- 1Department of Human Movement Science, Sport and Health, University of Graz, Graz, Austria
- 2Faculty of Environmental and Urban Change, York University, Toronto, ON, Canada
Adaptive cycling holds potential for promoting physical and mental health among individuals with disabilities, who often face barriers to traditional cycling and other forms of exercise. This scoping review systematically examines existing scientific literature to assess the effects of adaptive cycling on the physical and mental health of individuals with disabilities. Following a widely recognized methodological scoping review framework, 35 qualitative and quantitative studies were identified through comprehensive database searches and manual screenings. The review highlights the positive impacts of adaptive cycling on cardiovascular fitness, muscle strength, and overall physical well-being, as well as improvements in mental health and quality of life. Despite these benefits, significant research gaps remain, particularly concerning adaptive cycling modalities, such as sociable cycles, chair transporters, and power-assisted bikes, which were underrepresented in the existing literature. This review underscores the need for further studies to provide a comprehensive understanding on the effects of different adaptive cycling modalities. Such studies are essential to improve accessibility and ultimately support the health and social inclusion of individuals with disabilities.
1 Introduction
Cycling is widely acknowledged to have numerous health benefits including the enhancement of cardiovascular fitness, muscle strength, joint mobility, proprioception and mental health (1, 2). Regular participation in cycling can significantly reduce the risk of chronic diseases including cardiovascular diseases, metabolic diseases, and certain cancers (1, 2). Moreover, cycling supports weight management, usually reduces stress levels, and contributes to overall well-being. Its low-impact nature makes it an ideal form of exercise for individuals across various age groups and fitness levels, further solidifying its role as a valuable health-promoting activity (1, 2).
Despite the well-documented benefits of cycling, not everyone can engage in this form of activity. Individuals with certain disabilities may face significant barriers that limit their ability to participate in traditional cycling (3). As stated by the World Health Organization, about 1.3 billion people, or approximately 16% of the world's population, live with some form of disability (4). According to the United Nations, persons with disabilities “include those who have long-term physical, mental, intellectual, or sensory impairments which in interaction with various barriers may hinder their full and effective participation in society on an equal basis with others” [(5), p. 4]. This definition includes physical, sensory, cognitive, and developmental disabilities, affecting individuals across all age groups (4). The prevalence of disabilities is expected to increase as the population ages, with elderly individuals experiencing higher rates of physical impairment (6).
For people with disabilities, an inability to engage in regular physical activity, such as cycling, can lead to a range of health risks (7). High levels of sedentary behavior are common among this population, which can result in secondary health conditions including obesity, cardiovascular disease, and mental health issues such as depression and anxiety (8, 9). These risks underscore the importance of promoting accessible forms of physical activity to maintain health and prevent disease in individuals with disabilities.
Adaptive cycling plays a crucial role in addressing these challenges. By incorporating various technical adaptations—such as hand cycles for those with lower limb impairments, tricycles for enhanced stability and hemiplegia, tandem bicycles for individuals with visual impairments, specially adapted cycles for persons with skeletal dysplasia, and electrical-assisted features to accommodate varying levels of physical capability—adaptive cycling makes it possible for individuals with a wide range of disabilities to participate (3, 10). These innovations enable people with disabilities to enjoy the physical and psychological benefits of cycling, while promoting inclusion and active living (3, 10). Given these considerations, adaptive cycles present a distinctive opportunity to promote physical activity among individuals with disabilities, helping to mitigate sedentary behavior and the associated health risks.
While various forms of adaptive physical activity have been reviewed in the literature (11, 12), adaptive cycling has not yet received the same level of attention. This form of exercise may offer distinct benefits due to its low-impact nature, its potential for fostering social inclusion, and assumed adaptability to a wide range of impairments. A scoping review focused on adaptive cycling is thus necessary to address the specific needs, outcomes and possibilities associated with this activity. This review will not only summarize the current body of research but will also highlight critical gaps in knowledge and suggest directions for future research in this underexplored area.
The purpose of this scoping review is to systematically investigate the existing scientific literature. The guiding research question is: “Is there scientific information available about the effects of adaptive cycling on the physical and mental health of individuals with disabilities?” By synthesizing the available evidence, this review seeks to (1) highlight the potential benefits and limitations of adaptive cycling, (2) identify research gaps, and (3) suggest directions for future studies. The findings will provide valuable insights for healthcare providers, policymakers, and individuals with disabilities.
2 Methods
We adhered to the methodological framework for scoping reviews outlined by Arksey and O'Malley (13), which consists of five key stages: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; and (5) collating, summarizing, and reporting the results. We note that steps 4 and 5 were combined for efficacy, without compromising the quality of the analysis.
In addition, we adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines (14) throughout the review process, ensuring transparency and methodological rigor.
2.1 Identifying the research question
As outlined above, this scoping review is guided by the following research question: “Is there scientific information available about the effects of adaptive cycling on physical and mental health of individuals with disabilities?” Thus, the aim of the following steps is to synthesize existing research to understand the influence of adaptive cycling on the health of individuals with disabilities and to identify any research gaps.
2.2 Identifying relevant studies
To identify relevant studies, we conducted a literature search in April 2024 using three databases: PubMed, Scopus, and Web of Science. We performed a spot-check of two other databases (Cochrane and ScienceDirect) which resulted in no further identification of new, significant literature. No publication date restrictions were applied to ensure a comprehensive search, capturing all studies written in English or German available up to the search date. The search terms were developed based on the PICO framework (15), focusing on Population, Intervention, and Outcome, while the Comparison component was excluded to maximize the inclusion of all potential studies. The search was conducted in a two-step process:
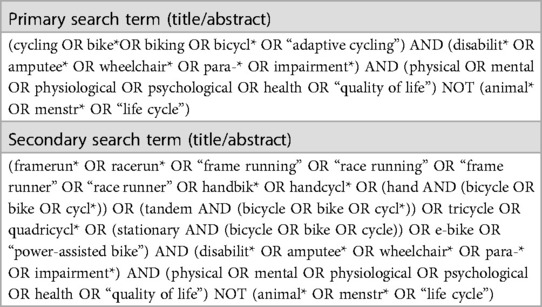
1. Initially, we conducted searches in each of the three databases using a primary search term based on the research question of our study, focusing on the Title/Abstract fields, as shown in Table 1.
