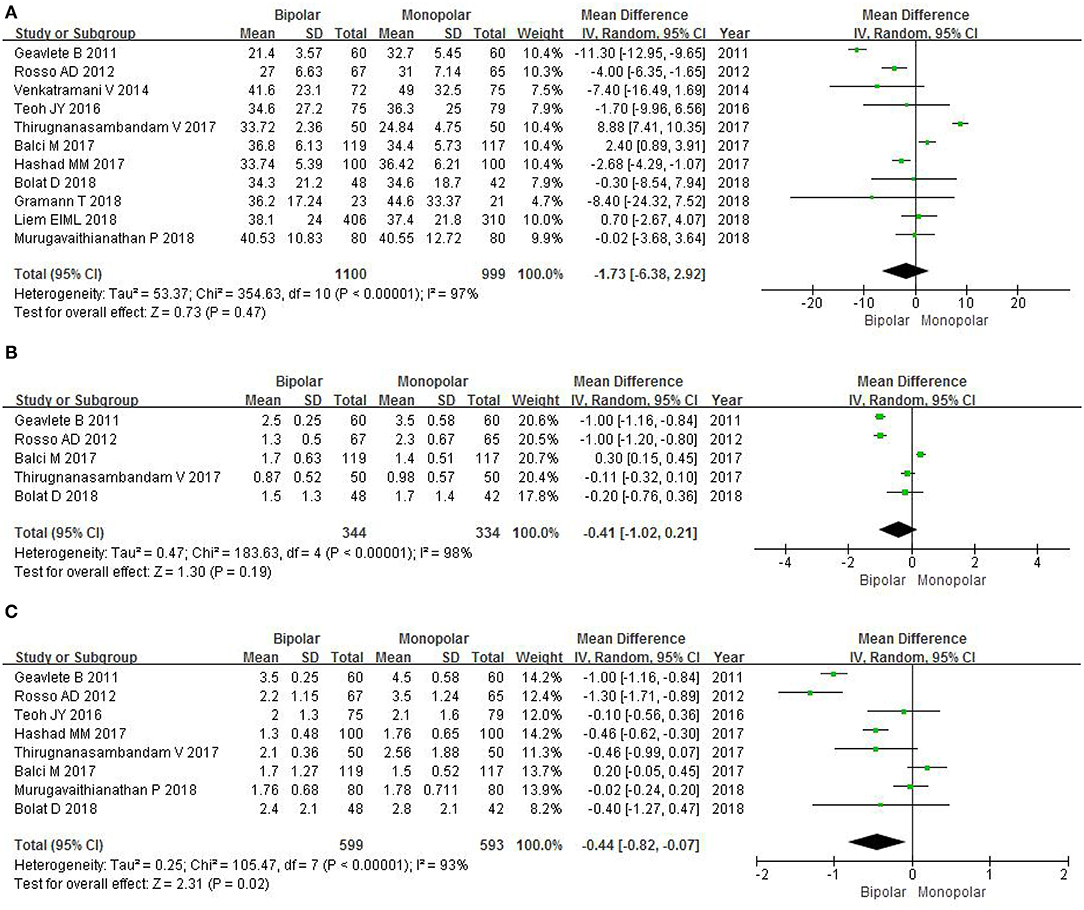
Figure 6. Forest plots showing length in (A) operation time; (B) catheterization time; (C) hospitalization time. SD, standard deviation; IV, inverse variance; CI, confidence interval; df, degrees of freedom.
Catheterization Time
Five RCTs gathering 678 patients included the data of catheterization time. The forest plots did not show a marked difference between b-TURB and m-TURB in the duration of the catheterization (MD −0.41, 95% CI −1.02 to 0.21, P = 0.19; Figure 6B).
Hospitalization Time
Eight RCTs gathering 1,192 patients included the data of hospitalization time. The forest plots showed that b-TURB spent less time in the hospital compared with m-TURB (MD −0.44, 95% CI −0.82 to −0.07, P = 0.02; Figure 6C).
Secondary Outcomes
Obturator Reflex
Eleven RCTs with a sample of 2,099 patients evaluated the severity of obturator reflex. The study showed that there is no statistical significance between b-TURB and m-TURB in the incidence of obturator reflex (OR 0.79, 95% CI 0.60–1.04, P = 0.10; Figure 7A).
