- Department of Psychiatry, Psychotherapy and Psychosomatics, Medical Faculty, Bezirkskrankenhaus Augsburg, University of Augsburg, Augsburg, Germany
Introduction: To date, concrete recommendations for physical activity in psychiatric treatments are limited. Thus, we evaluated knowledge, barriers and beliefs associated with exercise prescription of mental health professionals (MHP) to people with mental illnesses. We aimed to identify patients' barriers to exercise participation and to work out options addressing these barriers.
Methods: In our cross-sectional and questionnaire-based investigation, we recruited medical, nursing and therapeutic staff and patients of a psychiatric clinic by email and personal contact. Questionnaires contained the German versions of The Exercise in Mental Illness Questionnaire (EMIQ-G) and the International Physical Activity Questionnaires (IPAQ).
Results: We included 100 MHP and 100 patients. MHP had significantly more knowledge regarding positive effects of exercise on general health than patients. Exercise was prescribed mostly (48.4%) or always (37.9%) by MHP. The data showed missing education in exercise prescriptions and different recommendation behavior. Male patients seemed to experience exercise more often as a positive distraction and had lower physical health barriers than females.
Discussion: Physical activity needs to be more integrated in psychiatric treatments. Some strategies as educating MHP and patients regarding potential benefits of exercise via psychoeducative brochures and adapting recommendations to individual symptoms could improve exercise behavior in psychiatric patients.
1 Introduction
Regular physical activity is associated with many benefits for mental health (1): a meta-analysis of 25 randomized controlled trials (9 studies with major depressive disorder) was able to show a significant positive effect of physical activity on depressive symptoms (2). Further studies confirmed that aerobic endurance exercise (3) and physical activity in general (4) improve cognitive functioning in people with schizophrenia. Also, anxiety symptoms (5–7) and substance use disorders (8) can beneficially be influenced by physical activity.
Otherwise, data from 168 countries (representing 96.0% of the global population) showed that 27.5% of all adults were not sufficiently physical active (9). Several studies confirmed that sedentary lifestyle may increase the risk of obesity, cardiovascular diseases, diabetes, reduce quality of life and can contribute to the development of mental illnesses (10). The current WHO (World Health Organization) recommendations for physical activity levels in healthy adults (18–65 years) include a weekly amount of at least 150 min of moderate-intense physical activity, 75 min of vigorous-intense physical activity or a combination of moderate- and vigorous-intense exercise. In addition, 2–3 strength units per week of all large muscle groups are recommended (11).
In recent years, there has been increasing interest from researchers and mental health professionals (MHP) in physical activity as a means of improving and preventing mental symptoms (12). However, most patients with mental disorders have lower levels of physical activity compared to a healthy population (13). Individuals with mental disorders experience a range of barriers preventing them from engaging in regular physical activity, such as low mood, high levels of perceived stress, lack of social support and negative beliefs about capabilities (14–16). Therefore, there is a need for feasible and efficacious treatment options to overcome these barriers and to sustainably increase physical activity in patients with mental disorders. For such lifestyle changes towards more physical activity, patients with mental illnesses need the support and advice of MHP (17) because especially physicians, psychologists and nurses play an important role in providing information on health behavior to their patients (18).
To date, concrete recommendations or prescriptions for physical activity in psychological or psychiatric treatments are limited (19). In the US, less than one in three adults with symptoms of depression received advice from a healthcare provider regarding physical activity or exercise (19). This is in contrast to other medical specializations such as cardiology, where physical activity has already been well integrated into clinical therapy with specific recommendations for cardiovascular diseases (20). Physical exercise in mental illnesses can improve not only mental but also physical symptoms at the same time.
The vast majority of MHP in different parts of the world have stated that they hold a positive attitude towards exercise and prescribe it to their patients with mental illnesses (21–25). For example, a German study reported that most MHP recommend physical activity to some (N = 82, 54.5%) or all of their patients (N = 51, 33.8%) (25) while in an Australian study, Stanton et al. found that 72% of nurses reported prescribing exercise to patients with mental illnesses (24). Several barriers to the implementation of approaches to promote physical activity into clinical standard care in the psychiatric setting have been identified. Some of the main barriers include a lack of knowledge on the benefits of physical activity (26, 27) and lack of formal education or practice in the promotion of physical activity (23, 27, 28). However, most studies did not examine patients with mental disorders themselves, but only health professionals. Therefore, quantitative studies investigating psychiatric patients' perspectives are lacking.
The promotion of physical activity is required to improve daily life functions and to delay the progression of several mental and physical diseases. To take full advantage of the positive effects of physical activity, it is imperative that especially MHP are well placed to identify individual needs for exercise promotion and to support people with mental illness in being physically active.
1.1 Aim
In that regard, the aim of the present study was to evaluate knowledge, barriers and beliefs, including the importance, benefits and correlations associated with exercise prescription and recommendation by MHP to people with mental illnesses. Further, we aimed to identify patients' barriers to participation in exercise and to work out options addressing barriers of both MHP and patients. Finally, we aimed to identify sex differences in patients in order to be able to make sex-related conclusions and to give more specific exercise recommendations in clinical treating.
2 Methods
This study was a cross-sectional and questionnaire-based investigation into the knowledge, attitudes, beliefs and behaviors of health professionals working with patients with mental illnesses, regarding the role of exercise in the treatment of mental illnesses. In addition, we examined psychiatric patients' knowledge, barriers and expectations regarding the role of physical activity in their daily life and compared both perspectives.
2.1 Subjects
MHP of the psychiatric clinic of Psychiatry, Psychotherapy and Psychosomatics of the University Augsburg (Augsburg, Germany) and the oncological clinic of the university hospital Augsburg (CCCA—Comprehensive Cancer Center Augsburg) were recruited by email and personal contact. MHP are all clinical employees who are in direct contact with patients and are employed. In CCCA, MHP work with physically ill patients who often have comorbid mental health symptoms. Patients in the psychiatric clinic of Psychiatry, Psychotherapy and Psychosomatics of the University Augsburg (Augsburg, Germany) were recruited by personal contact without restrictions regarding their psychiatric diagnoses. The study size planning was based on a comparison (independent t-test) between mental health professionals and patients and their level of physical activity. With an expected effect size of 0.4, an α = 0.05 and a statistical power of 1–ß = 0.8, 100 participants must be recruited per group. Thus, a total of 200 participants (100 MHP, 100 patients) were recruited. Our inclusion criteria were sufficient German language, age range between 18 and 65 years, voluntary treatment and ability to consent. The participants who had contradiction for physical activity were not included in the study.