2. Subsequently, we conducted a further search using a secondary search term, also outlined in Table 1. This secondary term was developed based on the articles identified in the initial search. Specifically, we revisited the search using terms related to adaptive cycles that had already been identified. This step was taken to ensure that we did not overlook any specific designations or variations of adaptive cycles. The aim was to further refine the search results.
In addition to this two-step process, we conducted supplementary searches by reviewing the reference lists of identified articles and utilizing Google Scholar to identify any additional relevant sources. The final search terms, which were adjusted according to the requirements of each respective database, are presented in Table 1. For more information on the results, please refer to Figure 1.
2.3 Study selection
The study selection process was based on the PRISMA flow chart model (16). Following primary and secondary searches, a manual preselection of relevant studies was conducted based on their title and abstract. Subsequently, duplicates were removed, and another screening of the remaining articles was performed using the inclusion and exclusion criteria outlined in Table 2. During the review of these articles, reference lists were also examined for additional relevant literature. Additionally, Google Scholar was screened for further relevant articles. The study selection was initially conducted by one primary reviewer based on the inclusion and exclusion criteria defined beforehand by all authors. For the final selection, all authors were involved in reviewing the articles to ensure consensus. Any conflicts or disagreements that arose during the process were resolved through discussion among the authors. Only articles that met the inclusion criteria after thorough examination were included into the analysis. After agreement among the authors on the final selection of studies, one reviewer processed the findings. The final selection of articles then underwent the steps outlined in Chapter 2.4.
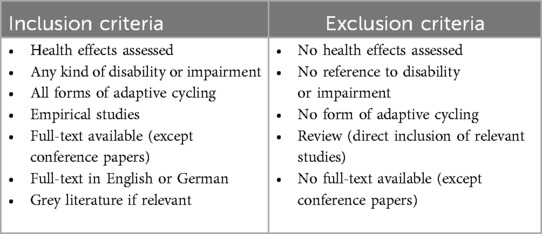
Table 2. Overview of inclusion and exclusion criteria applied during the manual preselection and subsequent screening of articles identified in the primary and secondary literature searches.
2.4 Charting data and collating, summarizing and reporting results
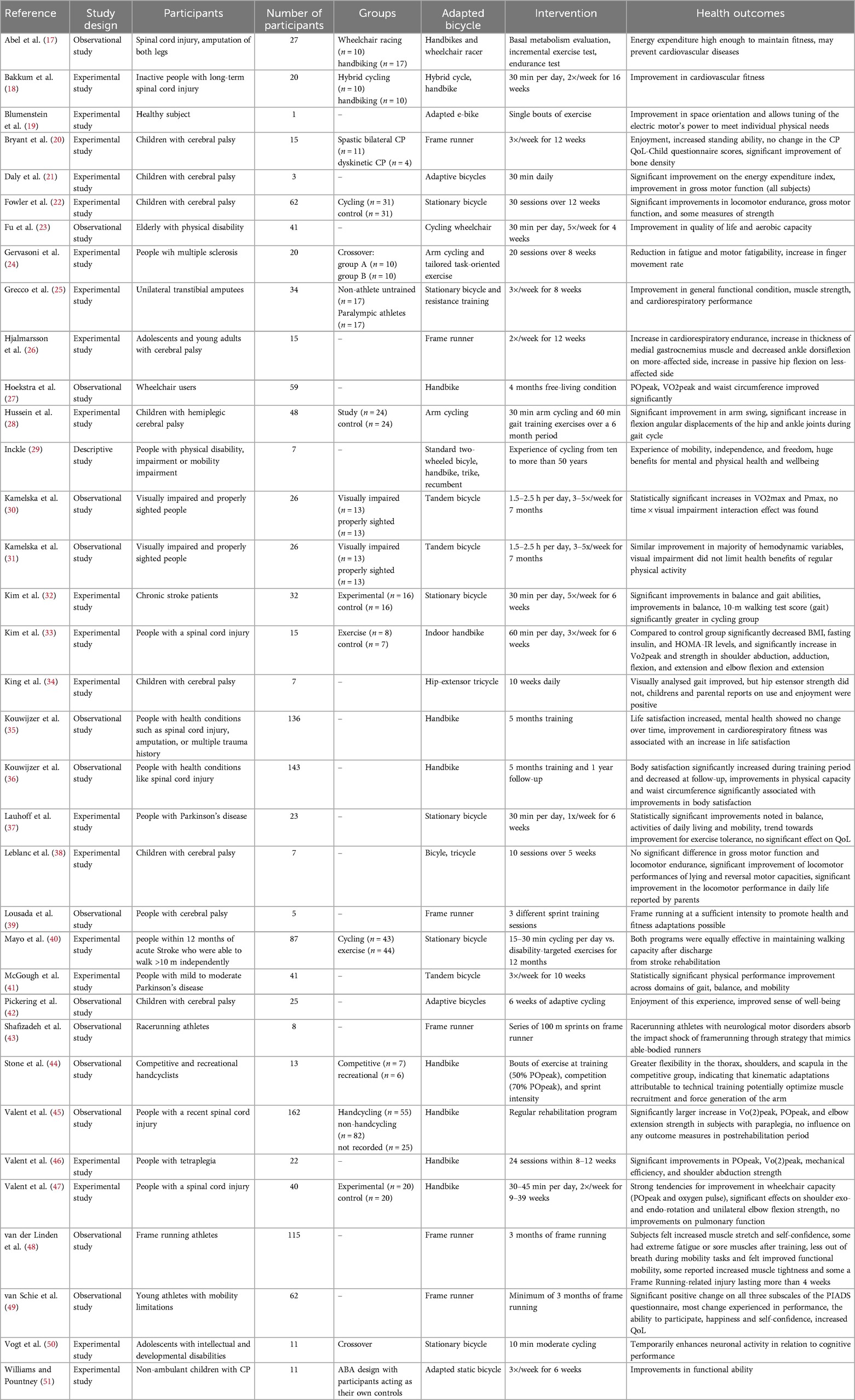
The previously selected studies were systematically organized in a table (see Table 3), wherein various characteristics of each study were collated. These characteristics included the reference (main author and publication year), study design, study participants, number of participants, type of adaptive cycle used, intervention employed, intervention groups, and identified health outcomes. Subsequently, an overview was generated based on this table, reflecting the current body of literature along with its gaps. Afterwards, a synthesis of the compiled data was conducted to provide a cohesive summary of the findings. This synthesis aimed to elucidate the significance and implications of the identified research outcomes, shedding light on major trends, patterns, and areas that require further investigation. In addition, particular attention was paid to placing the results into the broader context of adaptive cycling research in order to gain valuable insights for practitioners and researchers in this field.