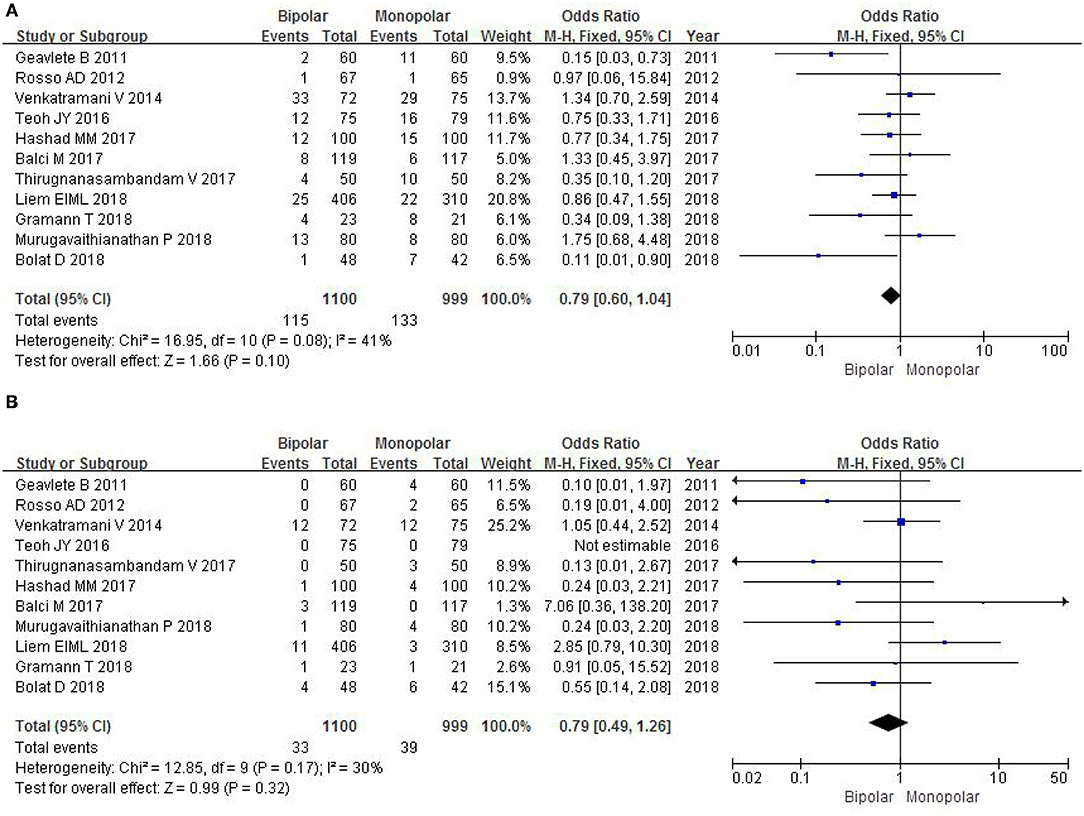
Figure 7. Forest plots showing numbers in (A) obturator reflex; (B) bladder perforation. M-H, Mantel–Haenszel; CI, confidence interval; df, degrees of freedom.
Bladder Perforation
Eleven RCTs accessed the severity of bladder perforation with a sample size of 2,099 patients. The OR was 0.79, and 95% CI was 0.49–1.26 (P = 0.32; Figure 7B). This result suggested that b-TURB did not show a significant difference in the incidence of bladder perforation compared with m-TURB.
Postoperative Blood Transfusion
Eight RCTs with a sample of 1,713 patients analyzed the number of postoperative blood transfusion. A fixed-effects model did not show a statistical significance between b-TURB and m-TURB in the occurrence rate of blood transfusion after operation (OR 0.68, 95% CI 0.33–1.38, P = 0.28; Figure 8A).
