- 1Research Institute for Sport and Exercise Sciences, Liverpool John Moores University, Liverpool, United Kingdom
- 2Research Institute for Health Sciences, Departments of Physiology and Cardiology, Radboud University Medical Center, Nijmegen, Netherlands
- 3Liverpool Centre for Cardiovascular Science, University of Liverpool and Liverpool Heart & Chest Hospital, Liverpool, United Kingdom
- 4Cardiovascular and Metabolic Medicine, Institute of Life Course and Medical Sciences, University of Liverpool, Liverpool, United Kingdom
- 5Department of Primary Care and Mental Health, University of Liverpool, Liverpool, United Kingdom
- 6TriNetX LLC., Cambridge, MA, United States
- 7TriNetX LLC., London, United Kingdom
Background: Despite pharmacological therapies to improve outcomes of pulmonary hypertension (PH), poor long-term survival remains. Exercised-based cardiac rehabilitation (ExCR) may be an alternative strategy to improve prognosis. Therefore, using an electronic medical record (EMR) database, the objective of this study was to compare mortality between patients with primary PH with ExCR vs. propensity-matched PH patients without ExCR.
Methods: The retrospective analysis was conducted on February 15, 2023 using anonymized data within TriNetX, a global federated health research network. All patients were aged ≥18 years with primary PH recorded in EMRs with at least 1-year follow-up from ExCR. Using logistic regression models, patients with PH with an EMR of ExCR were 1:1 propensity score-matched with PH patients without ExCR for age, sex, race, and comorbidities, and cardiovascular care.
Results: In total, 109,736 patients with primary PH met the inclusion criteria for the control group and 784 patients with primary PH met the inclusion criteria for the ExCR cohort. Using the propensity score-matched cohorts, 1-year mortality from ExCR was proportionally lower with 13.6% (n = 101 of 744 patients) in the ExCR cohort compared to 23.3% (n = 174 of 747 patients) in the controls (OR 0.52, 95% CI 0.40–0.68).
Conclusion: The present study of 1,514 patients with primary PH suggests that ExCR is associated with 48% lower odds of 1-year mortality, when compared to propensity score-matched patients without ExCR.
1. Introduction
Given poor long-term survival in patients with pulmonary hypertension (PH), even with optimum drug therapy (1), alternative treatment strategies are needed. Exercise-based cardiac rehabilitation (ExCR) may provide an answer. A recent European Respiratory Society statement highlighted the potential of ExCR for PH patients (2). Specifically, ExCR improves exercise capacity, quality of life and improves symptoms (NYHA classification), and currently holds a class IIa recommendation (2, 3). However, improvement of these outcomes have been observed only after relatively short time periods (3–4 months) and, more importantly, no study has examined the association between ExCR and mortality in PH patients. Therefore, adopting a retrospective observational study using a large electronic medical record (EMR) database, the objective of this study was to compare mortality between patients with primary PH with exCR vs. a propensity-matched control group of PH without ExCR.
2. Methods
The cohort analysis was conducted on February 15, 2023 using complete case, anonymized data within the online TriNetX platform, a global federated health research network with access to EMRs from participating academic medical centres, specialty physician practices, and community hospitals, predominantly in the United States. Eligible patients with PH were identified via Centers for Disease Control and Prevention (CDC) coding using ICD-10-CM code I27.0 “primary pulmonary hypertension”. To be eligible. For the exposure group (ExCR intervention), patients were aged ≥18 years with primary PH recorded in EMRs, prescribed ExCR within six months of PH diagnosis, and at least 12-months follow-up from ExCR. The control group included patients diagnosed with primary PH but not prescribed ExCR. EExCR in the exposure group was identified from ICD-10-CM code Z71.82 (Exercise counselling), HCPCS code S9472 (ExCR program, non-physician provider, per diem), or CPT code 1013171 (Physician or other qualified health care professional services for outpatient ExCR). ExCRPatients with secondary PH, less than 12-months follow-up, and <18 years of age were excluded. At the time of the search, 27 participating healthcare organizations had data available for patients meeting the study inclusion criteria [primary PH diagnosis, 12-month follow-up, and prescribed ExCR within 6-months of diagnosis (exposure cohort)]. Thus, following propensity score matching, the cohorts consisted of patients with primary PH, who either were referred for ExCR (exposure) or did not receive ExCR (control). 12-month mortality and rehospitalisation rates were investigated using EMR data. This study is reported as per the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Supplementary Data).
