- 1Department of Health Services Research, Management and Policy, College of Public Health and Health Professions, University of Florida, Gainesville, FL, United States
- 2Department of Speech, Language and Hearing Sciences, Communication Equity and Outcomes Laboratory, College of Public Health and Health Professions, University of Florida, Gainesville, FL, United States
Introduction: Aphasia, a communication disorder often resulting from stroke, can have profound impacts on both health outcomes and financial wellbeing. While the physical and cognitive consequences of stroke are well documented, the financial strain, or “financial toxicity,” associated with managing chronic conditions like aphasia remains underexplored. Furthermore, financial toxicity is not experienced equally across racial and ethnic groups, with disparities driven by socioeconomic factors, access to healthcare, and structural inequities. This study compares the financial toxicity of people with aphasia (PWA) to those with stroke alone, examining differences across racial and ethnic groups to highlight disparities in economic burden.
Methods: This study utilized data from the Medical Expenditure Panel Survey (MEPS) collected between 2018 and 2021 to examine the financial toxicity of PWA compared to those with stroke only. Financial toxicity was assessed using self-reported income and wealth data from the MEPS. Individual-level income and wealth values were calculated from the self-reported financial data to quantify the financial burden. Fixed effects regression models were employed to account for unobserved individual heterogeneity, controlling for time-invariant characteristics. Interaction terms were included in the models to capture the differential financial impacts of aphasia on Black and Hispanic individuals, compared to other racial and ethnic groups. The analysis examined both within-group and between-group differences in financial toxicity, highlighting potential racial and ethnic disparities among those affected by aphasia.
Results: Approximately 18.71% (N = 281) of respondents who reported having a stroke also had aphasia. After controlling for demographic, health, and household characteristics, PWA had 21% lower income and 7% lower wealth compared to stroke survivors without aphasia. Aphasia had a disparate impact on the income (−29%) and wealth (−24%) of Black stroke survivors. These findings were consistent across different model specifications, highlighting the robustness of the results indicating racial inequity in the financial toxicity of post-stroke aphasia.
Conclusion: This study showed the financial impact of post-stroke aphasia and the disparate burden among Black PWA. The findings highlight the need to address the financial ramifications of post-stroke morbidities such as aphasia among vulnerable populations.
Introduction
Aphasia is a communication disorder characterized by impairment of language that can negatively impact both speech and comprehension abilities as well as the ability to read or write (National Aphasia Association, 2024a). According to the National Aphasia Association, ~2 million Americans have aphasia and ~180,000 individuals acquire the communication disorder each year (National Aphasia Association, 2024b). Even in its mildest form, aphasia can cause significant disruption in communication ability (Armstrong et al., 2013). People with aphasia (PWA) have an increased risk of depression, fatigue, anxiety, and insomnia when compared to stroke survivors without the condition (Hersh et al., 2024). PWA also report loneliness (Hersh et al., 2024), loss of friendships (Archer et al., 2024; Madden et al., 2023), disruptions and dissatisfaction with healthcare experiences (Carragher et al., 2024; Tomkins et al., 2013), reduced social participation (Quique et al., 2023), and reductions in their quality of life (Filipska-Blejder et al., 2023).
Although substantial research related to the communication challenges of PWA (Poirier et al., 2024) and their loved ones (McGurk and Kneebone, 2013) exists, there has been virtually no research examining the financial problems that PWA face and the additive burden of the condition. Although recent estimates suggest that the annual cost of aphasia is $15.8 billion annually, or $30,599.78 per PWA, as related to medical/healthcare expenditures, lost wages, and informal caregiving (Jacobs and Ellis, 2023), virtually nothing is known about the specific factors that contribute to the “financial toxicity” of having aphasia. Financial toxicity refers to the “toxic effects” that a health condition can have on the financial resources of individuals with a health condition (Pisu and Martin, 2022). Financial toxicity is the result of the cumulative expenses associated with receiving medical care. Estimates suggest that 56% of US adults experience financial toxicity and have unavoidable medical expenses, even though many have insurance coverage (Yabroff et al., 2019).
Financial toxicity among PWA is potentially a devastating problem because of the nature of the communication disorder and the impact that it has on the PWA who are also recovering from stroke. For example, stroke itself is a condition that frequently requires long-term, organized, and high-cost care (Sarzyńska-Długosz, 2023). Communication issues such as aphasia that arise post-stroke are frequently one of the multiple potential problems that stroke survivors experience. Yet the burden is greater among individuals with communication issues because of the greater likelihood of disrupted healthcare access, utilization, and satisfaction over and above the experiences of stroke survivors without aphasia (Cummings, 2023). Some PWA are left with unmet needs that are linked to poor patient–provider communication due to aphasia (Anemaat et al., 2024). Therefore, understanding the issue of financial toxicity among stroke subpopulations (i.e., those with aphasia) is critically important to the determination of the multiple factors that drive stroke- and aphasia-related outcomes and the need for tailored interventions designed to optimize these outcomes. This study was designed to explore financial toxicity among PWA to profile financial toxicity among PWA and determine the sociodemographic factors that contribute to greater financial toxicity in this population compared to those individuals without aphasia.