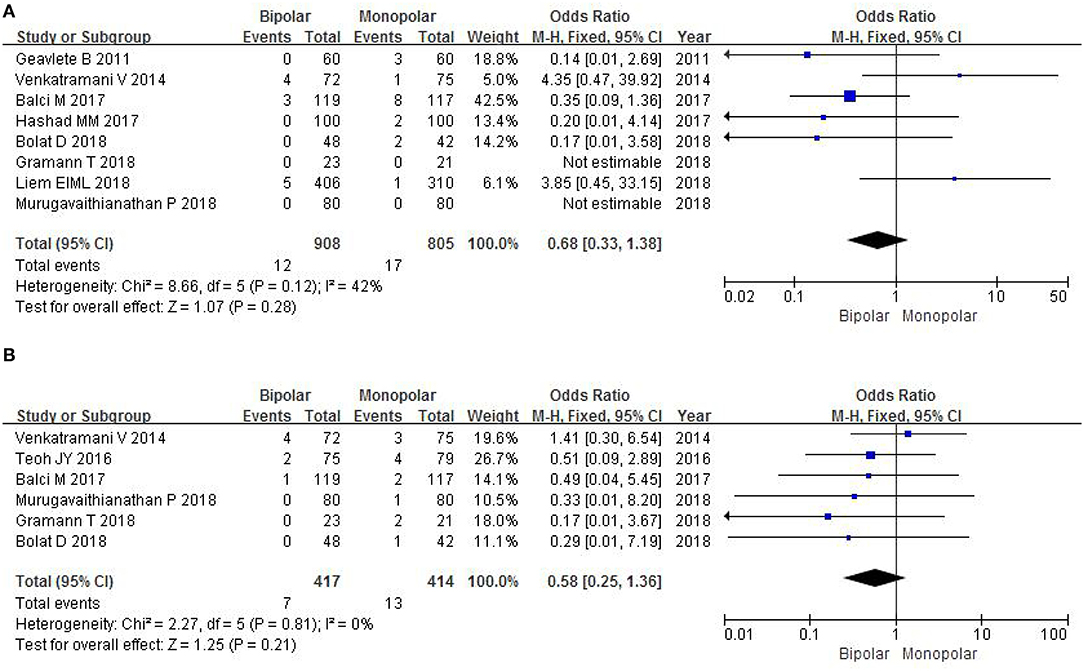
Figure 8. Forest plots showing numbers in (A) postoperative blood transfusion; (B) clot retention. M-H, Mantel–Haenszel; CI, confidence interval; df, degrees of freedom.
Clot Retention
Six RCTs with a sample of 831 patients analyzed the number of clot retention. A fixed-effects model showed that there was not statistical significance between b-TURB and m-TURB in the occurrence rate of clot retention after operation (OR 0.58, 95% CI 0.25–1.36, P = 0.21; Figure 8B).
Muscle Tissue Sampling
Four RCTs evaluated the number of muscle tissue sampling with a sample of 448 patients. The study found that there was no significant difference between b-TURB and m-TURB in muscle tissue sampling rates (OR 1.19, 95% CI 0.77–1.83, P = 0.43; Figure 9A).
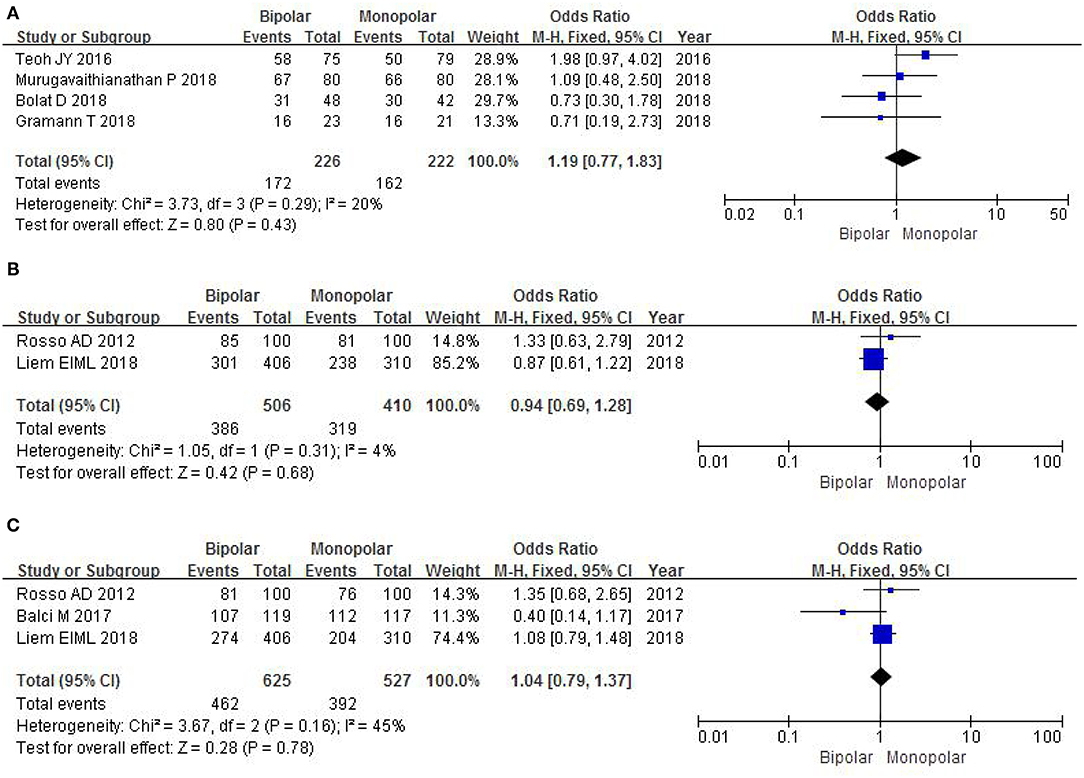
Figure 9. Forest plots showing numbers in (A) muscle tissue sampling; (B) recurrence-free survival at 6 months; (C) recurrence-free survival at 12 months. M-H, Mantel–Haenszel; CI, confidence interval; df, degrees of freedom.