Baseline characteristics were compared using chi-squared tests or independent-sample t-tests. Using logistic regression, patients with PH with an EMR of ExCR were 1:1 propensity score-matched with PH patients without ExCR for age, sex, race, diseases of the respiratory system, disease of the circulatory system, hypertensive disease, heart failure, diabetes mellitus, chronic kidney disease, cerebrovascular disease, cardiovascular procedures (e.g., cardiography, echocardiography, cardiac catheterization, cardiac devices, electrophysiological procedures), and cardiovascular medications (e.g., beta-blockers, antiarrhythmics, diuretics, antilipemic agents, antianginals, calcium channel blockers, ACE inhibitors). These variables were chosen because they are established risk factors for mortality or were significantly different between the two cohorts. Propensity score matching was undertaken using logistic regression with “greedy nearest-neighbour matching” and a calliper of 0.1 pooled standard deviations. Logistic regression models produced odds ratios (OR) with 95% confidence intervals (CI) for mortality and hospitalisation at 1-year following PH diagnosis, comparing ExCR with propensity score-matched controls. Analyses were conducted using the TriNetX online platform and regression packages in R (4). Statistical significance was set at p < 0.05.
3. Results
In total, 109,736 and 784 patients with primary PH met the inclusion criteria for the control group and the exercise-based ExCR cohort, respectively. Compared to controls, the exercise-based ExCR cohort were older, had less females, and reported more comorbidities (Table 1). Following propensity score-matching, cohorts were well balanced for age, race, sex, comorbidities, cardiovascular medications and cardiovascular procedures (p > 0.05; Table 1).
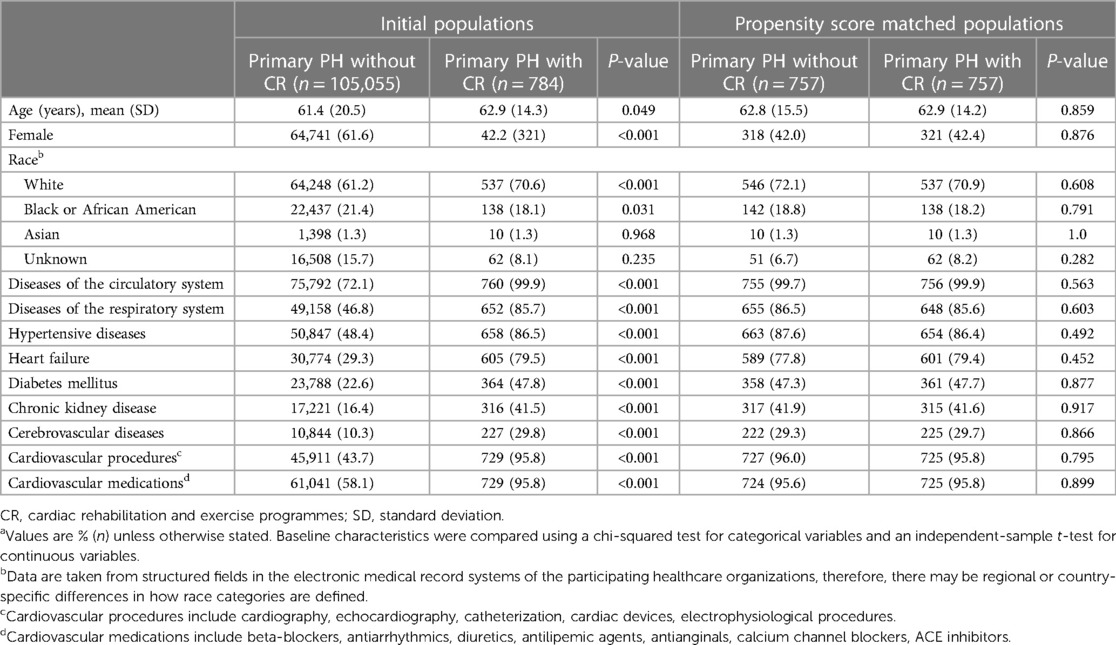
Table 1. Baseline characteristics % (n)a of the primary PH populations with and without CR before and after propensity score matching.
