
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Surg. , 21 October 2015
Sec. Visceral Surgery
Volume 2 - 2015 | https://doi.org/10.3389/fsurg.2015.00056
This article is part of the Research Topic Soft-tissue reconstruction using biologic tissue matrix: Where do we stand? View all 12 articles
The widespread use of meshes for hiatal hernia repair has emerged in the era of laparoscopic surgery, although sporadic cases of mesh augmentation of traumatic diaphragmatic rupture have been reported. The indications for biologic meshes in diaphragmatic repair are ill defined. This systematic review aims to investigate the available evidence on the role of biologic meshes in diaphragmatic rupture and hiatal hernia repair. Limited data from sporadic case reports and case series have demonstrated that repair of traumatic diaphragmatic rupture with biologic mesh is safe technique in both the acute or chronic setting. High level evidence demonstrates short-term benefits of biologic mesh augmentation in hiatal hernia repair over primary repair, although adequate long-term data are not currently available. Long-term follow-up data suggest no benefit of hiatal hernia repair using porcine small intestine submucosa over suture repair. The effectiveness of different biologic mesh materials on hernia recurrence requires further investigation.
Blunt or penetrating trauma of the abdomen and thorax may cause injury to the diaphragm (1). In the case of traumatic diaphragmatic rupture, abdominal organs such as the stomach, spleen, colon, or the liver may herniate into the thoracic cavity causing a wide range of symptoms, which may occur several years after the injury (2–5). Chest X-ray is often diagnostic, whereas computed tomography and magnetic resonance imaging provide detailed information about the herniated structures and the size of the defect (6, 7). There is no consensus on the absolute indications for surgery or the timing of surgical intervention. A traumatic rupture of the diaphragm is generally considered an indication for surgical repair, especially in the presence of symptoms.
Relevant literature evidence is limited, mainly due to the rarity of the condition. Primary suture repair or covering the defect with a synthetic mesh has been the standard of care during the past decades (8). Biologic meshes have been thought to be effective in closing the diaphragmatic defect, induce limited inflammatory response, and minimize adhesion formation.
In the presence of insufficient evidence, there is ongoing debate on the need of augmentation of the diaphragmatic hiatus during hernia repair (9). A number of randomized controlled trials (RCTs) and a meta-analysis have demonstrated lower recurrence rates after mesh repair; however, long-term data are not currently available (10). Several studies have reported complications, which has created skepticism with regard to the benefits of augmented hiatal hernia repair (11–13).Several biologic materials have been manufactured and are currently in use in surgical practice. Experimental data have shown biologic meshes to possess characteristics of an ideal mesh material, such as reduced adhesion formation, improved biocompatibility, decreased inflammatory response, and optimal neovascularization (14). Our objective was to review the evidence investigating the role of biologic meshes in traumatic repair of the diaphragm and in hiatal hernia repair.
Electronic searches of the Medline database were conducted using the PubMed search engine. The following combination of terms and keywords was applied: (trauma OR traumatic OR posttraumatic OR rupture*) AND (diaphragm* OR phren*) AND (mesh OR implant). The search returned 141 reports. The last search was run in November 2014. Titles and abstracts were interrogated and clinical reports on the use of biologic material for closure of traumatic diaphragmatic defects were selected. The full texts of 17 articles were assessed for eligibility; three relevant reports were identified (15–17). The remaining 15 articles were excluded because they reported on the use of synthetic materials in diaphragmatic rupture repair or did not provide relevant outcomes. A summary of the study characteristics and outcomes is presented in Table 1.