Recurrence-Free Survival at 6 Months
Two RCTs with a sample of 916 patients evaluated postoperative recurrence-free survival at 6 months. The study did not show a significant difference between b-TURB and m-TURB in recurrence-free survival at 6 months (OR 0.94, 95% CI 0.69–1.28, P = 0.68; Figure 9B).
Recurrence-Free Survival at 12 Months
Three RCTs evaluated postoperative recurrence-free survival at 12 months with a sample of 1,152 patients. A fixed-effects model showed that there was no significant difference between b-TURB and m-TURB in recurrence-free survival at 12 months (OR 1.04, 95% CI 0.79–1.37, P = 0.78; Figure 9C).
Grading of Evidence
Evidence overview of primary and secondary outcomes of b-TURB vs. m-TURB is shown in Tables 3, 4. Grading of quality of evidence was downgraded to moderate because it was unclear whether the population undergoing bipolar or monopolar TUR was representative of the whole study population.
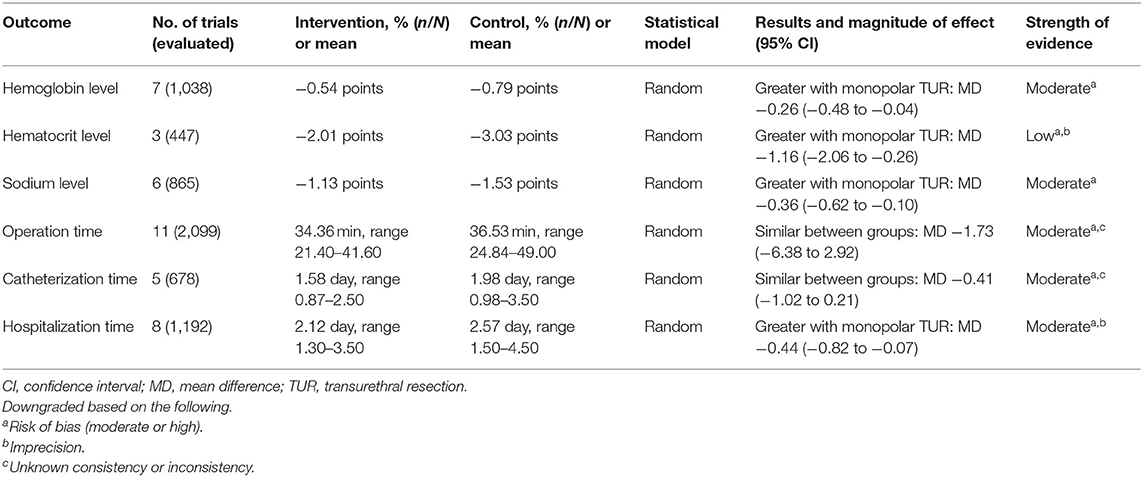
Table 3. Evidence overview of primary outcomes of bipolar vs. monopolar transurethral resection of bladder tumors.
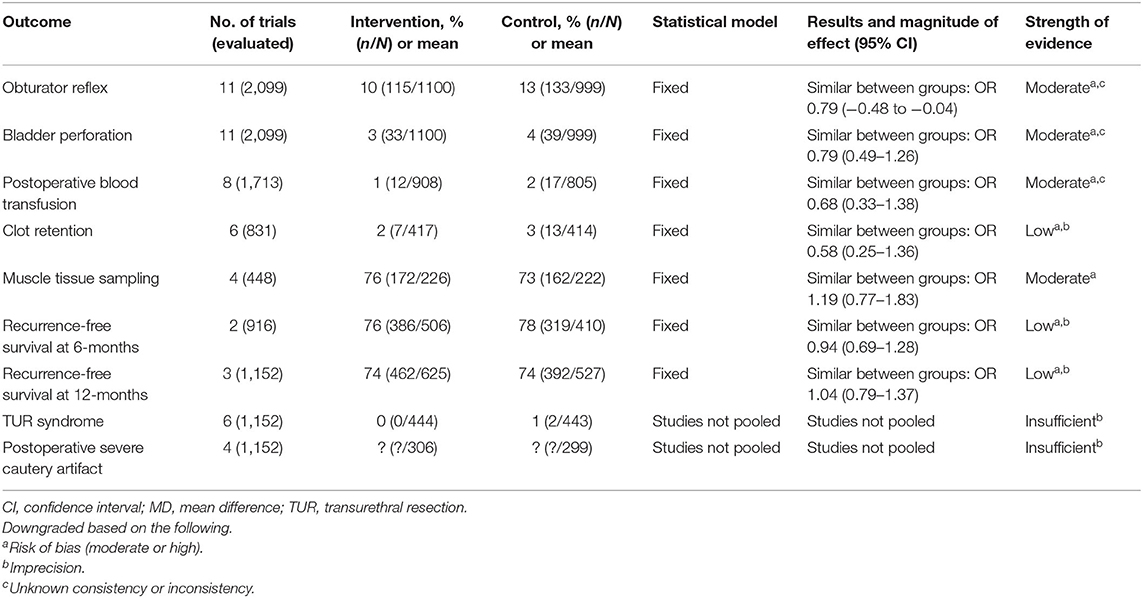
Table 4. Evidence overview of secondary outcomes of bipolar vs. monopolar transurethral resection of bladder tumors.