2.4.1 Definition of health categories
To ensure clarity in the presentation and interpretation of results, it is important to define the categories of health outcomes discussed in this review. In the following, physical health refers to improvements in physiological functions such as cardiovascular fitness, strength, and endurance (52), while mental health is conceptualized as changes in cognitive function, mood, and emotional well-being (53). Quality of Life (QoL) was included as an additional category due to its significant role in complementing overall health outcomes in the analyzed population. It encompasses broader dimensions of well-being, including life satisfaction, social participation, and general happiness (54). To avoid confusion, a clear distinction is made between these categories, acknowledging that some outcomes (e.g., life satisfaction) may overlap with both mental health and QoL. This distinction is made to more accurately capture the specific impacts of adaptive cycling interventions on different aspects of health and well-being, allowing for a more comprehensive understanding of their effects.
3 Results
Altogether 35 studies were identified, including 34 quantitative and 1 qualitative study, that have investigated the physical and mental health effects of adaptive cycling in individuals with disabilities. The selection process is illustrated in Figure 1 following an adapted form of the PRISMA flow chart (16). All of the studies included in this review concentrate on structured interventions with adaptive cycling, examining the effects of specific cycling interventions on health outcomes in controlled settings.
3.1 Overview of the study characteristics
3.1.1 Study characteristics
The following table (Table 4) provides a summary of key variables extracted from the reviewed literature, including sample size, study design, and intervention characteristics. The distribution of studies and their percentages within each variable category is presented. Notably, a wide variance in sample size is evident. The identified literature was categorized into three clusters of study designs: experimental (57.14%), observational (40.00%), and descriptive studies (2.86%). Additionally, the type of intervention was classified to better contextualize the health outcomes of the reviewed studies. This involved categorization into acute interventions (a single session of adaptive cycling), short-term interventions lasting less than 6 months, long-term interventions exceeding 6 months, and investigations examining follow-up effects. The relative share of each intervention type among the 35 articles is as follows: 17.14% for acute interventions, 62.86% for short-term interventions, 17.14% for long-term interventions, and 2.86% for follow-up studies.
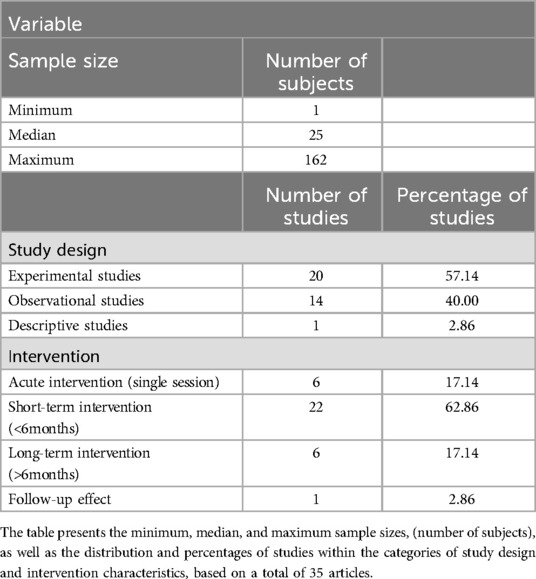
Table 4. Summary of key variables extracted from the reviewed literature, including sample size, study design, and intervention characteristics.
Moreover, based on the analysis, the majority of experimental studies focused on short-term interventions (16 studies), followed by acute interventions (2 studies) and long-term interventions (2 studies). Observational studies were predominantly short-term (6 studies), with fewer focusing on acute (4 studies), long-term (3 studies), and follow-up interventions (1 study). Descriptive studies primarily addressed long-term interventions (1 study).
3.1.2 Adaptive cycles
The variety of adapted cycles was categorized using the classification suggested by Norcliffe et al. (10). The proposed categories effectively cover the existing types of adaptive cycles and thus allowed for an examination of the available literature. As shown in Figure 2, the highest number of articles were found for stability machines (n = 14: 20, 21, 25, 26, 32, 34, 37, 39, 40, 43, 48–51) and handcycles (n = 13: 17, 18, 24, 27–29, 33, 35, 36, 44–47). Additionally, three articles were found for pedal (23, 29, 38) and tandem bicycles (30, 31, 41). Two articles could not be assigned to a specific cycle type attributed as undefined (21, 42) and one article was found for power-assisted bikes (19). It is noteworthy that the article of Inckle (29) focused on different types of adaptive cycles, making it assignable to multiple categories. As shown on the right side of Figure 2, no articles were found regarding the mental and physical health impacts of adaptive cycling among individuals with disabilities for the categories sociables (side-by-side), power-assisted bikes, and chair transporters.
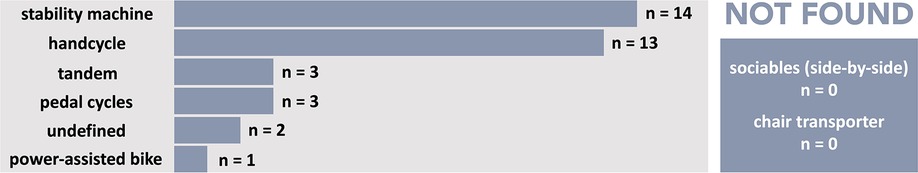
Figure 2. Adaptive cycling modalities identified in the literature search. The figure shows the types of cycling studied for their impact on the physical and mental health of individuals with disabilities, as well as areas lacking research.
