
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg. , 13 August 2018
Sec. Visceral Surgery
Volume 5 - 2018 | https://doi.org/10.3389/fsurg.2018.00047
Introduction: There continues to be very little agreement among experts on the precise treatment strategy for incisional hernias. That is the conclusion drawn from the very limited scientific evidence available on the repair of incisional hernias. The present review now aims to critically assess the data available on the sublay/retro-rectus technique for repair of incisional hernia.
Materials and Methods: A systematic search of the literature was performed in May 2018 using Medline, PubMed, and the Cochrane Library. This article is based on 77 publications.
Results: The number of available RCTs that permit evaluation of the role of the sublay/retro-rectus technique in the repair of only incisional hernia is very small. The existing data suggest that the sublay/retro-rectus technique has disadvantages compared with the laparoscopic IPOM technique for repair of incisional hernia, but in that respect has advantages over all other open techniques. However, the few existing studies provide only a limited level of evidence for assessment purposes.
Conclusion: Further RCTs based on a standardized technique are urgently needed for evaluation of the role of the sublay/retro-rectus incisional hernia repair technique.
Numerous guidelines, meta-analyses and systematic reviews explore the best possible surgical treatment for ventral and incisional hernias (1–26). Nonetheless, there is very little agreement among experts on the precise treatment strategy (27). The reasons for that are no doubt manifold. One systematic review of the prospective randomized studies and reviews in the treatment of ventral and incisional hernias found only a limited evidence base for determining the best treatment options for patients despite the large number of patients with ventral and incisional hernias and the high frequency of repair (28). Another analysis of the literature on elective surgery of ventral and incisional hernias identified inconsistencies in reporting of peri- and postoperative variables and poor definition of variables (29). A further problem is the pooling of primary ventral hernias and incisional hernias in many studies, meta-analyses and systematic reviews (30–33). Several studies have demonstrated that there is a significant difference between the outcomes for primary abdominal wall hernias and incisional hernias, hence these hernia entities should not be pooled (30–33). Against that background the present review aims to identify which data are available on the sublay/retro-rectus operation to demonstrate that this is the best open technique for repair of only incisional hernia. In terms of nomenclature the terms “sublay” and “retro-rectus” are intended as equivalent designations (34).
A systematic search of the available literature was performed in June 2018 using Medline, PubMed, and the Cochrane Library, as well as a search of relevant journals and reference lists. The following search terms were used: “Sublay,” “Retro-rectus,” “Incisional hernia,” “Sublay technique,” “Rives-Stoppa technique,” “Rives-Stoppa-Wantz technique,” “Retro-rectus mesh,” “Retromuscular mesh,” Retro muscular prefascial mesh,” “Sublay and ventral hernia,” “Sublay and incisional hernia.” The abstracts of 260 publications were checked. For the present analysis 77 publications were identified as relevant to the key question (Figure 1).
Numerous meta-analyses and systematic reviews pool primary ventral hernias and incisional hernias in their comparative evaluation of various surgical techniques (7–17). Therefore, the power of these meta-analyses and systematic reviews to answer the key question raised here is limited and they do not permit any binding statements to be made on the role of the sublay/retro-rectus technique in the repair of incisional hernia (7–17). There remain seven meta-analyses and systematic reviews that compared the outcomes of different surgical techniques for incisional hernia alone (18–26).
The same problems apply to randomized controlled trials (RCTs) that serve as the basis for the meta-analyses and systematic reviews (35–48). The 14 publications report on the findings of 11 RCTs since the results of a number of studies have been reported in several publications (35, 36, 43, 44, 46, 47). Only three RCTs (38, 45–47) were deemed suitable for answering the key question to be addressed here because the remaining studies had included a mixed patient group with primary ventral and incisional hernias (40, 43, 44), did not exclusively use the sublay/retro-rectus technique (41) or used a technique other than the sublay/retro-rectus technique (35–37, 39, 42, 48). Hence, there remains only a limited number of RCTs for evaluation of the role of the sublay/retro-rectus technique for the repair of incisional hernia. That naturally also detracts from the power of the remaining and relevant meta-analyses and systematic reviews. Below the open sublay/retro-rectus technique is compared first with the laparoscopic intraperitoneal onlay mesh (IPOM) technique, followed by comparison with the other open techniques for repair of incisional hernia, and is then evaluated. Due to the paucity of relevant RCTSs, the findings of comparative observational studies are also included in this review.
The meta-analysis of RCTs by Chalabi (24) included five studies (37, 40, 41, 45–47). The authors came to the conclusion that the short- and long-term outcomes of laparoscopic and open abdominal wall hernia repairs are equivalent: both techniques are safe and credible and the outcomes are very comparable (24). One aspect of this meta-analysis that must be criticized is that it contained one RCT with ventral hernia repair (40) and two RCTs with open surgical techniques other than the sublay/retro-rectus technique (37, 41). Hence the power of that meta-analysis must be greatly put into perspective.
Another meta-analysis that compared laparoscopic IPOM vs. open repair of incisional hernias by Awaiz (21–23) concluded after making an amendment that a statistically significant reduction in wound complications was noted with laparoscopic surgery compared to the open repair based on six studies (37–39, 41, 45, 46). Here, too, it must be pointed out that only in three RCTs was the open comparison group based on the sublay/retro-rectus technique (38, 45, 46).
Likewise, the last published meta-analysis of comparison of the laparoscopic vs. open repair by Dietz (26), which included only three (38, 45, 46) of nine RCTs with sublay/retro-rectus technique as open technique, identified comparative reoperation, complication and recurrence rates (26). Here only a total of 170 laparoscopic IPOM operations were compared with 181 open sublay/retro-rectus repairs.