Discussion
In the past years, m-TURB has still been thought of as a standard surgery for NMIBC, which was frequently associated with the more postoperative complications (27, 28). Bipolar energy, as an alternative to TUR, has developed rapidly in recent years (29). The main superiority of b-TURB is the ability to cut cleanly, reduce tissue burning, and provide clear vision due to the use of saline (8).
This meta-analysis including 11 RCTs with a sample of 2,099 participants aimed to compare bipolar vs. monopolar energy for TURB. The results found that m-TURB had a greater decrease in postoperative hemoglobin level, hematocrit level, and sodium level compared with b-TURB. Besides, patients using b-TURB spent relatively less time in the hospital than those with m-TURB. However, with respect to intraoperative complications, mainly including obturator reflex, bladder perforation, postoperative blood transfusion, and clot retention, there were no significant differences between the two techniques. Meanwhile b-TURB did not show a relative advantage than m-TURB in both intraoperative operation time and postoperative catheterization time.
B-TURB is a novel technology wherein the positive pole and the negative pole are on the same axis and separated from each other through a ceramic connector (30). No reflux current improved hemostasis and minimized blood loss during resection (31). The average coagulation depth of b-TURB is greater than the maximum micro-vessel diameter, and its hemostatic ability may be better than m-TURB (32). B-TURB can coagulate venous bleeding, providing a clearer view of the surgery compared with m-TURB, reducing the time of surgery and the incidence of early complications (32).
M-TURB is flushed with a mannitol solution that may cause TUR syndrome, which is one of the most important complications for patients; in contrast, b-TURB with perfusion of saline during the operational process can avoid the occurrence of TUR syndrome (29, 33). In the analysis, six RCTs (18–21, 23, 26) had a relevant statistic on the number of patients with TUR syndrome after operation. Among them, five RCTs (19–21, 23, 26) did not report the occurrence of this complication, and only one RCT (18) reported two patients with TUR syndrome in the m-TURB group. This result showed that there appears to be no obvious difference between b-TURB and m-TURB in the occurrence rate of TUR syndrome after operation.
In terms of postoperative severe cautery artifact, four RCTs (17, 18, 21, 23) contained some inconsistent statistics about the number of patients, so the present study cannot make a systematic analysis on this point. Venkatramani et al. (18) demonstrated that the percent of severe cautery artifact was significantly lower in the b-TURB than in the m-TURB (25 vs. 46.7%, P = 0.0096). The other three RCTs (17, 21, 23) showed that there was no statistical significance between b-TURB and m-TURB in the number of patients with severe cautery artifact.
For the secondary outcomes, including muscle tissue sampling and recurrence-free survival at 6 and 12 months, the study did not show a significant difference between b-TURB and m-TURB, which indicated that the difference in technique did not affect the depth of tumor cutting and the postoperative recurrence rate of bladder tumors. Del Rosso et al. (17) revealed that the median time until bladder recurrence after initial TUR was 12.4 and 11.9 months for b-TURB and m-TURB, respectively. The 2-year recurrence-free survival rates were, respectively, 67 and 60%, and the Kaplan–Meier curve showed no significant difference (P = 0.70) in the overall recurrence-free survival rate between b-TURB and m-TURB (17). It is noteworthy that the results of the above study may be affected by postoperative management such as early instillation with saline, intravesical chemotherapy, and cystoscopic evaluation (34).
There has been increasing interest in en bloc resection of bladder tumor (ERB) as an ontologically non-inferior alternative to TURB with fewer complications and better histology specimens recently (35). Teoh et al. did a systematic review and meta-analysis for a total of 10 RCTs, which showed that ERB had a shorter irrigation time and a lower rate of bladder perforation than TURB, both with no significant differences in recurrences at 0–12, 13–24, or 25–36 months (36). This study mobilized the international urology community to develop a consensus statement on ERB using transparent and robust methods, and important outcomes for future ERB studies were also identified (36).
