
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 22 June 2017
Sec. Neurosurgery
Volume 4 - 2017 | https://doi.org/10.3389/fsurg.2017.00033
Background: Direct comparisons of microscopic and endoscopic resection of sellar lesions are scarce, with conflicting reports of cost and clinical outcome advantages.
Objective: To determine if the proposed benefits of endoscopic resection are realized on a population level.
Methods: We performed a matched cohort study of 9,670 adult patients in the MarketScan database who underwent either endoscopic or microscopic surgery for sellar lesions. Coarsened matching was applied to estimate the effects of surgical approach on complication rates, length of stay (LOS), costs, and likelihood of postoperative radiation.
Results: We found that LOS, readmission, and revision rates did not differ significantly between approaches. The overall complication rate was higher for endoscopy (47% compared to 39%, OR 1.37, 95% CI 1.22–1.53). Endoscopic approach was associated with greater risk of neurological complications (OR 1.32, 95% CI 1.11–1.55), diabetes insipidus (OR 1.65, 95% CI 1.37–2.00), and cerebrospinal fluid rhinorrhea (OR 1.83, 95% CI 1.07–3.13) compared to the microscopic approach. Although the total index payment was higher for patients receiving endoscopic resection ($32,959 compared to $29,977 for microscopic resection), there was no difference in long-term payments. Endoscopic surgery was associated with decreased likelihood of receiving post-resection stereotactic radiosurgery (OR 0.67, 95% CI 0.49–0.90) and intensity-modulated radiation therapy (OR 0.78, 95% CI 0.65–0.93).
Conclusion: Our results suggest that the transition from a microscopic to endoscopic approach to sellar lesions must be subject to careful evaluation. Although there are evident advantages to transsphenoidal endoscopy, our analysis suggests that the benefits of the endoscopic approach are yet to be materialized.
Traditionally, sellar lesions such as pituitary adenomas, craniopharyngiomas, and Rathke’s cleft cysts were resected using a transsphenoidal approach with microscopy (1). However, since the introduction of endoscopic instruments and technique described by Jankowski et al. in 1992, many institutions have reported a gradual transition to the endoscopic approach (2, 3). The microscopic approach requires a nasal speculum to fracture the nasal septum and a sphenoidotomy to facilitate access to the anterior skull base. Endoscopic surgery may use one or both nostrils for access following a posterior septectomy. The endoscopic view is noted to provide a wider degree of freedom and improved visual access to the sella, although limitations related to lens cleaning and “sword fighting” with instruments have been acknowledged (4). The microscopic approach provides three-dimensional visualization and surgeon familiarity with the operating microscope (5).
The body of evidence comparing these two techniques is largely comprised of retrospective case series or cohort studies from single institutions (6–12). While individual studies report differences between the two approaches in complication rates, including cerebrospinal fluid (CSF) leak, temporary and permanent diabetes insipidus, hypopituitarism, meningitis, carotid artery injury, and visual and rhinologic complications, a consistent benefit regarding complication rates has not been observed in systematic reviews and meta-analyses (13–16). However, many studies report that endoscopic approach is associated with a shorter length of hospital stay (14, 17–20) and may be more cost-effective in the long term based on modeling (21, 22) as well as in a single-institution series (23).
The objectives of this study were to compare the microscopic and endoscopic approaches to assess (1) 30-day complication rates; (2) length of stay (LOS), readmission, and revision rate; (3) costs; and (4) likelihood of post-resection radiation therapy. To date, the comparison of endoscopic vs. microscopic approach to sellar lesions has not been conducted using a large database that contains a representative sample of the United States population.
We performed a retrospective observational administrative database study of 9,670 adult patients who underwent either endoscopic or microscopic surgery for sellar lesions in the United States from 2007 to 2014. We used claims data from the Truven Health Analytics MarketScan Commercial Claims and Encounters and Medicare Supplemental and Coordination of Benefits databases, which include data from >100 payers and use specific patient identifiers for longitudinal patient tracking of claims, billing, and payment history. The longitudinal characteristic of this database enabled assessment of patient comorbidities and complications both before and after the index procedure. The MarketScan database also allows tracking of patient health-care expenditures for the entirety of their private insurance coverage.
