- 1University of Rochester, Rochester, United States
- 2School of Medicine, University of Colorado Anschutz Medical Campus, Aurora, United States
At the intersection of injury-prone sports such as baseball and conditions like ADHD that affect all aspects of life, there is a lack of research. This limits the availability of preventive care programs designed to target potential risks and promote a safe experience. In this retrospective cohort study, we assess the frequency of injury in youth baseball players with and without ADHD, along with further investigation into how treatment with stimulant medication may modify risk factors. The data for this study were obtained in deidentified, aggregate format from the TriNetX research database. We identified all patients under 25 years of age with a designation of baseball activity. Within this population, we separated patients by presence or absence of ADHD diagnosis, and then by stimulant usage. The studied outcomes were injuries commonly occurring in baseball, including fractures, sprains, and specific injury patterns. We identified 17,710 patients under 25 years old with designated baseball activity, 1,183 of which had a diagnosis of ADHD. Of these, 511 had a history of stimulant medication and 470 had no history of stimulant use. For most events (i.e., injuries), there were no statistical differences between cohorts. The overall ADHD cohort significantly differed from the Not ADHD cohort in 3 events: “thorax, abdomen, pelvis injuries,” “ankle sprain,” and “concussion.” When athletes with ADHD received treatment, this trend reversed for select injuries: “any fracture”, “head or neck injuries”, “upper limb injuries”, and “lower limb injuries” were less likely in ADHD athletes on stimulants. Given the ongoing debate around stimulant use in athletics, our study is relevant to many patients, providers, and the baseball community.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common childhood neurodevelopmental disorders, affecting 6%–9% of children and adolescents in the United States (1). It is characterized by excessive hyperactivity, impulsivity, mood swings, and difficulty maintaining attention (2). ADHD often leads to difficulty at school and work, impaired relationships, low self-esteem, and risky behavior in organized activity, such as a sports (3). Organized sports, however, have also been shown to reduce symptoms in ADHD youth, often in team sports like baseball, particularly as hyperactive symptoms are known to be reduced after exercise (4).
Baseball is a longstanding facet of American culture. In 2020 alone, 3,403,000 children between the ages of 6–12 and 1,845,000 youths aged 13–17 played baseball; numbers which were even higher before the COVID-19 epidemic (5). However, the injury rate in baseball is higher than some other team sports (6). Similarly, ADHD is associated with far higher rates of injuries in all activities, not only sports (7). While hyperactive symptoms are improved by exercise, ADHD is known to impair motor function, reflexes, and situational awareness, all of which are important for avoiding injury in fast-paced sports like baseball (2, 8). Unfortunately, at the intersection of injury-prone sports such as baseball and conditions like ADHD that affect all aspects of life, there is a lack of research. This limits the availability of preventive care programs designed to target potential risks and promote a safe experience. In this retrospective cohort study, we assess the frequency of injury in youth baseball players with and without ADHD, along with further investigation into how treatment with stimulant medication is associated with particular risk factors. We hypothesize that our research will reinforce findings that individuals with ADHD will have higher rates of injury compared to players without ADHD. We also hypothesize that stimulant medications, known to effectively treat ADHD symptoms, may be associated with lower rates of injury in baseball players with ADHD compared to players without ADHD.
Methods
The data for this study were obtained in deidentified, aggregate format from the TriNetX research database. TriNetX contains electronic medical records from large healthcare organizations (HCOs) and has been well-established for medical research, including a wide range of fields such as obstetrics (9), sexuality (10), and surgery (11). TriNetX, LLC is compliant with the Health Insurance Portability and Accountability Act (HIPAA), the US federal law which protects the privacy and security of healthcare data, and any additional data privacy regulations applicable to the contributing HCO (12). TriNetX is certified to the ISO 27001:2013 standard and maintains an Information Security Management System (ISMS) to ensure the protection of the healthcare data it has access to and to meet the requirements of the HIPAA Security Rule. Any data displayed on the TriNetX Platform in aggregate form, or any patient level data provided in a data set generated by the TriNetX Platform only contains de-identified data as per the de-identification standard defined in Section §164.514(a) of the HIPAA Privacy Rule (12).
Using International Classification of Diseases (ICD) codes, we identified all patients under 25 years of age with a designation of baseball activity (Y93.64) between August 11, 2002 and August 11, 2022. Within this population, we separated patients by presence or absence of ADHD diagnosis (F90). The ADHD cohort was further separated by stimulant usage. Stimulant use was defined by the presence of either amphetamine-class medications or phenidate-class medications individually. Patients with both amphetamine- and phenidate-class medications present at the same instance in their chart were excluded from analysis, as combined stimulant use is reserved for significantly severe cases (13).
