
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Sports Act. Living, 18 December 2023
Sec. Elite Sports and Performance Enhancement
Volume 5 - 2023 | https://doi.org/10.3389/fspor.2023.1250223
This article is part of the Research TopicThe Youth Elite Football PlayersView all 11 articles
Objectives: This study prospectively investigated injury prevalence, incidence, and burden in male elite under-17 football players (N = 223) during a full season.
Methods: The players weekly completed a standardized web-based injury survey (OSTRC-H2) and a physical exposure report throughout the study.
Results: Average weekly response rate was 89.5%. Football exposure accounted for 52.4% of total physical exposure. On average (±SD), the players participated in individual football, strength, and rehabilitation practices for 1.2 ± 1.5, 3.0 ± .2.1, and 1.9 ± 3.4 h/week, respectively. In total, 742 health problems were reported. Mean weekly prevalence of health problems, injuries and illnesses were 20.1%, 16.5% and 3.8%, respectively. The injury incidence per 1,000 h of football exposure, match play and team practice were 8.28 (95% CI: 7.54–9.08), 16.77 (95% CI: 13.65–20.4), and 7.24 (95% CI: 6.5–8.04), respectively. Sudden-onset and gradual-onset injuries accounted for 36.7% and 43.4% of the total proportion of health problems. Hip/groin injuries had the highest incidence (1.58/1,000 h), whereas knee injuries had the highest burden (20.86 days lost/1,000 h). On average, the players experienced 3.33 health problems (average duration: 7.8 days). On average pr. player, 2.7 (95% CI: 2.2–3.3) wks of football exposure were lost.
Conclusion: Sudden and gradual-onset injuries influenced player availability during the season. Health problem prevalence fluctuated markedly, and injury incidence was higher during match play than training. The players had substantial volumes of training beyond football-specific training and matches. Our findings could assist medical and sports science practitioneers in enhancing training and recovery processes to maximize player availability.
Despite the many health benefits of sports participation (1), it is also the leading cause of injury among children and adolescents (2). In a recent study involving 3,498 adults and 3,221 children, Danish senior and youth football players had together with handball the highest prevalence of injuries in the past 12 months compared to 49 other sports (3). Injuries sustained during youth may negatively impact player development, well-being, future performance, and career prospects (4, 5). Also, an increased risk of drop-out and osteoarthritis in later life has been reported (6, 7, 8). Preventing injuries and health problems in youth football is therefore of paramount importance.
An integral first step towards prevention is gaining an understanding of the extent of injuries and illnesses (9). Traditionally, sports injury surveillance research in football has focused on the identification of serious time-loss acute sudden-onset or medical attention injuries. In addition, injury severity has commonly been defined by the duration of time lost as a proxy measure using a medical staff, athletic trainers or non-medical staff for injury reporting (10, 11). Consequently, little is known about other injury types (e.g., non-traumatic injuries or those that do not result in time-loss or medical attention) as well as the consequences of injury besides time-loss.
Recent technological and methodological advances have resulted in new opportunities to measure sport-related injury using player self-reports (10, 12). OSTRC Overuse Injury Questionnaire was developed to identify the occurrence of overuse injuries and their consequences. This represents an important step in injury epidemiology as it identifies many injuries missed with traditional approaches.
The updated Oslo Sport Traumatic Research Center questionnaire on Health Problems (OSTRC-H2) serves as an injury surveillance method with a broader focus on health problems (13). This tool was recently employed to assess the efficacy of a load management intervention on injury risk in young elite football players (14), to prospectively monitor injury incidence within a single football academy (15), and to describe prevalence and burden of injuries and illnesses in Japanese men's university football players (16). Recent research indicates, that youth elite football players are at an increased risk of health problems during periods of rapid growth and maturation (17). Additional research suggest that the incidence of time-loss injuries and injury burden could be especially high in age groups below the age of 17 (18). However, to our knowledge, no studies have yet used the OSTRC-H2 method to examine the prevalence and burden of health problems in young elite football players who are under the age of 17 across multiple clubs. Conducting a large scale study could be especially important as previous studies suggest that the injury pattern in youth players, as opposed to elite adult players, may be characterized by a higher frequency of gradual-onset injuries (17).
Thus, the present study aimed to prospectively investigate the prevalence, incidence, and burden of health problems in a group of male youth elite football players competing in the Danish under-17 premier league over a full competitive season, utilizing the OSTRC-H2.
The study was conducted as a prospective one-season cohort study on male youth elite football players (age: 15–17 yrs.). The procedures in this study were parts of a comprehensive investigational protocol (The National Danish Male Youth Elite Football Study) initiated by The Danish League exploring injury pattern as well as changes to physical and psychological performance during a full competitive season in male youth football. The participating players were prior to the beginning of the study period selected for the 1st team player rooster of a Danish male under-17 premier league club by others. The players self-reported weekly health problems using the OSTRC-H2 (13) as well as training and match exposure during the 2021/22 in-season playing period including the mid-season break. Players were recruited through initial official contacts to the front office of all clubs competing in the male Danish under-17 premier league. Individual inclusion criteria were selected as follows: male youth elite football player included in the 1st team under-17 player rooster in a football club competing in the Danish under-17 premier league during the 2021/22 season. The exclusion criteria were selected as: not accepting participation in the study, and not being willing to adhere to all protocol procedures throughout the investigation period. Players provided written informed consent to participate in the study, with the informed consent form being signed by a parent/legal guardian. The study was reviewed and approved by the local ethic committee (Ethic Committee of Southern Denmark, Identifier: 20212000–89).
In accordance with the International Olympic Committee (IOC) consensus statement on method for recording and reporting epidemiological data in sports, and the football-specific extension of the IOC consensus statement (19, 20) a health problem was defined as: “Any condition that reduced a player's normal state of complete health, irrespective of its consequences on football participation or performance, or whether the player sought medical attention”. Health problems were classified into injuries and illnesses. An injury was defined as a tissue damage or other derangement of normal physical function. An illness was defined as a complaint or disorder experienced by a player, not related to injury. Injuries were further classified by mode of onset. A sudden-onset injury was defined as a single, clearly identifiable energy transfer. A gradual-onset injury was defined as multiple accumulative bouts of energy transfer without a single, clearly identifiable event being responsible for the injury (19). A time-loss related health problem was defined as a time-loss health problem leading to a player not being able to fully participate in a planned training session or match play (19). As per the football-specific extension of the IOC consensus statement, injury burden was defined as the number of days lost per 1,000 h of football exposure (20).
Football exposure was defined as the total hours of team training and matches, with team training exposure defined as the total number of hours of specific football training team practice. This included all team sessions involving the techniques and/or tactics of football. A match was defined as organized and scheduled match play against an opposing team (including official matches, friendlies and junior/reserve team matches and international matches) (19).
Player characteristics (age, height, weight and playing position) were collected at baseline prior to study start by club sports science sector staff members following standardized procedures. Player characteristics were subsequently reported to the study leaders.