We queried the MarketScan database for patients who received either microscopic or endoscopic resection of sellar lesions. We utilized Current Procedural Terminology (CPT) codes to define the cohort (CPT 61548, microscopic approach; CPT 62165, neuroendoscopic approach). Patients who underwent open surgery, who were younger than 18 years, and who had concurrent microscopic and endoscopic CPT codes were excluded from this analysis (Figure S1 in Supplementary Material). International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used to characterize surgical indications and comorbidities. Subsequent revision procedures, complications, and in-hospital mortality were determined for all patients. The ICD-9 and CPT codes utilized in our study are detailed in Table S1 in Supplementary Material.
We used matched and unmatched regression models to estimate the effects of an endoscopic surgical approach on postoperative complication rates, mortality, length of hospital stay, readmission rates, surgical revision rates, costs of care, and extent of tumor resection. Patients with missing data for a variable of interest were excluded from the analysis. We used logistic regression to estimate models with binary outcomes (presence of various complications within 30 days of surgery, whether patient was discharged home after surgery, whether patient was readmitted to the hospital within 30 days of surgery, whether patient required a surgical revision, extent of tumor resection, and mortality), and used linear regression for continuous outcomes (length of hospital stay and total costs of care). All regression models controlled for the following covariates, which were considered likely to be associated with the outcomes of our models: patient age, gender, year of procedure, region of the country where the patient resides, and relevant comorbidities diagnosed prior to surgery (Cushing’s disease, acromegaly, hypertension, congestive heart failure, chronic obstructive pulmonary disorder, diabetes, obesity, past drug abuse, psychiatric illness, depression, electrolyte imbalance, hypothyroidism, and anemia).
We ran all regression models on our full sample of 9,670 patients. As a sensitivity analysis, we also ran the same models on a matched subset of our sample to correct for covariate imbalance in the full sample. This matched subset included 6,577 patients. We used coarsened exact matching (CEM) to create an analytic sample in which all covariates were distributed similarly among patients who received endoscopy and patients who received microscopic surgery. CEM is similar to propensity score matching, but it allows the analyst to specify a minimum degree of covariate balance and reduces model dependence and estimation error compared to propensity score matching (24). Similar results in the matched and unmatched models would indicate that covariate imbalance was not substantial enough to bias the results of our unmatched models.
From 2007 to 2014, we identified 3,621 patients (54.5% female, median age 50 years) who received endoscopic surgery and 6,049 patients (52.7% female, median age 50 years) who received microsurgery for sellar lesions. The most common primary surgical indications, as indicated by the preoperative ICD-9-CM codes, for both surgical approaches were identical, with over 80% of operations performed for benign neoplastic lesions of the pituitary gland and craniopharyngeal duct (ICD-9 code 227.3). Length of inpatient stay (3.5 days for endoscopic surgery vs. 3.6 days for microsurgery) did not differ significantly between these cohorts, while follow-up length was significantly longer among patients who received microsurgery (877 vs. 719 days for endoscopic surgical patients, p < 0.01). The distribution of demographic characteristics between endoscopic and microscopic approaches is given in Table 1. Coarsened matching allowed us to model cohorts balanced for patient demographics and comorbidities, also reflected in Table 1. We further observed an increase in total procedures during the duration of this study, with endoscopic surgery comprising a greater proportion of total procedures over time (Figure 1).
