- 1Movement Science Lab, Scottish Rite for Children, Dallas, TX, United States
- 2Therapeutic Recreation, Scottish Rite for Children, Dallas, TX, United States
- 3Research Department, Scottish Rite for Children, Dallas, TX, United States
- 4Department of Orthopedic Surgery, Nationwide Children’s Hospital, Columbus, OH, United States
Purpose: Limited research is available on the physical activity levels of children while playing on an inclusive playground, specifically designed to accommodate children with physical disabilities. The aims of this study were to objectively measure ambulatory activity and heart rate (HR) of children during unstructured play on an inclusive community playground.
Methods: Typically developing children at least 4 years of age were recruited to play freely upon entering the playground. Participants wore a StepWatch4 Activity Monitor and a Polar V800 Sport Watch. Ambulatory measures included total steps, percentage of recommended steps, total ambulatory time (TAT), bout intensity levels/duration periods. Time spent in HR zones and moderate-to-vigorous physical activity (MVPA) was determined.
Results: 95 children (48 males; Avg. age: 7 ± 2 years.) were included in this study. Children played for 31.8 ± 14.7 min., were ambulatory for 25.9 ± 12.0 min., took 1826 ± 824 steps, and accumulated 17 ± 8% of the recommended daily step count. Ambulatory bout intensity was predominantly lower intensity and bout durations varied in length. 99% of the play time was spent at a moderate HR or higher. Significant correlations were found between ambulatory and HR measures (ρ range from 0.23 to 0.99, p < 0.05), and 7–10 yo children spent a significantly higher percentage of TAT at higher intensity ambulation (p < 0.05).
Conclusions: Typically developing children can achieve moderate or higher intensity exercise and HR on an inclusive playground. Both typically developing children and those with disabilities, would benefit from a setting where they can interact and participate in parallel play with their peers.
Introduction
A recent global study on children showed that more than 80% do not meet physical activity (PA) guidelines (1). The World Health Organization (WHO) has developed a global strategy on diet, health and PA1. This plan outlines several ways to increase PA within communities and it is recommended that children and youth accumulate at least 60 min of moderate-to vigorous-intensity PA daily.
The 2018 United States PA Guidelines Advisory Committee Report demonstrates that higher amounts of PA are associated with reduced risk for an excessive weight gain in children 3–6 years of age (2). Greater emphasis should be placed on promoting PA in children, and researchers have been investigating the most effective strategies (3). There is evidence showing that access to indoor or outdoor recreation facilities is positively associated with greater PA among both children and adults (3, 4).
Playgrounds have been shown to be an effective resource promoting PA in children. Observational assessments of children on the playground have been conducted utilizing various tools (5–8). With advancements in wearable technology which can combine the measurement of ambulatory activity and heart rate (HR), there is great value in objectively measuring PA levels of children during unstructured playground-play. Studies utilizing such technology have shown that PA levels are influenced by environmental factors, differences in playground designs, sex and age (8–16). There is, however, limited research in the community playground setting (12–14).
City planners are also taking the necessary steps to construct playgrounds that are suitable for children with disabilities. These “inclusive playgrounds” allow children with disabilities to receive the health and psychosocial benefits of unstructured play along-side their typically developing peers (17). There is a negative perception that inclusive playgrounds cost significantly more and limit the typically developing child's ability to meet PA guidelines. An objective analysis of the PA of typically developing children on an inclusive playground has largely been unstudied. As more facilities are adapted and constructed for children of all physical abilities, it is important to understand, on a baseline level, the amount of physiological (elevated HR) and mechanical (ambulatory activity) loading the typically developing child experiences in these settings.
The purpose of this project was to objectively measure ambulatory activity and HR during unstructured play in typically developing children while playing on an inclusive community playground. It was hypothesized that typically developing children would spend significant portions of their time in play at a MVPA level, and the intensity/duration of ambulatory bouts would be predominantly high intensity for shorter duration periods. In addition, the relationships between age and overall play measures, such as total time spent on the playground, steps taken, and ambulatory time, to HR measures were explored.
Methods
In this institutional review board approved study, typically developing children at least 4 years of age were recruited as they entered the community playground at Scottish Rite for Children, Dallas Campus. Subject recruitment and data collection (during daylight hours) were conducted over two summers, including June-August, 2018 and May–July, 2019. Pediatric patients of the hospital, who were diagnosed with a neurologic condition, and/or were treated for an orthopedic condition in the last year, were excluded. Therefore a convenience sample of typically developing children utilizing the community playground were invited to participate. Written consent was obtained from the parent or guardian, and assent was obtained from children over the age of 10 years.
The inclusive community playground, occupies approximately 6,000 square feet (557 square meters) and is open to the community all year round during the day, excluding days where the ground surface or playground equipment is wet. The playground is structured with traditional features that have been adapted for children with physical disabilities, who may utilize walking aids such as crutches, walkers or ankle-foot orthoses or who may be non-ambulatory (wheelchair). The playground surface is a semi-firm foam material that can be easily traversed by those using a walker or wheelchair.