2.2 Ethics and registration
The study was conducted in accordance with the guiding principles of the Declaration of Helsinki 2008, local laws and regulations. The study protocol was approved by the ethics committee of the Ludwig-Maximilian University Munich (approval number 21-0462). The study was registered at https://www.drks.de (DRKS-ID: DRKS00025970). All participants provided written informed consent before inclusion in the study.
2.3 Instruments
2.3.1 EMIQ
Mental health professionals' knowledge about physical activity in people with mental illnesses was evaluated with the German version of The Exercise in Mental Illness Questionnaire (EMIQ-G) (29). The instrument is a self-report questionnaire containing 65 items assigned to 6 domains: (1) Knowledge on physical activity (2) Beliefs/Attitudes concerning physical activity (3) Recommendation/Prescription behavior (4) Barriers concerning physical activity (5) Physical activity behavior and (6) Demographics (29). As there is no validated version for patients, we adapted the questionnaire for this purpose containing 36 items assigned to 4 domains: (1) Knowledge on physical activity (2) Barriers concerning physical activity (3) Incentives concerning exercise participation (4) Expectations concerning regular exercise (see Supplementary Material S1).
2.3.2 Physical activity
We used the International Physical Activity Questionnaires (IPAQ) to evaluate detailed information about daily activity including physical exercise as well as physical activity in daily routines (30). MET (metabolic equivalent of task minutes) (31) per week were calculated as recommended by Craig et al. (30). There is already a German translation of the International Physical Activity Questionnaire—Short Form (IPAQ-SF) (32). Previous studies revealed high correlations of physical activity measured with accelerometers to the questionnaire (33).
2.4 Statistical data analysis
All analyses were conducted using SPSS 29.0 (IBM, Armonk, NY, USA), with a significance level of alpha <0.05. Descriptive statistics were used to report respondent participants' characteristics and answers regarding knowledge, beliefs, behaviors and barriers. Demographic and clinical differences between groups of MHP and patients were assessed using Mann–Whitney-U Test due to violation of the normal distribution (Shapiro–Wilk Tests, p < 0.05). Homogeneity of variances was tested with the Levene's test. Fisher's-Freeman–Halton Test was used to analyse sex contribution (female, male, divers) between the two groups MHP and patients (34). The effect size r for Mann–Whitney-U Tests was calculated when comparing the sex differences in patients according to Cohen (35). In a separate analysis and in order to present the knowledge (summed score of the six questions) and the barriers (summed score from the 16 questions), we used the mean response from the levels of agreement questions. Differences in respondents' (MHP vs. patients) summed scores were examined using Mann–Whitney-U Test based on Stanton et al. (27). All datasets were screened for plausible values. Only items that were filled out correctly and completely were included in the data analysis.
3 Results
3.1 Participants characteristics
Of the 100 MHP, 11 were medical doctors, 30 were psychologists, 37 were nurses, 10 were specialized therapists, 7 were physiotherapists or sports therapists and 5 medical doctors were of CCCA. Of the 100 patients, 90 were inpatients and 10 were outpatients at the time of inclusion. All patients had a main diagnosis according to ICD-10 (F1:1, F2:4, F3:92, F4:2, F5:1). Almost all patients (N = 83/97) reported taking psychotropic drugs, including antidepressants (78/83), antipsychotics (42/83), anxiolytics (23/83) or stimulants (2/83).
Significant differences between both groups regarding sex, age, BMI, education, and IPAQ are presented in Table 1.
3.2 Knowledge regarding the benefits of exercise
Of all MHP (N = 100), only 97 participants reported whether they had ever received any formal training in exercise prescription, 3 gave no answer. Of these, only 19 participants (19.6%) had received one and 78 (80.4%) had received none. Additional questions were only asked to participants who had received formal training (N = 19). All 19 participants (3 doctors, 5 psychologists, 5 nurses, 6 physiotherapists or sports therapists) referred to their professional education when asked to specify the formal training. Ten participants rated their knowledge of exercise prescription for people with mental illness as “Good” (N = 8, 42.1%) or “Excellent” (N = 2, 10.5%). Fourteen participants rated their confidence to prescribe exercise to people with mental illness as “Good” (N = 9, 47.4%) or “Excellent” (N = 5, 26.3%).
Comparing MHP and patients, the results of the Mann–Whitney-U Tests showed that MHP knew significantly more regarding the beneficial effects of exercise in cholesterol level (p = 0.004), blood pressure (p < 0.001), depression (p < 0.001) and risk of cancer (p < 0.001) than patients. However, basic knowledge seems to be missing., e.g., 18.0% of MHP did not know for sure that physical activity is preventive regarding the development of depression. The results of the sum score (mean response from the six question) revealed that MHP had significantly more knowledge overall than the patients (U = 2,609.0, Z = −4.775, p < 0.001). Detailed information about the participant's response is shown in the Supplementary Table S1.
3.3 Mental health professionals' perspective
3.3.1 Beliefs regarding exercise
MHP were asked to rank the importance of several treatment strategies in people with mental illness. Only 75 participants fully completed this item. Medication (N = 22, 29.7%) was ranked first most frequently, followed by social support (N = 17, 23.0%), electroconvulsive therapy (N = 7, 9.5%), social skills training (N = 6, 8.1%), psychotherapy (N = 5, 6.8%), vocational rehabilitation (N = 4, 5.4%), family therapy (N = 4, 5.4%), hospitalization (N = 3, 4.1%) and light therapy (N = 3, 4.1%). Exercise (N = 3, 4.1%) was least frequently ranked on first position, but mostly on fourth position (N = 27, 36.5%).