Using the propensity score-matched cohort, mortality at 1-year from ExCR was proportionally lower 14% (n = 101 of 744 patients) in the exercise-based ExCR cohort compared to 23% (n = 174 of 747 patients) in the controls (OR 0.52, 95% CI 0.40–0.68). There was no significant association with re-hospitalisation: 55% (n = 350 out of 632 patients) in the exercise-based ExCR cohort, compared to 57% (n = 361 out of 632 patients) in the controls (OR 0.93, 95% CI 0.75–1.16).
4. Discussion
We provide the first evidence that ExCR in patients with PH is associated with significantly lower 1-year mortality compared to patients who did not receive ExCR. Specifically, PH patients who were prescribed ExCR demonstrated 48% lower odds of 1-year mortality. Previous RCTs have shown improvement in exercise capacity, symptomatology, and quality of life after a relatively short-term follow-up (3–15 weeks) (5–10). However, whether these surrogate endpoints are associated with outcomes in PH has never been demonstrated (11). Our data suggests exercise-based ExCR may ultimately translate to clinically meaningful improvements in mortality. The poor long-term survival in PH, which also is demonstrated in the high 1-year mortality rate in this cohort of 23%, stresses the urgency of additional (non)-pharmacolxogical treatment to improve survival. These novel observations highlight the need for prospective research studies to confirm the utility of ExCR for patients with PH.
Some limitations warrant consideration. First, characterization of disease states and therapy were based on ICD-codes, which may vary between healthcare organisations. As such, distinction was made between primary PH (i.e., caused by disease of the pulmonary arteries) and secondary PH (i.e., secondary to other, non-vascular causes) rather than the current WHO-classification for PH into group 1–5 (3). Given the complexity of PH phenotypes, some PH patients labelled as “secondary PH” may also have a variant of primary PH. A second limitation is that we were unable to evaluate characteristics or adherence to ExCR, which limits the ability to identify “active ingredients”. Third, although we matched patients for important co-morbidities and demographic factors, residual confounding and the relatively modest sample size should be considered. Finally, we were unable to evaluate the potential effect of ExCR on morbidity, primarily due to small sample sizes of subgroups. The relatively small sample size may also explain why ExCR was not associated with lower rehospitalisation, despite the lower absolute prevalence of rehospitalisation PH patients undergoing ExCR.
5. Conclusion
The present study of 1,514 patients with primary PH suggests that ExCR was associated with 48% lower odds of 1-year mortality, when compared to propensity score-matched patients without ExCR. This novel data on clinical outcomes highlights the promising potential of ex CR and urgency of appropriately powered RCTs to investigate the causal effects of ex CR for patients with PH.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Datasets are only available for persons aligned to TriNetX. Specific data may be requested with the corresponding author. Requests to access these datasets should be directed to Benjamin Buckley,Yi5qLmJ1Y2tsZXlAbGptdS5hYy51aw==.
Author contributions
BB, GK and DT contributed to conception and design of the study. GK wrote the initial draft of the manuscript. BB performed the statistical analyses. BB, GK, AD, GL and DT interpreted the data. All authors contributed to the article and approved the submitted version.
Funding
TriNetX LLC. funded the acquisition of the data used through use of the database.
Conflict of interest
BB has received funding from Bristol–Myers Squibb (BMS)/Pfizer. SH has received funding from BMS. EF-E and PU are employees of TriNetX LLC. AD has received speakers fees from Janssen. GL: consultant for Bayer/Janssen, BMS/Pfizer, Medtronic, Boehringer Ingelheim, Novartis, Verseon and Daiichi-Sankyo and speaker for Bayer, BMS/Pfizer, Medtronic, Boehringer Ingelheim, and Daiichi-Sankyo. No fees are directly received personally.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fspor.2023.1247615/full#supplementary-material
References
1. Farber HW, Miller DP, Poms AD, Badesch DB, Frost AE, Muros-Le Rouzic E, et al. Five-year outcomes of patients enrolled in the REVEAL registry. Chest. (2015) 148(4):1043–54. doi: 10.1378/chest.15-0300
2. Grunig E, Eichstaedt C, Barbera JA, Benjamin N, Blanco I, Bossonne E, et al. ERS statement on exercise training and rehabilitation in patients with severe chronic pulmonary hypertension. Eur Respir J. (2019) 53(2):1800332. doi: 10.1183/13993003.00332-2018
3. Galie N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the joint task force for the diagnosis and treatment of pulmonary hypertension of the European society of cardiology (ESC) and the European respiratory society (ERS): endorsed by: association for European paediatric and congenital cardiology (AEPC), international society for heart and lung transplantation (ISHLT). Eur Heart J. (2016) 37(1):67–119. doi: 10.1093/eurheartj/ehv317
4. R: A language and environment for statistical computing [program]. Vienna, Austria: R Foundation for Statistical Computing (2023).