Table 1 features the results of RCTs comparing the laparoscopic IPOM with only the open sublay/retro-rectus technique. This does not give a clear picture. One RCT showed a highly significant difference in the surgical site infection rate to the advantage of the laparoscopic IPOM (46), whereas the other two RCTs reported more postoperative complications for the laparoscopic IPOM (38, 45). No significant differences were discerned in the recurrence rates or the hospital stay (45, 46).
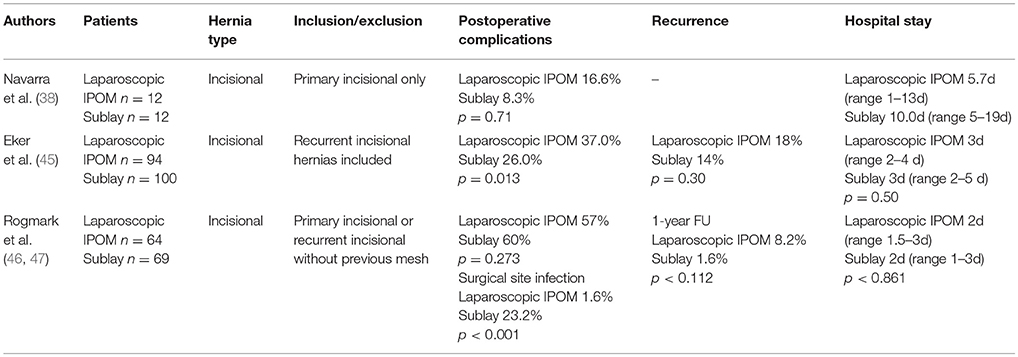
Table 1. Results of RCTs comparing laparoscopic IPOM vs. open sublay/retro-rectus technique in incisional hernia repair.
Hence, based on the available meta-analyses, systematic reviews and RCTs it is not possible to make any clear statement about which surgical technique has advantages when comparing laparoscopic IPOM vs. open sublay/retro-rectus repair. Therefore, the findings of comparative observational studies are included additionally in this review when seeking to answer the key question.
In a registry-based, propensity score-matched comparison of laparoscopic IPOM and sublay/retro-rectus incisional hernia repairs, 3,965 matched pairs were created and compared. The comparison revealed disadvantages for the open sublay/retro-rectus technique regarding postoperative surgical complications, complication-related reoperations and postoperative general complications. The majority of surgical postoperative complications were surgical site occurrences. Laparoscopic IPOM had disadvantages in terms of intraoperative complications, mainly bleeding and bowel injuries. No significant differences were observed in the recurrence and pain rates at 1-year follow-up (Köckerling et al., in review).
One meta-analysis of comparison of suture vs. mesh repair by Mathes (14) included only two RCTs for incisional hernias and sublay/retro-rectus repair (35, 36, 42), with one RCT reporting different follow-up intervals (35, 36). The results are summarized in Table 2. The publications included in the RCTs showed a significantly lower recurrence rate following sublay/retro-rectus mesh repair compared with suture repair of incisional hernias.
The meta-analysis by Timmermans (25) compared the sublay /retro-rectus with the onlay technique only for incisional hernias. For that meta-analysis only two RCTs (42, 44) were identified, with one RCT also featuring primary abdominal wall hernias (44). The other studies were one prospective (49) and seven retrospective comparative studies (50–56). The meta-analysis then compared 775 onlay operations with 1,173 sublay/retro-rectus operations (25). A trend was observed for incisional hernia recurrence in favor of the sublay repair (OR 2.41; 95% CI [0.99–5.88] p = 0.05) (25). Surgical site infection occurred significantly less often after sublay/retro-rectus repair (OR = 2.42; 95% CI [1.02–5.74]; p = 0.05) (25). The results of the meta-analysis were also confirmed by the three RCTs available in the meantime comparing sublay/retro-rectus vs. onlay incisional hernia repair (42, 57, 58) (Table 3). Here, too, significantly more wound complications as well as a trend toward higher recurrence rates were identified for onlay repair of incisional hernias.
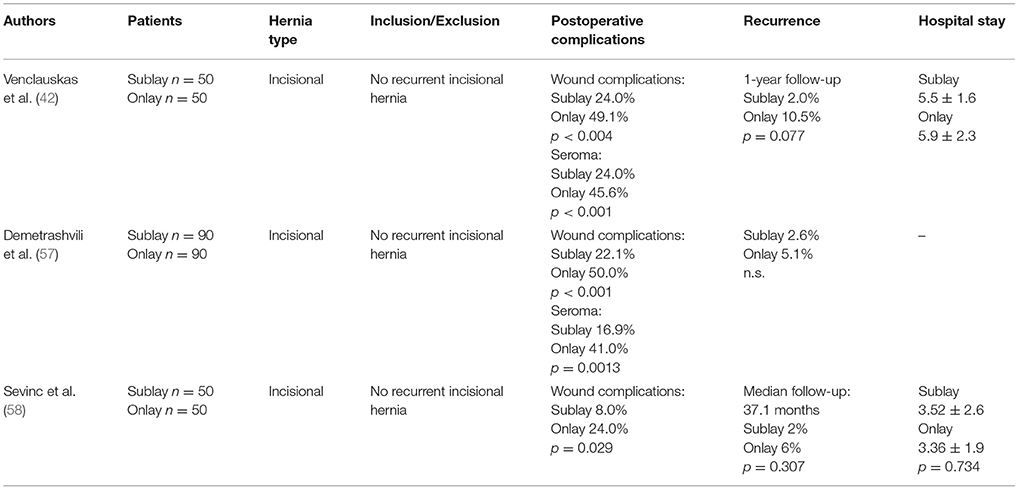
Table 3. RCTs comparing sublay/retro-rectus vs. onlay mesh repair technique in incisional hernia repair.