Materials and methods
Data
This panel data study used longitudinal data from the Medical Expenditure Panel Study (MEPS) collected between 2018 and 2021 (Agency for Healthcare Research Quality, 2023). The sample was restricted to adults aged 18 years and above. The MEPS data provide nationally representative estimates of healthcare use, expenditures, sources of payment, and health insurance coverage for the US civilian non-institutionalized population (Agency for Healthcare Research Quality, 2023). The MEPS Household Component (HC) also provides estimates of respondents' health status, demographic and socioeconomic characteristics, employment, access to care, and satisfaction with healthcare. The panel design of the survey includes rounds of interviews covering four full calendar years, allowing for analysis of person-level changes in selected variables such as expenditures, health insurance coverage, and health status.
The Panel 23 Four-Year Longitudinal Data File from the MEPS Household Component (MEPS-HC) (Agency For Healthcare Research Quality, 2012) provided data collected on a nationally representative sample of the civilian non-institutionalized population of the United States for the 4-year period 2018–2021. This dataset includes records for 7,080 persons in Panel 23 who were respondents during the period they were in-scope for the survey (i.e., part of the civilian non-institutionalized population) over the 4-year period. Only persons with positive person-level weights (PERWT18F, PERWT19F, PERWT20F, or PERWT21F) are included in the longitudinal Public Use Files (PUF) data. Data are available for all nine rounds for 87.46% of the cases (6,192 persons). The remaining 12.54% (888 persons) did not have data for one or more rounds but were in-scope for all rounds in which they participated in the survey. These persons are those who were born, died, were in the military or an institution, or who left the country during the 4-year period. In contrast, persons in the panel who participated in the survey for only part of the period they were in-scope are not included in this file. Variables in the file pertaining to survey administration, demographics, employment, health status, disability days, quality of care, patient satisfaction, health insurance, and medical care use and expenditures were obtained from the MEPS 2018, 2019, 2020, and 2021 Full-Year Consolidated Files (HC-209, HC-216, HC-224, and HC-233, respectively).
Sample
In each year of the panel, respondents indicated whether they had ever been told by a doctor or other health professionals that they had a stroke. To identify those with post-stroke aphasia, the subset of individuals who reported a prior stroke diagnosis in the Panel 23 Four-Year Longitudinal Data File were merged with the 2018 (HC-231), 2019 (HC-222), 2020 (HC-214), and 2021 (HC-207) MEPS Medical Condition files using individual-specific surrogate identifiers. These files contain household-reported medical conditions from a nationally representative sample in the calendar year. Each record represents one current medical condition reported during the respective data collection period. Reported conditions were reported by interviewers using a condition picklist with the International Classification of Diseases, Medical Classification, 10th Revision (ICD-10-CM) codes already assigned to conditions in the list. To preserve confidentiality, all the conditions in the file were grouped into three-digit diagnosis code categories, rather than using the fully specified ICD-10-CM codes. Codes R47 and I69 indicated a stroke survivor with aphasia.
This study was granted exempt status by the University of Florida Institutional Review Board (IRB) as it does not involve human subjects. Similarly, informed consent was not obtained because the study involved the secondary analysis of existing data.
Financial outcomes
Two financial indicators were created—income and wealth—consistent with the methodology used by Bernard et al. (2009). Conceptually, income was considered the money an individual earns in a calendar year, while wealth was the value of a person's assets minus their debts. Income was calculated as money received during the current calendar year from Individual Retirement Accounts (IRAs), Keogh Accounts, or 401Ks; private pensions, military retirement, other federal government employee pensions, state or local government employee pensions, or annuities; Social Security and equivalent tier 1 Railroad Retirement benefits; wages or salary, tips, commissions, or bonuses; business or practice; unemployment compensation; veterans payments; workers compensation; Supplemental Security Income (SSI); and public assistance payments. Wealth included net income as well as the total net gain or loss from alimony; dividends; cash contributions received from non-household members such as gifts or sporadic payments; interest income from savings accounts, bonds, NOW accounts, money market accounts, or similar types of investments; the sale of property or other assets including home(s); estates, trusts, partnerships, S corporations, rent, and royalties; and other sources specified elsewhere.
Individual characteristics
The variables used in this analysis are described below. For categorical variables, “*” denotes the reference group.
Individuals' characteristics included sex (male*, female), region of geographic residence (Northeast*, Midwest, South, West), age in years (<65*, ≥65), household size (1–2*, ≥3), education (less than high school/high school, beyond a high school education*), Black race (Black, non-Black*), and Hispanic ethnicity (Hispanic, non-Hispanic*). Race and ethnicity were self-reported by respondents. MEPS respondents provided information about their insurance status and type of coverage, which was then categorized into two groups: private health insurance and non-private health insurance*.
An indicator for employment status was created using two survey items. First, respondents reported weekly hours worked at their current main job (CMJ) in each round. Those reporting working more than zero hours at their CMJ were considered employed. To validate this classification schema, responses were compared to reported reasons for not working in the same round. This comparison ensured that indicators of employment captured financially compensated market work rather than part-time student or retirement jobs.
Comorbid disease burden was captured using the Grouped Charlson Comorbidity Index (CCI), which has been used frequently in studies involving the MEPS data (de Groot et al., 2004; Salami et al., 2018; Charlson et al., 1987). For this analysis, however, the CCI excluded stroke to avoid collinearity in regression analyses. Two categories of the CCI included zero or one comorbidity* and two or more comorbidities. Finally, to account for differences in healthcare utilization and spending, total healthcare expenditure—defined as the sum of direct payments for care provided during the year, including out-of-pocket payments and payments by private insurance, Medicaid, Medicare, and other sources—was included as a dichotomous variable indicating an annual healthcare expenditure in the top 30% of the annual distribution. This variable was referred to as “high healthcare costs.”