3.3.2 Behavior of exercise prescription
Frequency of exercise prescription
This question (Q16) only applied to MHP (N = 95). 36 respondents (37.9%) reported Always prescribing exercise, 46 (48.4%) reported prescribing exercise Most of the time, 13 (13.7%) reported prescribing exercise Occasionally and none reported Never prescribing exercise.
Behavior in recommending exercise
Table 2 shows MHP behavior in recommending exercise (explaining to patients what to do and how to do it) to people with mental illnesses. Brochures were named very rarely (13.5%) as a possible method prescribing exercise to people with a mental illness. Personal discussion/recommendation (88.5%) is used the most, followed by referral to an exercise professional (43.8%). The practices of MHP regarding the type, the duration and the intensity of physical activity were very different. However, aerobic exercise (92.6%) was named the most as a possible type of exercise training. MHP stated that they most often recommend 20 min (30.9%) or 30 min (31.9%) per session and mostly in a moderate intensity (44.6%).
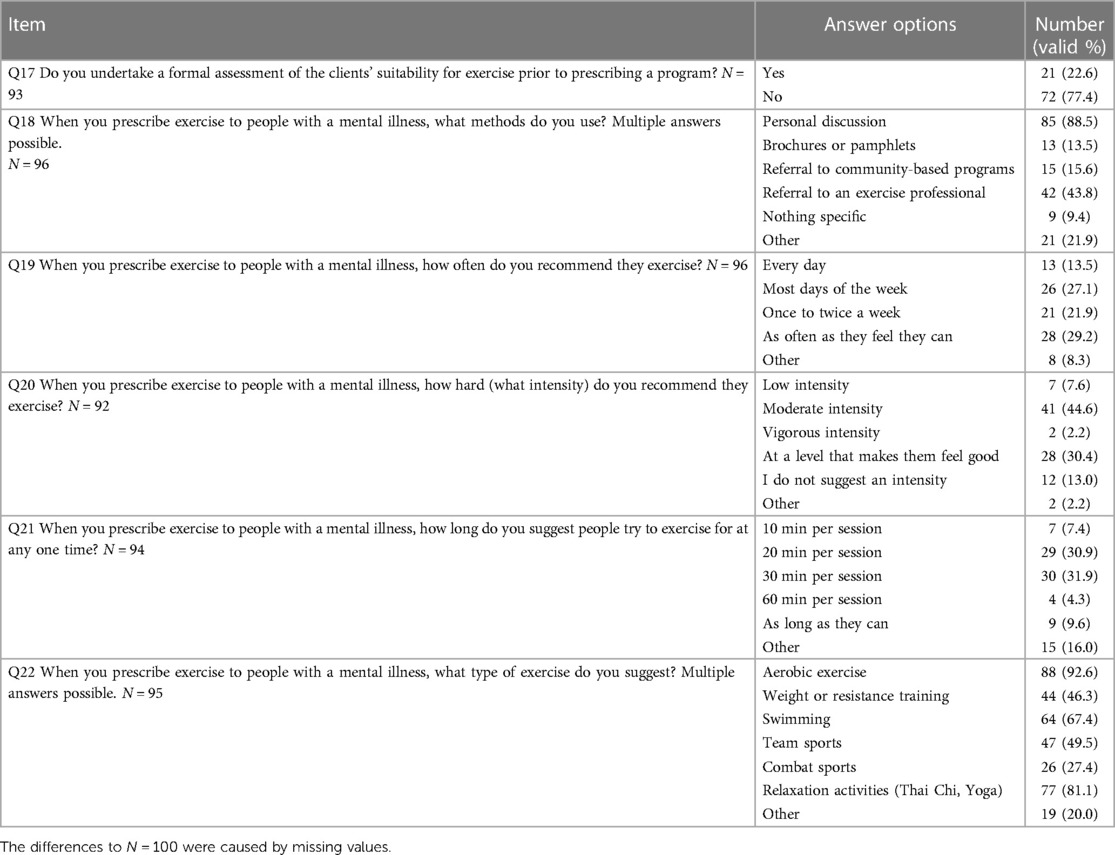
Table 2. Behavior (Q17–Q22) regarding exercise for patients with mental illnesses of mental health professionals.
3.3.3 Barriers to exercise prescription
MHP responses to statements regarding the barriers to exercise prescription for people with mental illness are shown in Table 3. The data showed low organizational barriers (e.g., Q30 too excessive workload: 50.0% strongly disagree; Q31 not part of their job: 52.1% strongly disagree).
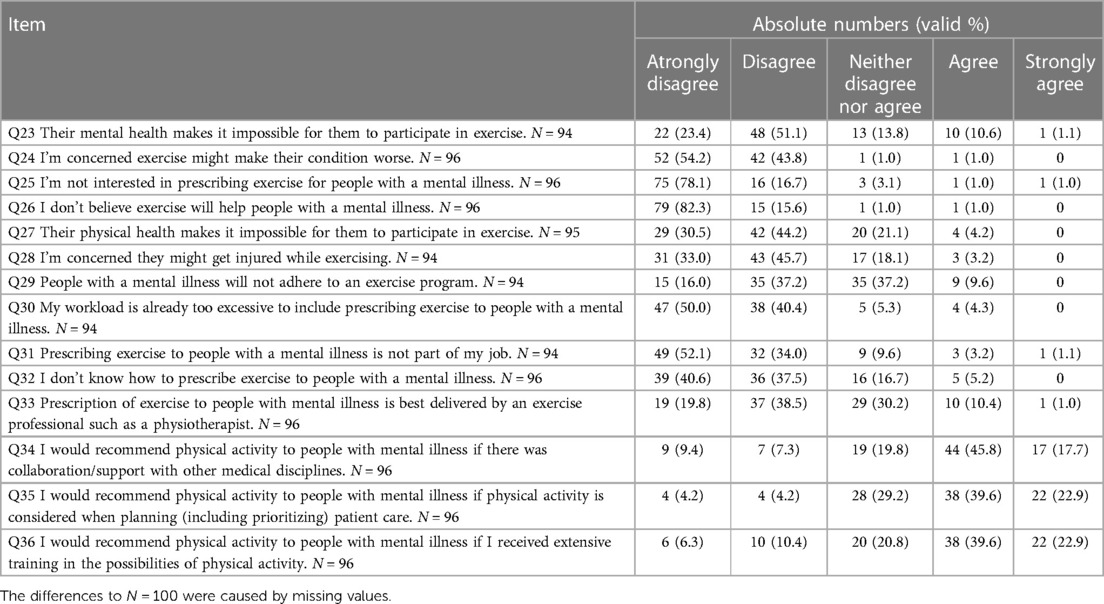
Table 3. Levels of agreement by mental health professionals with statements regarding barriers to exercise prescriptions (Q23–Q36) for patients with mental illnesses.