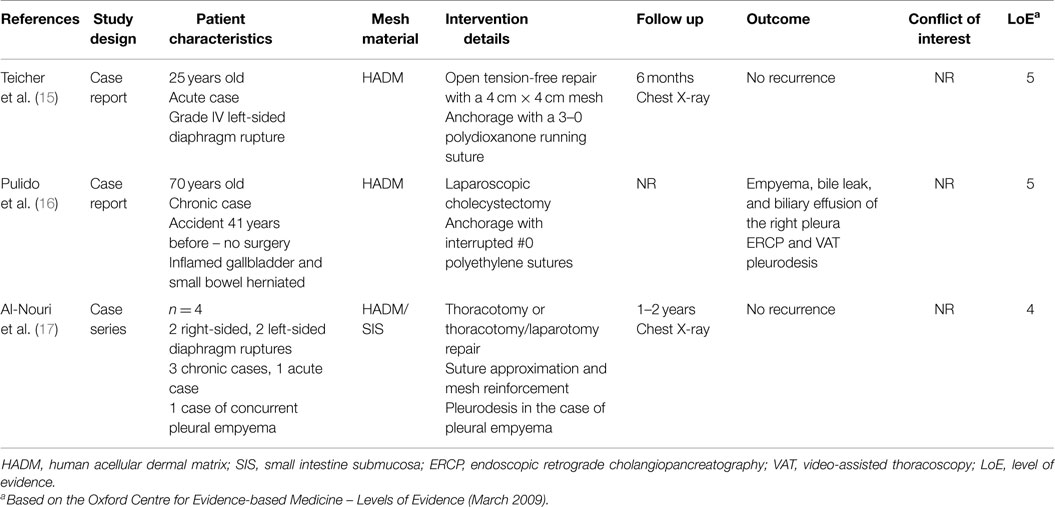
Table 1. Characteristics and outcomes of studies reporting on repair of traumatic diaphragmatic rupture with the use of biologic mesh.
Similarly, Medline was searched to identify relevant clinical evidence using the PubMed interface up to November 2014. The keywords (hiat*) AND (hernia) AND (mesh OR implant) were used. Of a total of 309 records, 28 articles were selected for full text review based on relevant information from titles and abstracts. Twenty-two articles provided relevant outcome data on mesh-reinforced hiatal hernia repair with biologic meshes (18–39). The study characteristics and outcomes are listed in Table 2.
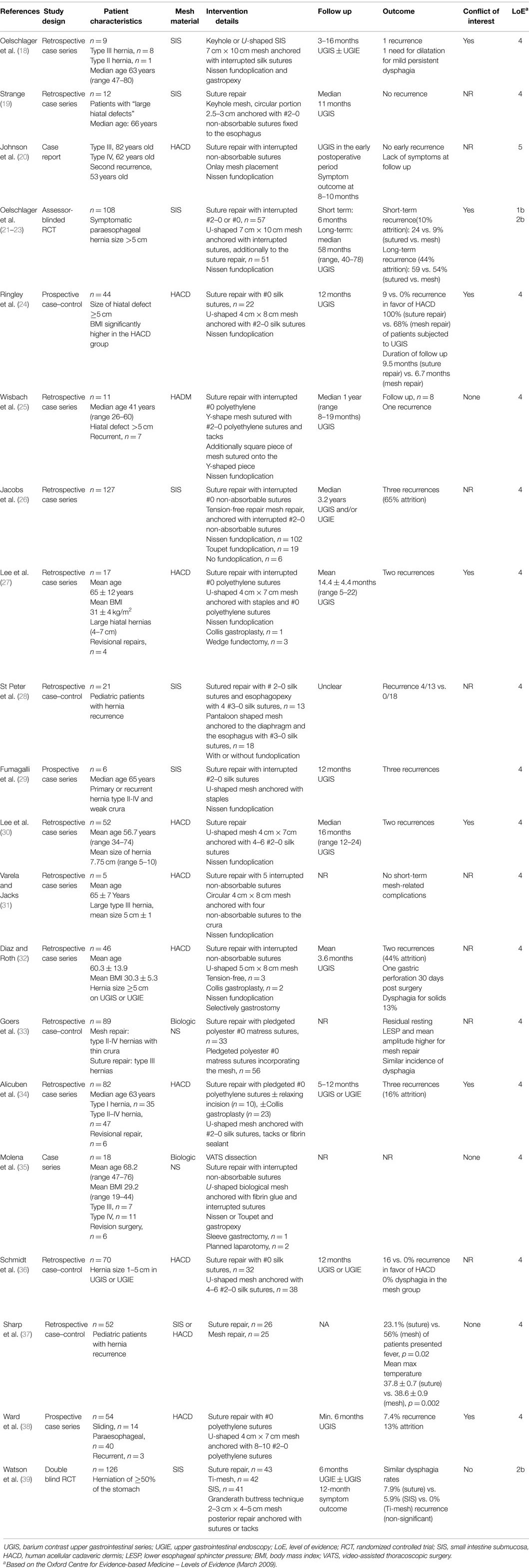
Table 2. Characteristics and outcomes of studies reporting on hiatal hernia repair with the use of biologic mesh.