For clarity, the identified cycles were categorized as follows: handcycles encompassed all cycles propelled by hand, including arm cycles, indoor handcycles, and traditional handcycles. Stability machines included cycles such as frame runners, stationary bikes, and hip-extensor tricycles. Pedal cycles comprised all adapted cycles with pedals not classified under stability machines, such as recumbent bicycles and tricycles, cycling wheelchairs, trikes, and standard bicycles. Additionally, adaptive cycles were labeled as undefined if the articles did not specify the type of cycle being used.
3.1.3 Population
Within this scoping review, various groups of individuals with disabilities who participated in adaptive cycling interventions were identified. These subject groups encompassed individuals with medical conditions such as spinal cord injuries (17, 18, 33, 35, 36, 45, 47), cerebral palsy (20–22, 26, 28, 34, 38, 39, 42, 51) multiple sclerosis (24), Parkinson's disease (37, 41), and those recovering from acute and chronic strokes (32, 40). Additionally, participants with conditions such as amputations, physical disabilities, impairments, or mobility restrictions, tetraplegia, paraplegia, intellectual and developmental disabilities, multiple trauma histories, and visual impairments (17, 23, 25, 29–31, 35, 46, 49, 50), as reported by the original authors, were also included. Furthermore, other groups of individuals with disabilities were identified that were not clearly categorized by the authors under a specific condition but were described as wheelchair users, frame running athletes, and competitive and recreational handcyclists (27, 43, 44, 48).
3.2 Health outcomes of adapted cycling on individuals with disabilities
This section provides an overview of the health effects examined in the selected studies. The outcomes are categorized into physical and mental health effects, and effects on QoL. Within each of the categories, the impact of interventions is discussed based on the duration of the interventions as well as the adaptive cycle used.
3.2.1 Physical health effects
From the examined articles, 27 focused on the physical health effects of adaptive cycling, encompassing various aspects and dimensions of physical performance and health. The acute physical effects of adaptive cycling activities were investigated through handcycling, power-assisted cycling and frame running. Handcycling demonstrated high energy expenditure levels, sufficient to maintain fitness levels and potentially prevent cardiovascular diseases, even when performed at moderate intensity corresponding to 2 mmol/L lactate (17). Similar effects promoting health and fitness adaptations were observed with frame running (39). Moreover, competitive handcyclists exhibited greater flexibility in the thorax (∼5°, p < 0.05) and extended their shoulder (∼10°, p < 0.01), and posteriorly tilted their scapular (∼15°, p < 0.05) more compared to recreational handcyclists suggesting kinematic adaptations attributable to technical training that may optimize muscle recruitment and force generation of the arm (44). Additionally, frame running athletes with neurological motor disorders employed strategies akin to able-bodied runners to absorb impact shock during frame running, positively influencing their movement behavior (43). The use of adapted E-bikes, as shown by Blumenstein et al. (19), can enhance space orientation for individuals with perceptual disorders and allow for the tuning of the electric motor's power to meet individual physical needs, offering tailored support during physical activity.
Regarding the short-term effects of adaptive cycling on physical health, as defined by studies with intervention durations of less than 6 months, a variety of cycles were examined, including handcycles, stability machines, pedal cycles, and tandem cycles. Handcycling interventions, as demonstrated by Bakkum et al. (18) and Gervasoni et al. (24), have shown positive effects on cardiovascular fitness and reductions in fatigue and motor fatigability. Valent et al. (46) and Valent et al. (47) highlighted significant improvements in peak oxygen uptake, mechanical efficiency, and wheelchair capacity associated with handcycle use, including enhancements in arm and shoulder strength and mobility. Similarly, Hoekstra et al. (27) and Kim et al. (33) reported significant improvements in peak oxygen uptake, power output, strength in various muscle groups and body composition parameters following handcycle interventions. These findings collectively underscore the effectiveness of handcycle interventions in promoting both cardiovascular health and muscular strength and suggest their potential in enhancing overall physical well-being.
Using short-term interventions involving stability machines, similar findings were observed. frame running, described by Hjalmarsson et al. (26), contributed to an average increase in cardiorespiratory endurance, accompanied by enhancements in muscle thickness and passive hip flexion, although it was associated with decreased ankle dorsiflexion. As highlighted by Bryant et al. (20), frame running interventions also led to improvements in standing ability and significant improvements of bone quality index scores. Van der Linden et al. (48) highlighted the multiple effects of frame running, including improved muscle stretching, increased self-confidence, and improved functional mobility, although they reported fatigue and muscle soreness. Nevertheless, the latter is a common training adaption of the muscle which improves its strength in the long-term. An intervention with a hip-extensor tricycle by King et al. (34), yielded improvements in gait analysis, although no significant changes were observed in hip extensor strength. Using stationary bicycles, Grecco et al. (25) demonstrated enhancements in overall functional condition, muscle strength, and cardiorespiratory performance. This was further underscored by Fowler et al. (22), who reported substantial improvements in locomotor endurance, gross motor function, and strength. Additionally, individuals with disabilities using stationary bicycles were observed to experience additional enhancements in balance, mobility, and gait abilities, along with improvements in activities of daily living (32, 37). Overall, these findings emphasize the positive impact of short-term interventions involving stability machines in enhancing cardiorespiratory endurance, strength and functional mobility, thereby supporting improvements in overall physical health.
Pedal cycles, including cycling wheelchairs, bicycles, and tricycles, have also demonstrated substantial benefits in various physical health aspects, particularly through short-term interventions. Interventions with cycling wheelchairs resulted in improvements in aerobic capacity (23), while interventions involving bicycles and tricycles significantly enhanced locomotor performance, lying, and reversal motor capacities (38). Following a tandem cycling intervention, McGough et al. (41) observed statistically significant improvements in physical performance across gait, balance, and mobility domains.
In addition, two short-term interventions with undefined adaptive cycles found that significant improvements in the energy expenditure index as well as gross motor function can be achieved (21) and improvements in functional ability were associated with adapted cycles (51).