For a total of 45 weeks during the 2021/2022 season (August 2021 - June 2022), players reported any health problems experienced during the preceding 7 day period by completing the OSTRC-H2 (13) using a mobile application (AthleteMonitoring.com, FITSTATS Technologies Inc., Moncton, Canada) at the end of each week (Sunday at 7 p.m.). The standards and procedures of the OSTRC-H2 has previously been described (12). In brief, the OSTRC-H2 is based on four key questions (Figure 1) related to the difficulties in training and football participation (Q1, response options: 1 = full, 2 = full with a health problem, 3 = reduced with a health problem, 4 = absent due to a health problem), the extent to which participation was modified (Q2, response options: 1 = no modification, 2 = minor extent, 3 = moderate extent, 4 = major extent), the extent a health problem affected performance (Q3, response options: 1 = no effect, 2 = minor extent, 3 = moderate extent, 4 = major extent), and the extent of experienced symptoms/complaints (Q4, response options: 1 = no symptoms/complaints, 2 = mild extent, 3 = moderate extent, 4 = severe extent). Based on the responses to these questions, health problems were classified into any health problems (responses above 1 to Q1) or substantial health problems leading to a moderate or severe reduction in training volume or a moderate or severe reduction in sports performance (responses 3 or 4, respectively, for Q2 and Q3) (12). A time-loss injury was registered in the case players selected option 4 in Q1.
After completing the OSTRC-H2, the players reported their individual total weekly physical exposure over the last week by answering the following five question; 1) “How many hours did you in total dedicate to team practice (not matches)?”, 2) “How many hours did you in total dedicate to self-practice and individual practice with the ball (not team practice)?”, 3) “How many hours did you in total dedicate to strength training including injury prevention?”, 4) “How many hours did you in total dedicate to self-practice and individual practice without the ball (not strength or injury prevention)?”, 5) “How many hours did you in total dedicate to rehabilitation from an injury or a health problem (all types of training)?”.
The players were orally and in writing instructed on all technical matters related to the reporting process. At least one staff member at each club was assigned to support the players throughout the study period. To enhance individual response rates, the research team utilized a follow-up system in which individuals who did not complete the OSTRC-H2 or the individual exposure report on time received a text push-message. Also, a dedicated club staff member contacted them personally.
The team training and match exposure was cross-checked by evaluating micro-cycle training plans provided by the coaching staff, which were sent via e-mail to the study personnel in a pre-formatted Excel spreadsheet. Individual match exposure was confirmed by examining official match reports provided the Danish league association. All exposure values were reported weekly with the precision of 0.5 h, except match exposure which was reported with a precision of 1 min. Figure 1 illustrates the question logic of the weekly survey.
The cumulative severity scores for all health problems were summed, with the proportion of the total burden of health problems made up by the number of illnesses and injuries (10). The weekly prevalence of health problems (e.g., injury and illness) was determined by dividing the number of players reporting any form of health problem by the number questionnaire respondents (12). The prevalence of substantial health problems was calculated using the same approach. The weekly prevalence of health problems and substantial health problems was reported as average percentages with 95% confidence intervals (95% CI). To assess player availability, the prevalence of each degree of participation was determined by calculation the number of players reporting each type of participation degree by the number of questionnaire respondents. The degree of participation was lead from OSTRC-H2 Q1, which divided the degree of participation into four categories: “Full participation without any health problem”, “Full participation, but with a health problem”, “Reduced participation due to a health problem”, or “Could not participate due to a health problem” (13). Injury incidence was expressed as the number of injuries per 1,000 h of both football team training and match play (football exposure) (21). Injury incidence was reported as mean values with 95% confidence intervals (95% CI). Mean injury burden was calculated as the number of injury days lost per 1,000 h (injury incidence multiplied by mean absence per injury divided by 1,000), accounting for both the frequency and severity of injuries (21). No attempts to impute missing health data were performed. Periods of vacation (e.g., winter break off-season period and periods during which the players had no planned training or matches) were considered a part of the total yearly macro-cycle and included for analysis (22). Duplicate OSTRC-H2 reports were excluded. All statistical analyses were conducted in Stata V.17.0 software (StataCorp, College station, TX, US).
Twelve out of fourteen eligible clubs agreed to participate in the study. In total, 292 players were individually invited to participate in the study, with 223 players included for final analysis (Figure 2). In total, 18 players were excluded due to an insufficient response rate, with the average response rate for the excluded players being 5.55 ± 0.0% (mean ± SD). During the study period, 8 players were additionally transferred to clubs outside the scope of present investigation, and 11 players were transferred to older age-group teams. These players were excluded from the final analysis. Furthermore, 32 players left the study within study period with reason (N = 15) or no reason (N = 17) provided. Baseline player characteristics are reported in Table 1. The mean weekly response rate during the study was 89.5% (95% CI 87.1 to 92.0).
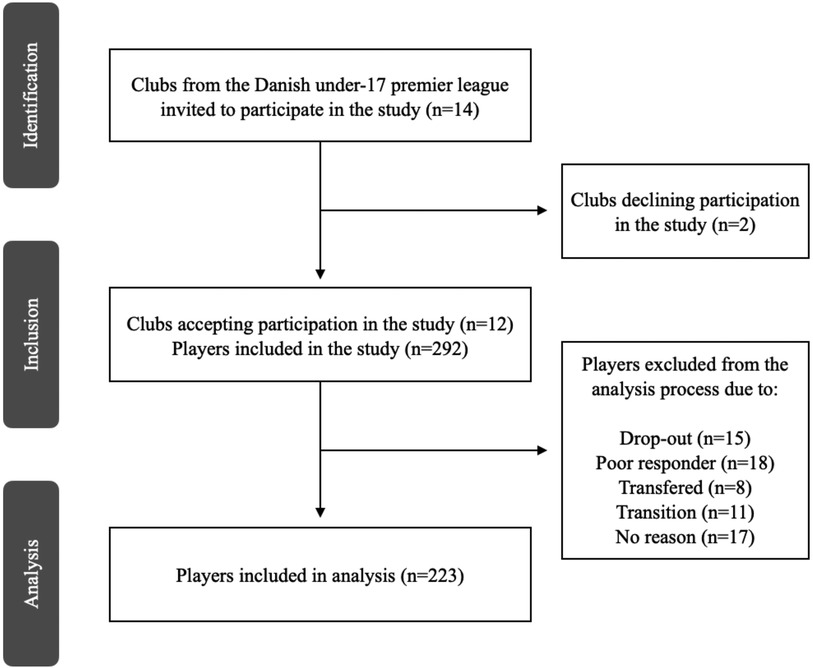
Figure 2. Recruitment and inclusion/exclusion flow chart of clubs and players from the Danish under-17 premier league included in the study.
Total football exposure and training distribution are presented in Table 2. Football exposure accounted for more than half of the total yearly exposure time. Training activities conducted to increase strength qualities and reduce injury risk accounted for around 25% of total yearly exposure. Individual training with and without the ball and time dedicated to rehabilitations purposes accounted for approximately 25% of total yearly exposure.