Using the TriNetX software, we performed statistical analysis between the cohort without ADHD and each of the other groups, for a total of 3 analyses (Not ADHD vs. ADHD with stimulant use; ADHD without stimulant use; and ADHD overall). Prior to comparison, the cohorts were balanced based on age, sex, and race using nearest-neighbor matching to a difference in propensity scores <0.1 (10). After matching, cohorts had no significant differences in sex, age, or race. Table 1 contains cohort demographic information for the Not ADHD and overall ADHD cohorts, both before and after balancing on these characteristics. Balancing was performed before each of the three analyses. As the reference group without ADHD was matched to each of the above groups before analysis, the N of the reference group was equal to the matched group being analyzed.
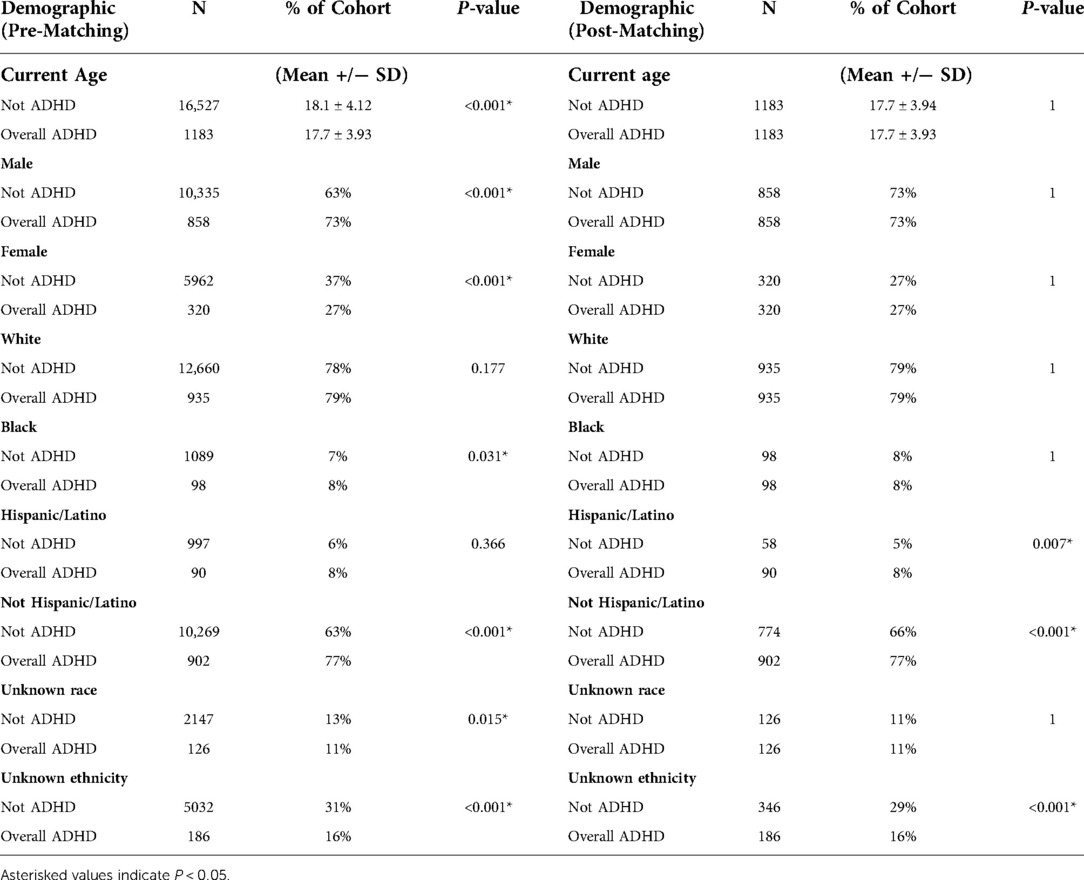
Table 1. Demographics of overall ADHD cohort and not ADHD reference cohort, before and after propensity score matching on sex, race, and age.