The playground includes equipment for children ages 2–5 and 6–10 years. Features within the large play structures comprise of balance beams, sound features (i.e., bells, megaphones), climbing walls, slides and kinetic energy features (powered as the child quickly turns the handle producing various sounds). Coupled with these large play structures, include free-standing features for climbing/bouncing, sitting/spinning and a playhouse for imaginative play. Two unique play structures include the AeroGlider™ (Playworld®, Lewisburg, PA, United States), a large see-saw structure with a rocker-style platform, and the NEOS 360™ (Playworld®, Lewisburg, PA, United States), an interactive device where various competitive games can be performed.
Height, weight, age and sex were recorded, and the participant was fitted with a StepWatch4 Activity Monitor (SAM, Modus Health, Edmonds, WA, United States), to record ambulatory activity. The SAM is a research grade ambulatory activity monitor that provides a time stamp of when strides are taken (18). The SAM has been shown to be accurate and reliable for assessing the ambulatory activity of able-bodied children (19) and has been utilized to assess the intensity and duration of daily ambulatory bouts (20, 21). The SAM was worn on the lateral ankle just superior to the lateral malleolus, and the movement calibration settings were based on the participant's height which was entered into the software. To assess HR and overall distance traveled, a Polar V800 Sport Watch (Polar, Polar Electro Inc., Bethpage, NY, United States) with GPS capability along with a Polar H10 chest strap, were worn.
The SAM and Polar monitors were verified to be configured correctly, and GPS signal was obtained on the Polar watch. The research team confirmed with the participant that the comfort and fit of the devices was satisfactory, and the participant was instructed to play freely. Once the participant was ready to leave the playground, data collection concluded, and the devices were removed.
The raw SAM stride data were exported in Microsoft Excel file format along with a time stamp of the number of strides taken every 10 s. The Polar watch data was uploaded to the Polar Flow app, and a Microsoft Excel file containing the HR data and distance traveled every second was exported. A custom written MATLAB code (Mathworks, Natick, MA, United States) down-sampled the Polar data to the maximum HR every 10 s and synchronized it with the time stamp of the SAM output.
Ambulatory measures were calculated using previously published methods (20, 21). Single strides counted by the SAM were doubled to account for the other leg, and a total number of steps (strides × 2) was determined for each 10 s interval. The total steps taken during play (Steps) were summated and divided by 11,000 steps for a general estimate of the daily recommended step count for children (% of recommended steps) (22, 23). Steps in sequential intervals were grouped into ambulatory bouts (24). Total ambulatory time (TAT) in minutes was computed by summating the duration of all ambulatory bouts.
The intensity and duration of each individual ambulatory bout was calculated (20). Intensity levels were defined using the average cadence (steps/min) of typically developing age-matched children during over-ground walking at a self-selected speed, with definitions of Easy (<60% of cadence) and Moderate+ (≥60% of cadence) (20). Duration of ambulatory bouts was calculated in minutes and summarized into the following categories: Short – less than 2 min, Intermediate—2–5 min, and Long—greater than 5 min. In addition, there were six intensity/duration combination categories for each ambulatory bout: Easy/Short, Easy/Intermediate, Easy/Long, Moderate+/Short, Moderate+/Intermediate and Moderate+/Long. The intensity/duration combination categories were reported as a percentage of the TAT.
Participant maximum HR was calculated using a child specific regression equation based on their age (208–0.7 × age) (25). Due to the lack of research in younger children, this equation (previously validated for older children) was applied. HR zones were calculated as a percentage of each child's age-based, calculated maximum HR: HR Easy (<50% of max HR), HR Moderate (50%–70% of max HR), HR Vigorous (70- 85% of max HR) and HR Peak (>85% of max HR)2. The percentage of time in each HR zone was calculated along with the total number of minutes in each zone. The total number of minutes in MVPA was summed. Additional measures included in this analysis were outside temperature in degrees Fahrenheit (°F)/Celsius(°C), total distance traveled in meters (Distance, m) and total time playing (Total Time) in minutes.
Spearman's rank correlations (ρ) were made on all measures. Participants were also divided into three groups: 4–6 yo, 7–10 yo and 11+ yo. A Mann-Whitney U test for nonparametric comparisons were run across the age groups and between sex. Statistical analysis was conducted using SPSS (version 24, IBM Inc., Chicago, IL, USA) Statistical significance was set at alpha 0.05.
Results
There were 100 typically developing children who enrolled in this study. Two children were excluded from the data analysis due to a lack of documented written assent. Three children were excluded to a HR monitor hardware malfunction. There were no incidences of reported discomfort or refusal to wear the monitors.