In a nationwide prospective study of the Danish Hernia Database of outcomes after elective incisional hernia repair, the sublay/retro-rectus mesh position resulted in a significantly lower risk for recurrence operations (cumulative risk 12.1%) compared with onlay mesh position (16.1%) and intraperitoneal mesh position (21.2%) (p = 0.03) (59).
No RCTs are available for comparison of the open IPOM technique/underlay technique vs. the open sublay/retro-rectus technique. The existing meta-analyses also include primary ventral hernias (15–17). Besides, one RCT for that comparison is not available. Therefore, recourse had to be had to comparative observational studies.
It has already been pointed out above that in the Danish registry study the recurrence rate at 21.2% was markedly higher for the open intraperitoneal onlay mesh technique or underlay technique compared with the sublay/retro-rectus technique (59).
The most important technical steps of sublay/retro-rectus repair of incisional hernias are as follows (60–65):
a. Excision of scar and partial hernia sac, adhesiolysis (60–65)
For avoidance of wound complications the thinned out portion of skin with the part of the hernia scar remaining in this area and the scar are elliptically excised. Excision of the umbilicus is also recommended. Further dissection between the skin/subcutaneous tissue and myofascial abdominal wall should be avoided. The remaining parts of the scarred hernia sac margins should be preserved and are later included in the suture of the anterior rectus sheath. Via the opened hernia sac adhesiolysis of intestinal loops and parts of the greater omentum is then carried out.
b. Incision of the posterior rectus sheath and creation of the retromuscular, prefascial space (60–65)
The position of the mesh in the space between the rectus abdominis muscle and the posterior rectus sheath requires opening of the rectus sheath. The posterior rectus sheath is opened near the linea alba to enter the retromuscular space and expose the posterior aspect of the rectus muscle (Figure 2). The space is developed using a combination of blunt and sharp dissection (Figure 3). The lateral extent of this dissection is the linea semilunaris, the junction between the posterior and anterior rectus sheaths. Careful identification and preservation of the intercostal nerves and vessels is critical to maintaining an innervated functional abdominal wall (Figure 4). The retromuscular plane can be extended cephalad to the retroxiphoid and retrosternal areas (Figures 5, 6). Inferiorly, the space of Retzius is entered to expose the pubis symphysis and both Cooper's ligaments (Figure 7). Since this area is below the arcuate line, posterior layer includes peritoneum and transversalis fascia only (Figure 7).
c. Closure of the posterior rectus sheath (60–65)
In most cases, suture of the posterior rectus sheath's margins can be achieved when correctly and widely freed (Figures 8–10). When closure of the posterior rectus sheath is not possible, the remaining defect can be closed by a slowly absorbable mesh (Figure 11).
d. Placement of the mesh and fixation (60–65)
The upper part of the mesh is placed between the rectus abdominis muscle, the ribs and xiphoid process and the reconstructed posterior rectus sheath. The lower part of the mesh is fixed to Cooper's ligament. Centrally, the mesh is placed on the retromuscular space limited by the linea semilunaris (Figure 12). The mesh can be fixed circumferentially with full-thickness, transabdominal sutures using a Reverdin needle or by single sutures to the posterior rectus sheath. Finally, the linea alba is reconstructed by suturing together the anterior rectus shealt, hernia scar and the remaining hernia sac over the mesh (Figure 13).
e. Comparison of lightweight vs. standard mesh in sublay/retro-rectus repair of incisional hernias
One meta-analysis (66) compared the results of the sublay/retro-rectus repair of incisional hernias based on a single RCT (67), three prospective (68–70) and one retrospective (71) study. The authors concluded that the use of lightweight mesh in open sublay/retro-rectus repair seems to be associated with less chronic pain, and with no increase in recurrence or in other postoperative complications (66).
Another RCT compared for incisional hernias the sublay/retro-rectus technique with a lightweight polypropylene mesh and a partially absorbable polypropylene mesh (72). With a total of 80 randomized patients no significant difference was observed between these two groups (72).
f. Comparison of self-adhering meshes with suture fixation in sublay/retro-rectus incisional hernia repair
In a comparative study 12 patients with transfacially sutured mesh and 14 patients with self-adhering mesh in sublay/retro-rectus incisional hernia repair were followed up for at least 12 months. The results show low rates of surgical site occurrences, recurrences and significantly less acute pain with self-adhering mesh (73).
In a prospective comparative study with 50 patients comparing self-adhering, with suture fixed, meshes in sublay/retro-rectus incisional hernia repair, postoperative pain in the first 48 h was less in the self-adhering mesh group (74).
g. Comparison of fibrin glue vs. transfascial suture mesh fixation
In a comparative study of open abdominal wall reconstruction with retromuscular mesh fixation using fibrin glue vs. transfascial sutures the probability of reporting pain at 6-month follow-up was significantly higher in the transfascial suture group (OR 12.29, 95% CI [1,26–120.35]; p = 0.031) (75). No hernia recurrences were noted in either group with a mean follow-up of 390 ± 330 days (75).
h. Comparison of drain vs. no drain placement
In a registry-based comparison of drain placement vs. no drain placement of the retromuscular ventral hernia repair surgical drains do not increase the risk of surgical infection complications and may be protective against some surgical site occurrences, such as seroma formation (76).
