- Department of Gynecology-Obstetrics, University Hospital of Geneva, Geneva, Switzerland
Background: Abscesses located in the cesarean-section (CS) induced isthmoceles are rarely encountered and are usually treated surgically, mostly by hysterectomy.
Case description: We here report the case of a 40-year-old primiparous woman presenting a symptomatic abscess in the isthmocele 10 years after a CS. She was treated by antibiotics and was closely monitored by clinical evaluation, ultrasonography, and pelvic magnetic resonance imaging. This treatment led to complete resolution of symptoms and a disappearance of the abscess at imagery.
Conclusion: Our report shows that a conservative medical management of isthmocele abscesses can be an effective approach in women wishing to preserve their uterus.
Introduction
The cesarean delivery rate is steadily increasing worldwide (1). Cesarean sections (CSs) and resulting uterine scars are associated with obstetric complications, such as cesarean scar pregnancies, uterine rupture, abnormal placental implantation, and secondary infertility (2). Surgical site infection after CS is rare and happens mostly within 30 days (3). The reported rate of abdominal wound infection under prophylactic antibiotic coverage is usually around 0.52% (4). We present a rare case of a CS scar abscess having developed 10 years after delivery that was successfully managed by conservative antibiotic therapy.
Materials and Methods
A 40-year-old woman, primigravida, primiparous by CS, attended our hospital with a 3-week history of malodorous uterine discharge, and recent dysmenorrhea. She was not on any contraception. Her CS had taken place 10 years previously for non-progression and her baby had been born in good condition. There were no risk factors for sexually transmitted diseases. Physical examination revealed apyrexia with abdominal tenderness. Speculum inspection showed a brown malodorous cervical discharge with pus, and digital examination of the uterus was painful.
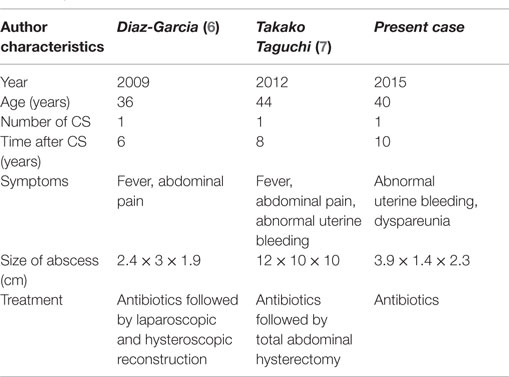
Pelvic ultrasonography demonstrated an ante-flexed, normal-sized uterus with a spherical mass within the uterus scar tissue between the cervix and the body of uterus, involving myometrium and measuring 39 mm × 14 mm × 23 mm. The center contained mixed echogenic and anechogenic material, evoking liquid and tissue components. The myometrium covering the lesion was thickened. There was no sign of adenomyosis. The endometrium measured 6 mm and was of normal appearance. Both ovaries were normal and there was no intra-peritoneal fluid (Figure 1).
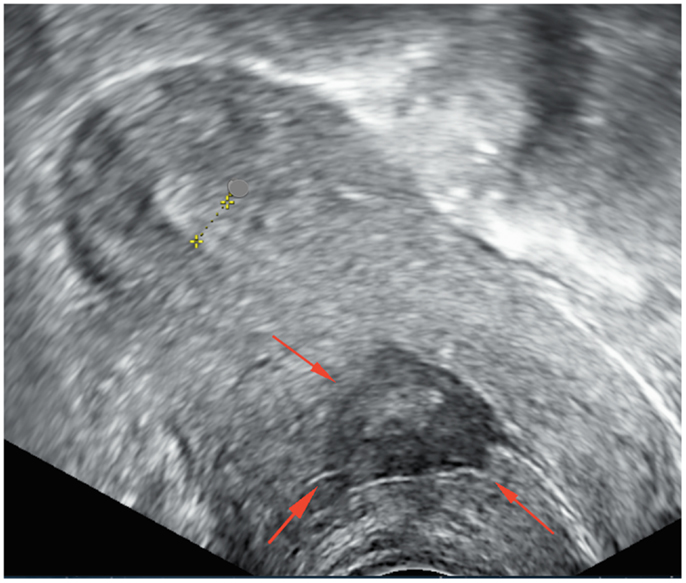
Figure 1. Pelvic ultrasonography before treatment shows a heterogenic cavity at the site of cesarean section.