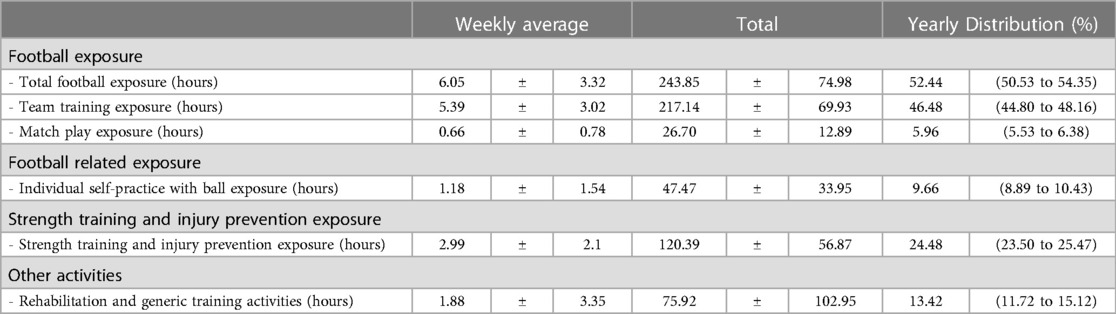
Table 2. Weekly average and total exposure values per player during the 45-week study period (N = 223). Data are presented as mean ± SD. Yearly distribution is presented as percentage with 95% confidence intervals.
During the 45-week study period, a total of 742 health problems were reported. Based on severity score, injuries accounted for 80.2% of the total proportion of health problems (60.7% of all health problems). Sudden-onset and gradual-onset injuries accounting for 36.7% and 43.4% of the total proportion of health problems, respectively (28.0% and 32.7% of all cases, respectively). Lower extremity injuries accounted for 67.4% of the total proportion of injuries (equivalent to 51.6% of the total number of injuries). Illnesses accounted for 19.8% of the total proportion of health problems (39.2% of all reported health problems). Respiratory illness had the highest no. of illnesses (N = 126) (weekly average: 2.7 ± 2.6 cases), followed by COVID-19 (N = 82: weekly average: 1.8 ± 4.5 cases) (Table 3). On average, a player had 3.33 health problems throughout the study period, with an average duration of 7.8 days per health problem.
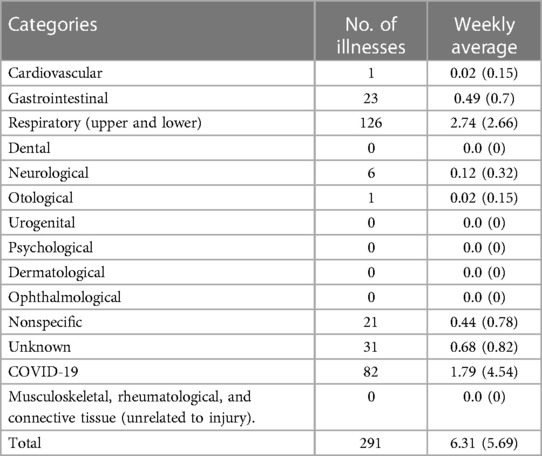
Table 3. Illnesses in danish male elite youth football players (N = 223) during the 45-week study period.
The mean weekly prevalence of health problems, injuries and illnesses were 20.1%, 16.5% and 3.8%, respectively. Sudden-onset and gradual-onset injuries accounted for 34.8% and 47.8% of the total injury prevalence. Mean weekly prevalence of all health problems, as well as health problems of substantial and time-loss character, is reported in Table 4. During the study period, fluctuations in health problem, injury and illness prevalence were observed (Figure 3).
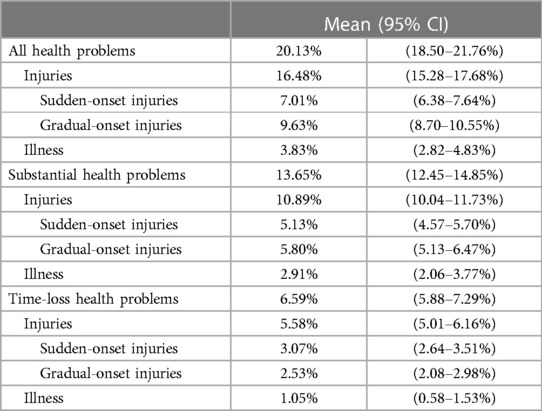
Table 4. Weekly health problem prevalence in danish male elite youth football players (N = 223). Values are presented as mean percentages with 95% confidence intervals (CI). .
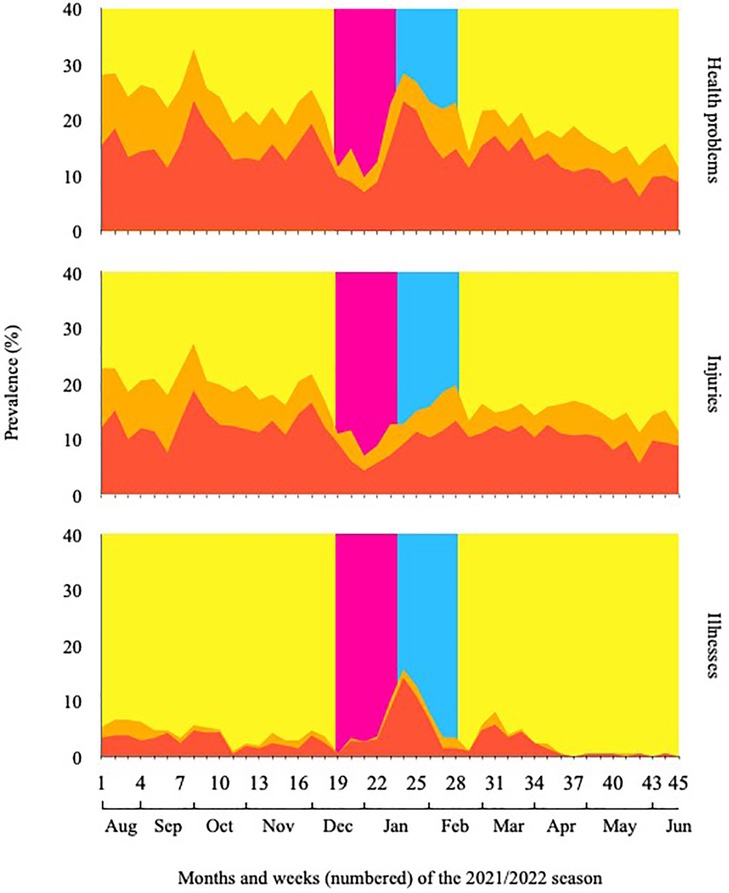
Figure 3. Weekly health problem (top), injury (mid), and illness (bottom) prevalence during the 45-week study period. Graph orange area: any complaint. Graph red area: substantial problem. Background color indication: Blue area = pre-season, Yellow area = in-season, Green area = mid-season winter break.