Statistical analysis
This analysis evaluated the association between income, wealth, and aphasia among stroke survivors accounting for the differential financial implications of age, employment, and health insurance. This approach integrates the distinct financial mechanisms and safety nets, such as retirement income or disability benefits, that shape the experience of financial toxicity following a stroke. Wealth and income were adjusted for inflation to 2024 dollars and natural-logged because of their skewed distribution, and separate regression models were specified to avoid concerns of collinearity and heteroskedasticity (Equation 1).
Outcomeit was the outcome variable (income or wealth) in the logarithmic form to be estimated of individual i in year t. Aphasiait was the primary explanatory variable assuming a value of 1 for diagnosis of aphasia and 0 otherwise*. Residential sampling units and year-fixed effects were denoted by μi and τt, and εit is the error term. The remaining covariates indicated characteristics of individual i in year t. As suggested by the MEPS, all analyses utilized survey-specific commands. These commands allowed for the incorporation of survey weights, the inclusion of multiple waves, and the identification of survey-specific parameters that account for the complex survey design and sampling framework. Using the survey parameters and sampling weights correctly estimated standard errors and generated findings that reflect the national population.
First, descriptive statistics for the “aphasia” and “no aphasia” samples were calculated. The F-tests tested for statistically significant differences in characteristics between groups. Next, the fixed effects (FE) regression models evaluated the association between income/wealth (modeled separately), aphasia diagnosis, and individual characteristics. The FE regression modeled individual-level income/wealth changes throughout the panel while controlling for unobserved time-invariant individual heterogeneity that remained constant within the study period. This approach has been used extensively in similar studies and is regarded as statistically robust and conservative (Babiarz and Yilmazer, 2017; Jeon and Pohl, 2017; Gaspar et al., 2021). The results can be interpreted as the relationship between annual changes in income/wealth and the regressors. Significant interaction terms between Black race and Hispanic ethnicity and aphasia indicated between group differences in the association between income/wealth and race/ethnicity.
To test the robustness of the FE analyses, two-part “Heckman-style” models were estimated. The two-part specification accounted for the skewed nature of income and wealth distributions. Two-part models are frequently used when estimating earnings functions to account for the portion of the sample who have no earnings within a given period. In the first stage, a probit model estimated the probability that the outcome was greater than zero conditional on covariates. For those observations with non-zero outcome values, the second stage estimated the outcome conditional on the covariates.
Results
Sample characteristics
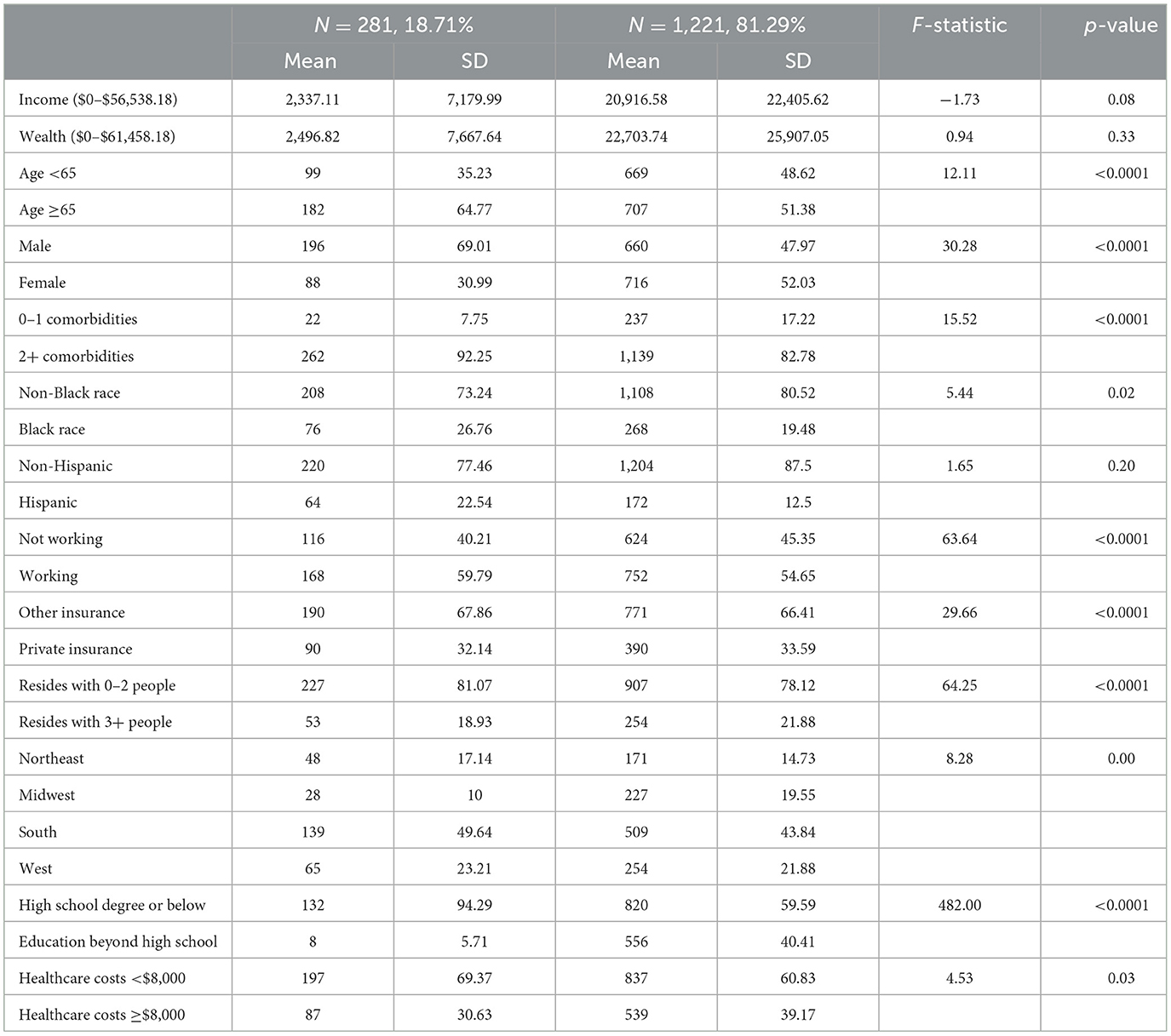