Recently, although three new meta-analyses have been published to directly confirm our results, there are many differences in the design and analysis of each study. Among them, two papers lack the analysis of the following indicators: decrease in postoperative hemoglobin level and sodium level, postoperative blood transfusion, clot retention, muscle tissue sampling, and recurrence-free survival at 6 and 12-months (37, 38). In the Tzelves's review, RCTs and observational study were included for qualitative and quantitative synthesis, which will reduce the evidence strength of the study (39). For the main evidence from RCTs, we rated our confidence in the estimates of effect for the outcome as strength of evidence (SOE) as high, moderate, low, or insufficient. Obviously, Xie et al. (38) found that b-TURB has no significant advantages in efficacy and safety in NMIBC treatment compared with that in m-TURB. Thus, b-TURB could not completely replace m-TURB as a safer and more effective NMIBC treatment. However, our study found that the bipolar technique was more effective than the monopolar technique in minimizing intraoperative or postoperative bleeding with relatively small loss of hemoglobin and a shorter hospitalization time for NMIBC. In addition, if there was more than one publication resulting from the same patient cohort, the most recent publication would be used to analyze, and the study may not follow this principle and include studies from the same population.
Although those articles included in the study were all randomized controlled trials to reinforce the findings, we must acknowledge the limitations of this meta-analysis. Selection bias, subjective factors, and publication bias may also affect the final results of our study. One limitation of our findings is some variables, such as local culture, the skill and experience of the operating surgeon, efficacy of perioperative care, and tumor size and number. We note also that the quality of some studies is flawed, primarily in terms of study design, patient selection, blinding, and outcome data. Therefore, the results of a meta-analysis should be interpreted carefully.
Conclusion
The b-TURB was more effective than m-TURB in minimizing bleeding with relatively small loss of hemoglobin and a shorter hospitalization time. For operation time and catheterization time, both techniques did not show statistical significance. B-TURB did not show significant differences in the incidence rate of obturator reflex, bladder perforation, postoperative blood transfusion, and clot retention compared with m-TURB. Besides, there were no significant differences in terms of muscle tissue sampling, and recurrence-free survival at 6 and 12 months.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
MY and YZ conceptualized and designed the study and provided administrative support. XM, ZZ, and YC collected, assembled, analyzed, and interpreted the data. All authors provided the study materials or patients, and wrote and gave the final approval of the manuscript.
Funding
This work was supported by the National Nature Science Foundation of China, Code: 81801429, Beijing Municipal Administration of Hospitals' Ascent Plan, Code: DFL20190502, and Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support, Code: ZYLX201820.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. American Cancer Society. Key Statistics for Bladder Cancer. (2019). Retrieved from: http://www.cancer.org/cancer/bladdercancer/detailedguide/bladder-cancer-key-statistic (accessed February 02, 2021).
2. Burger M, Catto JW, Dalbagni G, Grossman HB, Herr H, Karakiewicz P, et al. Epidemiology and risk factors of urothelial bladder cancer. Eur Urol. (2013) 63:234–41. doi: 10.1016/j.eururo.2012.07.033
3. Kamat AM, Hegarty PK, Gee JR, Clark PE, Svatek RS, Hegarty N, et al. ICUD-EAU International Consultation on Bladder Cancer 2012: screening, diagnosis, and molecular markers. Eur Urol. (2013) 63:4–15. doi: 10.1016/j.eururo.2012.09.057
4. Antoni S, Ferlay J, Soerjomataram I, Znaor A, Jemal A, Bray F. Bladder cancer incidence and mortality: a global overview and recent trends. Eur Urol. (2016) 71:96–108. doi: 10.1016/j.eururo.2016.06.010
5. Chang SS, Boorjian SA, Chou R, Clark PE, Daneshmand S, Konety BR, et al. Diagnosis and treatment of non-muscle invasive bladder cancer: AUA/SUO guideline. J Urol. (2016) 196:1021–9. doi: 10.1016/j.juro.2016.06.049
6. Herr HW, Donat SM. Quality control in transurethral resection of bladder tumours. BJU Int. (2008) 102:1242–46. doi: 10.1111/j.1464-410X.2008.07966.x
7. Burke N, Whelan JP, Goeree L, Hopkins RB, Campbell K, Goeree R, et al. Systematic review and meta-analysis of transurethral resection of the prostate versus minimally invasive procedures for the treatment of benign prostatic obstruction. Urology. (2010) 75:1015–22. doi: 10.1016/j.urology.2009.08.015
8. Puppo P, Bertolotto F, Introini C, Germinale F, Timossi L, Naselli A. Bipolar transurethral resection in saline (TURis): outcome and complication rates after the first 1000 cases. J Endourol. (2009) 23:1145–9. doi: 10.1089/end.2009.0011
9. Rose A, Suttor S, Goebell PJ, Rossi R, Rübben H. Transurethral resection of bladder tumors and prostate enlargement in physiological saline solution (TURIS). A prospective study. Urologe A. (2017) 46:1148–50. doi: 10.1007/s00120-007-1391-9
10. Cui Y, Chen H, Liu L, Chen J, Qi L, Zu X. Comparing the efficiency and safety of bipolar and monopolar transurethral resection for non-muscle invasive bladder tumors: a systematic review and meta-analysis. J Laparoendosc Adv Surg Tech A. (2016) 26:196–202. doi: 10.1089/lap.2015.0507
11. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. (2009) 62:1006–12. doi: 10.1016/j.jclinepi.2009.06.005
13. Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.3.0. The Cochrane Collaboration (2011). Available online at: www.cochrane-handbookorg (accessed December 10, 2018).