Inflammation markers were slightly raised and a pregnancy test was negative. Cervical bacteriology was not contributive. Endometrial biopsy revealed purulent material with a lot of leukocytes and rare fragments of benign endometrial epithelium. We suspected an abscess. Magnetic resonance imaging (MRI) showed a well-defined uterine mass embedded in myometrium, made-up of mixed liquid and tissue components, without hypersignal in diffusion rating and taking up contrast peripherally (Figure 2).
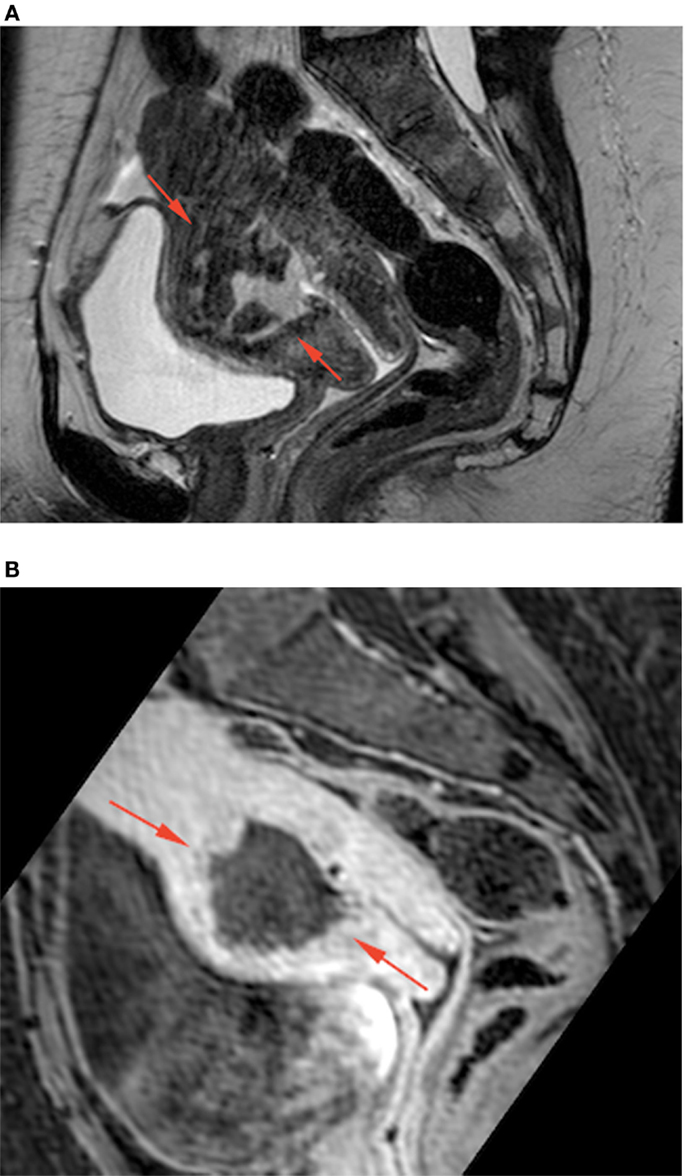
Figure 2. Sagittal T2-weighted TSE (A) and Dixon T1-weighted fat saturated after iv gadolinium injection (B) MRI images at presentation, showing a cavity with thick enhancing walls (red arrows) containing heterogeneous fluid and solid non-enhancing material at the anterior wall of the uterus at the site of cesarian section.
These images lead to a differential diagnosis, including necrotic fibroid and myosarcoma. Diagnostic hysteroscopy was difficult; we found a lot of inflammatory material, pus, and revealed necrotic tissue located in the lower anterior wall, forming a new cavity (“isthmocele”). We found no blood inside the cavity. The rest of the endometrial cavity was of normal appearance. All these elements led us to suspect an infection. Hence, a scar abscess having developed in a cesarean-induced isthmocele was suspected. We decided to attempt conservative treatment. She was a patient with an unremarkable medical history wishing to preserve her fertility. She was empirically treated with amoxicillin–clavulanic acid 1 g/12 h for 2 weeks with good tolerance.
Results
At the end of the 2 weeks, the patient was no longer symptomatic and a repeat ultrasound showed a reduction of the lesion of about 50% to 23 mm × 12 mm (Figure 3).