Two case reports and one case series reported on the use of biologic meshes in traumatic diaphragmatic rupture. Four chronic traumatic defects and two acute ruptures were repaired laparoscopically, or with a laparotomy or a combined (thoracotomy and laparotomy) approach using human acellular cadaveric dermis (HACD) or porcine small intestine submucosa (SIS). Two of the repairs were performed in contaminated surgical fields, one due to inflammation of the herniated gallbladder and one due to pleural empyema. No septic complications requiring prolonged hospital stay or reintervention were reported. Chest X-ray in five of these cases did not reveal recurrence within a 6- to 24-month follow-up period.
A plethora studies reporting use of biologic mesh augmentation of the esophageal hiatus have been published since 2003. Most of these are retrospective industry-sponsored cohort studies. Both HACD and SIS meshes have been used, most commonly in a U-shape or a pantaloon fashion, placed in a retroesophageal position with the limbs of the mesh encircling the esophagus. The graft is anchored to the diaphragm and, in some cases, to the esophagus with non-absorbable sutures, tacks, or fibrin sealant, most commonly following suture repair of the crura or in a tension-free bridging fashion. A Collis gastroplasty has also been reported as a lengthening procedure in cases of a short esophagus (27, 32). Although no adverse effects associated with allografts or xenografts have been reported, in a chart review of 51 pediatric patients, Sharp and colleagues found that fever occurred more frequently after mesh repair and this group of subjects presented with a higher mean temperature during their hospital stay (37).
The best available evidence is provided by two well-designed RCTs (21–23, 39). In an industry-sponsored trial, Oelschlager and colleagues assigned 108 patients with paraesophageal hernia to receive either U-shaped SIS or suture repair. The authors found a significant reduction in the incidence of hernia recurrence (24 vs. 9%) at 6 months (21); however, long-term follow-up data (median 58 months, range 40–78) demonstrated no such benefit (22). Although this outcome may be biased by significant attrition (exceeding 20%), the reported recurrence rate for the mesh group remains unacceptably high.
In a recent double blind RCT that was sponsored by a national authority, suture mesh repair was compared with SIS or collagen-coated titanium mesh augmentation of the hiatus(39); similar recurrence rates at 6 months (7.9 vs. 5.9%, respectively) were found in the suture and biologic mesh repair groups, whereas no recurrence occurred in the synthetic mesh group. This finding, however, should be cautiously interpreted in the presence of wide confidence interval (95% confidence interval, 0.24–9.78). Long-term follow-up data of this trial are pending.
Most authors have focused their interest on potential beneficial effects of biologic grafts in paraesophageal hernia. In a cohort study, Schmidt and colleagues compared suture repair and mesh augmentation with HACD in small hernias (1–5 cm as assessed by barium upper gastrointestinal series or esophagogastroscopy) (36). A benefit of mesh repair was demonstrated, as indicated by a reduced recurrence rate (16 vs. 0%) at 1 year and improvement of symptoms of dysphagia.
Limited evidence exists investigating the role of biologic meshes in traumatic diaphragmatic repair. Low quality evidence (Level 4) suggests that this approach is feasible, at least in chronic cases. Biologic meshes have also been used in contaminated surgical fields with favorable results (Level 5). Because of the difficulties randomizing patients in the acute setting and the rarity of this condition, clinicians should be encouraged to publish their experience with biologic meshes in traumatic diaphragmatic rupture.
Level 1b data currently support lower recurrence rates for biologic mesh repair in the setting of paraesophageal hernia in the short term with conflicting evidence, whereas level 2b data support that this outcome benefit is lost in the long term. In a recent systematic review and meta-analysis of randomized and observational studies conducted by our research group, we found a beneficial short-term effect of mesh augmentation of the hiatus using biologic mesh (odds ratio 3.74, 95% confidence interval 0.92–8.98, p = 0.003) (40). However, no long-term outcome data were available for meta-analysis. Low quality data (level 4) suggest that patients with hiatal hernia measuring between 1 and 5 cm may benefit from biologic mesh augmentation. Nevertheless, cost-benefit assessment is lacking and the available evidence favoring biologic over synthetic meshes is insufficient.