3.4 Patients' perspective
For the final analysis and sex comparisons, only patients who indicated male or female were included. The sample size of the sex diverse (N = 3) was too small for further sex-related comparisons.
3.4.1 Motivating factors and barriers towards exercise
We summarized the questionnaire's categories of incentives and expectations as the motivating factors towards exercise in patients with mental illnesses. In part, we identified significant differences in males and females with a weak to moderate effect. We compared whether the barriers to exercise participation experienced by patients with mental illness corresponded to MHP assumptions regarding these barriers. The statements largely matched, except for the statement that they believe physical activity will not help psychiatric patients. More details can be seen in the Supplementary Table S2.
3.4.2 Sex differences
The results of the Mann–Whitney-U Tests revealed that males were more likely to have positive expectations of regular exercise than females [e.g., reduced need in medication (Q26) or positive distraction (Q33)]. Otherwise, female participants expected less improvement in their health values (Q27) than males. Regarding barriers to exercise participation, females showed more negative associations with exercise than males in the statements of well-being (Q12), of confidence (Q18), of safe place (Q21) and of physical health (Q20) [e.g., weight (Q19)]. Social support (Q16) was experienced as a greater barrier by men compared to women. More details can be seen in Table 4.
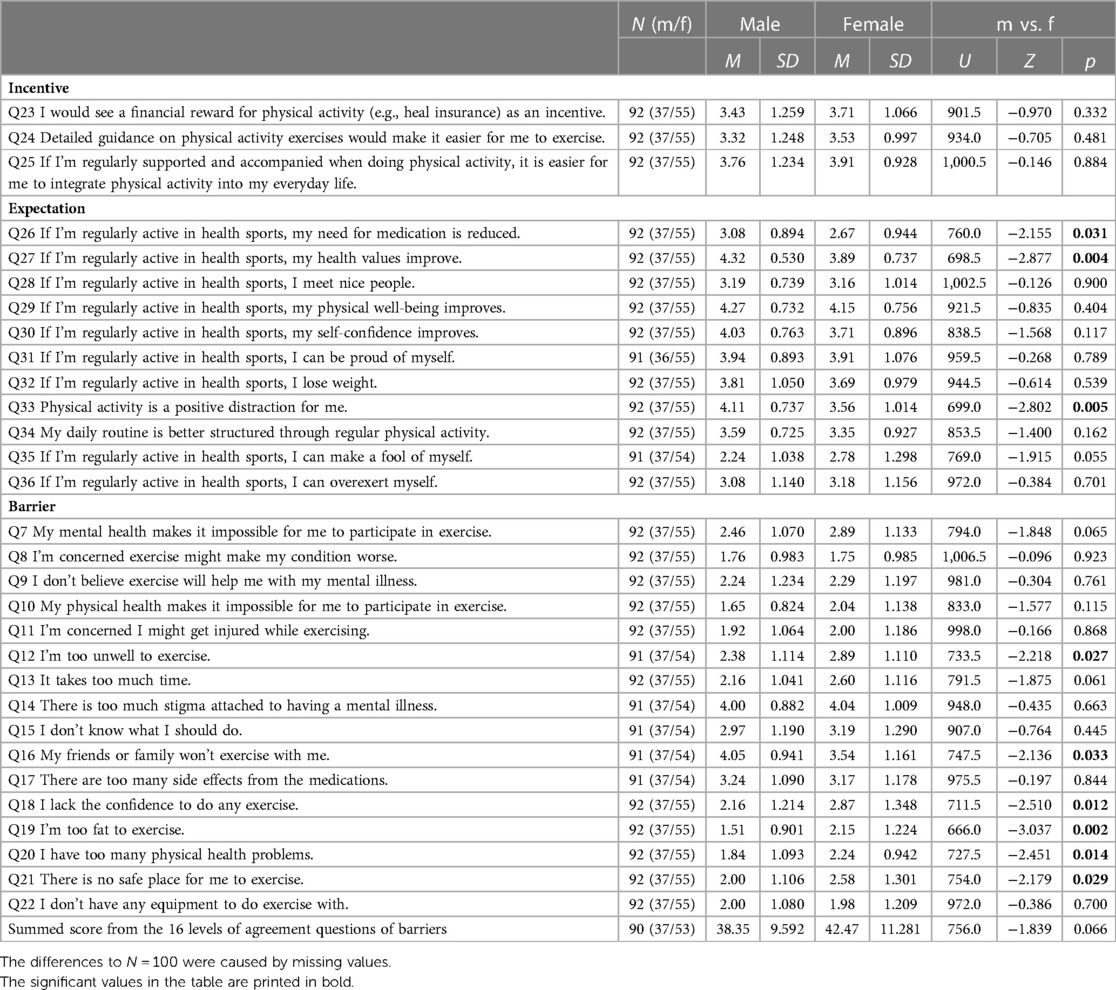
Table 4. Motivating factors (incentives Q23–Q25 and expectations Q26–Q36) and barriers (Q7–Q22) regarding exercise for patients with mental illnesses and comparison between males (m) and females (f) within the patients.
4 Discussion
With the present study, we evaluated the knowledge, beliefs, barriers and behaviors of MHP regarding exercise for people with mental illnesses combined with patients' perspective and sex differences in patients' exercise participation using the EMIQ-G.