The injury incidence rate was 8.28 (95% CI: 7.54 to 9.08) per 1,000 h of football exposure, with injury incidence rate for team training and match play being 7.24 (95% CI: 6.50 to 8.04) and 16.77 (95% CI: 13.65 to 20.4) per 1,000 h of football exposure, respectively, resulting in a match play to team training incidence rate ratio of 2.3. All injuries sustained during matches (N = 100) were categorized as having a sudden-onset, whereas the injury incidence in training for sudden-onset and gradual-onset was 2.23 (95% CI: 1.83 to 2.69) and 5.01 (95% CI: 4.4 to 5.68) per 1,000 h of exposure, respectively. Hip/groin injuries had the highest incidence rate of 1.58 (95% CI: 1.26 to 1.95) per 1,000 h of football exposure, while knee injuries had the highest injury burden with 20.86 days lost per 1,000 h of football exposure. Elbow and head injuries resulted in the highest mean time-loss days of all body regions, with a mean of 35.0 ± 0.0 (N = 1, hence no SD) and 22.1 ± 53.95 days lost per injury, respectively. Injury incidence and burden are presented in Table 5. Risk matrixes displaying the overall incidence and severity of injuries for each body region is presented in Figures 4 and 5.
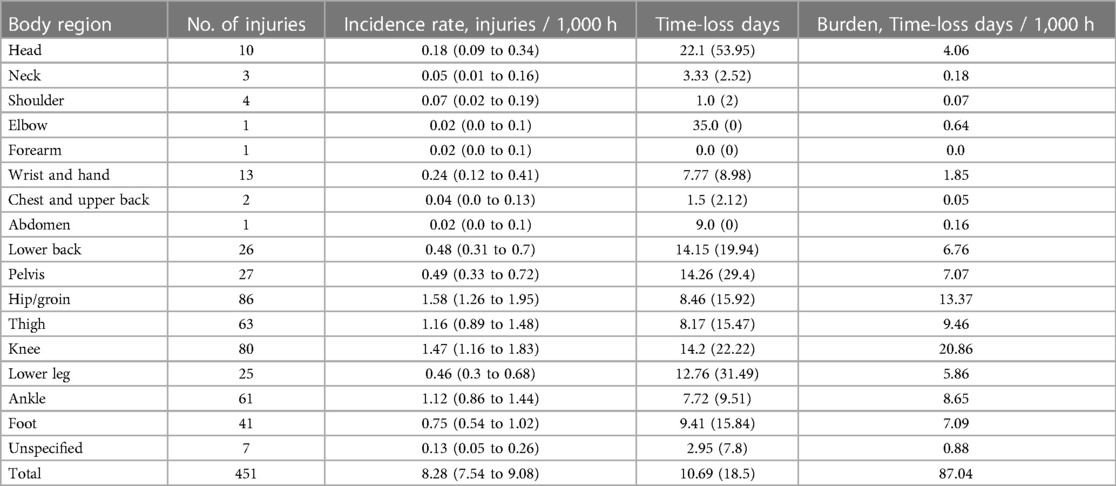
Table 5:. Injury number, Incidence rate, time-loss, and burden per body region. Total and mean values related to injury incidence rates are presented with 95% confidence intervals (CI). Values related to the specific body regions and total values are presented as absolute values. Total and mean values related to time-loss days are presented with mean (SD).
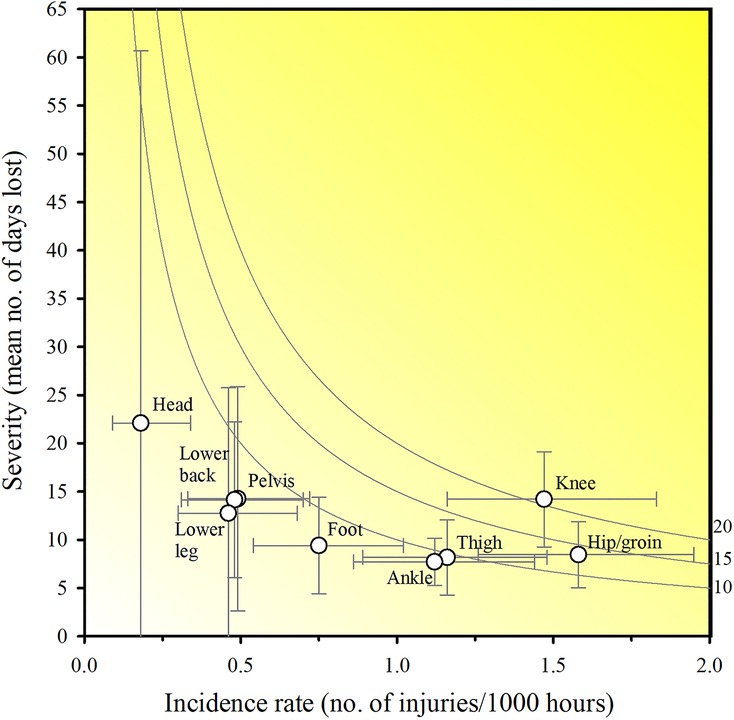
Figure 4. Risk matrix based on Oslo Sports Trauma Research Center questionnaire on health problems. Mean time-loss days illustrating the burden of injuries. Error bars represent 95% CIs. Incidence calculations are based on the total football exposure. A darker shade represents a greater burden with isobars indicating equal burden lines.
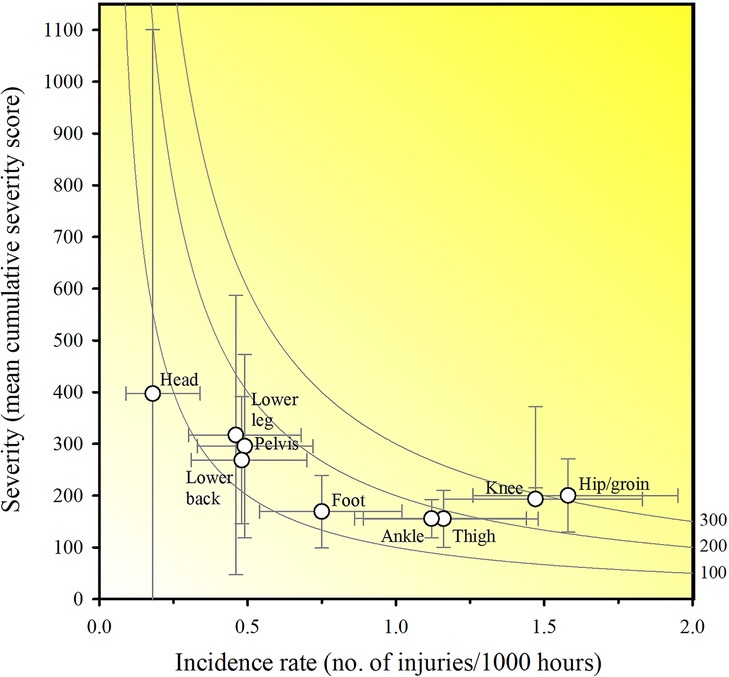
Figure 5. Risk matrix based on Oslo Sports Trauma Research Center questionnaire on health problems. Mean cumulative severity scores illustrating the burden of injuries. Error bars represent 95% CIs. Incidence calculations are based on the total football exposure. A darker shade represents a greater burden with isobars indicating equal burden lines.