While the findings of short-term interventions collectively underscore the diverse and significant positive impacts of adaptive cycling on physical health and function, it is equally important to consider the long-term effects of interventions lasting more than 6 months to fully understand the potential of adaptive cycling on physical health for individuals with disabilities. Altogether five studies were found that investigated the long-term effects including handcycles, tandem cycles and stability machines. Handcycling led to significant improvements in arm swing and flexion angles during the gait cycle (28), with a notable increase in physiological parameters among paraplegic individuals, while its influence post-rehabilitation was inconclusive (45). Tandem cycling resulted in statistically significant increases in VO2max and Pmax, with elite cyclists exhibiting significantly higher VO2max compared to sub-elite cyclists (30); additionally, it demonstrated similar improvements in hemodynamic variables (e.g., heart rate, stroke volume, cardiac output, ejection fraction, systemic vascular resistance), suggesting that severe visual impairment does not impede the health benefits of regular physical activity (31). Following a long-term intervention with stationary bicycles, Mayo et al. (40), found that stationary cycling was equally effective in maintaining walking capacity after discharge from stroke rehabilitation as were mobility exercises and brisk walking.
3.2.2 Mental health effects
Seven articles addressed the mental health effects of adaptive cycling among individuals with disabilities. Vogt et al. (50) found that acute stationary bicycle use temporarily enhances neuronal activity, particularly in relation to cognitive performance in individuals with intellectual and developmental disabilities. Short-term effects were observed across a restricted range of cycling modalities. Frame runner and hip-extensor tricycle interventions were associated with increased enjoyment (20, 34) and increased self-confidence (48), while adaptive bicycle use was associated with an improved sense of well-being (42). Handcycling was linked to increased life satisfaction during the training period, although no significant changes in mental health were noted over time (35). When examining the long-term effects studied by Inckle (29), a perceived enhancement in the experience of mobility, independence, and freedom, along with significant benefits for mental and physical health and wellbeing of the individuals involved, can be observed.
3.2.3 Effects on quality of life
In addition to the physical and mental health benefits, five studies also examined changes in QoL among individuals with disabilities throughout adaptive cycling interventions. Fu et al. (23) reported enhancements in QoL using cycling wheelchairs among elderly with physical disability. Similarly, frame running interventions have been associated with positive changes in various aspects of QoL, as reported by parents of participating children. These changes were particularly evident in performance, participation ability, happiness, and self-confidence, suggesting an overall increase in QoL (49). In contrast, Bryant et al. (20) found an increase in enjoyment using frame runner but no changes in QoL. Lauhoff et al. (37) supported those findings, observing no significant impact on QoL following a stationary bicycle use.
Follow-up examinations of handcycle interventions conversely revealed significant changes in body satisfaction. Body satisfaction significantly increased during the training period but decreased back to pre-training levels at follow-up, whereby individuals with more severe impairments exhibited a larger decrease in body satisfaction. Additionally, improvements in physical capacity and waist circumference were significantly associated with improvements in body satisfaction (36).
4 Discussion
The present scoping review aimed to comprehensively examine the existing literature on the physical and mental health effects of adaptive cycling in individuals with disabilities. While the review identified a substantial body of research investigating the effects of various adaptive cycling interventions, several noteworthy gaps and future research directions emerged from the analysis.
Adaptive cycling interventions demonstrated significant potential for enhancing physical health outcomes, including improvements in cardiovascular fitness, muscle strength, mobility, and functional capacity. Specifically, interventions involving handcycles, stability machines, pedal cycles, and tandem cycles were associated with positive changes in physical fitness parameters such as peak oxygen uptake, power output, and muscle strength. Moreover, adaptive cycling activities promoted cardiovascular health, with studies indicating improvements in cardiorespiratory endurance and energy expenditure levels. In terms of mental health, a limited number of studies addressed this aspect, but those available found positive effects. Short-term effects on mental well-being were observed across various cycling modalities, including increased enjoyment and a sense of well-being. However, the evidence base for mental health outcomes was less extensive compared to physical health outcomes, indicating a need for further research in this area.
Controversies and inconsistencies were also observed, particularly regarding QoL outcomes. While some studies reported significant enhancements in QoL domains, such as performance, participation ability, happiness, and self-confidence, others found no effects of adaptive cycling on QoL. These discrepancies underscore the need for further research to elucidate the true impact of adaptive cycling on QoL outcomes and to address potential confounding factors that may influence individual perceptions.
Furthermore, there was variability in the quantity and quality of evidence across different categories of adaptive cycling modalities. While certain modalities, such as handcycles and stability machines, were supported by a relatively robust body of evidence, others, such as sociable cycles, chair transporters, and power-assisted bikes, were underrepresented or lacked sufficient empirical support. This underscores the necessity for further research to investigate the diverse array of adaptive cycling options and their effects on health outcomes among individuals with disabilities, particularly as those alternative cycling modalities show potential but have not been adequately studied. Future research should explore their potential benefits and feasibility to provide a more comprehensive understanding of adaptive cycling options.
Moreover, it is essential to consider the broader context of adaptive physical activity. Research on other forms of physical activity, such as adapted sports and exercise interventions for individuals with disabilities, has shown similar benefits in terms of physical and mental health, as well as QoL (55–57). This review's findings align with the broader literature on adaptive physical activity, underscoring the importance of structured and inclusive physical exercise for individuals with disabilities. Future studies should explore how adaptive cycling may complement or differ from other adaptive physical activities, contributing to a more comprehensive understanding of the role of physical activity in improving overall health outcomes.
Another significant issue in the existing literature is the inconsistency in how populations are defined and categorized. While various groups of individuals with disabilities have participated in adaptive cycling interventions, the studies often lack clear and standardized definitions of these populations. For instance, some studies include individuals with spinal cord injuries, cerebral palsy, multiple sclerosis, and other specific conditions, while others broadly categorize participants as wheelchair users or individuals with physical disabilities. This lack of uniformity in population categorization limits the ability to compare and generalize findings across studies. Moreover, some disability groups, such as those with intellectual and developmental disabilities or sensory impairments, remain underrepresented. Additionally, gaps remain in assessing health outcomes related to the community usage of adaptive cycling, which could provide valuable insights into its real-world impact and broader applicability. Future research should aim to standardize the categorization of disability populations and ensure inclusivity, also in relation to community settings, to better capture the diverse needs and experiences of individuals with disabilities.