Table 1 describes the characteristics of both PWA and those without aphasia. Approximately 35% of the PWA were below the age of 65 compared to 49% of those without aphasia (F = 12.11, p < 0.0001). Nearly 70% of PWA were male compared to only 48% of those without aphasia (F = 30.28, p < 0.0001). Over 90% of PWA had two or more comorbidities compared to only 80% of those without aphasia (F = 15.52, p < 0.0001). More than 25% of PWA were Black and 23% were Hispanic compared to only 19% and 13% of those without aphasia (Black F = 5.11, p = 0.02; Hispanic F = 165, p = 0.20). Nearly 60% of PWA were employed and 32% of PWA had private health insurance compared to 55% and 34%, respectively, of those without aphasia (working F = 63.61, p < 0.00021; private insurance F = 29.66, p < 0.0001). Among PWA, 19% lived with three or more individuals and 23% resided in the South (of those without aphasia 22% resided with 3+ individuals, F = 64.25, p < 0.0001; 22% resided in the South, F = 8.28, p = 0.00). Only 6% of PWA had education beyond a high school degree compared to 40% of those without aphasia (F = 82.00, p < 0.0001). However, 40% of those without aphasia had high healthcare costs compared to 31% of PWA (F = 4.53, p = 0.03).
Regression results
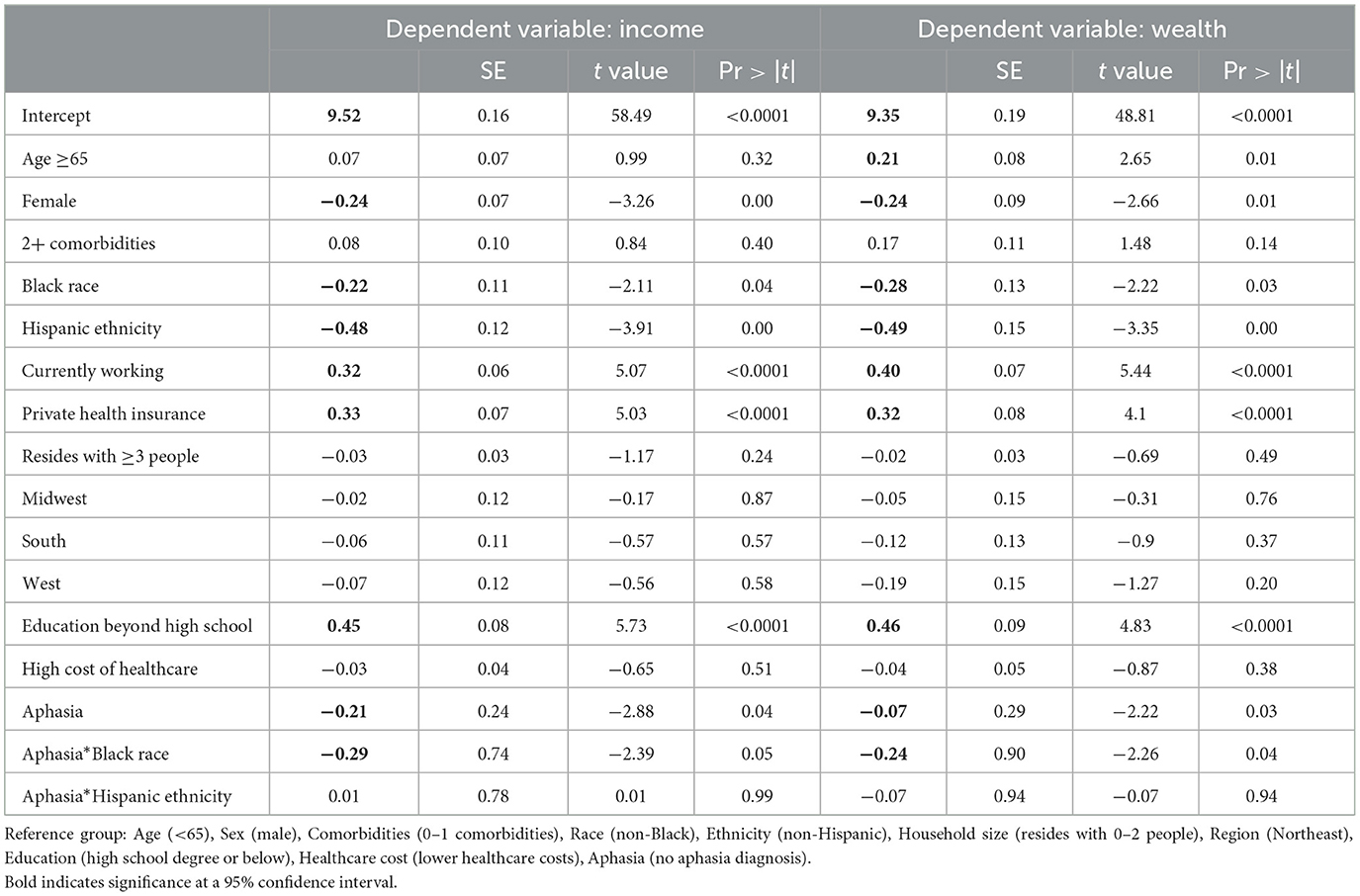
Table 2 shows the FE regression results for income and wealth for all stroke survivors (for PWA and those without aphasia). The results indicated that, relative to men, women have 24% (SE = 0.07) lower income and 24% (SE = 0.01) lower wealth. Relative to their counterparts, respondents with educational attainment of a high school degree or beyond (income 45%, SE = 0.08; wealth 46%, SE = 0.09), private insurance (income 33%, SE = 0.07; wealth 32%, SE = 0.08), and who were employed (income 32%, SE = 0.06; wealth 40%, SE = 0.07) had higher income and wealth. Compared to non-Black individuals, Black PWA had significantly lower income (−22%, SE = 0.11) and wealth (−28%, SE = 0.13). Similarly, compared to non-Hispanic individuals, Hispanic individuals had lower income (−48%, SE = 0.12) and wealth (−49%, SE = 0.15). The presence of aphasia was associated with 21% (SE = 0.24) lower income and 7% (SE = 0.29) lower wealth compared to stroke survivors without aphasia. Compared to Black stroke survivors without aphasia, Black PWA had 29% (SE = 0.74) lower income and 24% (SE = 0.90) lower wealth even after controlling for age, employment, educational, and residential heterogeneity.
Robustness test
Table 3 shows the regression results for the two-stage estimation models for income and wealth. The results mirror the findings discussed above. On average, Black stroke survivors had 26% (95% CI = −0.42, −0.10) lower income and 34% (95% CI = −0.54, −0.15) lower wealth compared to non-Black stroke survivors and Hispanic stroke survivors had 55% (95% CI = −0.81, −0.30) lower income and 53% (95% CI = −0.81, −0.25) lower wealth than non-Hispanic stroke survivors. The estimates showed the PWA had 71% (95% CI = −0.83, −0.20) lower income and 54% lower wealth (95% CI = −0.67, −0.35) compared to stroke survivors without aphasia. However, Black PWA had 31% (95% CI = −0.83, −0.20) lower income and 46% (95% CI = −0.67, −0.35) lower wealth than their counterparts without aphasia.
Discussion