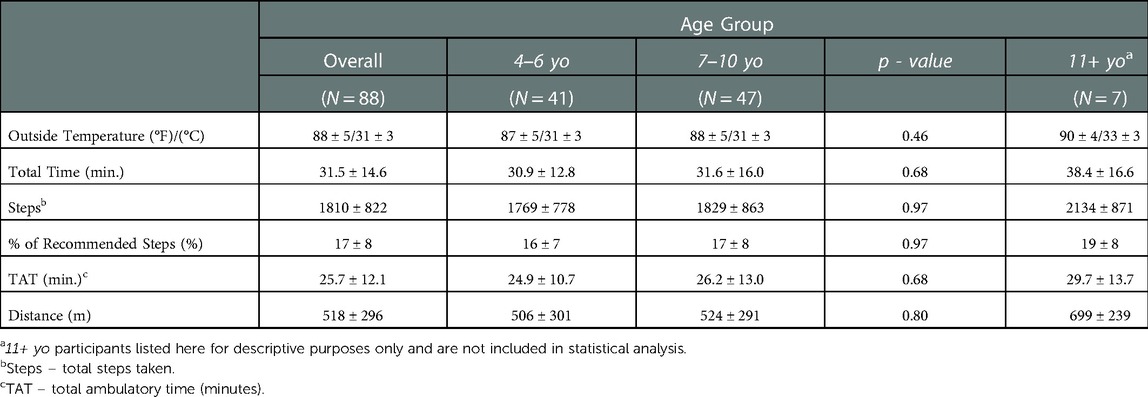
For the 95 remaining children (Table 1), the average age was 7 ± 2 years old (4–12 years old). Due to the small number of participants in the 11+ yo cohort, this group was not included in the statistical analysis (Supplementary Figure S1 and Table S1). All statistical results presented in this paper included 88 children categorized into 4–6 yo and 7–10 yo age groups.
There was no statistical difference in BMI between the age groups (p = 0.52). The majority of the children (86 of the 88 children, 98%) were observed playing with a sibling or friend during the data collection period. The average outdoor temperature on the day of testing was 88 ± 5°F (31 ± 3°C) and was not statistically significant between age groups (Table 2). The average total time spent playing was 31.5 ± 14.6 min (min.) and was not statistically different between the age groups (4–6 yo vs. 7–10 yo, Table 2). An average of 1810 ± 822 steps were taken and TAT was 25.7 ± 12.1 min across the entire cohort. Neither were statistically significant between age groups (p > 0.05, Table 2). The play period accounted for 17 ± 8% of the recommended daily step count for both groups, and there was no statistically significant difference between age groups. Distance traveled as determined by the GPS was 518 ± 296 meters and was not significantly different between age groups (Table 2).
Ambulatory bout intensity levels were summarized into Easy or Moderate+ and were reported as a percentage of TAT. The percentage of TAT at Easy intensity was significantly higher in 4–6 yo compared to 7–10 yo (Supplementary Figure S2A). 7–10 yo group spent a significantly greater percentage of TAT at Moderate+ intensity compared to the 4–6 yo group. Ambulatory bout duration periods were summarized into Short, Intermediate or Long, reported as a percentage of TAT. There were no differences between age groups in Short (p = 0.39), Intermediate (p = 0.62) or Long duration ambulatory bouts (p = 0.29) (Supplementary Figure S2B).
Significant differences between the age groups were seen in the combined intensity/ duration categories (Table 3). There were no significant differences between age groups in the percentage of ambulatory time in the Easy/Short, Easy/Intermediate or Easy/Long categories (Table 3). Moderate+/Intermediate ambulatory activity was significantly higher in the 7–10 yo group. This significant difference was also observed in Moderate+/Long ambulatory activity, as the 7–10 yo group spent more ambulatory time. There was no significant difference between groups in Moderate+/Short ambulatory activity (Table 3).
The HR data, as previously described, was categorized into the following zones based on a percentage of age-based calculated maximum HR: HR Easy, HR Moderate, HR Vigorous and HR Peak. There were no significant differences seen in the percentage time spent in any of the HR categories (p > 0.05, Table 3). Only a very small percentage of time was spent in the HR Easy category (0.8 ± 3.0%, all groups mean), with approximately 77% of the time spent at HR Moderate and HR Vigorous combined and 21.0 ± 19.2% at HR Peak. The total number of minutes of MVPA was 31.7 ± 14.7 min., and this was not significantly different between age groups (Table 3).
Across all ambulatory and HR measures, there were no significant differences between sex within each age group (4–6 yo females vs. 4–6 yo males, 7–10 yo females vs. 7–10 yo males, p > 0.05). There were statistically significant differences when comparing the same sex between each age group (4–6 yo females vs. 7–10 yo females and 4–6 yo males vs. 7–10 yo males, Supplementary Table S2). In Moderate+/Intermediate, 7–10 yo males spent a higher percentage of ambulatory time when compared to 4–6 yo males. There was a trend for Easy/Short and Easy/Intermediate being significantly higher in 4–6 yo males compared to 7–10 yo males (p = 0.06). The amount of time in HR Moderate was significantly higher in 7–10 yo males (Supplementary Table S2).