4.1 Knowledge regarding the benefits of exercise (MHP and patients)
The results of the “knowledge” section indicate that both groups (MHP and patients) already knew a lot about the benefits of exercise. Contrary to other studies (22, 36, 37), we addressed the physical benefits of regular exercise including cholesterol level, blood pressure, depression and risk of cancer. Our data showed that MHP knew more than patients. This finding suggests a relationship between education level and knowledge about physical activity since our MHP had higher levels of education than the patients. Nevertheless, gaps in knowledge about the very basic effects of physical activity on several disorders can be recognized, e.g., only 67% knew that exercise can prevent the development of chronic diseases, only 85% knew that physical activity can lower total blood cholesterol levels, only 79% of MHP are aware of physical activity in the prevention of depression and only 60% knew for sure that physical activity may reduce the risk of cancers.
However, most MHP (78.0%) reported that they had never received any formal training in exercise prescription, which is in line with a previously published study that examined MHP's knowledge, attitudes and behaviors regarding exercise for patients with a mental illness in forensic psychiatric inpatient care (22). The authors revealed that out of the 239 participants, only 39 (16.3%) stated that they had undergone formal training in exercise prescription emphasizing that expertise in exercise is of importance to patient adherence (22). Of our 19 MHP (19.6%) that had received formal training, all referred to their professional education when asked to specify the formal training. However, most of our employees were still untrained which is also criticized in another study that evaluated 73 MHP's knowledge about exercise in people with mental illness in Brazil (23). The authors suggested that it is necessary to include physical activity and exercise training in mental health curricula.
Due to the importance of exercise in mental illness treatment, all MHP should acquire sufficient knowledge to be able to recommend a more active lifestyle for their patient. Handing out brochures about the positive effects or even concrete training recommendations could be a useful tool for promoting more exercise as it is time efficient, easy to distribute and realizable in a short period of time.
4.2 Mental health professionals' perspective
4.2.1 Beliefs regarding exercise
Medication was ranked as the most important therapeutic option by MHP, while exercise was ranked scarcest on first position. This is in line with another study which stated that exercise is important, but also named medication first (23). Nevertheless, with increasing recognition of the benefits of exercise, we emphasize the importance of integrating exercise into clinical practice guidelines as an essential complement to the treatment of mental illnesses (38).
4.2.2 Behavior of exercise prescription
Despite only part of the MHP (19.0%) stated that they had undergone formal training, they prescribed exercise most of the time (48.4%) or always (37.9%). This is especially positive comparing data in severe mental illnesses (23) and forensic psychiatric care (22) where partially 40%–50% of MHP never prescribe physical activity. However, it seems that brochures were hardly used and especially the MHP group of nurses used “referral to an exercise professional” more often than other methods of promoting exercise. Developing specific booklets might be a low-threshold method in order to provide helpful information and recommendation for exercise in people with mental illnesses. Further, our MHP seemed to give different recommendations for exercise regarding the type, duration, and intensity of the activity, which apparently do not follow current guidelines. It would be more consistent to provide standardized recommendations (e.g., WHO guidelines), with the option of individual adjustment for psychiatric patient. Following the FITT (frequency, intensity, time, type) principle (39) may facilitate MHP to recommend consistent training instructions, as previously indicated by Lee et al. (40).
4.2.3 Barriers to exercise prescription
In general, the barriers inquired were not very high. More than 85.0% of the MHP Strongly Disagree (52.1%) or Disagree (34.0%) with the statement that prescribing exercise to people with a mental illness is not part of their job. This is consistent with previous research (37, 41, 42), showing nurses working in mental health would believe that exercise prescription is part of their role. However, in contrast to other studies (43, 44), respondents in the present study indicated that current workloads are not a barrier to exercise prescription (50.0% Strongly Disagree and 40.4% Disagree). This is an important finding since previous studies suggested that exercise prescription would extend to systemic barriers such as competing priorities, limited resources and fragmentation of the health care system in which they work (18, 43, 45). Despite the reported low organizational barriers in prescribing exercise in our study, the potential of exercise within the multidisciplinary treatment needs to be further developed. Brochures and the training of individuals (e.g., one expert on every ward) could help to overcome possible barriers.
4.3 Patients' perspective
4.3.1 Motivating factors and barriers towards exercise
When being regularly active in health sports, our patients expected consistently positive effects. In accordance with previous finding (46, 47), our patients tended to be less active and had a higher BMI than the general population/MHP. Quantitative studies providing data on motivating factors towards exercise among patient with mental illnesses established losing weight (83.0% of patients), improving mood (81.0%) and reducing stress (78.0%) as the most common motivation (15). However, according to our data, there might be a higher level of interest in being more active with a financial reward (e.g., bonus in health insurance, free or discounted gym membership), with detailed training counselling and regular exercise support. Supervision by trained exercise professionals is a factor for stable adherence rates in people with depression (48). Patients with mental illnesses experienced several barriers that would make it difficult to take full advantage of the benefits associated with physical activity. The results revealed that patients agreed with several statements located at socio-ecological level where stigma and lack of support from their family and friends were considered as major barriers to engage in exercise. Social support is a potential moderator catching patients' volition to exercise. It has been shown that those who exercise with others may have extra health benefits compared to exercising alone (49). Thus, it might be of great benefit encouraging patients to exercise with friends or family (50) or providing group activities in a mental health setting.
4.3.2 Sex differences
Concerning sex differences in patients, our data revealed interesting evidence. Males seemed to experience exercise more often as a positive distraction than females and seemed to have less physical health barriers to exercise (e.g., feeling unwell, feeling too fat). In some patients, depressive episodes present with higher values of irritability and anger rather than sadness and low self-esteem, which is more often the case in male patients (51). Our data have two main implications in this regard: first, in order to find ways to manage impulsiveness and inner restlessness, exercise programs with high intensity might be helpful in reducing such symptoms. This could be the reason that male patients in our cohort experienced more positive distractions from exercise. Second, developing exercise activities in order to overcome low self-esteem and physical health related barriers (more often named by female participants), activities done with others of the same gender (e.g., only-women groups) or at the same level of ability, exercising alone or with low intensity might be helpful for this female patient group (52). In summary, our findings could help to personalize our training recommendations in order to target more specific symptoms and thereby to motivate more patients to exercise.