The impact of type of biologic graft on hernia recurrence remains to be investigated. Further experimental and clinical research is required to assess new biologic implants in hiatal hernia repair. Although current data have shown SIS implants to be associated with high recurrence rates, other biologic materials have not been adequately investigated. Considering the rarity of cases with traumatic diaphragmatic defects, the effectiveness of biologic implants in such situations may be extrapolated from evidence derived from hiatal hernia repair. Future RCTs are required to investigate the role of biologic meshes in both paraesophageal and small hiatal hernias and evaluate their comparative efficacy to synthetic meshes.
Conception and design: SA, FK. Acquisition and interpretation of data: SA, FG, RP. Drafting the work or revision for important intellectual content: SA, FG, RP, FK. Final approval: SA, FG, RP, FK. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: SA, FG, RP, FK.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Morgan BS, Watcyn-Jones T, Garner JP. Traumatic diaphragmatic injury. J R Army Med Corps (2010) 156:139–44. doi: 10.1136/jramc-156-03-02
2. Disler DG, Deluca SA. Traumatic rupture of the diaphragm and herniation of the liver. Am Fam Physician (1992) 46:453–6.
3. Barbiera F, Nicastro N, Finazzo M, Lo Casto A, Runza G, Bartolotta TV, et al. The role of MRI in traumatic rupture of the diaphragm. Our experience in three cases and review of the literature. Radiol Med (2003) 105:188–94.
4. Zarzavadjian Le Bian A, Costi R, Smadja C. Delayed right-sided diaphragmatic rupture and laparoscopic repair with mesh fixation. Ann Thorac Cardiovasc Surg (2014) 20 Suppl:550–3. doi:10.5761/atcs.cr.12.02065
5. Matz A, Landau O, Alis M, Charuzi I, Kyzer S. The role of laparoscopy in the diagnosis and treatment of missed diaphragmatic rupture. Surg Endosc (2000) 14:537–9. doi:10.1007/s004640000362
6. Desir A, Ghaye B. CT of blunt diaphragmatic rupture. Radiographics (2012) 32:477–98. doi:10.1148/rg.322115082
7. Sliker CW. Imaging of diaphragm injuries. Radiol Clin North Am (2006) 44:199–211. doi:10.1016/j.rcl.2005.10.003
8. Haciibrahimoglu G, Solak O, Olcmen A, Bedirhan MA, Solmazer N, Gurses A. Management of traumatic diaphragmatic rupture. Surg Today (2004) 34:111–4. doi:10.1007/s00595-003-2662-8
9. Furnée E, Hazebroek E. Mesh in laparoscopic large hiatal hernia repair: a systematic review of the literature. Surg Endosc (2013) 27:3998–4008. doi:10.1007/s00464-013-3036-y
10. Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Lower recurrence rates after mesh-reinforced versus simple hiatal hernia repair: a meta-analysis of randomized trials. Surg Laparosc Endosc Percutan Tech (2012) 22:498–502. doi:10.1097/SLE.0b013e3182747ac2
11. Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ Jr, Michael Brunt L, Hunter JG, et al. Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc (2009) 23:1219–26. doi:10.1007/s00464-008-0205-5
12. Parker M, Bowers SP, Bray JM, Harris AS, Belli EV, Pfluke JM, et al. Hiatal mesh is associated with major resection at revisional operation. Surg Endosc (2010) 24:3095–101. doi:10.1007/s00464-010-1095-x
13. Antoniou SA, Koch OO, Antoniou GA, Pointner R, Granderath FA. Mesh-reinforced hiatal hernia repair: a review on the effect on postoperative dysphagia and recurrence. Langenbecks Arch Surg (2012) 397:19–27. doi:10.1007/s00423-011-0829-0
14. Antoniou SA, Pointner R, Granderath FA. Hiatal hernia repair with the use of biologic meshes: a literature review. Surg Laparosc Endosc Percutan Tech (2011) 21:1–9. doi:10.1097/SLE.0b013e31820ad56c
15. Teicher EJ, Madbak FG, Dangleben DA, Pasquale MD. Human acellular dermal matrix as a prosthesis for repair of a traumatic diaphragm rupture. Am Surg (2010) 76:231–2.