When comparing 4–6 yo females to 7–10 yo females, significant differences were observed only in the ambulatory activity measures. The amount of time spent in Easy intensity was significantly higher in 4–6 yo females. This difference became even more apparent when assessing the amount of time spent in Moderate+/Long as 4–6 yo females spent no ambulatory in this category (Supplementary Table S2).
There was a strong positive correlation between the total time that subject's spent on the playground (Total Time) with their TAT (ρ = 0.96, p < 0.01, Figure 1A), the number of steps taken (Steps, ρ = 0.90, p < 0.01, Figure 1B) and distance traveled (Distance, ρ = 0.64, p < 0.01, Figure 1C). Total minutes of MVPA was positively correlated to TAT (ρ = 0.96, p < 0.01, Figure 1D), Steps (ρ = 0.90, p < 0.01, Figure 1E) and Total Time (ρ = 0.99, p < 0.01, Figure 1F). A weak negative correlation was observed between outside temperature and Distance (ρ = −0.25, p = 0.01, Supplementary Figure S3A). Distance was positively correlated to Steps (ρ = 0.76, p < 0.01, Supplementary Figure S3B). Total minutes of MVPA was also positively correlated to Distance (ρ = 0.62, p < 0.01, Supplementary Figure S3C).
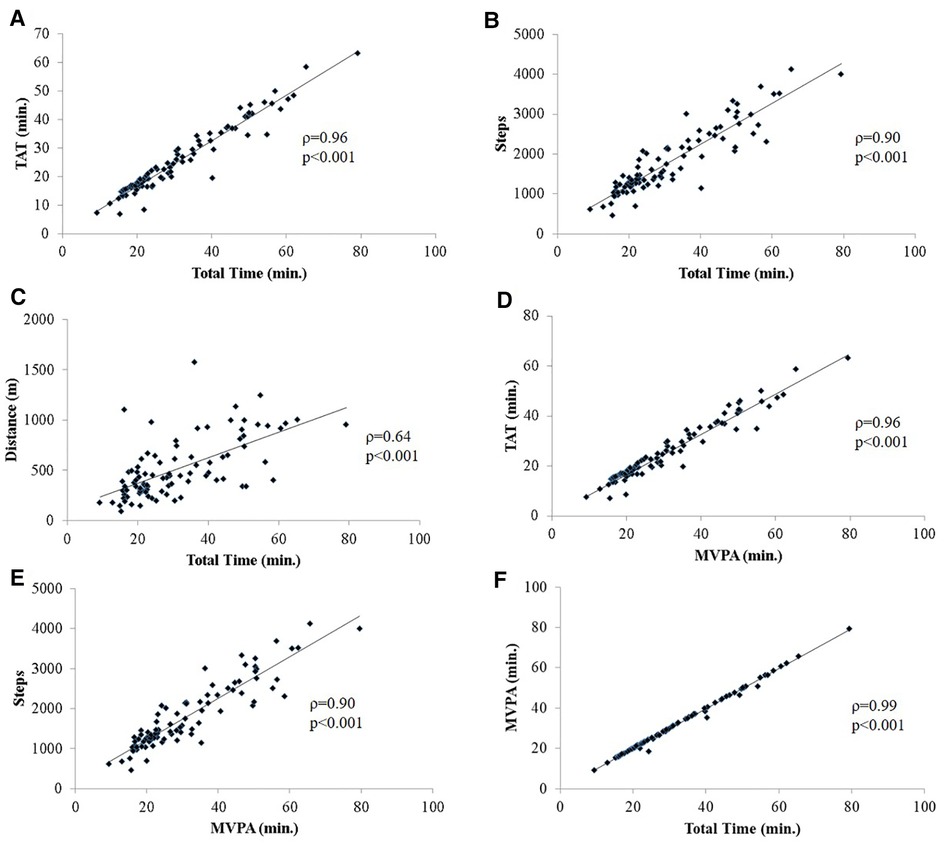
Figure 1. (A–F). Spearman rank correlations (ρ) between overall play measures; (A) total time spent on the playground (Total Time, minutes) and total ambulatory time (TAT, minutes), (B) total steps taken (Steps), (C) total distance traveled in meters (Distance, m); (D) minutes of moderate-to-vigorous (including peak) physical activity (MVPA, min.) and TAT, (E) Steps; (F) Total Time; all correlations were run including 4–6 yo and 7–10 yo participants only. p-value <0.05.
There was a weak negative correlation between age and the intensity/duration categories of Easy/Short (ρ = −0.23, p = 0.03) and Easy/Intermediate (ρ = −0.21, p = 0.04) (Supplementary Figures S4A,B). There was a weak positive correlation between age and the combination categories of Moderate+/Short (ρ = 0.25, p = 0.02), Moderate+/Intermediate (ρ = 0.33, p < 0.01) and Moderate+/Long (ρ = 0.38, p < 0.01) (Supplementary Figures S4C–E).