The mean weekly proportion of players able to fully participate in football with or without a health problem during the study period was 84.9% (95% CI: 83.5 to 86.3). The average weekly proportion of players who were able to participate fully but had a health problem was 5.04% (95% CI: 4.48 to 5.6). During the study period the mean weekly proportion of players fully unable to participate in any football activities was 6.6% (95% CI: 5.9 to 7.3). On average, the number of weeks a player was unable to participate in any football activities was 2.7 (95% CI: 2.12 to 3.24) during the study period. The player availability during the full study period is presented in Figure 6.
During a full playing season, our study prospectively investigated health problems in Danish male youth elite football players. A major finding is, that the injury pattern of young elite football players below the age of 17 years resembled that of adult level professional players (6). As such, lower extremity sudden-onset and gradual-onset injuries was shown to be the main causes of missed team practice and match play. Furthermore, knee and head injuries displayed the highest burden and had the most days lost per injury, respectively. Also, a higher injury incidence rate per 1,000 h was observed during match play compared to team practice. Another finding of the study is, that the weekly prevalence of health problems fluctuated over the time-course of the study. This indicates that injury risk in youth footballers may be different at various stages during a playing season. In addition, the current study reveals, that young football players take part of a significant number of weekly supportive activities (i.e., strength training, self-practice etc.). This finding suggests that football exposure per se, may not reflect the actual physical load of contemporary youth elite football.
The total injury incidence rate in elite youth football players is in our study 8.3 injuries per 1,000 h of football exposure. This is higher compared to estimates (6.19 injuries/1,000 h) presented in a recent meta-analysis (23), and lower than reported for similar age-group players from the Netherlands (10.1 injuries/1,000 h) and Qatar (17.0 injuries/1,000 h (18, 24). These discrepancies may be related to differences in study designs, clubs, age-groups, and to individual training and match exposure. In our study, a broader definition of health problems was applied. This is suggested to potentially reveal more health problems (e.g., minor injuries, mild illness symptoms, and mental health issues) compared to other methods (19). Furthermore, the current investigation was conducted across several clubs, each applying a unique approach to player development (25). In addition, the average weekly football exposure in the present study was comparable to that recently demonstrated in under-19 international level players (26). Lastly, the players weekly conducted several hours of non-coach lead practice (Table 2). Collectively, this may influence our results compared to other studies.
The burden of injuries during the study period is 87 time-loss days per 1,000 h of football exposure (Table 5). This is low when compared to well-trained youth players (425 and 316 injury days/1,000 h of football exposure for U16 and U17 male elite football players, respectively) (18). It is reasonable to suggest, that youth elite footballers generally have access to necessary resources such as equipment, comprehensive medical support, and expert coaches with the ability to control match and training load. Therefore, the reason for this discrepancy is not clear. However, several teams recruited for the present investigation competed at international level standards. As such, it is possible that we have included players who are more experienced, stronger, physically fit, and thus more resistant to injuries.
In this study, gradual-onset injuries account for 43.4% of the total proportion and 32.7% of all health problems, respectively. In youth football, between 10 and 40% of all injuries are reported to be the result of gradual-onset (27), with differences in definitions being a major contributor to this considerable variation. Our findings are comparable to that in adult elite players, whereas a markedly higher match injury incidence rate is consistently reported for adults (28). It is an unexpected finding in our study, that all match injuries are reported as being of sudden-onset nature. As such, difficulties in assessing the underlying cause behind an injury may influence our results (29). Alternatively, players with pre-match clinical signs of over-use may have been excluded from match participation after medical examination. Also, the types of gradual-onset injuries appear to be age-dependent, with tendinopathies and growth-related conditions being more prevalent in young players. For example, Osgood-Schlatter disease is a common major injury peaking in the under-13 and under-14 age groups, whereas Sever's disease is most frequent in the under-11 age group (30). Although previously established (18), sudden-onset injuries may thus not always differentiate under-17 youth and adult elite football players (5). Finally, a significant proportion (23,6%) of the players were either excluded or left the study, with the remaining players upholding a high response rate throughout the study period. As such, selection bias is likely to have influenced our findings.
In our study, a significant proportion of all reported health problems are related to injuries in the lower extremity. This is in alignment with previous reports on youth elite football (5, 31, 32). The physical demands of elite youth football include high-intensity runs, frequent tackling situations and exposure to collisions and contacts (33). This is believed to increase lower extremity injury risk (27). Also, we report a higher match injury and sudden-onset injury incidence per 1,000 h of exposure compared to team practice. A more pronounced accumulation of physical fatigue as well as an increased number of contacts and collision may influence injury incidence rates during matches (34). Furthermore, a decreased predictability of specific game situations when facing opposing teams may substantially increase match play injury risk (35).
Knee injuries display the highest burden in this study. Knee injuries represent 17% (7%–23%) of all injuries in male youth players (32). In addition, one-third are reported to be due to poor knee function and to occur without contact (36, 37). It has previously been shown that 10–15 min of neuromuscular training 2–3 times weekly reduces non-contact injuries by 45% in youth football players (38). However, although the provision and application of injury treatment and rehabilitation services appears to be adequate in elite football, the provision of injury prevention services is not (39). Therefore, medical and sports science staff may benefit from revising their injury prevention strategies and placing more emphasis on the most burdensome injuries.
Elbow and head injuries have the most time-loss days per injury in present study. Head injury incidence rate in football (soccer) is commonly reported to be low (40) and comparable to our current findings (10 injuries; 0.1 injuries/1,000 h). However, head injuries may substantially impair a youth player's ability to perform at the elite level. Head injuries may also be subjected to inconsistencies in the interpretation and reporting of the symptoms and are hence frequently underdiagnosed (41). As such, future prospective studies using accurate definitions, recognition, and report on this type of injury are needed to comprehensively study the incidence of concussions among youth footballers. In this study, a single elbow injury (due to a fracture) sustained during a match was reported (Table 5). Fractures represent 4% of all injuries in elite football, with 23% of traumatic football fractures occurring in the upper extremity in professional players. Match-play related fracture incidence rate has been reported to be 12-times higher than training fracture incidence rate. This may be explained by differences in playing intensities between training and matches (42). Mean time to return to football after a proximal forearm fracture has been reported to be 5.3 wks (43). As such, fractures, despite their relatively low representation, denote one of the most serious injuries incurred by football players, and account for the most time to recover post-injury. This is confirmed by our findings.
Visual inspections reveal marked fluctuations in health problem, injury, and illness prevalence (Figure 3) during the study period with concomitant variability in player availability (Figure 5). Also, health problems, injury, and illness prevalence appear to decrease during the latter part of the study period compared to the former. Several factors may explain these findings. Our study included young players from elite football academies. During their academy training, players undergo several phases of transitioning from one playing level or team to the next. These transitions usually occur after the summer break and are often characterized by changes in coaching and support staff, squad composition, training processes, and playing intensities. In fact, football players may not always acquire the necessary levels of fitness during preseason conditioning to resist the load associated with playing competitive football (4). Consequently, the above may have influenced the risk of illnesses as well as of sudden-onset and gradual-onset injury at the beginning of the study period (32). Throughout the duration of the study period, the players dedicated a substantial amount of time to strength/power training and injury prevention activities (Table 2). It is thus reasonable to speculate, that the players may have adapted to the level and intensity of football exposure and reduced their risk of injury. Alternatively, the coaching staff may have adjusted the training processes to better align with the players' capacities as the players were exposed to a significant amount of football activities on a weekly basis. Lastly, it is important to acknowledge that the decline observed may potentially be attributed to player responder fatigue.