16. Pulido J, Reitz S, Gozdanovic S, Price P. Laparoscopic repair of chronic traumatic diaphragmatic hernia using biologic mesh with cholecystectomy for intrathoracic gallbladder. Int J Surg Case Rep (2012) 3:349–53. doi:10.4293/108680811X13176785204472
17. Al-Nouri O, Hartman B, Freedman R, Thomas C, Esposito T. Diaphragmatic rupture: is management with biological mesh feasible? JSLS (2011) 15:546–9. doi:10.1016/j.ijscr.2012.04.011
18. Oelschlager BK, Barreca M, Chang L, Pellegrini CA. The use of small intestine submucosa in the repair of paraesophageal hernias: initial observations of a new technique. Am J Surg (2003) 186:4–8. doi:10.1016/S0002-9610(03)00114-4
19. Strange PS. Small intestinal submucosa for laparoscopic repair of large paraesophageal hiatal hernias: a preliminary report. Surg Technol Int (2003) 11:141–3.
20. Johnson JM, Carmody BJ, Jamal MK, DeMaria EJ. Onlay hiatal reinforcement utilizing human acellular dermal matrix: three case series. Surg Innov (2005) 12:239–41. doi:10.1177/155335060501200309
21. Oelschlager BK, Pellegrini CA, Hunter J, Soper N, Brunt M, Sheppard B, et al. Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: a multicenter, prospective, randomized trial. Ann Surg (2006) 244:481–90. doi:10.1097/01.sla.0000237759.42831.03
22. Oelschlager BK, Pellegrini CA, Hunter JG, Brunt ML, Soper NJ, Sheppard BC, et al. Biologic prosthesis to prevent recurrence after laparoscopic paraesophageal hernia repair: long-term follow-up from a multicenter, prospective, randomized trial. J Am Coll Surg (2011) 213:461–8. doi:10.1016/j.jamcollsurg.2011.05.017
23. Oelschlager BK, Petersen RP, Brunt LM, Soper NJ, Sheppard BC, Mitsumori L, et al. Laparoscopic paraesophageal hernia repair: defining long-term clinical and anatomic outcomes. J Gastrointest Surg (2012) 16:453–9. doi:10.1007/s11605-011-1743-z
24. Ringley CD, Bochkarev V, Ahmed SI, Vitamvas ML, Oleynikov D. Laparoscopic hiatal hernia repair with human acellular dermal matrix patch: our initial experience. Am J Surg (2006) 192:767–72. doi:10.1016/j.amjsurg.2006.08.042
25. Wisbach G, Peterson T, Thoman D. Early results of the use of acellular dermal allograft in type III paraesophageal hernia repair. JSLS (2006) 10:184–7.
26. Jacobs M, Gomez E, Plasencia G, Lopez-Penalver C, Lujan H, Velarde D, et al. Use of surgisis mesh in laparoscopic repair of hiatal hernias. Surg Laparosc Endosc Percutan Tech (2007) 17:365–8. doi:10.1097/SLE.0b013e318123fc49
27. Lee E, Frisella MM, Matthews BD, Brunt LM. Evaluation of acellular human dermis reinforcement of the crural closure in patients with difficult hiatal hernias. Surg Endosc (2007) 21:641–5. doi:10.1007/s00464-006-9117-4
28. St Peter SD, Ostlie DJ, Holcomb GW III. The use of biosynthetic mesh to enhance hiatal repair at the time of redo Nissen fundoplication. J Pediatr Surg (2007) 42:1298–301. doi:10.1016/j.jpedsurg.2007.03.040
29. Fumagalli U, Bona S, Caputo M, Elmore U, Battafarano F, Pestalozza A, et al. Are surgisisbiomeshes effective in reducing recurrences after laparoscopic repair of large hiatal hernias? Surg Laparosc Endosc Percutan Tech (2008) 18:433–6. doi:10.1097/SLE.0b013e3181802ca7
30. Lee YK, James E, Bochkarev V, Vitamvas M, Oleynikov D. Long-term outcome of cruroplasty reinforcement with human acellular dermal matrix in large paraesophageal hiatal hernia. J Gastrointest Surg (2008) 12:811–5. doi:10.1007/s11605-007-0463-x
31. Varela JE, Jacks SP. Laparoscopic circular biomeshhiatoplasty during paraesophageal hernia repair. Surg Innov (2009) 16:124–8. doi:10.1177/1553350609336420
32. Diaz DF, Roth JS. Laparoscopic paraesophageal hernia repair with acellulardermal matrix cruroplasty. JSLS (2011) 15:355–60. doi:10.4293/108680811X13125733356594