There was a positive correlation between Total Time and minutes in the following HR zones: HR Moderate (ρ = 0.44, p < 0.01), HR Vigorous (ρ = 0.79, p < 0.01), and HR Peak (ρ = 0.23, p = 0.02) (Supplementary Figures S5A–C). The total steps taken (Steps) was positively correlated to minutes at HR Moderate (ρ = 0.30, p < 0.01), HR Vigorous (ρ = 0.73, p < 0.01,), and HR Peak (ρ = 0.29, p < 0.01) (Supplementary Figures S5D–F). TAT was positively correlated to minutes at HR Moderate (ρ = 0.41, p < 0.01), HR Vigorous (ρ = 0.79, p < 0.01,), and HR Peak (ρ = 0.25, p = 0.02) (Supplementary Figures S5G–I). Distance was positively correlated to minutes at HR Vigorous (ρ = 0.47, p < 0.01), and HR Peak (ρ = 0.39, p < 0.01).
Discussion
The current study utilized wearable activity monitors to objectively measure ambulatory activity and HR of typically developing children during unstructured play in an inclusive community playground. Research on PA patterns of typically developing children on a community playground designed for varying levels of physical disabilities is largely understudied. It was feasible to utilize the SAM to measure ambulatory activity and a Polar HR monitor to assess time spent in specific HR zones. These different methodological approaches allowed for an in-depth analysis of the level of activity performed, and researcher's utilizing such wearable technologies can observe the advantages to both.
In this study, children spent 30 min on the playground with most of the time (∼80% of total time on the playground) spent in active ambulation. By using total steps taken as a global assessment of ambulatory activity, it was revealed that playground play accounted for more than 16% of the daily step count recommendation. Though daily step counts have been shown to be quite variable in children (22, 23), it is encouraging to observe that a reasonable amount of ambulatory activity occurred in a relatively short period of time. The present study evaluates ambulatory activity by “ambulatory bout”, which allows for a more discrete analysis of the quality of the activity (20, 24).
The evaluation of objectively measured intensity/duration during ambulatory activity in an inclusive community playground setting has not been previously reported. The predominant duration period of ambulatory activity was 2–5 min (Intermediate) and was not significantly different between 4 and 6 yo and 7–10 yo children. Play patterns varied in bout duration for both age groups as there was an uneven distribution in the amount of ambulatory time spent across the duration periods. Contrary to our hypothesis, ambulatory bout intensity was not predominantly at the higher intensity level Moderate+. Age group analysis showed that 7–10 yo children engaged in more Moderate+/Intermediate and Moderate+/Long ambulatory activity (Table 3), and correlations revealed positive weak relationships between increasing age and a higher percentage of time spent at Moderate+ ambulatory activity (Supplementary Figures S4C–E). This suggests an added health benefit for the older children, who may reach higher intensity activity levels while engaged in playground play.
The United States PA Guidelines Advisory Committee most recently reported that there is a paradigm shift in public health recommendations to support greater emphasis on total daily MVPA as an important lifestyle behavior regardless of the bout duration (26). The WHO PA guidelines for children and youth also state that efforts to accumulate 60 min of MVPA can be obtained by performing multiple shorter bouts spread throughout the day1. Our findings showed that children spent almost all of their time in MVPA while on the playground (∼99%, more than 30 min). Overall, there was a strong positive correlation between MVPA and Total Time, Steps and TAT (ρ > 0.90) (Figure 1). Fjørtoft et al. also showed that children 6 years of age achieved a moderate HR or higher for more than 20 min while playing on a typical playground (10). In a large study assessing the impact of a playground redesign, children (average age: 8 years) spent between 24%–37% of their recess time in MVPA. Similar to our study, the amount of MPVA increased with playtime duration (16). Unique to the Ridgers et al. study was the fact that playgrounds were redesigned into zones which also included a quiet play zone, which may explain the lower percentage of time in MVPA and highlight the fact that play structures can have an influence on PA levels (16). Adams et al. showed that children spent between 10 and 14 min in MVPA across various community playgrounds designs, however, activity levels were categorized by hip-worn accelerometers (12).
Researchers have reported age and sex differences in PA on the playground with boys reported to have engaged in more MVPA (27, 28). In the present study, there were no statistically significant sex related differences (p > 0.05) observed within the age groups (e.g., 4–6 yo males vs. 4–6 yo females), however, there were differences between the age groups when separated by sex (e.g., 4–6 yo males vs. 7–10 yo males). Older 7–10 yo males demonstrated twice the time in the HR Moderate zone when compared to younger male children (Supplementary Table S2). In females, 4–6 yo females did not spend any time in Moderate+/Long ambulatory activity when compared to almost 10% TAT in older female children (Supplementary Table S2). Though not specifically assessed only during playground play, Tulchin-Francis et al. showed that children 10 years and older spent more ambulatory time throughout the day in Moderate+/Intermediate and Moderate+/Long compared to younger children (ages seven to 9 years) (20). These findings, in conjunction with the current study, suggest older children are able to sustain continuous play longer than younger children, which may be related to multiple factors (attention span, social skills, peer interaction). Future research is needed to investigate the complexity of playground play (playground features, social interaction, etc.).