After matching the endoscopic and microscopic cohorts, we observed a greater risk of any complication when the endoscopic approach was used at a rate of 47% compared with 39% for microscopic approach (OR 1.37, 95% CI 1.22–1.53). We further found that patients receiving endoscopic surgery were at significantly greater risk of wound-related complications at a rate of 5.2 vs. 3.7% (OR 1.42, 95% CI 1.08–1.86), neurologic complications at a rate of 15 vs. 12% (OR 1.32, 95% CI 1.11–1.55), renal complications at a rate of 3.8 vs. 2.4% (OR 1.59, 95% CI 1.15–2.19), diabetes insipidus at a rate of 12 vs. 7.9% (OR 1.65, 95% CI 1.37–2.00), fluid electrolyte imbalance at a rate of 19.4 vs. 17.2% (OR 1.16, 95% CI 1.00–1.34), and cerebrospinal fluid (CSF) rhinorrhea at a rate of 1.7 vs. 0.9% (OR 1.83, 95% CI 1.07–3.13). We did not observe any significant differences between the two approaches for eye movement injury (1.1% in endoscopic vs. 1.2% in microscopic) or iatrogenic pituitary disorder (2.6% in endoscopic vs. 2.9% in microscopic) (Figure 2).
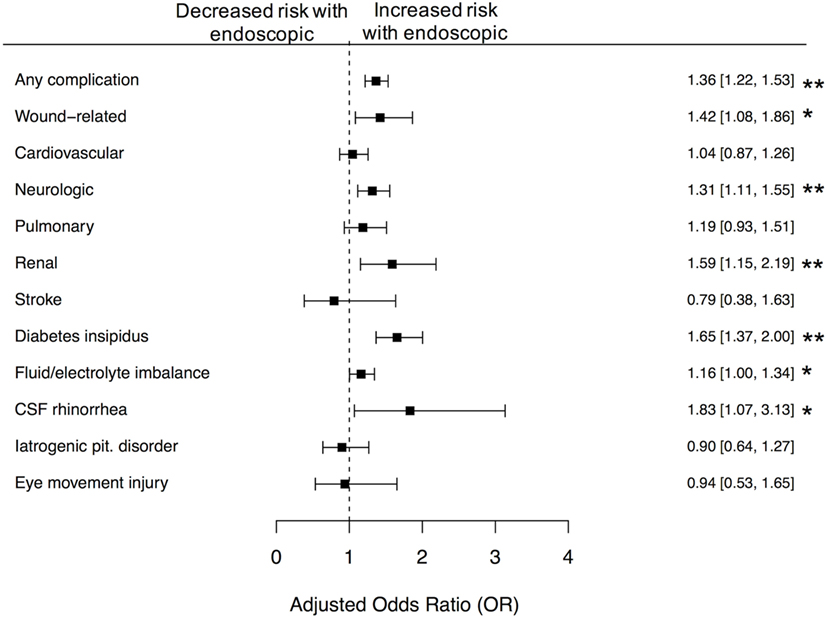
Figure 2. Differences in 30-day complications between microscopic and endoscopic approaches, following adjustment with CEM. Following coarsened exact matching (CEM), we observed significantly increased risk of any complication (p < 0.01), wound-related complications (p < 0.05), neurologic complications (p < 0.01), renal complications (p < 0.01), diabetes insipidus (p < 0.01), fluid and electrolyte imbalance (p < 0.05), and CSF rhinorrhea (p < 0.05), following receipt of endoscopic approach. Error bars indicate 95% CI; dashed line, no difference (OR = 1.0).
We found that 30-day all-cause readmission rates at 28% for both endoscopic and microscopic approaches (OR 0.98, 95% CI 0.86–1.12), rate of discharge home at a rate of 94% for both approaches (OR 1.03, 95% CI 0.82–1.29), and inpatient mortality at a rate of 0.2% for endoscopic compared to 0.4% for microscopic approach (OR 0.63, 95% CI 0.17–2.36) were comparable between the two approaches in the matched cohort. While we observed that endoscopic surgery was protective for receipt of revision procedure (OR 0.73, 95% CI 0.57–0.92) in the unmatched cohort, this difference did not reach statistical significance after controlling for differences in demographics and comorbidities between those who received endoscopic surgery and those who did not (OR 0.77, 95% CI 0.58–1.34) (Table 2).