The studies reviewed in this scoping review varied considerably in terms of sample size, study design, and intervention duration, highlighting challenges in interpreting the findings. The wide variance in sample sizes, with some studies involving very small participant groups, may impact the reliability and generalizability of the results. Additionally, while adaptive cycling shows potential for improving physical and mental health, the predominance of short-term interventions limits our understanding of its long-term effects, underscoring the need for further research with larger sample sizes and extended intervention and follow-up periods.
4.1 Limitations
While every effort was made to conduct a comprehensive search of the literature, it is always possible that some studies were not captured by the search terms. Despite trying alternative search criteria, it is always possible that mis-specified keywords and inaccurate abstracts led to the exclusion of certain studies that could have provided further insights into the topic. This review included studies published in English and German to reflect the authors linguistic abilities; studies in other languages were therefore not included, which may have limited representation from regions where research is predominantly published in other languages. Furthermore, the quality and heterogeneity of the included studies may have influenced the synthesis and interpretation of the findings. Although we did not develop a formal protocol or conduct a critical appraisal—given that our aim was to map the breadth of the existing literature rather than evaluate study quality—we adhered to the remaining PRISMA-ScR guidelines to ensure a comprehensive and transparent report of our methods and findings.
5 Conclusion
In summary, this scoping review consolidates the current evidence on the physical and mental health effects of adaptive cycling for individuals with disabilities, and emphasises significant gaps in the literature. The findings demonstrate the potential of adaptive cycling to enhance physical health, mental health, and quality of life. However, inconsistencies in the evidence, especially concerning quality-of-life outcomes, highlight the need for further investigation.
Beyond summarizing existing evidence, this review underscores the importance of expanding research to include underrepresented populations and modalities, such as sociable cycles and chair transporters. Future research should also explore the long-term effects of adaptive cycling interventions and consider the broader spectrum of health outcomes associated with various cycling modalities over different time periods. Such efforts could provide a more comprehensive understanding of adaptive cycling's benefits and ensure its accessibility for diverse disability groups.
Ultimately, this review serves as a foundation for future research and practice in the field of adaptive cycling for individuals with disabilities. Its findings have the potential to inform clinical decision-making, guide future research endeavors, and thereby foster improved health and well-being of individuals with disabilities.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
NM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. GN: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing. AK: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Open access funding was provided by the University of Graz. Social Sciences and Humanities Research Council of Canada Grant 430-2023-00891 also funded this research.
Acknowledgments
The authors acknowledge the financial support by the University of Graz and the Social Sciences and Humanities Research Council of Canada.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Garrard J, Rissel C, Bauman A. Health benefits of cycling. In: Pucher J, Buehler R, editors. City Cycling. Cambridge, MA: MIT Press (2012). p. 31–56.
2. Oja P, Titze S, Bauman A, De Geus B, Krenn P, Reger-Nash B, et al. Health benefits of cycling: a systematic review. Scand J Med Sci Sports. (2011) 21(4):496–509. doi: 10.1111/j.1600-0838.2011.01299.x
3. Clayton W, Parkin J, Billington C. Cycling and disability: a call for further research. J Transp Health. (2017) 6:452–62. doi: 10.1016/j.jth.2017.01.013
4. World Health Organization. Global Report on Health Equity for Persons with Disabilities. Geneva, Switzerland: World Health Organization (2022).
5. United Nations. Convention on the Rights of Persons with Disabilities. New York, NY: United Nations (2006). Available online at: https://www.un.org/disabilities/documents/convention/convoptprot-e.pdf (accessed July 8, 2024).
6. Chatterji S, Byles J, Cutler D, Seeman T, Verdes E. Health, functioning, and disability in older adults—present status and future implications. Lancet. (2015) 385(9967):563–75. doi: 10.1016/S0140-6736(14)61462-8
7. Rimmer JH, Schiller W, Chen MD. Effects of disability-associated low energy expenditure deconditioning syndrome. Exerc Sport Sci Rev. (2012) 40(1):22–9. doi: 10.1097/JES.0b013e31823b8b82
8. Carty C, van der Ploeg HP, Biddle SJ, Bull F, Willumsen J, Lee L, et al. The first global physical activity and sedentary behavior guidelines for people living with disability. J Phys Act Health. (2021) 18(1):86–93. doi: 10.1123/jpah.2020-0629
9. Smith L, Hamer M, Gardner B. Sedentary behavior and mental health. In: Stubbs B, Rosenbaum S, editors. Exercise-Based Interventions for Mental Illness. Cambridge, MA: Academic Press (2018). p. 107–19. doi: 10.1016/B978-0-12-812605-9.00006-X
10. Norcliffe G, Buliung R, Kruse A, Radford J. Disability and cycling technology: a socio-historical analysis. Disabil Stud Q. (2022) 42(1). doi: 10.18061/dsq.v42i1.8276
11. Derakhshan P, Miller WC, Bundon A, Labbé D, Bolt T, Mortenson WB. Adaptive outdoor physical activities for adults with mobility disability: a scoping review. Front Rehabil Sci. (2024) 4:1331971. doi: 10.3389/fresc.2023.1331971