The shift from strictly observational studies of playground play towards studies that also obtain objective measures using a wearable device (accelerometers, HR monitors, etc.), has been emerging in recent years (29). McCrorie et al. highlights the need for more longitudinal studies on objectively measured PA of children (30). While an ambulatory activity monitor measures step accumulation there is additional useful information provided by the HR data which should be taken into account, as playgrounds are designed with features that engage the upper body would not be detected via an ambulatory monitor. The inclusive community playground used during data collection in the present study was specifically designed with structures to engage children with varying levels of physical ability. These features included, for example, ramps and a playground surface which allows easier mobility for individuals using a wheelchair/walker. By adopting an inclusive playground design, school and city planners would be addressing the needs of the whole community (17, 31, 32, 33) (United Nations Human Rights—Convention on the Rights of the Child3). This study demonstrates that typically developing children can achieve moderate or higher intensity exercise and HR, on an inclusive playground, which improves the likelihood that they will meet WHO guidelines for PA. Both typically developing children and those with disabilities, would benefit from a setting where they can easily interact and participate in parallel play with their peers.
In the present study, there are several limitations. The playground utilized in this study was designed for children ages 2–10 years, therefore, older children did not appear to frequent this playground as often. This was reflected in the participant demographics, with only 7 children at or above 11 years of age (Table 1). While a small sample size prevented statistical comparisons to other age groups, the results of the adolescent age group have been included in the data tables and in the supplementary Tables. The WHO has recently shown a global increase in the number of adolescent children failing to meet PA guidelines and there is a need for more research into the interest of these children in regards to playground usage.
Playground features have been shown to have a significant effect on a child's PA levels (7, 9, 12, 16, 34, 35). This study was conducted on a single inclusive community playground with specific design features to engage and include children with mobility restrictions. The current findings are limited to one inclusive playground.
Another limitation of the study was that all participants were required to wear a chest strap, sport watch and an ankle device while they played. Although no child complained or refused to participate after donning the devices, it is unclear if these multiple devices affected the participants’ typical play activity. Finally, numerous studies have shown that weather can also affect PA levels (36). To minimize this effect, all data in the current study were collected during the summer months; however, this does limit the interpretation of these results to other seasons or other regions of the country.
Further work is needed to objectively analyze the ambulatory intensity/duration and the time spent in various HR zones of children with physical disabilities, in this same setting. In addition, further analysis can be conducted investigating the inclusive playground features usage and their relation to elevated physical activity levels. Data presented in the current study serves as a baseline analysis that can be used for comparison purposes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by University of Texas Southwestern Institutional Review Board. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
WS conceptualized and designed the study, oversaw data collection, performed data analysis, drafted the initial manuscript, and reviewed and revised the manuscript; JB conceptualized and designed the study, developed data collection tools, performed data analysis, reviewed and revised the manuscript; PS performed data collection, performed data analysis, reviewed and revised the manuscript; DD, KJ conceptualized and designed the study, performed data analysis, reviewed and revised the manuscript. CJ performed data analysis, reviewed and revised the manuscript; KTF conceptualized and designed the study, performed data analysis, reviewed and revised the manuscript, served as the supervisory PI. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by the Scottish Rite for Children Research Program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fspor.2022.1100574/full#supplementary-material.
Footnotes
1World Health Organization Physical activity fact sheet: World Health Organization; https://www.who.int/dietphysicalactivity/factsheet_young_people/en/.
2Centers for Disease Control and Prevention Target Heart Rate and Estimated Maximum Heart Rate: Centers for Disease Control and Prevention. https://www.cdc.gov/physicalactivity/basics/measuring/heartrate.htm.
3United Nations Human Rights – Office of the High Commissioner: Convention on the Rights of the Child – Article 31 https://www.ohchr.org/en/instruments-mechanisms/instruments/convention-rights-child#:∼:text=Article%2031,-1.&text=States%20Parties%20shall%20respect%20and%20promote%20the%20right%20of%20the,artistic%2C%20recreational%20and%20leisure%20activity.