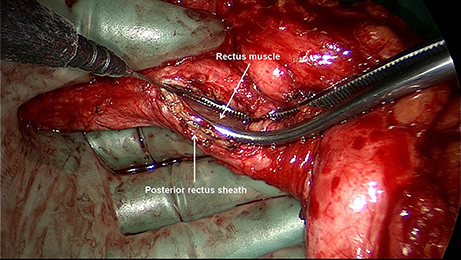
Figure 2. The posterior rectus sheath is opened near the linea alba and the posterior aspect of the rectus muscle exposed.
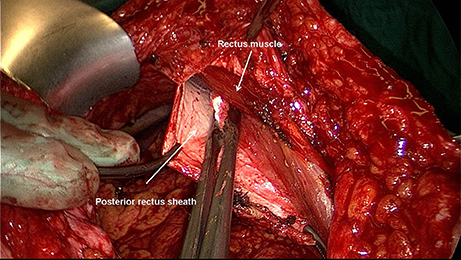
Figure 3. The space between the posterior rectus sheath and the rectus muscle is developed using a combination of blunt and sharp dissection.
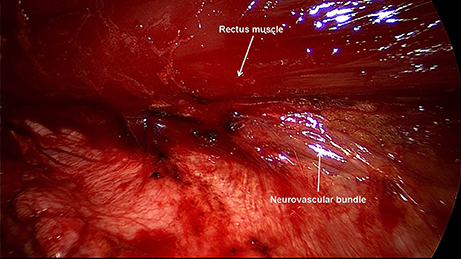
Figure 4. Careful identification and preservation of the intercostal nerves and vessels are critical.
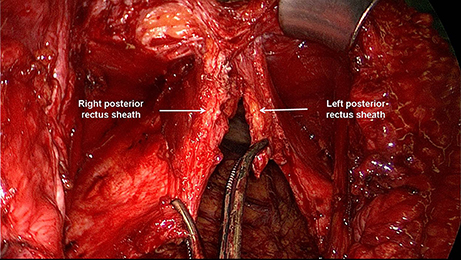
Figure 5. The retromuscular plane can be extended cephalad to the retroxiphoid and retrosternal areas. Typical finding before transection of the right and left posterior rectus sheath.
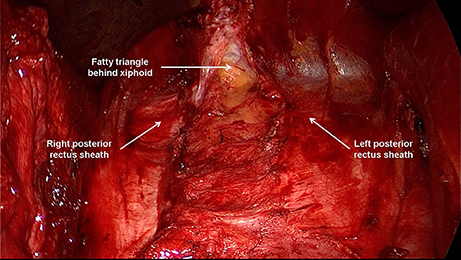
Figure 6. Typical finding after transection of the right and left posterior rectus sheaths and opening of the space between fatty triangle and xiphoid.
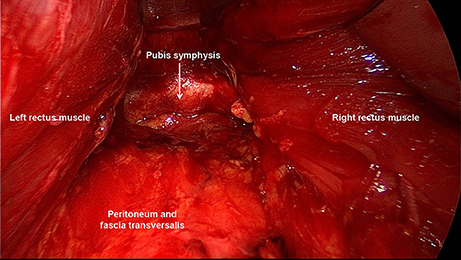
Figure 7. Inferiorly, the space of Retzius is entered to expose the pubis symphysis. Below the arcuate line, the posterior layer only includes peritoneum and transversalis fascia.
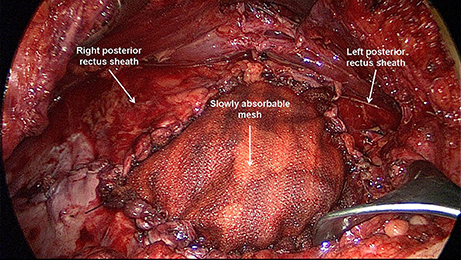
Figure 11. Closure of a remaining defect in the posterior rectus sheath by a slowly absorbable mesh (Phasix ST).
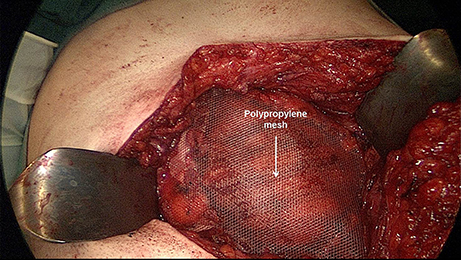
Figure 12. The non-absorbable mesh (TiMesh strong) is placed between the rectus abdominis muscle, the ribs and xiphoid process and the reconstructed posterior rectus sheath.
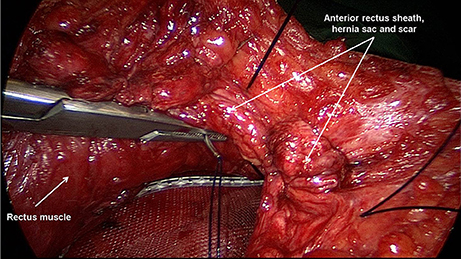
Figure 13. Reconstruction of the linea alba by suturing together the anterior rectus sheath, hernia scar and the remaining hernia sac over the mesh.
There are considerable limitations when engaging in critical analysis of the literature available for evaluation of the sublay/retro-rectus technique for repair of incisional hernia. Several meta-analyses, systematic reviews and RCTs report on a pooled patient group with primary (umbilical hernias, epigastric hernias) and secondary (incisional hernias) abdominal wall hernias (7–17, 40, 43, 44) despite the fact that there are significant differences in the outcomes of primary and secondary abdominal wall hernias (30–33). Hence, these findings are only of limited value. Furthermore, the open incisional hernia repair group also included other techniques in addition to the sublay/retro-rectus technique (35–39, 41, 42, 48). As such, only a very limited number of studies are available for evaluation of the sublay/retro-rectus technique in repair of incisional hernia.