12. Isidoro-Cabanas E, Soto-Rodriguez FJ, Morales-Rodriguez FM, Perez-Marmol JM. Benefits of adaptive sport on physical and mental quality of life in people with physical disabilities: a meta-analysis. Healthcare. (2023) 11(18):2480. doi: 10.3390/healthcare11182480
13. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8(1):19–32. doi: 10.1080/1364557032000119616
14. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169(7):467–73. doi: 10.7326/M18-0850
15. Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. (2007) 7:6. doi: 10.1186/1472-6947-7-16
16. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372. doi: 10.1136/bmj.n71
17. Abel T, Kröner M, Rojas VS, Peters C, Klose C, Platen P. Energy expenditure in wheelchair racing and handbiking-a basis for prevention of cardiovascular diseases in those with disabilities. Eur J Prev Card. (2003) 10(5):371–6. doi: 10.1097/01.hjr.0000096542.30533.59
18. Bakkum AJT, De Groot S, Stolwijk-Swüste JM, Van Kuppevelt DJ, Van Der Woude LHV, Janssen TWJ. Effects of hybrid cycling versus handcycling on wheelchair-specific fitness and physical activity in people with long-term spinal cord injury: a 16-week randomized controlled trial. Spinal Cord. (2015) 53(5):395–401. doi: 10.1038/sc.2014.237
19. Blumenstein T, Zeitlmann H, Alves-Pinto A, Turova V, Lampe R. Optimization of electric bicycle for youths with disabilities. SpringerPlus. (2014) 3:1–6. doi: 10.1186/2193-1801-3-646
20. Bryant E, Cowan D, Walker-Bone K. The introduction of Petra running-bikes (race runners) to non-ambulant children with cerebral palsy: a pilot study. Dev Med Child Neurol. (2015) 57(S4):34–5. doi: 10.1111/dmcn.12780_23
21. Daly C, Moore CL, Johannes S, Middleton J, Kenyon LK. Pilot evaluation of a school-based programme focused on activity, fitness, and function among children with cerebral palsy at GMFCS level IV: single-subject research design. Physiother Can. (2020) 72(2):195–204. doi: 10.3138/ptc-2018-0053
22. Fowler EG, Knutson LM, DeMuth SK, Siebert KL, Simms VD, Sugi MH, et al. Pediatric endurance and limb strengthening (PEDALS) for children with cerebral palsy using stationary cycling: a randomized controlled trial. Phys Ther. (2010) 90(3):367–81. doi: 10.2522/ptj.20080364
23. Fu JCM, Fu PK, Cheng YY. Benefits of cycling wheelchair training for elderly with physical disability: a prospective cohort study. Int J Environ Res Public Health. (2022) 19(24):16773. doi: 10.3390/ijerph192416773
24. Gervasoni E, Cattaneo D, Bertoni R, Grosso C, Bisio A, Rovaris M, et al. Effect of arm cycling and task-oriented exercises on fatigue and upper limb performance in multiple sclerosis: a randomized crossover study. Int J Rehabil Res. (2019) 42(4):300–8. doi: 10.1097/MRR.0000000000000362
25. Grecco MV, Brech GC, Soares Junior JM, Baracat EC, Greve JMDA, Silva PRS. Effect of concurrent training in unilateral transtibial amputees using paralympic athletes as a control group. Clinics. (2023) 78:100165. doi: 10.1016/j.clinsp.2023.100165
26. Hjalmarsson E, Fernandez-Gonzalo R, Lidbeck C, Palmcrantz A, Jia A, Kvist O, et al. Racerunning training improves stamina and promotes skeletal muscle hypertrophy in young individuals with cerebral palsy. BMC Musculoskelet Disord. (2020) 21:1–9. doi: 10.1186/s12891-020-03202-8
27. Hoekstra S, Valent L, Gobets D, van der Woude L, de Groot S. Effects of four-month handbike training under free-living conditions on physical fitness and health in wheelchair users. Disabil Rehabil. (2017) 39(16):1581–8. doi: 10.1080/09638288.2016.1200677
28. Hussein ZA, Abd-Elwahab MS, El-Shennawy SA. Effect of arm cycling on gait of children with hemiplegic cerebral palsy. Egypt J Med Hum Genet. (2014) 15(3):273–9. doi: 10.1016/j.ejmhg.2014.02.008
29. Inckle K. Disability, cycling and health: impacts and (missed) opportunities in public health. Scand J Disabil Res. (2020) 22(1):417–27. doi: 10.16993/sjdr.695
30. Kamelska AM, Krzysztof M, Piotr Z. Visual impairment does not limit training effects in development of aerobic and anaerobic capacity in tandem cyclists. J Hum Kinet. (2015) 48(1):87–97. doi: 10.1515/hukin-2015-0095
31. Kamelska AM, Mazurek KL, Nowakowski JJ. Hemodynamic adaptation to training in visually-impaired professional tandem cyclists. J Sports Med Phys Fitness. (2018) 58(7–8):1153–62. doi: 10.23736/s0022-4707.17.07598-3
32. Kim SJ, Cho HY, Kim YL, Lee SM. Effects of stationary cycling exercise on the balance and gait abilities of chronic stroke patients. J Phys Ther Sci. (2015) 27(11):3529–31. doi: 10.1589/jpts.27.3529
33. Kim DI, Lee H, Lee BS, Kim J, Jeon JY. Effects of a 6-week indoor hand-bike exercise program on health and fitness levels in people with spinal cord injury: a randomized controlled trial study. Arch Phys Med Rehabil. (2015) 96(11):2033–40. doi: 10.1016/j.apmr.2015.07.010
34. King EM, Gooch JL, Howell GH, Peters ML, Bloswick DS, Brown DR. Evaluation of the hip-extensor tricycle in improving gait in children with cerebral palsy. Dev Med Child Neurol. (1993) 35(12):1048–54. doi: 10.1111/j.1469-8749.1993.tb07922.x
35. Kouwijzer I, de Groot S, van Leeuwen CM, Valent LJ, van Koppenhagen CF, Comtesse PGP, et al. Changes in quality of life during training for the HandbikeBattle and associations with cardiorespiratory fitness. Arch Phys Med Rehabil. (2020) 101(6):1017–24. doi: 10.1016/j.apmr.2019.12.015
36. Kouwijzer I, de Groot S, van Leeuwen CM, Valent LJ, Stolwijk-Swüste JM, HandbikeBattle group*, et al. Changes in body satisfaction during and after a 5-month handcycle training period and associations with physical capacity and body composition in individuals with a physical impairment. Disabil Rehabil. (2024) 46(13):2839–46. doi: 10.1080/09638288.2023.2232732