References
1. Guthold R, Stevens GA, Riley LM, Bull FC. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. Lancet Child Adolesc Health. (2020) 4:23–35. doi: 10.1016/S2352-4642(19)30323-2
2. Pate RR, Hillman CH, Janz KF, Katzmarzyk PT, Powell K, Torres A, et al. Physical activity and health in children younger than 6 years: a systematic review. Med Sci Sports Exerc. (2019) 51(6):1282–91. doi: 10.1249/MSS.0000000000001940
3. King AC, Whitt-Glover MC, Marquez DX, Buman MP, Napolitano MA, Jakicic J, et al. Physical activity promotion: highlights from the 2018 physical activity guidelines advisory committee systematic review. Med Sci Sports Exerc. (2019) 51(6):1340–53. doi: 10.1249/MSS.0000000000001945
4. Ding D, Sallis JF, Kerr J, Lee S, Rosenberg DE. Neighborhood environment and physical activity among youth A review. Am J Prev Med. (2011) 41(4):442–55. doi: 10.1016/j.amepre.2011.06.036
5. McKenzie TL, Marshall SJ, Sallis JF, Conway TL. Leisure-time physical activity in school environments: an observational study using SOPLAY. Prev Med. (2000) 30:70–7. doi: 10.1006/pmed.1999.0591
6. Farley TA, Meriwether RA, Baker ET, Rice JC, Webber LS. Where do the children play? The influence of playground equipment on physical activity of children in free play. J Phys Activ Health. (2008) 5:319–31. doi: 10.1123/jpah.5.2.319
7. Anthmatten P, Brink L, Kingston B, Kutchman E, Lampe S, Nigg C. An assessment of schoolyard features and behavior patterns in children’s utilization and physical activity. J Phys Activ Health. (2014) 11:564–73. doi: 10.1123/jpah.2012-0064
8. Barnas J, Ball S. The effects of playground zoning on physical activity during recess in elementary-aged children. Med Sci Sports Exerc. (2019) 51(6):514. doi: 10.1249/01.mss.0000562045.96833.7a
9. Cardon G, Cauwenberghe EV, Labarque V, Haerens L, Bourdeaudhuij ID. The contribution of preschool playground factors in explaining children’s physical activity during recess. Int J Behav Nutr Phys Act. (2008) [cited 2018 July 20] 5(11). doi: 10.1186/1479-5868-5-11
10. Fjørtoft I, Kristoffersen B, Sageie J. Children in schoolyards: tracking movement patterns and physical activity in schoolyards using global positioning system and heart rate monitoring. Landsc Urban Plan. (2009) 93:210–17. doi: 10.1016/j.landurbplan.2009.07.008
11. Mota J, Silva P, Santos MP, Ribeiro JC, Oliveia J, Duarte JA. Physical activity and school recess time: differences between the sexes and the relationship between children’s playground physical activity and habitual physical activity. J Sports Sci. (2005) 23(3):269–75. doi: 10.1080/02640410410001730124
12. Adams J, Veitch J, Barnett L. Physical activity and fundamental motor skill performance of 5–10 year old children in three different playgrounds. Int J Environ Res Public Health. (2018) 15:1896–908. doi: 10.3390/ijerph15091896
13. Quigg R, Gray A, Reeder AI, Holt A, Waters D. Using accelerometers and GPS units to identify the proportion of daily physical activity located in parks with playgrounds in New Zealand children. Prev Med. (2010) 50(5–6):235–40. doi: 10.1016/j.ypmed.2010.02.002
14. Quigg R, Reeder AI, Gray A, Holt A, Waters D. The effectiveness of a community playground intervention. J Urban Health. (2012) 89(1):171–84. doi: 10.1007/s11524-011-9622-1
15. Howe CA, Clevenger KA, Jackson M, Ragan BG, Sinha G. Children’s free-play physical activity intensity by school playground location. Med Sci Sports Exerc. (2015) 47(5S):916–7. doi: 10.1249/01.mss.0000479215.38591.56
16. Ridgers ND, Stratton G, Fairclough SJ, Twisk JWR. Long-term effects of a playground markings and physical structures on children’s recess physical activity levels. Prev Med. (2007) 44:393–97. doi: 10.1016/j.ypmed.2007.01.009
17. Yantzi NM, Young NL, Mckeever P. The suitability of school playgrounds for physically disabled children. Child Geographies. (2010) 8(1):65–78. doi: 10.1080/14733281003650984
18. Coleman KL, Smith DG, Boone DA, Joseph AW, del Aguila MA. Step activity monitor: long-term, continuous recording of ambulatory function. J Rehabil Res Dev. (1999) 36:8–18.10659890
19. McDonald CM, Widman L, Abresch T, Walsh SA, Walsh DD. Utility of a step activity monitor for the measurement of daily ambulatory activity in children. Arch Phys Med Rehabil. (2005a) 86:793–801. doi: 10.1016/j.apmr.2004.10.011
20. Tulchin-Francis K, Stevens W Jr, Jeans KA. Intensity and duration of activity bouts decreases in healthy children between 7 and 13 years of age: a new, higher resolution method to analyze StepWatch activity monitor data. Physiol Meas. (2014) 35:2239–54. doi: 10.1088/0967-3334/35/11/2239