When comparing open sublay/retro-rectus repairs of incisional hernias it is not possible to base a reliable evaluation of these operations on the existing meta-analyses, systematic reviews or RCTs because of the contradictory nature of the data (38, 45, 46). Only one registry-based, prospective observational study with a relatively large case number demonstrated clear advantages for the laparoscopic IPOM in the early postoperative course thanks to a significantly low postoperative complication rate, in particular in respect of the surgical site occurrences, complication-related reoperations and the general postoperative complications. Disadvantages of laparoscopic IPOM related to intraoperative complications. No differences were identified in the pain and recurrence rates at 1-year follow-up (Köckerling et al., in review).
However, the open sublay/retro-rectus technique has been found to have advantages over the other incisional hernia open repair techniques (14, 25, 58). In comparison with the open suture technique, onlay and underlay or intraperitoneal onlay technique, consistently lower recurrence rates have been identified for the sublay/retro-rectus technique. Likewise, the surgical site infection rate is lower after sublay/retro-rectus repair of incisional hernias than after the onlay technique (45).
Although there are much less data available for evaluation of the sublay/retro-rectus technique for repair of incisional hernia than suggested by the myriad meta-analyses and systematic reviews, the sublay/retro-rectus technique appears to have advantages over the other open techniques. But it appears to have more disadvantages compared with laparoscopic IPOM.
However, a precise analysis of the existing literature clearly demonstrates that further studies are urgently needed to evaluate the role of the sublay/retro-rectus technique in repair of incisional hernia. To that effect, it is of paramount importance to focus on a single hernia entity and on two comparative surgical techniques. To evaluate the outcome it would also appear important to include here all details of the sublay/retro-rectus surgical technique with its different variants of meshes, fixation techniques and drain placement (60–76). Therefore, further RCTs using a standardized technique and restricted to incisional hernias should be carried out for comparison with both the laparoscopic IPOM and with other open techniques.
FK literature search, literature analyses, publication concept, publication draft. HS and CS-P literature search, literature analyses, publication concept, critical review of the publication draft.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Liang MK, Holihan JL, Itani K, Alawadi ZM, Gonzalez JR, Askenasy EP, et al. Ventral hernia management. Ann Surg. (2017) 265:80–9. doi: 10.1097/SLA.0000000000001701
2. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc. (2014) 28:2–29. doi: 10.1007/s00464-013-3170-6
3. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 2. Surg Endosc. (2014) 28:353–79. doi: 10.1007/s00464-013-3171-5
4. Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part III. Surg Endosc. (2014) 28:380–404. doi: 10.1007/s00464-013-3172-4
5. Silecchia G, Campanile FC, Sanchez L, Ceccarelli G, Antinori A, Ansaloni L, et al. Laparoscopic ventral/incisional hernia repair: updated consensus development conference based guidelines [corrected]. Surg Endosc. (2015) 29:2463–84. doi: 10.1007/s00464-015-4293-8
6. Earle D, Roth JS, Saber A, Haggerty S, Bradley JF, Fanelli R, et al. SAGES guidelines for laparoscopic ventral hernia repair. Surg Endosc. (2016) 30:3163–83. doi: 10.1007/s00464-016-5072-x
7. Goodney PP, Birkmeyer CM, Birkmeyer JD. Short-term outcomes of laparoscopic and open ventral hernia repair: a meta-analysis. Arch Surg. (2002) 137:1161–5. doi: 10.1001/archsurg.137.10.1161
8. Pham CT, Perera CL, Watkin DS, Maddern GJ. Laparoscopic ventral hernia repair: a systematic review. Surg Endosc. (2009) 23:4–15. doi: 10.1007/s00464-008-0182-8
9. Forbes SS, Eskicioglu C, McLeod RS, Okrainec A. Meta-analysis of randomized controlled trials comparing open and laparoscopic ventral and incisional hernia repair with mesh. Br J Surg. (2009) 96:851–8. doi: 10.1002/bjs.6668
10. Sajid MS, Bokhari SA, Mallick AS, Cheek E, Baig MK. Laparoscopic versus open repair of incisional/ventral hernia: a meta-analysis. Am J Surg. (2009) 197:64–72. doi: 10.1016/j.amjsurg.2007.12.051
11. Sauerland S, Walgenbach M, Habermalz B, Seiler CM, Miserez M. Laparoscopic versus open surgical techniques for ventral or incisional hernia repair. Cochrane Database Syst Rev. (2011) 3: CD007781. doi: 10.1002/14651858.CD007781.pub2