4.4 Limitations
Some limitations need to be considered when interpreting our data. First, all results must be interpreted with caution because more female MHP and patients participated in the study. Some of our results (EMIQ, demographics) are based on self-reported data, derived from questionnaires and surveys administered to patients and MHP. Therefore, the results could be affected by response bias, or participations lacking interest or experience with exercise to accurately describe knowledge, barriers or motivation factors. We measured daily activity level in patients with mental illness only by the questionnaire IPAQ-SF (32). Although there are high correlations between this questionnaire and accelerometers (33), the assessment of physical activity was self-reported in this study and patients may have been inclined to overrate, for example, moderate activities as vigorous activities, as previously discussed by Petzold et al. (53). For future studies and individual diagnosis, the authors recommend a combination of both self-reported and objective measurements at the same time (53). We could not explore the differences between MHP in detail due to a small number of participants from each profession group. Future studies should investigate these limitations and include a greater number of MHP from all areas. It should also be considered that the large majority of patients (92.0%) had a diagnosis of affective disorders, while schizophrenia, dissociative disorders, eating disorder and mental and behavioral disorders were relatively under-represented among our included patients. Thus, future research should examine if the same identified barriers and motivation factors towards exercise also generalize to patients with other mental illnesses. Additionally, the positive results from MHP statements (e.g., high frequency of exercise prescription) can possibly be explained because clinical staff with high interest in exercise or physical activity were more likely to participate in this study.
5 Conclusion
Exercise offers great potential to improve mental and physical health of people with mental illnesses. There is now an abundance of data demonstrating that physical activity needs to be more integrated, recommended and prescribed in the clinical context of treating mental illnesses. However, due to this importance, all MHP should acquire sufficient knowledge to be able to educate the positive effects of exercise and to recommend a more active lifestyle for their patients. Additionally, being/becoming physically active and seeing oneself responsible as a role model may increase the authenticity of physical activity recommendations and facilitate exercise uptake.
In light of the results of the present study as well as based on research on the positive effects of exercise for patients with mental illness in general, in addition to the implementation of these findings within concrete recommendations in therapeutic guidelines, strategies can help to assist uptake and continuation of exercise in order to consider the benefits of exercise beyond the physical domain:
(1) Educating MHP and patients on the potential benefits of physical activity in a time efficient and easily accessible way, e.g., via psychoeducative brochures.
(2) Providing consistent exercise recommendations (e.g., WHO guidelines).
(3) Adapting exercise prescription should account for personal preferences and previous experiences in terms of making it the most enjoyable experience.
(4) Offering specific exercise intervention, e.g., supervised exercise interventions, training with detailed guidance and regular support or financial reward for physical activity.
(5) Developing exercise activities that address specific symptoms, e.g., high intensity workouts to manage impulsiveness and inner restlessness (more often seen in male patients with depression) or low-intensity groups/smaller groups/female-only groups to overcome low self-esteem and health-related barriers (more often seen in female patients with depression).
(6) Encouraging patients to exercise with family and friends or to participate in peer groups.
Increased use of exercise in psychiatric care, individually adapted to the patients' needs is important in order to address psychiatric symptoms.
Data availability statement
The datasets generated for this study are available on request to the corresponding author.
Ethics statement
The studies involving humans were approved by The Ethics Committee of the Ludwig-Maximilians University Munich. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AHi, AR and AHa conceptualized the study. AHi and DK wrote the first draft of the manuscript. AHi, DK and HS collected data. AHi and DK made the statistical analyses. All authors revised the manuscript critically and have approved the final manuscript.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article.
This work was funded by an intramural grant of Medical Faculty (University of Augsburg) to AR (Sport study Move = Motivation for Exercise).
Acknowledgments
The project was carried out using the clinical trials infrastructure of the DZPG (German Center for Mental Health) [FKZ: 01EE2303C]. We thank all participants of the trial and the whole study group.
Conflict of interest
Within the last 6 years, AH has received paid speakerships from Janssen, Otsuka, Recordati, and Lundbeck. He was member of Rovi, Recordati, Otsuka, Lundbeck, and Janssen advisory boards. He is the editor of the German AWMF S3 and the WFSBP schizophrenia guidelines. S-KG is an advisory board member of the GOLDKIND Stiftung.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer MP declared a past co-authorship with the author AR to the handling editor.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fspor.2024.1336356/full#supplementary-material
References
1. Tamminen N, Reinikainen J, Appelqvist-Schmidlechner K, Borodulin K, Mäki-Opas T, Solin P. Associations of physical activity with positive mental health: a population-based study. Ment Health Phys Act. (2020) 18:100319. doi: 10.1016/j.mhpa.2020.100319
2. Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J Psychiatr Res. (2016) 77:42–51. doi: 10.1016/j.jpsychires.2016.02.023
3. Firth J, Stubbs B, Rosenbaum S, Vancampfort D, Malchow B, Schuch F, et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull. (2017) 43(3):546–56. doi: 10.1093/schbul/sbw115
4. Dauwan M, Begemann MJH, Slot MIE, Lee EHM, Scheltens P, Sommer IEC. Physical exercise improves quality of life, depressive symptoms, and cognition across chronic brain disorders: a transdiagnostic systematic review and meta-analysis of randomized controlled trials. J Neurol. (2021) 268(4):1222–46. doi: 10.1007/s00415-019-09493-9
5. Gordon BR, McDowell CP, Lyons M, Herring MP. Resistance exercise training for anxiety and worry symptoms among young adults: a randomized controlled trial. Sci Rep. (2020) 10(1):17548. doi: 10.1038/s41598-020-74608-6
6. Schuch FB, Stubbs B, Meyer J, Heissel A, Zech P, Vancampfort D, et al. Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress Anxiety. (2019) 36(9):846–58. doi: 10.1002/da.22915