In the matched cohorts, we found significantly higher total index payments for patients receiving endoscopic resection at $32,959 compared to $29,977 for microscopic resection (mean increase of $2,982.78, 95% CI 1,316.28–4,649.29). Notably, we observed no difference in either 90- or 180-day payments between the groups (Table 3). The majority of these higher index payments went to hospitals (hospital payments were $2,508.87 higher among endoscopy patients, p < 0.01) rather than to physicians (no significant difference).
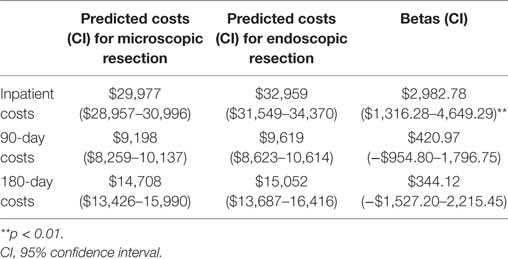
Table 3. Comparative payments between microscopic and endoscopic approaches during the initial inpatient admission and at 90 and 180 days.
We observed an overall decrease in likelihood of receiving post-resection radiation after endoscopic surgery relative to microscopic surgery in both the unmatched and matched cohorts (Figure 3). The endoscopic approach was predicted to decrease the likelihood of receiving post-resection stereotactic radiosurgery (SRS) in the unmatched (OR 0.76, 95% CI 0.61–0.95) and matched cohorts (OR 0.67, 95% CI 0.49–0.90). Similarly, the endoscopic approach was predicted to decrease likelihood of receiving post-resection intensity-modulated radiation therapy in the unmatched (OR 0.79, 95% CI 0.69–0.91) and matched cohorts (OR 0.78, 95% CI 0.65–0.93).
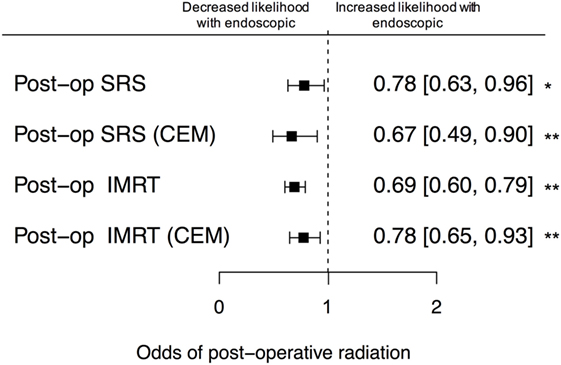
Figure 3. Likelihood of post-resection stereotactic radiosurgery (SRS) and intensity-modulated radiation therapy (IMRT). There was a lower unadjusted odds of receiving either SRS or IMRT following endoscopic resection, relative to microscopic resection. After coarsened exact matching (CEM), these differences were preserved and statistically significant (p < 0.01). Error bars indicate 95% CIs; dashed line, no difference (OR = 1.0).
Based on existing literature of single-institution studies and systematic reviews, we expected no significant differences between the complication rates when comparing microscopic and endoscopic approach to resection of sellar lesions using the MarketScan claims database. However, our results provide additional and unexpected insight into the recent practice of the two techniques from 2007 to 2014 in a large representative sample of the general United States population that allows rigorous statistical analysis with strict matching criteria.
Our endoscopic (n = 3,621) and microscopic (n = 6,049) cohorts were overall similar, including primary indications for surgery. This suggests that both approaches are currently considered viable in the same clinical context. Neither approach seemed to prefer one indication over the other, although this may be due to the high prevalence of benign pituitary lesions as well as the non-specific diagnostic code in ICD-9, “227.3 Benign neoplasm of pituitary gland and craniopharyngeal duct.” We saw an increase in endoscopic approach over the eight years of study duration. This result is consistent with the literature of single-center studies that report institutional transition from microscopic to endoscopic approach.