15. Berkman ND, Lohr KN, Ansari M, McDonagh M, Balk E, Whitlock E, et al. Grading the Strength of a Body of Evidence When Assessing Health Care Interventions for the Effective Health Care Program of the Agency for Healthcare Research and Quality: An Update. AHRQ Publication No. 13(14)-EHC130-EF. Rockville, MD: Agency for Healthcare Research and Quality (2013). Available online at: www.effectivehealthcare.ahrq.gov/reports/final.cfm (accessed February 02, 2021).
16. Geavlete B, Multescu R, Georgescu D, Jecu M, Dragutescu M, Geavlete P. Innovative technique in nonmuscle invasive bladder cancer-bipolar plasma vaporization. Urology. (2011) 77:849–54. doi: 10.1016/j.urology.2010.08.062
17. Del Rosso A, Pace G, Masciovecchio S, Saldutto P, Galatioto GP, Vicentini C. Plasmakinetic bipolar versus monopolar transurethral resection of non-muscle invasive bladder cancer: a single center randomized controlled trial. Int J Urol. (2013) 20:399–403. doi: 10.1111/j.1442-2042.2012.03174.x
18. Venkatramani V, Panda A, Manojkumar R, Kekre NS. Monopolar versus bipolar transurethral resection of bladder tumors: a single center, parallel arm, randomized, controlled trial. J Urol. (2014) 191:1703–7. doi: 10.1016/j.juro.2013.12.004
19. Teoh JY, Chan ES, Yip SY, Tam HM, Chiu PK, Yee CH, et al. Comparison of detrusor muscle sampling rate in monopolar and bipolar transurethral resection of bladder tumor: a randomized trial. Ann Surg Oncol. (2017) 24:1428–434. doi: 10.1245/s10434-016-5700-7
20. Thirugnanasambandam V, Ramanathan J. Safety and efficacy of bipolar energy for transurethral resection of bladder tumours: a prospective quasi-randomized study. Turk J Urol. (2017) 43:141–6. doi: 10.5152/tud.2017.33396
21. Balci M, Tuncel A, Keten T, Guzel O, Lokman U, Koseoglu E, et al. Comparison of monopolar and bipolar transurethral resection of non-muscle invasive bladder cancer. Urol Int. (2018) 100:100–4. doi: 10.1159/000467397
22. Hashad MM, Abdeldaeim HM, Moussa A, Assem A, Youssif TMA. Bipolar vs. monopolar resection of bladder tumours of >3 cm in patients maintained on low-dose aspirin: a randomised clinical trial. Arab J Urol. (2017) 15:223–7. doi: 10.1016/j.aju.2017.04.001
23. Bolat D, Gunlusoy B, Aydogdu O, Aydin ME, Dincel C. Comparing the short - term outcomes and complications of monopolar and bipolar transurethral resection of bladder tumors in patients with coronary artery disease: a prospective, randomized, controlled study. Int Braz J Urol. (2018) 44:717–25. doi: 10.1590/S1677-5538
24. Gramann T, Schwab C, Zumstein V, Betschart P, Meier M, Schmid HP, et al. Transurethral resection of bladder cancer on the lateral bladder wall without obturator nerve block: extent of adductor spasms using the monopolar versus bipolar technique-a prospective randomised study. World J Urol. (2018) 36:1085–91. doi: 10.1007/s00345-018-2248-0
25. Liem EIML, McCormack M, Chan ESY, Matsui Y, Geavlete P, Choi YD, et al. Monopolar vs. bipolar transurethral resection for non-muscle invasive bladder carcinoma: A post-hoc analysis from a randomized controlled trial. Urol Oncol. (2018) 36:338.e1–e11. doi: 10.1016/j.urolonc.2018.03.015
26. Murugavaithianathan P, Devana SK, Mavuduru R, Kumar S, Singh SK, Mandal AK, et al. Bipolar transurethral resection of bladder tumor provides better tissue for histopathology but has no superior efficacy and safety: a randomized controlled trial. J Endourol. (2018) 32:1125–30. doi: 10.1089/end.2017.0328