The key finding of this study was that communication disability (aphasia) resulted in lower incomes and wealth. Additionally, Black PWA saw the greatest decreases in income and wealth. More specifically, the presence of aphasia resulted in a 21% decrease in income and a 7% decrease in wealth for PWA, yet Black PWA experienced decreases of 29% in income and 24% in wealth. We believe the distinction between income and wealth is important given that after the age of 65 income and wealth can differ substantially as individuals transition from earned income to fixed income. Consequently, the financing of healthcare for chronic conditions such as stroke becomes more difficult (Park and Stimpson, 2024). Furthermore, the impact of being Black and having a post-stroke communication disorder such as aphasia further magnifies the complexity of the income and wealth problem. We consider these collective issues in the context of known income and wealth disparities that exist among racial and ethnic minorities and individuals with communication issues such as aphasia.
Race and income–wealth disparities among individuals with disabilities
Income and wealth disparities among individuals with disabilities have been previously reported (Jajtner et al., 2020). Households with adult members with a disability are two times more likely to live under the federal poverty line, have a higher liquid asset poverty rate, and earn more than $33,000 less than households without a disability (Prosperity Now, 2018). Individuals with disabilities frequently experience disadvantages related to employment, and subsequently are susceptible to economic vulnerability (Jajtner et al., 2020). Consequently, individuals with disability experience a “disability penalty” or disadvantage that further reduces their likelihood of employment and income and long-term wealth accumulation (Willson et al., 2024).
Income and wealth disparities are further impacted by racial and ethnic background. The National Disability Institute Report titled “Financial Inequality: Disability, Race, and Poverty in America” (Goodman et al., 2019) showed that racial and ethnic minorities and people with disabilities face barriers that limit their earning potential. The report notes a dynamic interaction between disability, race, and poverty (Goodman et al., 2019). More specifically, individuals from racial and ethnic minority groups are more likely to have a disability during working age compared to white Americans. Given the complex relationship between race and disability, many of these individuals experience higher healthcare costs while simultaneously being disadvantaged by their inability to work or earn equitable incomes (Goodman et al., 2019). The authors argue that disability is a cause and consequence of poverty while, at the same time, disability reinforces poverty (Goodman et al., 2019, p. 5). Even after adjusting for educational level, individuals from racial and ethnic minorities with disabilities are more likely to live in poverty than other disability groups. Ultimately, the authors conclude that race and disability are not completely different sources of disadvantage but are more likely to parallel one another (Goodman et al., 2019).