The studied outcomes were injuries commonly occurring in baseball: “upper limb fractures,” consisting of fractures of the shoulder, humerus, forearm, wrist, or hand (ICD-10: S42, S52, S62); “lower limb fractures,” consisting of fractures of the femur, lower leg, ankle, or foot (ICD: S72, S82, S92); “any fractures,” consisting of any prior mentioned fracture type; “head & neck injuries” consisting of injuries to the musculoskeletal system above the clavicle (ICD: S00–19); “upper limb injuries” consisting of injuries from the shoulder to fingers (ICD: S40–69); “lower limb injuries” consisting of injuries from the hip to toes (ICD: S70–99); “thorax, abdomen, pelvis injuries” consisting of injuries from the clavicle to the hip, including the innominate and genitals (ICD: S40–69); shoulder sprain (ICD: S43.4); rotator cuff and/or labrum injury (ICD: M75.1, S43.42–43, S46.0); elbow sprain (ICD: S53.4); ulnar collateral ligament (UCL) damage (IDC: S53.44 & S53.3); knee sprain (ICD: S83.4–5); ankle sprain (S93.4); and concussion (ICD: S06.0). Injuries were considered binary variables based on presence or absence of the corresponding ICD code in the health record within the time window. A t-test was used to compare event rates between cohorts. Odds ratios with a 95% confidence interval were also calculated from event rates. The results are compiled in Table 2. Significance for this study was set at P < 0.05. As this study contained only deidentified aggregate data, the Colorado Multiple Institutional Review Board (COMIRB) designated it as non-human research not in need of approval.
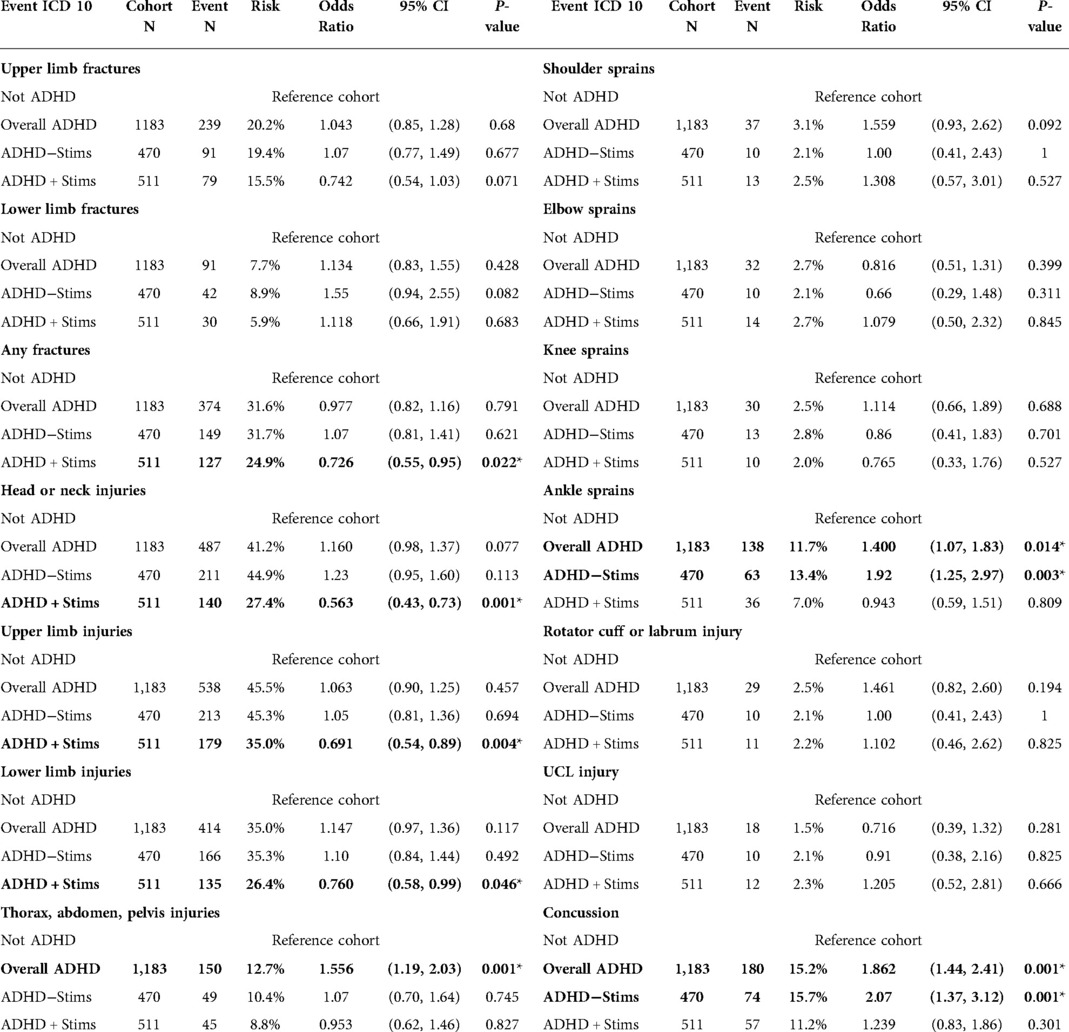
Table 2. Cohort size, absolute risk, odds ratio with confidence interval, and t-test P-value by outcome. Stimulants abbreviated as “Stims.” Asterisked values indicate P < 0.05.