5. Mereles D, Ehlken N, Kreuscher S, Ghofrani S, Hoeper MM, Halank M, et al. Exercise and respiratory training improve exercise capacity and quality of life in patients with severe chronic pulmonary hypertension. Circulation. (2006) 114(14):1482–9. doi: 10.1161/CIRCULATIONAHA.106.618397
6. Weinstein AA, Chin LM, Keyser RE, Kennedy M, Nathan SD, Woolstenhulme JG, et al. Effect of aerobic exercise training on fatigue and physical activity in patients with pulmonary arterial hypertension. Respir Med. (2013) 107(5):778–84. doi: 10.1016/j.rmed.2013.02.006
7. Chan L, Chin LMK, Kennedy M, Woolstenhylme JG, Nathan SD, Weinstein AA, et al. Benefits of intensive treadmill exercise training on cardiorespiratory function and quality of life in patients with pulmonary hypertension. Chest. (2013) 143(2):333–43. doi: 10.1378/chest.12-0993
8. Ley S, Fink C, Risse F, Fisher C, Ley-Zaporozhan J, Kauczor HU, et al. Magnetic resonance imaging to assess the effect of exercise training on pulmonary perfusion and blood flow in patients with pulmonary hypertension. Eur Radiol. (2013) 23(2):324–31. doi: 10.1007/s00330-012-2606-z
9. Ehlken N, Lichtblau M, Klose H, Weidenhammer J, Fischer C, Nechwatal R, et al. Exercise training improves peak oxygen consumption and haemodynamics in patients with severe pulmonary arterial hypertension and inoperable chronic thrombo-embolic pulmonary hypertension: a prospective, randomized, controlled trial. Eur Heart J. (2016) 37(1):35–44. doi: 10.1093/eurheartj/ehv337
10. Grunig E, MacKenzie A, Peacock AJ, Eichstaedt CA, Benjamin N, Nechwatal R, et al. Standardized exercise training is feasible, safe, and effective in pulmonary arterial and chronic thromboembolic pulmonary hypertension: results from a large European multicentre randomized controlled trial. Eur Heart J. (2020) 42(23):2284–95. doi: 10.1093/eurheartj/ehaa696
Keywords: pulmonary hypertension, primary pulmonary hypertension, exercise, cardiac rehabilitation, secondary prevention
Citation: Kleinnibbelink G, Buckley BJR, Harrison SL, Williams N, Fazio-Eynullayeva E, Underhill P, van Dijk APJ, Lip GYH and Thijssen DHJ (2023) Exercised-based cardiac rehabilitation associates with lower all-cause mortality in patients with primary pulmonary hypertension. Front. Sports Act. Living 5:1247615. doi: 10.3389/fspor.2023.1247615
Received: 26 June 2023; Accepted: 28 November 2023;
Published: 11 December 2023.
Edited by:
Alejandro Santos-Lozano, Miguel de Cervantes European University, SpainReviewed by:
Saúl Peñín-Grandes, Miguel de Cervantes European University, SpainSusana López-Ortiz, Miguel de Cervantes European University, Spain
© 2023 Kleinnibbelink, Buckley, Harrison, Williams, Fazio-Eynullayeva, Underhill, van Dijk, Lip and Thijssen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benjamin J. R. Buckley Yi5qLmJ1Y2tsZXlAbGptdS5hYy51aw==
†These authors share first authorship
‡These authors share senior authorship
 Geert Kleinnibbelink
Geert Kleinnibbelink Benjamin J. R. Buckley
Benjamin J. R. Buckley Stephanie L. Harrison
Stephanie L. Harrison Nefyn Williams5
Nefyn Williams5 Gregory Y. H. Lip
Gregory Y. H. Lip Dick H. J. Thijssen
Dick H. J. Thijssen