27. Traxer O, Pasqui F, Gattegno B, Pearle MS. Technique and complications of transurethral surgery for bladder tumours. BJU Int. (2004) 94:492–6. doi: 10.1111/j.1464-410X.2004.04990.x
28. Brunken C, Qiu H, Tauber R. Transurethrale Resektion von Blasentumoren in Kochsalzlösung. Urologe A. (2004) 43:1101–5. doi: 10.1007/s00120-004-0653-z
29. Wang DS, Bird VG, Leonard VY, Plumb SJ, Konety B, Williams RD, et al. Use of bipolar energy for transurethral resection of bladder tumors: pathologic considerations. J Endourol. (2004) 18:578–82. doi: 10.1089/end.2004.18.578
30. Dincel C, Samli MM, Guler C, Demirbas M, Karalar M. Plasma kinetic vaporization of the prostate: clinical evaluation of a new technique. J Endourol. (2004) 18:293–8. doi: 10.1089/089277904773582921
31. de Sio M, Autorino R, Quarto G, Damiano R, Perdonà S, di Lorenzo G, et al. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial. Urology. (2006) 67:69–72. doi: 10.1016/j.urology.2005.07.033
32. Huang X, Wang XH, Wang HP, Qu LJ. Comparison of the microvessel diameter of hyperplastic prostate and the coagulation depth achieved with mono and bipolar transurethral resection of the prostate. A pilot study on hemostatic capability. Scand J Urol Nephrol. (2008) 42:265–8. doi: 10.1080/00365590701702168
33. Moorthy H K, Philip S. TURP syndrome-current concepts in the pathophysiology and management. Indian J Urol. (2001) 17:97–102.
34. Zhou Z, Zhao S, Lu Y, Wu J, Li Y, Gao Z, et al. Meta-analysis of efficacy and safety of continuous saline bladder irrigation compared with intravesical chemotherapy after transurethral resection of bladder tumors. World J Urol. (2019) 37:1075–84. doi: 10.1007/s00345-019-02628-7
35. Kitamura K, Kataoka K, Fujioka H, Kashiwai K. Transurethral resection of a bladder tumor by the use of a polypectomy snare. J Urol. (1980) 124:808–9.
36. Teoh JY, MacLennan S, Chan VW, Miki J, Lee HY, Chiong E, et al. An international collaborative consensus statement on en bloc resection of bladder tumour incorporating two systematic reviews, a two-round Delphi survey, and a consensus meeting. Eur Urol. (2020) 78:546–69. doi: 10.1016/j.eururo.2020.04.059
37. Sharma G, Sharma AP, Mavuduru RS, Bora GS, Devana SK, Singh SK, et al. Safety and efficacy of bipolar versus monopolar transurethral resection of bladder tumor: a systematic review and meta-analysis. World J Urol. (2021) 39:377–87. doi: 10.1007/s00345-020-03201-3
38. Xie K, Cao D, Wei Q, Ren Z, Li J, Li Y, et al. Bipolar versus monopolar transurethral resection of non-muscle-invasive bladder cancer: a systematic review and meta-analysis of randomized controlled trials. World J Urol. (2021) 39:1177–86. doi: 10.1007/s00345-020-03271-3
Keywords: monopolar and bipolar, transurethral resection, bladder cancer, randomized controlled trials, systematic review and meta-analysis, complications
Citation: Mao X, Zhou Z, Cui Y, Zhang Y and Yang M (2021) Outcomes and Complications of Bipolar vs. Monopolar Energy for Transurethral Resection of Bladder Tumors: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Surg. 8:583806. doi: 10.3389/fsurg.2021.583806
Received: 16 July 2020; Accepted: 20 April 2021;
Published: 02 June 2021.
Edited by:
Jeremy Teoh, The Chinese University of Hong Kong, ChinaReviewed by:
Riccardo Campi, Careggi Hospital, ItalyBogdan Geavlete, St. John Hospital Emergency Clinic, Romania
Copyright © 2021 Mao, Zhou, Cui, Zhang and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingshan Yang, bTE1Mjc1NTI1MzE2QDE2My5jb20=
†These authors have contributed equally to this work
 Xin Mao1†
Xin Mao1† Zhongbao Zhou
Zhongbao Zhou Yong Zhang
Yong Zhang