7. Stubbs B, Vancampfort D, Rosenbaum S, Firth J, Cosco T, Veronese N, et al. An examination of the anxiolytic effects of exercise for people with anxiety and stress-related disorders: a meta-analysis. Psychiatry Res. (2017) 249:102–8. doi: 10.1016/j.psychres.2016.12.020
8. Giménez-Meseguer J, Tortosa-Martínez J, Cortell-Tormo JM. The benefits of physical exercise on mental disorders and quality of life in substance use disorders patients. Systematic review and meta-analysis. Int J Environ Res Public Health. (2020) 17(10):1–36.. doi: 10.3390/ijerph17103680
9. Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. (2018) 6(10):e1077–86. doi: 10.1016/S2214-109X(18)30357-7
10. Cunningham C, O’Sullivan R, Caserotti P, Tully MA. Consequences of physical inactivity in older adults: a systematic review of reviews and meta-analyses. Scand J Med Sci Sports. (2020) 30(5):816–27. doi: 10.1111/sms.13616
11. Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. (2020) 54(24):1451–62. doi: 10.1136/bjsports-2020-102955
12. Ashdown-Franks G, Sabiston CM, Stubbs B. The evidence for physical activity in the management of major mental illnesses: a concise overview to inform busy clinicians’ practice and guide policy. Curr Opin Psychiatry. (2019) 32(5):375–80. doi: 10.1097/YCO.0000000000000526
13. Mangerud WL, Bjerkeset O, Lydersen S, Indredavik MS. Physical activity in adolescents with psychiatric disorders and in the general population. Child Adolesc Psychiatry Ment Health. (2014) 8(1):2. doi: 10.1186/1753-2000-8-2
14. Ussher M, Stanbury L, Cheeseman V, Faulkner G. Physical activity preferences and perceived barriers to activity among persons with severe mental illness in the United Kingdom. Psychiatr Serv. (2007) 58(3):405–8. doi: 10.1176/ps.2007.58.3.405
15. Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med. (2016b) 46(14):2869–81. doi: 10.1017/S0033291716001732
16. Glowacki K, Duncan MJ, Gainforth H, Faulkner G. Barriers and facilitators to physical activity and exercise among adults with depression: a scoping review. Ment Health Phys Act. (2017) 13:108–19. doi: 10.1016/j.mhpa.2017.10.001
17. Verhaeghe N, De Maeseneer J, Maes L, Van Heeringen C, Annemans L. Perceptions of mental health nurses and patients about health promotion in mental health care: a literature review. J Psychiatr Ment Health Nurs. (2011) 18(6):487–92. doi: 10.1111/j.1365-2850.2011.01692.x
18. Happell B, Platania-Phung C, Scott D. Physical health care for people with mental illness: training needs for nurses. Nurse Educ Today. (2013) 33(4):396–401. doi: 10.1016/j.nedt.2013.01.015
19. Grabovac I, Stefanac S, Smith L, Haider S, Cao C, Jackson SE, et al. Association of depression symptoms with receipt of healthcare provider advice on physical activity among US adults. J Affect Disord. (2020) 262:304–9. doi: 10.1016/j.jad.2019.11.023
20. Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, et al. 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. (2021) 42(1):17–96. doi: 10.1093/eurheartj/ehaa605
21. Vancampfort D, Stanton R, Probst M, De Hert M, van Winkel R, Myin-Germeys I, et al. A quantitative assessment of the views of mental health professionals on exercise for people with mental illness: perspectives from a low-resource setting. Afr Health Sci. (2019) 19(2):2172–82. doi: 10.4314/ahs.v19i2.42
22. Bergman H, Nilsson T, Andiné P, Degl'Innocenti A, Thomeé R, Gutke A. The use of physical exercise in forensic psychiatric care in Sweden: a nationwide survey. J Ment Health. (2021) 30(1):1–9. doi: 10.1080/09638237.2021.1875406
23. Kleemann E, Bracht CG, Stanton R, Schuch FB. Exercise prescription for people with mental illness: an evaluation of mental health professionals’ knowledge, beliefs, barriers, and behaviors. Braz J Psychiatry. (2020) 42(3):271–7. doi: 10.1590/1516-4446-2019-0547
24. Stanton R, Happell B, Reaburn P. Investigating the exercise-prescription practices of nurses working in inpatient mental health settings. Int J Ment Health Nurs. (2015) 24(2):112–20. doi: 10.1111/inm.12125
25. Petzold MB, Ernst F, Spitzer U, Gabrysch J, Schweinfurth N, Satorius N, et al. Ärztliche Vorbildfunktion bezüglich körperlicher Aktivität für Patienten mit psychischen Erkrankungen. Psychotherapeut. (2020) 65(3):167–75. doi: 10.1007/s00278-020-00421-1
26. Carlbo A, Claesson HP, Åström S. Nurses’ experiences in using physical activity as complementary treatment in patients with schizophrenia. Issues Ment Health Nurs. (2018) 39(7):600–7. doi: 10.1080/01612840.2018.1429508
27. Way K, Kannis-Dymand L, Lastella M, Lovell GP. Mental health practitioners’ reported barriers to prescription of exercise for mental health consumers. Ment Health Phys Act. (2018) 14:52–60. doi: 10.1016/j.mhpa.2018.01.001
28. Kinnafick F-E, Papathomas A, Regoczi D. Promoting exercise behaviour in a secure mental health setting: healthcare assistant perspectives. Int J Ment Health Nurs. (2018) 27(6):1776–83. doi: 10.1111/inm.12484
29. Petzold MB, Frank G, Bendau A, Plag J, Betzler F, Ströhle A. The German version of the exercise in mental illness questionnaire (EMIQ-G): translation and testing of psychometric properties. Ment Health Phys Act. (2020) 19:100353. doi: 10.1016/j.mhpa.2020.100353
30. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. (2003) 35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
31. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. (2011) 43(7):1334–59. doi: 10.1249/MSS.0b013e318213fefb
32. Hagströmer M, Oja P, Sjöström M. The international physical activity questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. (2006) 9(6):755–62. doi: 10.1079/PHN2005898
33. Mäder U, Martin BW, Schutz Y, Marti B. Validity of four short physical activity questionnaires in middle-aged persons. Med Sci Sports Exerc. (2006) 38(7):1255–66. doi: 10.1249/01.mss.0000227310.18902.28
34. Freeman GH, Halton JH. Note on an exact treatment of contingency, goodness of fit and other problems of significance. Biometrika. (1951) 38(1–2):141–9. doi: 10.1093/biomet/38.1-2.141
36. Carraro A, Gobbi E, Stanton R, Santi G, Rosenbaum S. Psychometric properties of the Italian version of the Emiq-Hp (exercise in mental illness questionnaire-health professionals version) to investigate the views of health professionals regarding exercise for treatment of mental illness. Clin Neuropsychiatry. (2023) 20(1):55–60. doi: 10.36131/cnfioritieditore20230107
37. Stanton R, Reaburn P, Happell B. Barriers to exercise prescription and participation in people with mental illness: the perspectives of nurses working in mental health. J Psychiatr Ment Health Nurs. (2015) 22(6):440–8. doi: 10.1111/jpm.12205
38. Ashdown-Franks G, Firth J, Carney R, Carvalho AF, Hallgren M, Koyanagi A, et al. Exercise as medicine for mental and substance use disorders: a meta-review of the benefits for neuropsychiatric and cognitive outcomes. Sports Med. (2020) 50(1):151–70. doi: 10.1007/s40279-019-01187-6
39. American College of Sports M, Thompson WR, Gordon NF, Pescatello LS. ACSM’s Guidelines for Exercise Testing and Prescription. 8th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins (2010).