Complication and mortality rate are major ways of assessing whether one procedure is preferable to the other. While endoscopic approach was protective in the context of inpatient mortality rates, this result was not significant at the alpha level of 0.05. Endoscopic cases had 37% higher odds of any 30-day complication compared to microscopic cases as well as higher odds for specific complications including diabetes insipidus, electrolyte imbalance, CSF rhinorrhea, wound-related, neurologic, and renal complications. This is unexpected, given that existing studies suggest overall no difference between the two approaches. However, most single-institution studies were conducted in high-volume endoscopic centers while our study includes cases from all levels of care. Interestingly, although there were higher odds of complications among the endoscopic cases, the endoscopic approach was observed to have decreased rates of revision procedure in the unmatched comparison. However, this result was not statistically significant in the strictly matched cohort. The higher rate of complications along with decreased rate of revision suggests a more aggressive resection in the endoscopic approach.
Since transsphenoidal endoscopic approach is a relatively new technique compared to the traditional gold standard of the microscopic approach, we examined whether there was a training effect that may play a role in the higher complication rate observed among endoscopic cases. However, the complication rate for the endoscopic approach remains higher than microscopic throughout every year of our data and does not appear to be trending downward at a faster rate than the microscopic approach. To further evaluate complication rate on an individual basis, we anticipate further studies that compare complication rates among individual surgeons stratified by volume based on several studies examining the learning curve associated with transsphenoidal endoscopic surgery (3, 25). It is possible that our finding of a higher complication rate in endoscopic resection is due to surgeon experience and/or volume. This result has been suggested in previous Nationwide Inpatient Sample studies (1, 26).
While this is important to bear in mind, the observation itself is important for surgeons and patients to be aware of. The single-institution studies in the literature that describe outcomes of endoscopy are from early-adopters and often from high-volume centers. Our finding is that the advantages of endoscopic resection have not yet materialized on a population level.
Additionally, there was a 21% reduction in odds for stroke complication in endoscopic cases compared to microscopic cases in our matched cohort, although this finding was not significant at an alpha level of 0.05. Carotid injury was a rare complication in our study with only five occurrences in endoscopic cases and two occurrences in microscopic cases. Given the small sample size, we could not analyze whether this difference was statistically significant.
Length of hospital stay, 30-day readmission rate, and rate of discharge home were similar for both endoscopic and microscopic cases, which was surprising because previous studies had shown the endoscopic approach to have shorter LOS. One major advantage of this dataset is the longitudinal follow-up of patients based on unique identifiers. Based on this, we could characterize the duration of follow up, which was significantly longer among microscopic cases. This may be due to differences in preference of the duration of follow-up between endoscopic vs. microscopic surgeons, as increased complication rates do not seem to correlate with the increased length of follow-up. Although the length of hospital stay was shorter in the endoscopic cohort (3.5 vs. 3.6 days), endoscopic cases had higher total index payment by $2,982.78. Given that the 90-day and 180-day payments were similar, the increased cost from longer duration of follow-up among microscopic cases may balance the higher index cost for endoscopic cases.
The likelihood of receiving post-resection radiation in the endoscopic group was overall decreased relative to the microscopic group in both stereotactic radiosurgery and intensity-modulated radiation therapy. The decreased likelihood in the endoscopic group may suggest that the endoscopic group had less residual tumor and more complete resection. This may also explain the increased complication rates in the endoscopic group, suggesting that endoscopic approach is more aggressive, undergoes more complete resection, and requires less post-resection radiation.
One important limitation of our study is the inability to analyze complication rates stratified by tumor size and extent, which may confound the actual complication rates attributable to each technique. Many groups employ an endoscopic approach for anatomically extensive tumors not amenable to microscopic resection and this difference may underlie the observed differences in complication rates. However, this is an inherent limitation of the claims data since there are no ICD-9 or CPT codes that provide indication with respect to the size or extent of the tumor.
Taken together, our results suggest that the transition from a microscopic to endoscopic approach to sellar lesions must be subject to careful evaluation. While there are evident advantages to transsphenoidal endoscopy, our analysis suggests that the benefits of the endoscopic approach are yet to be materialized.
TA, AV, PH, JR, and GL developed the concept for the study. TA and DV carried out statistical analysis. TA, YJL, DV, AV, PH, JR, and GL contributed to the drafting of the paper and editing of the final manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at http://journal.frontiersin.org/article/10.3389/fsurg.2017.00033/full#supplementary-material.