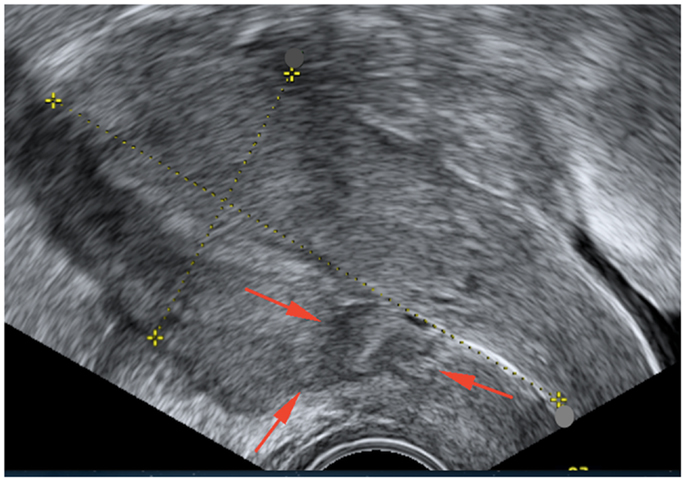
Figure 3. Pelvic ultrasonography after medical treatment shows a small residual heterogenic cavity at the site of cesarean section.
MRI 1 month later showed the disappearance of the entire lesion and the residual myometrial scar measured 5 mm (Figure 4).
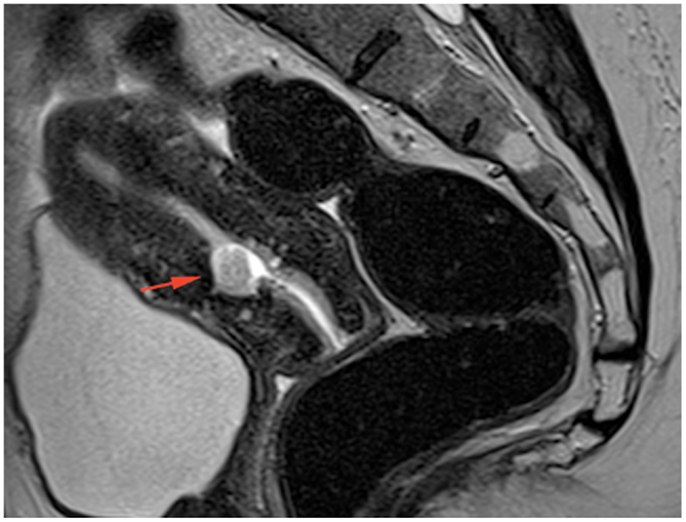
Figure 4. Sagittal T2-weighted TSE MRI image 1 month after medical treatment showing a small residual cavity containing some debris at the site of the abscess.
The patient remained asymptomatic at 20 months follow-up. The clinical response to the antibiotics and the results of imaging confirm our suspected initial diagnosis.
Discussion
New complications are appearing with the recorded increase in number of CS. The relative risk reduction with prophylactic antibiotics in maternal infection is well known, the incidence currently hovering around 2% for post-partum endometritis and around 0.52% for superficial wound infection (5). Infection after CS usually occurs within the first 30 days after delivery (3). Barbut et al. identified primiparity, CS in emergency circumstances or during labor and post-partum bacteriuria as the main risk factors for infective complications. Microorganisms most frequently identified include enterobacteria, anaerobes, staphylococcus aureus, and enterococcus. An abscess developing at the uterine incision site long after a CS is considered very rare. Only two cases have so far been reported (shown in Table 1 with their characteristics). One 6 years after CS treated by hysteroscopic and laparoscopic surgery after failed antibiotics (6), and one 8 years after CS treated by hysterectomy (7). Defects have been described in the scar location after CS in 4.8% (8, 9) such as myometrial discontinuity at the site of a previous CS scar, including the production of mucus, blood, and the collection of menstrual product (10–12). Abnormal uterine bleeding and lower abdominal pain are observed in 46% of women with cesarean scar dehiscence (10). The risk increases with the number of CS and with a retroflexed uterus. The collection may get infected locally which would explain the finding of leukocytes and signs of necrosis in the endometrial biopsy. Ultrasonography, CT, and MRI are useful tools in evaluating the location, dimension, and etiology of a pelvic abscess (13). To this day, the only cases reported were managed surgically, mostly by hysterectomy. In our case, as the patient wished to preserve her fertility, we opted for conservative management with amoxicillin–clavulanic acid covering a wide selection of gynecological infections. We were successful and complete resolution of the abscess was achieved.
Close monitoring with ultrasound and MRI allowed us to continue managing this patient conservatively.
Conclusion
Cesarean section scar abscess after 10 years is a very rare complication. Symptoms seem to be related to the CS defect. To our knowledge, this is the first case describing successful conservative management leading to the complete resolution of symptoms and disappearance of radiological evidence. In our patient, pus and necrosis on endometrial biopsy oriented us toward local infection rather than a malignant process and the patient was systemically well and symptoms improved with treatment. This case shows that under these circumstances, surgery may be kept as a second-line option or can even be completely avoided.