40. Lee YH, Kim H, Cho H. The effectiveness of physical activity interventions on depression in Korea: a systematic review and meta-analysis. Healthcare. (2022) 10(10):1886. doi: 10.3390/healthcare10101886
41. Faulkner G, Biddle S. Mental health nursing and the promotion of physical activity. J Psychiatr Ment Health Nurs. (2002) 9:659–65. doi: 10.1046/j.1365-2850.2002.00520.x
42. Robson D, Haddad M, Gray R, Gournay K. Mental health nursing and physical health care: a cross-sectional study of nurses’ attitudes, practice, and perceived training needs for the physical health care of people with severe mental illness. Int J Ment Health Nurs. (2013) 22(5):409–17. doi: 10.1111/j.1447-0349.2012.00883.x
43. Happell B, Scott D, Platania-Phung C, Nankivell J. Nurses’ views on physical activity for people with serious mental illness. Ment Health Phys Act. (2012a) 5:4–12. doi: 10.1016/j.mhpa.2012.02.005
44. Happell B, Scott D, Platania-Phung C, Nankivell J. Should we or shouldn’t we? Mental health nurses’ views on physical health care of mental health consumers. Int J Ment Health Nurs. (2012b) 21(3):202–10. doi: 10.1111/j.1447-0349.2011.00799.x
45. Happell B, Scott D, Nankivell J, Platania-Phung C. Screening physical health? Yes! but…: nurses’ views on physical health screening in mental health care. J Clin Nurs. (2013b) 22(15–16):2286–97. doi: 10.1111/j.1365-2702.2012.04325.x
46. Stubbs B, Firth J, Berry A, Schuch FB, Rosenbaum S, Gaughran F, et al. How much physical activity do people with schizophrenia engage in? A systematic review, comparative meta-analysis and meta-regression. Schizophr Res. (2016) 176(2–3):431–40. doi: 10.1016/j.schres.2016.05.017
47. Vancampfort D, Firth J, Schuch F, Rosenbaum S, De Hert M, Mugisha J, et al. Physical activity and sedentary behavior in people with bipolar disorder: a systematic review and meta-analysis. J Affect Disord. (2016) 201:145–52. doi: 10.1016/j.jad.2016.05.020
48. Stubbs B, Vancampfort D, Rosenbaum S, Ward PB, Richards J, Soundy A, et al. Dropout from exercise randomized controlled trials among people with depression: a meta-analysis and meta regression. J Affect Disord. (2016) 190:457–66. doi: 10.1016/j.jad.2015.10.019
49. Kanamori S, Takamiya T, Inoue S, Kai Y, Kawachi I, Kondo K. Exercising alone versus with others and associations with subjective health status in older Japanese: the JAGES cohort study. Sci Rep. (2016) 6:39151. doi: 10.1038/srep39151
50. Schuch FB, Dunn AL, Kanitz AC, Delevatti RS, Fleck MP. Moderators of response in exercise treatment for depression: a systematic review. J Affect Disord. (2016) 195:40–9. doi: 10.1016/j.jad.2016.01.014
51. Price EC, Gregg JJ, Smith MD, Fiske A. Masculine traits and depressive symptoms in older and younger men and women. Am J Mens Health. (2018) 12(1):19–29. doi: 10.1177/1557988315619676
52. Fraser SJ, Chapman JJ, Brown WJ, Whiteford HA, Burton NW. Physical activity attitudes and preferences among inpatient adults with mental illness. Int J Ment Health Nurs. (2015) 24(5):413–20. doi: 10.1111/inm.12158
Keywords: barriers, exercise recommendations, knowledge, mental illnesses, mental health professional, physical activity behavior
Citation: Hirschbeck A, Kossmann D, Schwegler H, Greiner S-K, Hasan A and Roeh A (2024) Implementing exercise recommendations into clinical practice—new findings from mental health professionals' and patients' perspectives in a university psychiatric setting. Front. Sports Act. Living 6:1336356. doi: 10.3389/fspor.2024.1336356
Received: 10 November 2023; Accepted: 19 April 2024;
Published: 20 May 2024.
Edited by:
Francesco Sartor, Philips Medical Systems, NetherlandsReviewed by:
Francesco Monaco, Azienda Sanitaria Locale Salerno, ItalyMoritz Bruno Petzold, Charité University Medicine Berlin, Germany
© 2024 Hirschbeck, Kossmann, Schwegler, Greiner, Hasan and Roeh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna Hirschbeck, YW5uYS5oaXJzY2hiZWNrQG1lZC51bmktYXVnc2J1cmcuZGU=
 Anna Hirschbeck
Anna Hirschbeck David Kossmann
David Kossmann Sophie-Kathrin Greiner
Sophie-Kathrin Greiner Alkomiet Hasan
Alkomiet Hasan Astrid Roeh
Astrid Roeh