Using time-loss as a single measure of injury severity to assess health problem burden, may underrepresent gradual-onset injuries and fail to address the most important injuries (19). Our study presents risk matrices to identify the importance of each football-related injury (Figures 4 and 6). This approach shows injuries located to the knee to be the most burdensome in our study. Knee injuries alongside ankle, thigh and hip/groin injuries have consistently been reported to have a high prevalence in football (23). In youth football, lower extremities injuries represent about four out of five injuries with thigh, ankle, knee, and hip/groin injuries accounting for 25% (range: 11%–39%), 18% (range: 9%–31%), knee 17% (range: 7%–23%), and 14% (2%–33%) of all injuries, respectively (32). However, isolated proportions for body parts and types are of limited value since they do not consider injury severity. Reporting injury burden (i.e., days lost for combinations injury types) may therefore represent an advancement in our understanding (44). For instance, in a study of male academy football players, thigh muscle injuries were the most frequent (16% of all injuries, accounting for 11% of total time-loss), whereas joint sprains to the knee had the greatest impact on player availability (3% of injuries and 18% of total time-loss) (18). This information is lost if severity is not accounted for. Therefore, using more measures of health problem severity may provide additional insight, and the information could potentially help practitioners improve the injury-prevention measures used.
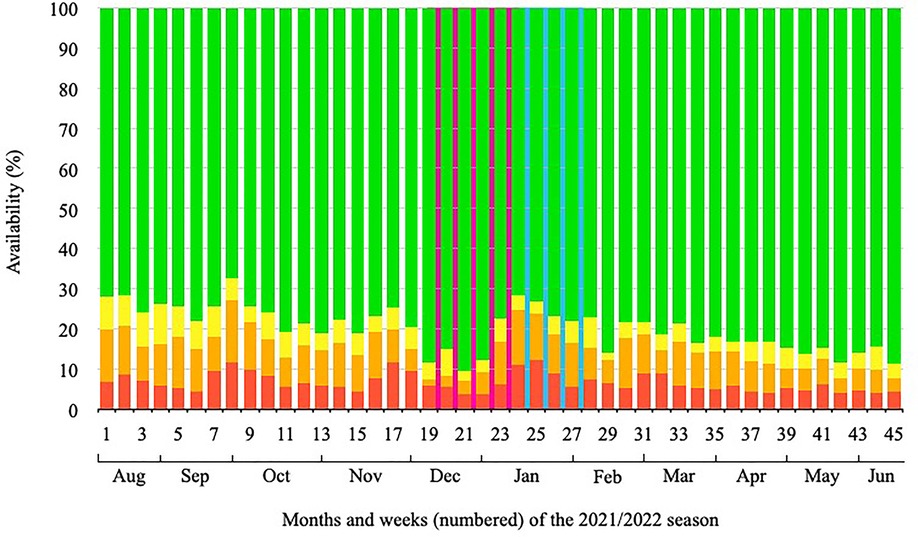
Figure 6. Weekly player availability (%) during the 45-week study period. Green area = full participation, yellow area = full participation but with a health problem, orange area = reduced participation due to a health problem, red area = no participation due to a health problem.
Weekly throughout the study period, on average 84.91% (95% CI: 83.5 to 86.32) of all players were able to fully participate in football without or with only a minor health problem. Hence, the player availability in this study is comparable to previous findings reporting an overall player availability of 82.7% in youth academy players (18). Assuming a team size of 20 players, 17 players should at any given time point during the season be available for full participation in practice or matches. In addition, two players should be expected to participate at a reduced level, whereas one player should not be able to participate due to an injury or illness. Being able to participate (i.e., having more football exposure), is suggested as a factor for development success in professional football (45). As presented in this study, a youth elite football player must expect to be unable to participate for on average 2.7 weeks per season. Extending this, although injury incidence rates and time-loss may vary greatly, approximately 4 months of health problem related time-loss must be accounted for during a six year-long academy career. Being away from football for more than 28 days due to a severe injury has been suggested to affect playing skills, long-term development, health outcomes, and future career opportunities significantly (4, 46). As such, introducing effective measure to secure a safe and timely return to football after an injury should be a main priority for football academy medical and sports science practitioneers to optimize player development.
This study took place during the later stages of the COVID-19 pandemic, with the prevalence of COVID-19 remaining at a low level throughout the study period. Also, it is worth mentioning that nearly 80% of all COVID-19 positive tests were reported immediately after the mid-season winter break. Therefore, the impact of COVID-19 on our results may be considered negligible, although the long-term relationship between COVID-19 and changes in injury risks among elite football players is only sparsely investigated (47).
Several limitations apply to our study. For instance, our study includes self-reported football exposure which may introduce measurement errors. However, collecting data through athlete management systems (questionnaire collection) may actually facilitates more accurate measures of exposure (48). In addition, this study does not report categories of tissue or injury pathology as recommended by others (19). From a practical and a research perspective, it is relevant to obtain as much information as possible about an injury, and this would have qualified our findings further. Also, the study includes participants from a selected group of male elite level football players below the age of 17 years. Injury risk in football may depend on gender, playing level and age-group. Therefore, extending our findings to other groups of players or other high-risk team sports should be done with caution. Finally, specific playing positions (e.g., goal keepers) may be subjected to different injury risk profiles (49). However, this is less well-described in youth elite football players (17) and is subject to future investigations.
In summary, during the investigation period, the main causes of missed team practice and match play in young male elite football players were lower extremity sudden-onset and gradual-onset. Injury incidence per 1,000 h was higher during match play compared to team practice, and the players took part of a significant number of weekly supportive activities. The injury pattern in youth players was comparable to that of adult players, with knee and head injuries displaying the highest burden and resulted in the most days lost per injury, respectively. As such, effective monitoring of health problems and physical exposure may guide medical and sports science practitioneers to optimize training and recovery processes, and to secure player development and long-term academy productivity.
Implementing a continuous monitoring system across age groups and teams will allow for the identification of players at particular risk during transition phases or other periods of increased risk (e.g., after holiday periods, national team camp breaks, or during congested match fixtures). Applying this approach may aid sports science staff members in adapting their training processes to align with the players' capacities at different time points throughout the season.