33. Goers TA, Cassera MA, Dunst CM, Swanström LL. Paraesophageal hernia repair with biomesh does not increase postoperative dysphagia. J Gastrointest Surg (2011) 15:1743–9. doi:10.1007/s11605-011-1596-5
34. Alicuben ET, Worrell SG, DeMeester SR. Impact of crural relaxing incisions, collis gastroplasty, and non-cross-linked human dermal mesh crural reinforcement on early hiatal hernia recurrence rates. J Am Coll Surg (2014) 219:988–92. doi:10.1016/j.jamcollsurg.2014.07.937
35. Molena D, Mungo B, Stem M, Lidor AO. Novel combined VATS/laparoscopic approach for giant and complicated paraesophageal hernia repair: description of technique and early results. Surg Endosc (2015) 29:185–91. doi:10.1007/s00464-014-3662-z
36. Schmidt E, Shaligram A, Reynoso JF, Kothari V, Oleynikov D. Hiatal hernia repair with biologic mesh reinforcement reduces recurrence rate in small hiatal hernias. Dis Esophagus (2014) 27:13–7. doi:10.1111/dote.12042
37. Sharp NE, Alemayehu H, Desai A, Holcomb GW III, St Peter SD. Fever after redo Nissen fundoplication with hiatal hernia repair. J Surg Res (2014) 190:594–7. doi:10.1016/j.jss.2014.05.021
38. Ward KC, Costello KP, Baalman S, Pierce RA, Deeken CR, Frisella MM, et al. Effect of acellular human dermis buttress on laparoscopic hiatal hernia repair. Surg Endosc (2015) 29:2291–7. doi:10.1007/s00464-014-3946-3
39. Watson DI, Thompson SK, Devitt PG, Smith L, Woods SD, Aly A, et al. Laparoscopic repair of very large hiatus hernia with sutures versus absorbable mesh versus nonabsorbable mesh: a randomized controlled trial. Ann Surg (2015) 261:282–9. doi:10.1097/SLA.0000000000000842
40. Antoniou SA, Müller-Stich BP, Antoniou GA, Köhler G, Luketina RR, Koch OO, et al. Laparoscopic augmentation of the diaphragmatic hiatus with biologic mesh versus suture repair: a systematic review and meta-analysis. Langenbecks Arch Surg (2015) 400:577–83. doi:10.1007/s00423-015-1312-0
Ferdinand Köckerling (Chairman), Stavros A. Antoniou, René Fortelny, Frank A. Granderath, Markus Heiss, Franz Mayer, Marc Miserez, Agneta Montgomery, Salvador Morales-Conde, Filip Muysoms, Alexander Petter-Puchner, Rudolph Pointner, Neil Smart, MarciejSmietanski, Bernd Stechemesser undertaken by the BioMesh Study Group.
The BioMesh Study Group has set itself the task of identifying how best to use biological meshes for the various indications. The first step toward achieving that goal is to compile systematic reviews of the different indications on the basis of the existing literature. The available literature sources will be evaluated in accordance with the Oxford Centre for Evidence-based Medicine-Levels of Evidence (March 2009). Next, based on the review findings corresponding Statements and Recommendations are to be formulated in a Consensus Conference for the use of biological meshes for the different indications. The findings of the Consensus Conference are then to be summarized for a joint publication. This present publication is part of the project undertaken by the BioMesh Study Group.
Keywords: biologic mesh, biologic graft, hiatal hernia, diaphragmatic rupture, paraesophageal hernia, fundoplication
Citation: Antoniou SA, Pointner R, Granderath F-A and Köckerling F (2015) The use of biological meshes in diaphragmatic defects – an evidence-based review of the literature. Front. Surg. 2:56. doi: 10.3389/fsurg.2015.00056
Received: 05 August 2015; Accepted: 08 October 2015;
Published: 21 October 2015
Edited by:
Vincenzo Neri, University of Foggia, ItalyReviewed by:
Kun-Ming Chan, Chang Gung Memorial Hospital at Linkou, TaiwanCopyright: © 2015 Antoniou, Pointner, Granderath and Köckerling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Stavros A. Antoniou, c3RhdnJvcy5hbnRvbmlvdUBob3RtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.