12. Zhang Y, Zhou H, Chai Y, Cao C, Jin K, Hu Z. Laparoscopic versus open incisional and ventral hernia repair: a systematic review and meta-analysis. World J Surg. (2014) 38:2233–40. doi: 10.1007/s00268-014-2578-z
13. Nguyen MT, Berger RL, Hicks SC, Davila JA, Li LT, Kao LS, et al. Comparison of outcomes of synthetic mesh vs. suture repair of elective primary ventral herniorrhaphy: a systematic review and meta-analysis. JAMA Surg. (2014) 149:415–21. doi: 10.1001/jamasurg.2013.5014
14. Mathes T, Walgenbach M, Siegel R. Suture versus mesh repair in primary and incisional ventral hernias: a systematic review and meta-analysis. World J Surg. (2016) 40:826–35. doi: 10.1007/s00268-015-3311-2
15. Holihan JL, Hanon C, Goodenough C, Flores-Gonzalez JR, Itani KM, Olavarria O, et al. Ventral hernia repair: a meta-analysis of randomized controlled trials. Surg Infect. (2017) 18:647–58. doi: 10.1089/sur.2017.029
16. Albino FP, Patel KM, Nahabedian M, Sosin M, Attinger CE, Bhanot P. Does mesh location matter in abdominal wall reconstruction? A systematic review of the literature and a summary of recommendations. Plast Rconstr Surg. (2013) 132:1295–304. doi: 10.1097/PRS.0b013e3182a4c393
17. Holihan JL, Nguyen DH, Nguyen MT, Mo J, Kao LS, Liang MK. Mesh location in open ventral hernia repair: a systematic review and network meta-analysis. World J Surg. (2015) 40:89–99. doi: 10.1007/s00268-015-3252-9
18. Den Hartog D, Dur AH, Tuinebreijer WE, Kreis RW. Open surgical procedures for incisional hernias. Cochrane Database Syst Rev. (2008) 2008:D006438. doi: 10.1002/14651858.CD006438.pub2
19. Deerenberg EB, Timmermans L, Hogerzeil DP, Slieker JC, Eilers PHC, Jeekel J, et al. A systematic review of the surgical treatment of large incisional hernia. Hernia (2015) 19:89–101. doi: 10.1007/s10029-014-1321-x
20. Eriksson A, Rosenberg J, Bisgaard T. Surgical treatment for giant incisional hernia: a qualitative systematic review. Hernia (2014) 18:31–38. doi: 10.1007/s10029-013-1066-y
21. Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, et al. Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia (2015) 19:449–63. doi: 10.1007/s10029-015-1351-z
22. Awaiz A, Rahman F, Hossain MB, Yunus RM, Khan S, Memon B, et al. Reply to comment to meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia (2015) 19:1027–9. doi: 10.1007/s10029-015-1432-z
23. Jensen KK, Jorgensen LN. Comment to: meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Awaiz A, et al. Hernia. 19:449–463. Hernia (2015) 19:1025–6. doi: 10.1007/s10029-015-1412-3
24. Chalabi HA, Larkin J, Mehigan B, McCormick P. A systematic review of laparoscopic versus open abdominal incisional hernia repair, with meta-analysis or randomized controlled trials. Int J Surg. (2015) 20:65–74. doi: 10.1016/j.ijsu.2015.05.050
25. Timmermans L, de Goede B, van Dijk SM, Kleinrensink GJ, Jeekel J, Lange JF. Meta-analysis of sublay versus onlay mesh repair in incisional hernia surgery. Am J Surg. (2014) 6:980–9. doi: 10.1016/j.amjsurg.2013.08.030
26. Dietz UA, Menzel S, Lock J, Wiegering A. The treatment of incisional hernia. Dtsch Ärztebl Int. (2018) 115:31–7. doi: 10.3238/arztebl.2018.0031
27. Kokotovic D, Gögenur I, Helgstrand F. Substantial variation among hernia experts in the decision for treatment of patients with incisional hernia: a descriptive study on agreement. Hernia (2017) 21:271–8. doi: 10.1007/s10029-016-1562-y
28. Holihan J, Nguyen DH, Flores-Gonzalez JR, Alawadi ZM, Nguyen MT, Ko TC, et al. A systematic review of randomized controlled trials and reviews in the management of ventral hernias. J Surg Res. (2016) 204:311–8. doi: 10.1016/j.jss.2016.05.009
29. Parker SG, Wood CPJ, Butterworth JW, Boulton RW, Plumb AAO, Mallet S, et al. A systematic methodological review of reported perioperative variables, postoperative outcomes and hernia recurrence from randomized controlled trials of elective ventral hernia repair: clear definitions and standardized datasets are needed. Hernia (2018) 22:215–26. doi: 10.1007/s10029-017-1718-4
30. Kurian A, Gallagher S, Cheeyandira A, Josloff R. Laparoscopic repair of primary versus incisional ventral hernias: time to recognize the differences? Hernia (2010) 14:383–7. doi: 10.1007/s10029-010-0649-0
31. Subramanian A, Clapp ML, Hicks SC, Awad SS, Liang MK. Laparoscopic ventral hernia repair: primary versus secondary hernias. J Surg Res. (2013) 181:e1–5. doi: 10.1016/j.jss.2012.06.028
32. Stirler VMA, Schoenmaeckers EJP, de Haas RJ, Raymakers JTFJ, Rakic S. Laparoscopic repair of primary and incisional ventral hernias: the differences must be acknowledged. Surg Endosc. (2014) 28:891–5. doi: 10.1007/s00464-013-3243-6
33. Köckerling F, Schug-Paß C, Adolf D, Reinpold W, Stechemesser B. Is pooled data analysis of ventral and incisional hernia repair acceptable? Front Surg. (2015) 2:15. doi: 10.3389/fsurg.2015.00015