Figure S1. CONSORT diagram.
Table S1. Compendium of ICD9/CPT codes used in the study.
1. Barker FG II, Klibanski A, Swearingen B. Transsphenoidal surgery for pituitary tumors in the United States, 1996-2000: mortality, morbidity, and the effects of hospital and surgeon volume. J Clin Endocrinol Metab (2003) 88:4709–19. doi:10.1210/jc.2003-030461
2. Jankowski R, Auque J, Simon C, Marchal JC, Hepner H, Wayoff M. Endoscopic pituitary tumor surgery. Laryngoscope (1992) 102:198–202. doi:10.1288/00005537-199202000-00016
3. Singh H, Essayed WI, Cohen-Gadol A, Zada G, Schwartz TH. Resection of pituitary tumors: endoscopic versus microscopic. J Neurooncol (2016) 130:309–17. doi:10.1007/s11060-016-2124-y
4. de Divitiis E, Laws ER, Giani U, Iuliano SL, De Divitiis O, Apuzzo ML. The current status of endoscopy in transsphenoidal surgery: an international survey. World Neurosurg (2015) 83:447–54. doi:10.1016/j.wneu.2014.12.029
5. Louis RG, Eisenberg A, Barkhoudarian G, Griffiths C, Kelly DF. Evolution of minimally invasive approaches to the sella and parasellar region. Int Arch Otorhinolaryngol (2014) 18:S136–48. doi:10.1055/s-0034-1395265
6. DeKlotz TR, Chia SH, Lu W, Makambi KH, Aulisi E, Deeb Z. Meta-analysis of endoscopic versus sublabial pituitary surgery. Laryngoscope (2012) 122:511–8. doi:10.1002/lary.22479
7. Komotar RJ, Starke RM, Raper DM, Anand VK, Schwartz TH. Endoscopic endonasal compared with microscopic transsphenoidal and open transcranial resection of craniopharyngiomas. World Neurosurg (2012) 77:329–41. doi:10.1016/j.wneu.2011.07.011
8. Fathalla H, Cusimano MD, Di Ieva A, Lee J, Alsharif O, Goguen J, et al. Endoscopic versus microscopic approach for surgical treatment of acromegaly. Neurosurg Rev (2015) 38:541–8; discussion 548–9. doi:10.1007/s10143-015-0613-7
9. Gondim JA, Almeida JP, De Albuquerque LA, Gomes E, Schops M, Mota JI. Endoscopic endonasal transsphenoidal surgery in elderly patients with pituitary adenomas. J Neurosurg (2015) 123:31–8. doi:10.3171/2014.10.JNS14372
10. Karppinen A, Kivipelto L, Vehkavaara S, Ritvonen E, Tikkanen E, Kivisaari R, et al. Transition from microscopic to endoscopic transsphenoidal surgery for nonfunctional pituitary adenomas. World Neurosurg (2015) 84:48–57. doi:10.1016/j.wneu.2015.02.024
11. Guvenc G, Kizmazoglu C, Pinar E, Imre A, Kaya I, Bezircioglu H, et al. Outcomes and complications of endoscopic versus microscopic transsphenoidal surgery in pituitary adenoma. J Craniofac Surg (2016) 27:1015–20. doi:10.1097/SCS.0000000000002684
12. Levi V, Bertani GA, Guastella C, Pignataro L, Zavanone ML, Rampini PM, et al. Microscopic versus endoscopic transsphenoidal surgery for pituitary adenoma: analysis of surgical safety in 221 consecutive patients. Clin Otolaryngol (2017) 42(2):466–69. doi:10.1111/coa.12631
13. Rotenberg B, Tam S, Ryu WH, Duggal N. Microscopic versus endoscopic pituitary surgery: a systematic review. Laryngoscope (2010) 120:1292–7. doi:10.1002/lary.20949
14. Goudakos JK, Markou KD, Georgalas C. Endoscopic versus microscopic trans-sphenoidal pituitary surgery: a systematic review and meta-analysis. Clin Otolaryngol (2011) 36:212–20. doi:10.1111/j.1749-4486.2011.02331.x