In this study, a web application was used to collect player data, and a high response rate was achieved. To ensure accurate and timely responses to the injury survey, it is advisable to assign dedicated staff members with the responsibility of guiding the players, as demonstrated in this study. This may increase the validity of the collected data and facilitate subsequent data processing and analysis. Similarly, it is advised to gather sufficient information on injury mechanisms regardless of the type of injury and to include injury burden as a tool for analysis. This will improve the possibility of tailoring individual injury prevention and performance-enhancing training processes. Including options for reporting self-initiated training activities may be beneficial, as not all training forms are included in load management models presently applied in elite football. This inclusion has the potential to enhance the identification of players at risk of sustaining undesirable states of overtraining and thus decrease the risk of gradual-onset injuries.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Ethic Committee of Southern Denmark. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Conceived and designed the study: TRA, MM Collected the data: TRA Analyzed the data and interpreted the findings: TRA, AD, SM, MM Wrote the paper: TRA, AD Accepted the final version of the manuscript: TRA, AD, SM, MM. All authors contributed to the article and approved the submitted version.
The authors would like to thank all participating players for their weekly efforts throughout the full study period. Also, the hard work and dedication to support the participating players provided by sports science trainees from the University of southern Denmark (SDU) and University of Aarhus (AU) as well as sport science and medical staff members across the participating clubs are highly appreciated. The authors would like to thank FITSTATS Technologies Inc., Moncton, Canada, and Francois Gazzano for providing technical support and free access to the AthleteMonitoring.com application used in the present study. The authors would sincerely like to thank Roar Amundsen for his time dedicated to produce the injury burden risk matrices presented in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act. (2010) 7:40. doi: 10.1186/1479-5868-7-40
2. Belechri M, Petridou E, Kedikoglou S, Trichopoulos D. Sports injuries among children in six European union countries. Eur J Epidemiol. (2001) 17(11):1005–12. doi: 10.1023/A:1020078522493
3. Bueno AM, Pilgaard M, Hulme A, Forsberg P, Ramskov D, Damsted C, et al. Injury prevalence across sports: a descriptive analysis on a representative sample of the Danish population. Inj Epidemiol. (2018) 5(1):6. doi: 10.1186/s40621-018-0136-0
4. Le Gall F, Carling C, Reilly T, Vandewalle H, Church J, Rochcongar P. Incidence of injuries in elite French youth soccer players: a 10-season study. Am J Sports Med. (2006) 34(6):928–38. doi: 10.1177/0363546505283271
5. Pfirrmann D, Herbst M, Ingelfinger P, Simon P, Tug S. Analysis of injury incidences in male professional adult and elite youth soccer players: a systematic review. J Athl Train. (2016) 51(5):410–24. doi: 10.4085/1062-6050-51.6.03
6. Dvorak J, Junge A, Derman W, Schwellnus M. Injuries and illnesses of football players during the 2010 FIFA world cup. Br J Sports Med. (2011) 45(8):626–30. doi: 10.1136/bjsm.2010.079905
7. Junge A, Lamprecht M, Stamm H, Hasler H, Bizzini M, Tschopp M, et al. Countrywide campaign to prevent soccer injuries in Swiss amateur players. Am J Sports Med. (2011) 39(1):57–63. doi: 10.1177/0363546510377424
8. Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. (2006) 34(4):612–20. doi: 10.1177/0363546505281813
9. van Mechelen W, Hlobil H, Kemper HC. Incidence, severity, aetiology and prevention of sports injuries. A review of concepts. Sports Med. (1992) 14(2):82–99. doi: 10.2165/00007256-199214020-00002
10. Clarsen B, Rønsen O, Myklebust G, Flørenes TW, Bahr R. The Oslo sports trauma research center questionnaire on health problems: a new approach to prospective monitoring of illness and injury in elite athletes. Br J Sports Med. (2014) 48(9):754–60. doi: 10.1136/bjsports-2012-092087
11. Ekegren CL, Gabbe BJ, Finch CF. Sports injury surveillance systems: a review of methods and data quality. Sports Med. (2016) 46(1):49–65. doi: 10.1007/s40279-015-0410-z
12. Clarsen B, Myklebust G, Bahr R. Development and validation of a new method for the registration of overuse injuries in sports injury epidemiology: the Oslo sports trauma research centre (OSTRC) overuse injury questionnaire. Br J Sports Med. (2013) 47(8):495–502. doi: 10.1136/bjsports-2012-091524
13. Clarsen B, Bahr R, Myklebust G, Andersson SH, Docking SI, Drew M, et al. Improved reporting of overuse injuries and health problems in sport: an update of the Oslo sport trauma research center questionnaires. Br J Sports Med. (2020) 54(7):390–6. doi: 10.1136/bjsports-2019-101337
14. Dalen-Lorentsen T, Bjørneboe J, Clarsen B, Vagle M, Fagerland MW, Andersen TE. Does load management using the acute:chronic workload ratio prevent health problems? A cluster randomised trial of 482 elite youth footballers of both sexes. Br J Sports Med. (2021) 55(2):108–14. doi: 10.1136/bjsports-2020-103003
15. Jaber A, Weishorn J, Berrsche G, Ott H, Bangert Y. Injury profile among elite youth male football players in a German academy. Int J Sports Med. (2022) 43(2):138–44. doi: 10.1055/a-1516-4139
16. Mashimo SYN, Hogan T, Waki H, Minakawa Y, Miyazaki S, Koido M. Prevalence and burden of injuries and illnesses in men’s university football players: a prospective cohort study in 2020 competitive season. Int J Sports Med. (2022) 11(4):9.
17. Mandorino M, Figueiredo AJ, Gjaka M, Tessitore A. Injury incidence and risk factors in youth soccer players: a systematic literature review. Part II: intrinsic and extrinsic risk factors. Biol Sport. (2023) 40(1):27–49. doi: 10.5114/biolsport.2023.109962
18. Wik EH, Lolli L, Chamari K, Materne O, Di Salvo V, Gregson W, et al. Injury patterns differ with age in male youth football: a four-season prospective study of 1111 time-loss injuries in an elite national academy. Br J Sports Med. (2021) 55(14):794–800. doi: 10.1136/bjsports-2020-103430
19. Bahr R, Clarsen B, Derman W, Dvorak J, Emery CA, Finch CF, et al. International olympic committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sports 2020 [including the STROBE extension for sports injury and illness surveillance (STROBE-SIIS)]. Orthop J Sports Med. (2020) 8(2):2325967120902908.32118084
20. Waldén M, Mountjoy M, McCall A, Serner A, Massey A, Tol JL, et al. Football-specific extension of the IOC consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020. Br J Sports Med. (2023).
21. Hägglund M, Waldén M, Magnusson H, Kristenson K, Bengtsson H, Ekstrand J. Injuries affect team performance negatively in professional football: an 11-year follow-up of the UEFA champions league injury study. Br J Sports Med. (2013) 47(12):738–42. doi: 10.1136/bjsports-2013-092215
22. Bjørndal CT, Bache-Mathiesen LK, Gjesdal S, Moseid CH, Myklebust G, Luteberget LS. An examination of training load, match activities, and health problems in Norwegian youth elite handball players over one competitive season. Front Sports Act Living. (2021) 3:635103. doi: 10.3389/fspor.2021.635103
23. Robles-Palazón FJ, López-Valenciano A, De Ste Croix M, Oliver JL, García-Gómez A, Sainz de Baranda P, et al. Epidemiology of injuries in male and female youth football players: a systematic review and meta-analysis. J Sport Health Sci. (2022) 11(6):681–95. doi: 10.1016/j.jshs.2021.10.002
24. Bult HJ, Barendrecht M, Tak IJR. Injury risk and injury burden are related to age group and peak height velocity among talented male youth soccer players. Orthop J Sports Med. (2018) 6(12):2325967118811042.30560140
25. McBurnie AJ, Dos’Santos T, Johnson D, Leng E. Training management of the elite adolescent soccer player throughout maturation. Sports (Basel). (2021) 9(12).