Income–wealth disparities among individuals with communication disabilities
Whereas the intersection of race and disability translates into lower income and wealth, understanding the type of disability is equally important. Evidence suggests that individuals with communication disabilities in general experience economic disadvantage (unemployment and lower income) and are more commonly represented in low socioeconomic groups (Jagoe et al., 2021). Many workplaces require good communication, and those with disabilities are more frequently under-employed, unemployed, or lack ideal workplace integration (Garcia et al., 2002).
Regarding aphasia specifically, PWA often experience significant difficulty returning to work, and only a small percentage are successful in returning to their pre-aphasia jobs (Gilmore et al., 2022; Burfein et al., 2024; Pike et al., 2017). A recent review highlighted a range of factors that contribute to greater success in returning to work, including personal factors (aphasia severity, motivation, and fatigue), rehabilitation factors (access to vocational rehabilitation), and workplace factors (employer engagement in supported and job adaptations) (Gilmore et al., 2022). At the same time, PWA frequently experience reintegration challenges, which can be influenced by their perceived value in the workplace and the support they receive from others (Pike et al., 2017). Others are limited by linguistic profiling or “when judgments about the identity or subgroup based on auditory cues or speech characteristics” are made, which reduces their likelihood of re-engaging in the workforce (Caldwell et al., 2024; Baugh, 2000). Finally, it is unclear how individuals with communication disorders are aware that the Americans with Disabilities Act of 2008 expanded the definition of disability to include “speaking, hearing, and communicating,” and has therefore given them the protection of the law that precludes employers from asking about the presence of a communication disorder (Isetti and Eadie, 2016; Equal Employment Opportunity Commission, 2013). Clearly, some individuals are precluded from returning to work based on the severity of their aphasia, and therefore the presence of communication disorders is a major contributor to income and wealth inequities that many individuals with aphasia and other communication disorders experience.
Limitations
Although this study provides valuable insights, it is subject to several limitations. First, the MEPS contains no information on the type of stroke or whether this was the first stroke or a recurrent stroke. Second, the MEPS does not contain any information about the type of acute stroke care received or any post-stroke rehabilitation services. Furthermore, these data do not allow for the identification of any morbidities, deficits, or physical symptoms other than aphasia that resulted from a stroke. Third, the racial and ethnic disparities in aphasia-related financial toxicity may be related to differences in the timing and/or quality of rehabilitation care received by different racial and ethnic groups; however, these data do not permit an assessment of these differences. Although the MEPS incorporates the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) to measure the perceived quality of care, these subjective measures only cover the last 12 months and do not specifically address stroke care. Fourth, although the data identifies respondents who died during the panel, it does not specify the cause of death, which may affect the interpretation of the financial impacts related to stroke by resulting in censoring observations. However, a sensitivity analysis indicated that excluding deceased individuals from the study did not meaningfully alter the results. Fifth, this study relies on the MEPS data, which categorizes gender as either “male” or “female.” This binary classification does not capture non-binary or gender-diverse identities, potentially excluding populations that may experience unique healthcare challenges and financial toxicity. This limitation restricts the study's ability to generalize findings across the full spectrum of gender identities. Future research should consider incorporating more inclusive gender data to ensure a better understanding of stroke-related financial toxicity among all individuals. The lack of granularity in the data limits our ability to discern and discuss the nuanced differences that might exist within these broad categories, potentially obscuring specific factors that contribute to financial toxicity. Future studies should aim to collect and analyze data that distinguish across diverse communities. Additionally, incomplete and inaccurate sex, race, or ethnic data may limit the ability to understand the sources of disparities in healthcare costs, quality, and outcomes. Finally, the use of self-reported financial data may introduce reporting bias. While FE models control for unobserved heterogeneity, they cannot account for time-varying factors that might influence financial outcomes or fully investigate the specific mechanisms underlying these observed disparities.
Conclusion
In conclusion, this study sheds light on the substantial financial burdens experienced by stroke survivors with aphasia, highlighting how communication disabilities potentially exacerbate the financial toxicity already present in stroke recovery. The findings underscore significant disparities in income and wealth between PWA and those without, particularly among racial and ethnic minorities, with Black PWA facing disproportionately greater financial challenges. These disparities emphasize the compounded disadvantage that individuals with both a communication disorder and a minority racial background endure, further complicating their ability to achieve financial stability. The study provides critical insight into the factors contributing to financial toxicity, such as reduced access to employment and the high costs of healthcare, which are particularly pronounced among those with aphasia.
These findings indicate a need for targeted interventions that address both the healthcare and financial needs of PWA. Policymakers and healthcare providers should consider the development of rehabilitation programs and job re-entry initiatives tailored to individuals with communication disabilities. Additionally, addressing racial disparities in healthcare access and post-stroke care is imperative to reduce the financial strain faced by minority groups. Future research should continue to explore the intersection of race, disability, and financial toxicity, with an emphasis on improving rehabilitation support, access to care, and economic outcomes for stroke survivors with aphasia. Such efforts will help ensure that all individuals, regardless of their communication abilities or racial background, have equitable opportunities for financial recovery and stability.
Data availability statement
Publicly available datasets were analyzed in this study. This study utilized Panel 23 Four-Year Longitudinal Data File (available at: https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=All&cboDataTypeY=1%2CHousehold+Full+Year+File&buttonYearandDataType=Search&cboPufNumber=All&SearchTitle=Longitudinal) and the HC 231, HC 222, HC 214, and HC 207 Medical Condition files (available at: https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_results.jsp?cboDataYear=All&cboDataTypeY=1%2CHousehold+Full+Year+File&buttonYearandDataType=Search&cboPufNumber=All&SearchTitle=Medical+Conditions).