37. Lauhoff P, Murphy N, Doherty C, Horgan NF. A controlled clinical trial investigating the effects of cycle ergometry training on exercise tolerance, balance and quality of life in patients with Parkinson’s disease. Disabil Rehabil. (2013) 35(5):382–7. doi: 10.3109/09638288.2012.694962
38. Leblanc V, Tubez F, Loge C, Abdi E, Verstraete I, Jacquemin D, et al. Influence of an adapted dynamic cycling activity on the motor function of children with cerebral palsy (CP). Comput Methods Biomech Biomed Engin. (2019) 22(sup1):454–56. doi: 10.1080/10255842.2020.1714979
39. Lousada H, Phillips S. The physiological and metabolic responses of individuals with cerebral palsy to habitual race running training. In: British Association of Sport and Exercise Sciences, editor. British Association of Sport and Exercise Sciences Annual Conference; 2014–2016 Nov 25–26; Burton Upon Trent, United Kingdom. Burton Upon Trent: British Association of Sport and Exercise Sciences (2016). doi: 10.1080/02640414.2016.1260807
40. Mayo NE, MacKay-Lyons MJ, Scott SC, Moriello C, Brophy J. A randomized trial of two home-based exercise programmes to improve functional walking post-stroke. Clin Rehabil. (2013) 27(7):659–71. doi: 10.1177/0269215513476312
41. McGough EL, Robinson CA, Nelson MD, Houle R, Fraser G, Handley L, et al. A tandem cycling program: feasibility and physical performance outcomes in people with Parkinson disease. J Neurol Phys Ther. (2016) 40(4):223–9. doi: 10.1097/NPT.0000000000000146
42. Pickering D, Horrocks LM, Visser KS, Todd G. “Every picture tells a story”: interviews and diaries with children with cerebral palsy about adapted cycling. J Paediatr Child Health. (2013) 49(12):1040–4. doi: 10.1111/jpc.12289
43. Shafizadeh M, Theis N, Davids K. Locomotor adaptations during RaceRunning in people with neurological motor disorders. Adapt Phys Act Q. (2019) 36(3):325–38. doi: 10.1123/apaq.2018-0155
44. Stone B, Mason BS, Warner MB, Goosey-Tolfrey VL. Shoulder and thorax kinematics contribute to increased power output of competitive handcyclists. Scand J Med Sci Sports. (2019) 29(6):843–53. doi: 10.1111/sms.13402
45. Valent LJ, Dallmeijer AJ, Houdijk H, Slootman HJ, Post MW, Van Der Woude LH. Influence of hand cycling on physical capacity in the rehabilitation of persons with a spinal cord injury: a longitudinal cohort study. Arch Phys Med Rehabil. (2008) 89(6):1016–22. doi: 10.1016/j.apmr.2007.10.034
46. Valent LJ, Dallmeijer AJ, Houdijk H, Slootman HJ, Janssen TW, Post MW, et al. Effects of hand cycle training on physical capacity in individuals with tetraplegia: a clinical trial. Phys Ther. (2009) 89(10):1051–60. doi: 10.2522/ptj.20080340
47. Valent L, Dallmeijer A, Houdijk H, Slootman HJ, Janssen TW, Van Der Woude LH. Effects of hand cycle training on wheelchair capacity during clinical rehabilitation in persons with a spinal cord injury. Disabil Rehabil. (2010) 32(26):2191–200. doi: 10.3109/09638288.2010.509461
48. Van der Linden ML, Van Schie PE, Hjalmarsson E, Andreopoulou G, Verheul MH, Von Walden F. Athlete-perceived impact of frame running on physical fitness, functional mobility and psychosocial outcomes. J Rehabil Med. (2022) 54. doi: 10.2340/jrm.v53.1393
49. van Schie PE, van Eck M, Bonouvrié LA, Edelman Bos AM, Buizer AI. The impact of frame running on quality of life in young athletes with mobility limitations. Front Sports Act Living. (2022) 4:839285. doi: 10.3389/fspor.2022.839285
50. Vogt T, Schneider S, Anneken V, Strüder HK. Moderate cycling exercise enhances neurocognitive processing in adolescents with intellectual and developmental disabilities. Res Dev Disabil. (2013) 34(9):2708–16. doi: 10.1016/j.ridd.2013.05.037
51. Williams H, Pountney T. Effects of a static bicycling programme on the functional ability of young people with cerebral palsy who are non-ambulant. Dev Med Child Neurol. (2007) 49(7):522–7. doi: 10.1111/j.1469-8749.2007.00522.x
52. Koipysheva E, Lebedinsky V, Koipysheva MA. Physical health (definition, semantic content, study prospects). In: Ardashkin IB, Iosifovich BV, Martyushev NV, editors. Research Paradigms Transformation in Social Sciences, vol 50. European Proceedings of Social and Behavioural Sciences. London: Future Academy (2018). 601–5. doi: 10.15405/epsbs.2018.12.73
53. World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice (Summary Report). Geneva, Switzerland: World Health Organization (2004).
54. Theofilou P. Quality of life: definition and measurement. Eur J Psychol. (2013) 9(1):150–62. doi: 10.5964/ejop.v9i1.337
55. Aitchison B, Rushton AB, Martin P, Barr M, Soundy A, Heneghan NR. The experiences and perceived health benefits of individuals with a disability participating in sport: a systematic review and narrative synthesis. Disabil Health J. (2022) 15(1):101164. doi: 10.1016/j.dhjo.2021.101164
56. Diaz R, Miller EK, Kraus E, Fredericson M. Impact of adaptive sports participation on quality of life. Sports Med Arthrosc Rev. (2019) 27(2):73–82. doi: 10.1097/JSA.0000000000000242
Keywords: impairment, disability, adaptive cycles, bicycling, health, mobility
Citation: Mosser N, Norcliffe G and Kruse A (2025) The impact of cycling on the physical and mental health, and quality of life of people with disabilities: a scoping review. Front. Sports Act. Living 6:1487117. doi: 10.3389/fspor.2024.1487117
Received: 27 August 2024; Accepted: 13 December 2024;
Published: 6 January 2025.
Edited by:
David Arthur Hart, University of Calgary, CanadaReviewed by:
Nadhir Hammami, University of Jendouba, TunisiaDelphine Labbé, University of Illinois Chicago, United States
Copyright: © 2025 Mosser, Norcliffe and Kruse. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annika Kruse, YW5uaWthLmtydXNlQHVuaS1ncmF6LmF0
 Nina Mosser
Nina Mosser Glen Norcliffe
Glen Norcliffe Annika Kruse
Annika Kruse