34. Parker SG, Wood CPJ, Sanders DL, Windsor ACJ. Nomenclature in abdominal wall hernias: is it time for consensus? World J Surg. (2017) 41:2488–91. doi: 10.1007/s00268-017-4037-0
35. Luijendijk RW, Hop WCP, van den Tol P, De Lange DCD, Braaksma MMJ, Ijzermans JNM, et al. A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med. (2000) 343:392–8. doi: 10.1056/NEJM200008103430603
36. Burger JWA, Luijendijk RW, Hop WCJ, Halm JA, Verdaasdonk EGG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. (2004) 240:578–85. doi: 10.1097/01.sla.0000141193.08524.e7
37. Itani KMF, Hur K, Kim LT, Anthony T, Berger DH, Reda D, et al. Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia—a randomized trial. Arch Surg. (2010) 145:322–8. doi: 10.1001/archsurg.2010.18
38. Navarra G, Musolino C, De Marco ML, Barolotta M, Barbera A, Centorrino T. Retromuscular sutured incisional hernia repair: a randomized controlled trial to compare open and laparoscopic approach. Surg Laparosc Endosc Percutan Tech. (2007) 17:86–90. doi: 10.1097/SLE.0b013e318030ca8b
39. Olmi S, Scaini A, Cesana C, Erba L, Croce E. Laparoscopic versus open incisional hernia repair: an open randomized controlled study. Surg Endosc. (2007) 21:555–9. doi: 10.1007/s00464-007-9229-5
40. Pring CM, Tran V, O'Rourke N, Martin IJ. Laparoscopic versus open ventral hernia repair: a randomized controlled trial. ANZ J Surg. (2008) 78:903–6. doi: 10.1111/j.1445-2197-2008.04689.x
41. Asencio F, Aguiló J, Peiró S, Carbo J, Ferri R, Caro F, et al. Open randomized clinical trial of laparoscopic versus open incisional hernia repair. Surg Endosc. (2009) 23:1441–8. doi: 10.1007/s00464-008-0230-4
42. Venclauskas L, Maleckas A, Kiudelis M. One-year follow-up after incisional hernia treatment: results of a prospective randomized study. Hernia (2010) 14:575–82. doi: 10.1007/s10029-010-0686-8
43. Wéber G, Horváth ÖP. Results of ventral hernia repair: a comparison of suture repair with mesh implantation (onlay vs. sublay) using open and laparoscopic approach (prospective, randomized, multicenter study). Magy Seb. (2002) 55:285–9.
44. Wéber G, Baracs J, Horváth ÖP. “Onlay” mesh provides significantly better results than “sublay” reconstruction. Magy Seb. (2010) 63:302–11. doi: 10.1556/MaSeb.63.2010.5.3
45. Eker HH, Hansson BME, Buunen M, Janssen IMC, Pierik REGJM, Hop WC, et al. Laparoscopic vs. open incisional hernia repair—a randomized clinical trial. JAMA Surg. (2013) 148:259–63. doi: 10.1001/jamasurg.2013.1466
46. Rogmark P, Petersson U, Bringman S, Eklund A, Ezra E, Sevonius D, et al. Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg. (2013) 258:37–45. doi: 10.1097/SLA.0b013e31828fe1b2
47. Rogmark P, Petersson U, Bringman S, Ezra E, Österberg J, Montgomery A. Quality of life and surgical outcome 1 year after open and laparoscopic incisional hernia repair—PROLOVE: a randomized controlled trial. Ann Surg. (2016) 263:244–50. doi: 10.1097/SLA.0000000000001305
48. Natarajan S, Meenaa S, Thimmaiah KA. A randomized prospective study to evaluate preperitoneal mesh repair versus onlay mesh repair and laparoscopic IPOM in incisional hernia surgery. Indian J Surg. (2017) 79:96–100. doi: 10.1007/s12262-015-1430-5
49. Kumar V, Rodrigues G, Ravi C, Kumar S. A comparative analysis on various techniques of incisional hernia repair-experience from a tertiary care teaching hospital in South India. Indian J Surg. (2013) 75:271–3. doi: 10.1007/s12262-012-0644-z
50. Israelsson LA, Smedberg S, Montgomery A, Nordin P, Spangen L. Incisional hernia repair in Sweden 2002. Hernia (2006) 10:258–61. doi: 10.1007/s10029-006-0084-4
51. Gleysteen JJ. Mesh-reinforced ventral hernia repair—preference for 2 techniques. Arch Surg. (2009) 144:740–5. doi: 10.1001/archsurg.2009.118
52. Forte A, Zullino A, Manfredelli S, Montalto G, Bezzi M. Incisional hernia surgery: report on 283 cases. Eur Rev Med Pharmacol Sci. (2011) 15:644–8.
53. Abdollahi A, Maddah GH, Mehrabi BM, Jangjoo A, Forghani MN, Sharbaf N. Prosthetic incisional hernioplasty: clinical experience with 354 cases. Hernia (2010) 14:569–73. doi: 10.1007/s10029-010-0685-9
54. Kingsnorth AN, Sivarajasingham N, Wong S, Butler M. Open mesh repair of incisional hernias with significant loss of domain. Ann R Coll Surg Engl. (2004) 86:363–6. doi: 10.1308/147870804236
55. De Vries Reilingh TS, van Geldere D, Langenhorst BLAM, de Jong D, van der Wilt GJ, van Goor H, et al. Repair of large midline incisional hernias with polypropylene mesh: comparison of three operative techniques. Hernia (2004) 8:56–9. doi: 10.1007/s10029-003-0170-9
56. Coskun M, Peker Y, Tatar F, Cin N, Kar H, Kahya MC. Median incisional hernia and the factors affecting the recurrence of median incisional hernia repair. Erciyes Tip Dergisi (Erciyes Med J). (2009) 31:244–9.