Ethics Statement
Written informed consent was obtained from the patient prior to presenting the case.
Author Contributions
All authors listed, have made substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Declercq E, Young R, Cabral H, Ecker J. Is a rising cesarean delivery rate inevitable? Trends in industrialized countries, 1987 to 2007. Birth (2011) 38(2):99–104. doi:10.1111/j.1523-536X.2010.00459.x
2. Florio P, Filippeschi M, Moncini I, Marra E, Franchini M, Gubbini G. Hysteroscopic treatment of the cesarean-induced isthmocele in restoring infertility. Curr Opin Obstet Gynecol (2012) 24(3):180–6. doi:10.1097/GCO.0b013e3283521202
3. Barbut F, Carbonne B, Truchot F, Spielvogel C, Jannet D, Goderel I, et al. [Surgical site infections after cesarean section: results of a five-year prospective surveillance]. J Gynecol Obstet Biol Reprod (2004) 33(6 Pt 1):487–96. doi:10.1016/S0368-2315(04)96561-1
4. Dinsmoor MJ, Gilbert S, Landon MB, Rouse DJ, Spong CY, Varner MW, et al. Perioperative antibiotic prophylaxis for non-Laboring cesarean delivery. Obstet Gynecol (2009) 114(4):752. doi:10.1097/AOG.0b013e3181b8f28f
5. Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, et al. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol (2007) 21(2):98–113. doi:10.1111/j.1365-3016.2007.00786.x
6. Diaz-Garcia C, Estellés JG, Escrivá AM, Mora JJH, Torregrosa RR, Sancho JM. Scar abscess six years after cesarean section: laparoscopic and hysteroscopic management. J Minim Invasive Gynecol (2009) 16(6):785–8. doi:10.1016/j.jmig.2009.07.020
7. Taguchi T, Mabuchi S, Kimura T, Kimura T. Cesarean scar abscess: a case report and a review of the literature. Open J Obstet Gynecol (2012) 2(03):244. doi:10.4236/ojog.2012.23050
8. Wang CB, Chiu WWC, Lee CY, Sun YL, Lin YH, Tseng CJ. Cesarean scar defect: correlation between cesarean section number, defect size, clinical symptoms and uterine position. Ultrasound Obstet Gynecol (2009) 34(1):85–9. doi:10.1002/uog.6405
9. Bromley B, Pitcher B, Klapholz H, Lichter E, Benacerraf B. Sonographic appearance of uterine scar dehiscence. Int J Gynaecol Obstet (1995) 51(1):53–6. doi:10.1016/0020-7292(95)80009-2
10. Fabres C, Aviles G, De La Jara C, Escalona J, Muñoz JF, Mackenna A, et al. The cesarean delivery scar pouch clinical implications and diagnostic correlation between transvaginal sonography and hysteroscopy. J Ultrasound Med (2003) 22(7):695–700.
11. Chang Y, Tsai EM, Long CY, Lee CL, Kay N. Resectoscopic treatment combined with sonohysterographic evaluation of women with postmenstrual bleeding as a result of previous cesarean delivery scar defects. Am J Obstet Gynecol (2009) 200(4):370.e1–4. doi:10.1016/j.ajog.2008.11.038
12. Gubbini G, Casadio P, Marra E. Resectoscopic correction of the “isthmocele” in women with postmenstrual abnormal uterine bleeding and secondary infertility. J Minim Invasive Gynecol (2008) 15(2):172–5. doi:10.1016/j.jmig.2007.10.004
Keywords: scar abscess, cesarean-induced isthmocele, uterine discharge after cesarean
Citation: Boukrid M and Dubuisson J (2016) Conservative Management of a Scar Abscess formed in a Cesarean-induced Isthmocele. Front. Surg. 3:7. doi: 10.3389/fsurg.2016.00007
Received: 27 November 2015; Accepted: 22 January 2016;
Published: 16 February 2016
Edited by:
Issam Lebbi, Ob-Gyn and Fertility Private Clinic, Dream Center, TunisiaReviewed by:
Frank W. R. C. Vandekerckhove, Ghent University Hospital, BelgiumTanja Premru-Sršen, University Medical Center Ljubljana, Slovenia
Copyright: © 2016 Boukrid and Dubuisson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Meriem Boukrid, bWVyaWVtLmJvdWtyaWRAZ21haWwuY29t
 Meriem Boukrid
Meriem Boukrid Jean Dubuisson
Jean Dubuisson