21. Stevens WR Jr, Tulchin-Francis K. Interval setting selection affects ambulatory activity outputs in children with cerebral palsy. Gait Posture. (2017) 57:69–73. doi: 10.1016/j.gaitpost.2017.05.020
22. Mayorga-Vega D, Casado-Robles C, Viciana J, López-Fernández I. Daily step-based recommendations related to moderate-to-vigorous physical activity and sedentary behavior in adolescents. J Sports Sci Med. (2019) 18(4):586–95.31827342
23. Tudor-Locke C, Craig CL, Beets MW, Belton S, Cardon GM, Duncan S, et al. How many steps/day are enough? For children and adolescents. Int J Behav Nutr Phys Act. (2011) [cited 2019 October 1] 8(78). doi: 10.1186/1479-5868-8-79
24. Orendurff MS, Schoen JA, Bernatz GC, Segal AD, Klute GK. How humans walk: bout duration, steps per bout and rest duration. J Rehabil Res Dev. (2008) 45:1077–89. doi: 10.1682/JRRD.2007.11.0197
25. Mahon AD, Marjerrison AD, Lee JD, Woodruff ME, Hanna LE. Evaluating the prediction of maximal heart rate in children and adolescents. Res Q Exerc Sport. (2010) 81(4):466–71. doi: 10.1080/02701367.2010.10599707
26. Jakicic JM, Kraus WE, Powell KE, Campbell W, Janz KF, Troiano RP, et al. Association between bout duration of physical activity and health: systematic review. Med Sci Sports Exerc. (2019) 51(6):1213–9. doi: 10.1249/MSS.0000000000001933
27. Ridgers ND, Salmon J, Parrish A, Stanley RM, Okely AD. Physical activity during school recess: a systematic review. Am J Prev Med. (2012) 43(3):320–8. doi: 10.1016/j.amepre.2012.05.019
28. Klinker CD, Schipperijn J, Christian H, Kerr J, Ersbøll AK, Troelsen J. Using accelerometers and global positioning system devices to assess gender and age differences in children’s school, transport, leisure and home based physical activity. Int J Behav Nutr Phys Act. (2011) [cited 2020 March 30] 11(8). doi: 10.1186/1479-5868-11-8
29. Bates B, Stone MR. Measures of outdoor play and independent mobility in children and youth: a methodological review. J Sci Med Sport. (2015) 18(5):545–52. doi: 10.1016/j.jsams.2014.07.006
30. McCrorie PRW, Fenton C, Ellaway A. Combining GPS, GIS, and accelerometry to explore the physical activity and environment relationship in children and young people—a review. Int J Behav Nutr Phys Act. (2014) [cited 2020 March 30] 11(93). doi: 10.1186/s12966-014-0093-0
31. Moore A, Boyle B, Lynch H. Designing public playgrounds for inclusion: a scoping review of grey literature guidelines for universal design. Children’s Geographies. (2022). doi: 10.1080/14733285.2022.2073197
32. Burke J. Just for the fun of it: making playgrounds accessible to all children. World Leis J. (2013) 55(1):83–95. doi: 10.1080/04419057.2012.759144
33. Jeanes R, Magee J. Can we play on the swings and roundabouts?: creating inclusive play spaces for disabled young people and their families. Leis Stud. (2012) 31(2):193–210. doi: 10.1080/02614367.2011.589864
34. Reimers AK, Knapp G. Playground usage and physical activity levels of children based on playground spatial features. J Public Health. (2017) 25:661–9. doi: 10.1007/s10389-017-0828-x
35. Stanton-Chapman TL, Toraman S, Morrison A, Dariotis JK, Schmidt EL. An observational study of children’s behaviors across two playgrounds: similarities and differences. Early Child Res Q. (2018) 44:114–23. doi: 10.1016/j.ecresq.2018.03.007
Keywords: inclusive, playground, community, physical activity, intensity/duration, heart rate
Citation: Stevens WR, Borchard JM, Sleeper P, Dempsey D, Jeans KA, Jo C and Tulchin-Francis K (2023) Inclusive community playgrounds benefit typically developing children: An objective analysis of physical activity. Front. Sports Act. Living 4:1100574. doi: 10.3389/fspor.2022.1100574
Received: 16 November 2022; Accepted: 28 December 2022;
Published: 1 February 2023.
Edited by:
Matthew Ahmadi, The University of Sydney, AustraliaReviewed by:
Risto Marttinen, George Mason University, United StatesNic Matthews, Cardiff Metropolitan University, United Kingdom
© 2023 Stevens, Borchard, Sleeper, Dempsey, Jeans, Jo and Tulchin-Francis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wilshaw Stevens Jr d2lsc2hhdy5seW5uLnN0ZXZlbnNAZ21haWwuY29t
Specialty Section: This article was submitted to Sports Science, Technology and Engineering, a section of the journal Frontiers in Sports and Active Living
 Wilshaw R. Stevens Jr
Wilshaw R. Stevens Jr Justine M. Borchard1
Justine M. Borchard1 Dana Dempsey
Dana Dempsey Kirsten Tulchin-Francis
Kirsten Tulchin-Francis