Ethics statement
The studies involving humans were approved by University of Florida Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
MJ: Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing – original draft, Writing – review & editing. CE: Conceptualization, Investigation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Agency for Healthcare Research and Quality (2023). MEPS Panel 23 Four-Year Longitudinal Data File. MEPS HC-236. Available at: https://meps.ahrq.gov/mepsweb/data_stats/download_data_files_detail.jsp?cboPufNumber=HC-236 (accessed September 6, 2024).
Anemaat, L. N., Palmer, V. J., Copland, D. A., Binge, G., Druery, K., Druery, J., et al. (2024). Understanding experiences, unmet needs and priorities related to post-stroke aphasia care: stage one of an experience-based co-design project. BMJ Open 14:e081680. doi: 10.1136/bmjopen-2023-081680
Archer, B., Azios, J. H., Douglas, N. F., Strong, K. A., Worrall, L., Simmons-Mackie, N., et al. (2024). “I Could Not Talk. She Did Everything She's Now My Sister”: people with aphasia's perspectives on friends who stuck around. Am. J. Speech Lang. Pathol. 33, 349–368. doi: 10.1044/2023_AJSLP-23-00205
Armstrong, E., Fox, S., and Wilkinson, R. (2013). Mild aphasia: is this the place for an argument? Am. J. Speech Lang. Pathol. 22, S268–278. doi: 10.1044/1058-0360(2012/12-0084)
Babiarz, P., and Yilmazer, T. (2017). The impact of adverse health events on consumption: understanding the mediating effect of income transfers, wealth, and health insurance. Health Econ. 26, 1743–1758. doi: 10.1002/hec.3496
Baugh, J. (2000). Racial identification by speech. Am Speech. 75, 362–364. doi: 10.1215/00031283-75-4-362
Bernard, D. M., Banthin, J. S., and Encinosa, W. E. (2009). Wealth, income, and the affordability of health insurance. Health Aff. 28, 887–896. doi: 10.1377/hlthaff.28.3.887
Burfein, P., Roxbury, T., Doig, E. J., McSween, M. P., de Silva, N., Copland, D. A., et al. (2024). Return to work for stroke survivors with aphasia: a quantitative scoping review. Neuropsychol. Rehabil. 1–35. doi: 10.1080/09602011.2024.2381874. [Epub ahead of print].
Caldwell, N. S., Holyfield, C., Lorah, E., and Rackensperger, T. (2024). Reducing linguistic profiling of individuals with communication disabilities to enhance careers: avoiding assumptions based on speech, language and communication mode. Career Dev. Int. 29, 367–380. doi: 10.1108/CDI-07-2023-0230
Carragher, M., Steel, G., O'Halloran, R., Lamborn, E., Torabi, T., Johnson, H., et al. (2024). Aphasia disrupts usual care: “I'm not mad, I'm not deaf” – the experiences of individuals with aphasia and family members in hospital. Disabil. Rehabil. 46, 6122–6133. doi: 10.1080/09638288.2024.2324115
Charlson, M. E., Pompei, P., Ales, K. L., and MacKenzie, C. R. (1987). A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40, 373–383. doi: 10.1016/0021-9681(87)90171-8
Cummings, L. (2023). Communication disorders: a complex population in healthcare. Lang. Health 1, 12–19. doi: 10.1016/j.laheal.2023.06.005
de Groot, V., Beckerman, H., Lankhorst, G., and Bouter, L. (2004). How to measure comorbidity: a critical review of available methods. J. Clin. Epidemiol. 57:323. doi: 10.1016/j.jclinepi.2003.09.002
Equal Employment Opportunity Commission (2013). PART 1630—Regulations of the Americans with Disabilities Act. Available at: https://www.ecfr.gov/current/title-29/subtitle-B/chapter-XIV/part-1630
Filipska-Blejder, K., Zielińska, J., Zieliński, M., Wiśniewski, A., and Slusarz, R. (2023). How does aphasia affect quality of life? Preliminary reports. J. Clin. Med. 12:7687. doi: 10.3390/jcm12247687
Garcia, L. J., Laroche, C., and Barrette, J. (2002). Work integration issues go beyond the nature of the communication disorder. J. Commun. Disord. 35, 187–211. doi: 10.1016/S0021-9924(02)00064-3
Gaspar, R. S., Rossi, L., Hone, T., and Dornelles, A. Z. (2021). Income inequality and non-communicable disease mortality and morbidity in Brazil States: a longitudinal analysis 2002-2017. Lancet Reg. Health Am. 2:100042. doi: 10.1016/j.lana.2021.100042
Gilmore, N., Fraas, M., and Hinckley, J. (2022). Return to work for people with aphasia. Arch. Phys. Med. Rehabil. 103, 1249–1251. doi: 10.1016/j.apmr.2021.12.020
Goodman, N., Mooris, M., and Boston, K. (2019). Financial Inequality: Disability, race and poverty in America. Available at: https://www.nationaldisabilityinstitute.org/wp-content/uploads/2019/02/disability-race-poverty-in-america.pdf (accessed October 2, 2024).