15. Ammirati M, Wei L, Ciric I. Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry (2013) 84:843–9. doi:10.1136/jnnp-2012-303194
16. Gao Y, Zhong C, Wang Y, Xu S, Guo Y, Dai C, et al. Endoscopic versus microscopic transsphenoidal pituitary adenoma surgery: a meta-analysis. World J Surg Oncol (2014) 12:94. doi:10.1186/1477-7819-12-94
17. Cho DY, Liau WR. Comparison of endonasal endoscopic surgery and sublabial microsurgery for prolactinomas. Surg Neurol (2002) 58:371–5; discussion 375–6. doi:10.1016/S0090-3019(02)00892-3
18. White DR, Sonnenburg RE, Ewend MG, Senior BA. Safety of minimally invasive pituitary surgery (MIPS) compared with a traditional approach. Laryngoscope (2004) 114:1945–8. doi:10.1097/01.mlg.0000147925.04605.cc
19. Neal JG, Patel SJ, Kulbersh JS, Osguthorpe JD, Schlosser RJ. Comparison of techniques for transsphenoidal pituitary surgery. Am J Rhinol (2007) 21:203–6. doi:10.2500/ajr.2007.21.2981
20. Gao Y, Zheng H, Xu S, Zheng Y, Wang Y, Jiang J, et al. Endoscopic versus microscopic approach in pituitary surgery. J Craniofac Surg (2016) 27:e157–9. doi:10.1097/SCS.0000000000002401
21. Rudmik L, Starreveld YP, Vandergrift WA, Banglawala SM, Soler ZM. Cost-effectiveness of the endoscopic versus microscopic approach for pituitary adenoma resection. Laryngoscope (2015) 125:16–24. doi:10.1002/lary.24780
22. Jethwa PR, Patel TD, Hajart AF, Eloy JA, Couldwell WT, Liu JK. Cost-effectiveness analysis of microscopic and endoscopic transsphenoidal surgery versus medical therapy in the management of microprolactinoma in the United States. World Neurosurg (2016) 87:65–76. doi:10.1016/j.wneu.2015.10.090
23. Oosmanally N, Paul JE, Zanation AM, Ewend MG, Senior BA, Ebert CS Jr. Comparative analysis of cost of endoscopic endonasal minimally invasive and sublabial-transseptal approaches to the pituitary. Int Forum Allergy Rhinol (2011) 1:242–9. doi:10.1002/alr.20048
24. Iacus SM, King G, Porro G. Causal inference without balance checking: coarsened exact matching. Polit Anal (2012) 20(1):1–24. doi:10.1093/pan/mpr013
25. Qureshi T, Chaus F, Fogg L, Dasgupta M, Straus D, Byrne RW. Learning curve for the transsphenoidal endoscopic endonasal approach to pituitary tumors. Br J Neurosurg (2016) 30:637–42. doi:10.1080/02688697.2016.1199786
Keywords: endoscopy, microscopy, pituitary, sellar lesions, complication rate
Citation: Azad TD, Lee YJ, Vail D, Veeravagu A, Hwang PH, Ratliff JK and Li G (2017) Endoscopic vs. Microscopic Resection of Sellar Lesions—A Matched Analysis of Clinical and Socioeconomic Outcomes. Front. Surg. 4:33. doi: 10.3389/fsurg.2017.00033
Received: 08 April 2017; Accepted: 06 June 2017;
Published: 22 June 2017
Edited by:
Ziya Levent Gokaslan, Brown University, United StatesReviewed by:
Shaan M. Raza, University of Texas MD Anderson Cancer Center, United StatesCopyright: © 2017 Azad, Lee, Vail, Veeravagu, Hwang, Ratliff and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gordon Li, Z29yZG9ubGlAc3RhbmZvcmQuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.