26. Andersen TR, Kästner B, Arvig M, Larsen CH, Madsen EE. Monitoring load, wellness and psychological variables in female and male youth national team football players during international and domestic playing periods. Front Sports Act Living. (2023) 5:1197766. doi: 10.3389/fspor.2023.1197766
27. Faude O, Rößler R, Junge A. Football injuries in children and adolescent players: are there clues for prevention? Sports Med. (2013) 43(9):819–37. doi: 10.1007/s40279-013-0061-x
28. Ekstrand J, Hägglund M, Waldén M. Injury incidence and injury patterns in professional football: the UEFA injury study. Br J Sports Med. (2011) 45(7):553–8. doi: 10.1136/bjsm.2009.060582
29. Bahr R. No injuries, but plenty of pain? On the methodology for recording overuse symptoms in sports. Br J Sports Med. (2009) 43(13):966–72. doi: 10.1136/bjsm.2009.066936
30. Le Gall F, Carling C, Reilly T. Biological maturity and injury in elite youth football. Scand J Med Sci Sports. (2007) 17(5):564–72. doi: 10.1111/j.1600-0838.2006.00594.x
31. Ruf L, Altmann S, Graf F, Romeike C, Wirths C, Wohak O, et al. Injury incidence, severity, and burden in elite youth soccer players—a 3-year prospective study. J Sci Med Sport. (2022) 25(9):737–42. doi: 10.1016/j.jsams.2022.06.003
32. Wik EH. Growth, maturation and injuries in high-level youth football (soccer): a mini review. Front Sports Act Living. (2022) 4:975900. doi: 10.3389/fspor.2022.975900
33. Varley M, Gregson W, McMillan K, Bonanno D, Stafford K, Modonutti M, et al. Physical and technical performance of elite youth soccer players during international tournaments: influence of playing position and team success and opponent quality. Sci Med Football. (2016) 1:12.
34. Bangsbo J, Mohr M, Krustrup P. Physical and metabolic demands of training and match-play in the elite football player. J Sports Sci. (2006) 24(7):665–74. doi: 10.1080/02640410500482529
35. Price RJ, Hawkins RD, Hulse MA, Hodson A. The football association medical research programme: an audit of injuries in academy youth football. Br J Sports Med. (2004) 38(4):466–71. doi: 10.1136/bjsm.2003.005165
36. Bjordal JM, Arnły F, Hannestad B, Strand T. Epidemiology of anterior cruciate ligament injuries in soccer. Am J Sports Med. (1997) 25(3):341–5. doi: 10.1177/036354659702500312
37. Chahla J, Sherman B, Cinque M, Miranda A, Garrett WE, Chiampas G, et al. Epidemiological findings of soccer injuries during the 2017 gold cup. Orthop J Sports Med. (2018) 6(8):2325967118791754. doi: 10.1177/2325967118791754
38. Steib S, Rahlf AL, Pfeifer K, Zech A. Dose-response relationship of neuromuscular training for injury prevention in youth athletes: a meta-analysis. Front Physiol. (2017) 8:920. doi: 10.3389/fphys.2017.00920
39. Fuller C, Drawer S. The application of risk management in sport. Sports Med. (2004) 34(6):349–56. doi: 10.2165/00007256-200434060-00001
40. Beaudouin F, Gioftsidou A, Larsen MN, Lemmink K, Drust B, Modena R, et al. The UEFA heading study: heading incidence in children’s and youth’ football (soccer) in eight European countries. Scand J Med Sci Sports. (2020) 30(8):1506–17. doi: 10.1111/sms.13694
41. Mooney J, Self M, ReFaey K, Elsayed G, Chagoya G, Bernstock JD, et al. Concussion in soccer: a comprehensive review of the literature. Concussion. (2020) 5(3):Cnc76. doi: 10.2217/cnc-2020-0004
42. Larsson D, Ekstrand J, Karlsson MK. Fracture epidemiology in male elite football players from 2001 to 2013: “how long will this fracture keep me out?”. Br J Sports Med. (2016) 50(12):759–63. doi: 10.1136/bjsports-2015-095838
43. Andersson JK, Bengtsson H, Waldén M, Karlsson J, Ekstrand J. Hand, wrist, and forearm injuries in male professional soccer players: a prospective cohort study of 558 team-seasons from 2001 to 2002 to 2018-2019. Orthop J Sports Med. (2021) 9(1):2325967120977091. doi: 10.1177/2325967120977091
44. Bahr R, Clarsen B, Ekstrand J. Why we should focus on the burden of injuries and illnesses, not just their incidence. Br J Sports Med. (2018) 52(16):1018–21. doi: 10.1136/bjsports-2017-098160
45. Ekstrand J, Gillquist J, Möller M, Oberg B, Liljedahl S-O. Incidence of soccer injuries and their relation to training and team success. Am J Sports Med. (1983) 11(2):63–7. doi: 10.1177/036354658301100203
46. Maffulli N, Longo UG, Gougoulias N, Loppini M, Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. (2010) 44(1):21–5. doi: 10.1136/bjsm.2009.069526
47. Waldén M, Ekstrand J, Hägglund M, McCall A, Davison M, Hallén A, et al. Influence of the COVID-19 lockdown and restart on the injury incidence and injury burden in men’s professional football leagues in 2020: the UEFA elite club injury study. Sports Med Open. (2022) 8(1):67. doi: 10.1186/s40798-022-00457-4
48. Moller M, Attermann J, Myklebust G, Wedderkopp N. Injury risk in Danish youth and senior elite handball using a new SMS text messages approach. Br J Sports Med. (2012) 46(7):531–7. doi: 10.1136/bjsports-2012-091022
Keywords: player availability, prevalence, incidence, time-loss, injury burden, OSTRC-H2, health problems, soccer
Citation: Andersen TR, Drevsfeldt A, Möller S and Møller M (2023) Injuries in male youth football: a one season prospective cohort study of 223 Danish elite players. Front. Sports Act. Living 5:1250223. doi: 10.3389/fspor.2023.1250223
Received: 29 June 2023; Accepted: 22 November 2023;
Published: 18 December 2023.
Edited by:
Harry George Banyard, Swinburne University of Technology, AustraliaReviewed by:
Yang Zhang, Independent Researcher, Orlando, United States© 2023 Andersen, Drevsfeldt, Möller and Møller. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Merete Møller bWVtb2xsZXJAaGVhbHRoLnNkdS5kaw==
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.