57. Demetrashvili Z, Pipia I, Loladze D, Metreveli T, Ekaladze E, Kenchadze G, et al. Open retromuscular mesh repair versus onlay technique of incisional hernia: a randomized controlled trial. Int J Surg. (2017) 37:65–70. doi: 10.1016/j.ijsu.2016.12.008
58. Sevinc B, Okus A, Ay S, Aksoy N, Karahan Ö. Randomized prospective comparison of long-term results onlay and sublay mesh repair techniques for incisional hernia. Turk J Surg. (2018) 34:17–20. doi: 10.5152/turkjsurg.2017.3712
59. Helgstrand F, Rosenberg J, Kehlet H, Jorgensen LN, Bisgaard T. Nationwide prospective study of outcomes after elective incisional hernia repair. J Am Coll Surg. (2013) 216:217–28. doi: 10.1016/j.jamcollsurg.2012.10.013
60. Flament JB, Palot JP. Prosthetic repair of massive abdominal ventral hernias. In: Fitzgibbons RJ, Greenburg AG, editors. Nyhus and Condon's Hernia. Philadelphia, PA: Lippincott Williams & Wilkins (2002). 341–365 p.
62. Novitsky YW. Open retromuscular ventral hernia repair. In: Rosen MJ, editor. Atlas of Abdominal Wall Reconstruction. Philadelphia, PA: Elsevier Saunders (2012). 74–95 p.
63. Conze J, Prescher A, Kisielinski K, Klinge U, Schumpelik V. Technical consideration for subxiphoidal incisional hernia repair. Hernia (2005) 9:84–7. doi: 10.1007/s10029-004-0239-0
64. Conze J, Prescher A, Klinge U, Saklak M, Schumpelik V. Pitfalls in retromuscular mesh repair for incisional hernia: the importance of the “fatty triangle.” Hernia (2004) 8:255–9. doi: 10.1007/s10029-004-0235-4
65. Klinge U, Conze J, Krones CJ, Schumpelik V. Incisional hernia: open techniques. World J Surg. (2005) 29:1066–72. doi: 10.007/soo268-005-7970-2
66. Li J, Ji Z, Zang W, Li L. The comparison of lightweight mesh and standard mesh in incisional hernia repair with the open sublay technique: the results of a meta-analysis. Surg Laparosc Endosc Percutan Tech. (2015) 25:238–44. doi: 10.1097/SLE.0000000000000144
67. Conze J, Kingsnorth AH, Flament JB, Simmermacher R, Arlt G, Langer C, et al. Randomized clinical trial comparing lightweight compositemesh with polyester of polypropylene mesh for incisional hernia repair. Br J Surg. (2005) 92:1488–93. doi: 10.1002/bjs.5208
68. Welty G, Klinge U, Klosterhalfen B, Kasperk R, Schumpelik V. Functional impairment and complaints following incisional hernia repair with different polypropylene meshes. Hernia (2001) 5:142–7. doi: 10.1007/s1002900100017
69. Schmidbauer S, Ladurner R, Hallfeldt KK, Mussack T. Heavy-weight versus low-weight polypropylene meshes for open sublay mesh repair of incisional hernia. Eur J Med Res. (2005) 10:247–53.
70. Berrevoet F, Maes L, De Baerdemaeker L, Rogiers X, Troisi R, de Hemptinne B. Comparable results with 3-year follow-up for large-pore versus small-pore meshes in open incisional hernia repair. Surgery (2010) 148:969–75. doi: 10.1016/j.surg.2010.02.011
71. Ladurner R, Chiapponi C, Linhuber Q, Mussak T. Long term outcome and quality of life after open incisional hernia repair—light versus heavy weight meshes. BMC Surg. (2011) 11:25. doi: 10.1186/1471-2482-11-25
72. Rickert A, Kienle P, Kuthe A, Baumann P, Engemann R, Kuhlgatz J, et al. A randomized, multi-centre, prospective, observer and patient blind study to evaluate a non-absorbable polypropylene mesh vs. a partly absorbable mesh in incisional hernia repair. Langenbecks Arch Surg. (2012) 397:1225–34. doi: 10.1007/s00423-012-1009-6
73. Khansa I, Janis JE. Abdominal wall reconstruction using retrorectus self-adhering mesh: a novel approach. Plast Reconstr Surg Glob Open (2016) 4:e1145. doi: 10.1097/GOX.0000000000001145
74. Bueno-Lledó J, Torregrosa A, Arguelles B, Carreno O, Garcia P, Bonafe S, et al. Progrip self-gripping mesh in Rives-Stoppa repair: are there any differences in outcomes versus a retromuscular polypropylene mesh fixed with sutures? A “case series” study. Int J Surg Case Rep. (2017) 34:60–4. doi: 10.1016/j.ijscr.2017.03.012
75. Weltz AS, Sibia US, Zahiri HR, Schoeneborn A, Park A, Belyansky I. Operative outcomes after open abdominal wall reconstruction with retromuscular mesh fixation using fibrin glue versus transfascial sutures. Am Surg. (2017) 83:937–42.
Keywords: incisional hernia, sublay, mesh, retro-rectus repair, systematic (literature) review
Citation: Köckerling F, Schug-Pass C and Scheuerlein H (2018) What Is the Current Knowledge About Sublay/Retro-Rectus Repair of Incisional Hernias? Front. Surg. 5:47. doi: 10.3389/fsurg.2018.00047
Received: 17 April 2018; Accepted: 05 July 2018;
Published: 13 August 2018.
Edited by:
René H. Fortelny, Department of General, Viszeral and Oncologic Surgery, Wilhelminenspital, AustriaReviewed by:
Ulf Gunnarsson, Umeå University, SwedenCopyright © 2018 Köckerling, Schug-Pass and Scheuerlein. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ferdinand Köckerling, ZmVyZGluYW5kLmtvZWNrZXJsaW5nQHZpdmFudGVzLmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.