Hersh, D., Williamson, C., Brogan, E., and Stanley, M. (2024). “It's day to day problems:” experiences of people with aphasia who live alone. Int. J. Speech Lang. Pathol. 26, 367–379. doi: 10.1080/17549507.2024.2358830
Isetti, D., and Eadie, T. (2016). The Americans with disabilities act and voice disorders: practical guidelines for voice clinicians. J. Voice 30, 293–300. doi: 10.1016/j.jvoice.2015.04.006
Jacobs, M., and Ellis, C. (2023). Aphasianomics: estimating the economic burden of poststroke aphasia in the United States. Aphasiology 37, 25–38. doi: 10.1080/02687038.2021.1985426
Jagoe, C., McDonald, C., Rivas, M., and Groce, N. (2021). Direct participation of people with communication disabilities in research on poverty and disabilities in low and middle income countries: a critical review. PLoS ONE 16:e0258575. doi: 10.1371/journal.pone.0258575
Jajtner, K. M., Mitra, S., Fountain, C., and Nichols, A. (2020). Rising income inequality through a disability lens: trends in the United States 1981–2018. Soc. Indic. Res. 151, 81–114. doi: 10.1007/s11205-020-02379-8
Jeon, S. H., and Pohl, R. V. (2017). Health and work in the family: evidence from spouses' cancer diagnoses. J. Health Econ. 52, 1–18. doi: 10.1016/j.jhealeco.2016.12.008
Madden, E. B., Bislick, L., Wallace, S. E., Therrien, M. C. S., and Goff-Albritton, R. (2023). Aphasia and friendship: stroke survivors' self-reported changes over time. J. Commun. Disord. 103:106330. doi: 10.1016/j.jcomdis.2023.106330
McGurk, R., and Kneebone, I. I. (2013). The problems faced by informal carers to people with aphasia after stroke: a literature review. Aphasiology 27, 765–783. doi: 10.1080/02687038.2013.772292
National Aphasia Association (2024a). What is aphasia. Available at: https://aphasia.org/what-is-aphasia/ (accessed September 27, 2024).
National Aphasia Association (2024b). How common is aphasia? Available at: https://aphasia.org/what-is-aphasia/ (accessed October 2, 2024).
Park, S., and Stimpson, J. P. (2024). Health care expenses and financial hardship among medicare beneficiaries with functional disability. JAMA Netw. Open 7:e2417300. doi: 10.1001/jamanetworkopen.2024.17300
Pike, C., Kritzinger, A., and Pillay, B. (2017). Social participation in working-age adults with aphasia: an updated systematic review. Top Stroke Rehabil. 24, 627–639. doi: 10.1080/10749357.2017.1366012
Pisu, M., and Martin, M. Y. (2022). Financial toxicity: a common problem affecting patient care and health. Nat. Rev. Dis. Primers 8:7. doi: 10.1038/s41572-022-00341-1
Poirier, S. È., Voyer, L. A., Poulin, V., Lamontagne, M. E., and Monetta, L. (2024). Communication challenges for people with chronic aphasia: a systematic qualitative review of barriers and facilitators in local services. Disabilities 4, 616–631. doi: 10.3390/disabilities4030038
Prosperity Now (2018). Financial stability of people with disabilities. Available at: https://prosperitynow.org/sites/default/files/resources/Financial-Stability-of-People-with-Disabilities.pdf (accessed October 2, 2024).
Quique, Y. M., Ashaie, S. A., Babbitt, E. M., Hurwitz, R., and Cherney, L. R. (2023). Fatigue influences social participation in aphasia: a cross-sectional and retrospective study using patient-reported measures. Arch. Phys. Med. Rehabil. 104, 1282–1288. doi: 10.1016/j.apmr.2023.02.013
Salami, J. A., Warraich, H. J., Valero-Elizondo, J., Spatz, E. S., Desai, N. R., Rana, J. S., et al. (2018). National trends in nonstatin use and expenditures among the US adult population from 2002 to 2013: insights from medical expenditure panel survey. J. Am. Heart Assoc. 7:e007132. doi: 10.1161/JAHA.117.007132
Sarzyńska-Długosz, I. (2023). An optimal model of long-term post-stroke care. Front. Neurol. 14:1129516. doi: 10.3389/fneur.2023.1129516
Tomkins, B., Siyambalapitiya, S., and Worrall, L. (2013). What do people with aphasia think about their health care? Factors influencing satisfaction and dissatisfaction. Aphasiology 27, 972–991. doi: 10.1080/02687038.2013.811211
Willson, A. E., Shuey, K. M., and Pajovic, V. (2024). Disability and the widening gap in mid-life wealth accumulation: a longitudinal examination. Res. Soc. Stratif. Mobil. 90:100896. doi: 10.1016/j.rssm.2024.100896
Keywords: stroke, aphasia, financial toxicity, disparities, income
Citation: Jacobs M and Ellis C Jr (2025) More than a communication disorder: inequities in the financial toxicity of post-stroke aphasia. Front. Stroke 3:1507025. doi: 10.3389/fstro.2024.1507025
Received: 06 October 2024; Accepted: 11 December 2024;
Published: 07 January 2025.
Edited by:
Anthony Pak Hin Kong, The University of Hong Kong, Hong Kong SAR, ChinaReviewed by:
Lluis Alzamora Llull, Massachusetts General Hospital and Harvard Medical School, United StatesCait Brown, University of Washington, United States
Copyright © 2025 Jacobs and Ellis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Charles Ellis Jr., ZWxsaXNjaEBwaGhwLnVmbC5lZHU=
 Molly Jacobs1
Molly Jacobs1 Charles Ellis Jr.
Charles Ellis Jr.