Results
We identified 17,710 patients under 25 years old with designated baseball activity, 1,183 of which had a diagnosis of ADHD. Of these, 511 had a history of stimulant medication and 470 had no history of stimulant use. For most events (i.e., injuries), there were no statistical differences between cohorts. The overall ADHD cohort significantly differed from the Not ADHD cohort in 3 events: “thorax, abdomen, pelvis injuries” (OR = 1.56, P = 0.001), “ankle sprain” (OR = 1.40, P = 0.014), and “concussion” (OR = 1.86, P = 0.001). The no stimulant group differed in “ankle sprain” (OR = 1.92, P = 0.003), and “concussion” (OR = 2.07, P = 0.001). The stimulant group differed in 4 of the 14 measured outcomes but not in the 3 outcomes mentioned previously by other groups. Further results are in Table 2, along with odds ratios and confidence intervals. All relationships described were comparing the Not ADHD cohort to the relevant ADHD cohort. Therefore, an odds ratio above 1 indicates the ADHD cohort was more likely to experience the outcome of interest, and an odds ratio less than 1 indicates the ADHD cohort was less likely to experience the outcome. Figures 1, 2 present visual depictions of odds ratios between athletes without ADHD and patients with stimulant use (Figure 1) and overall ADHD (Figure 2). Figure 3 presents visual depictions of odds ratios between athletes without ADHD and patients with non-stimulant use.
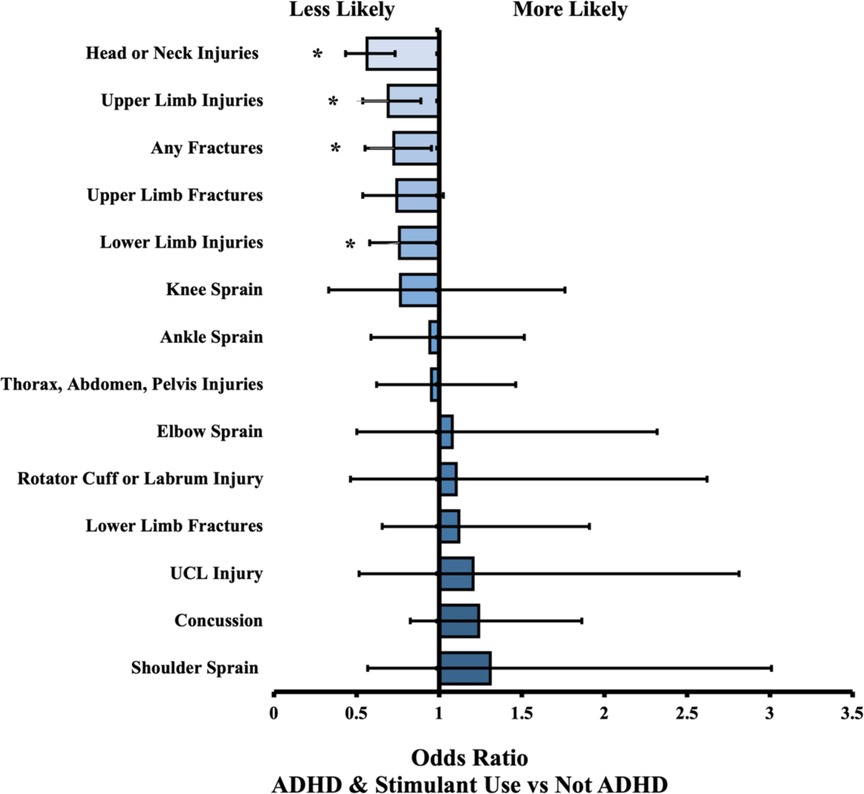
Figure 1. Odds ratio (OR) by injury type. OR < 1 indicates decreased likelihood of injury in ADHD (+) stimulant cohort compared to non-ADHD reference cohort. Confidence bars represent 95% interval. Asterisk (*) data labels indicate significant difference (P < 0.05).
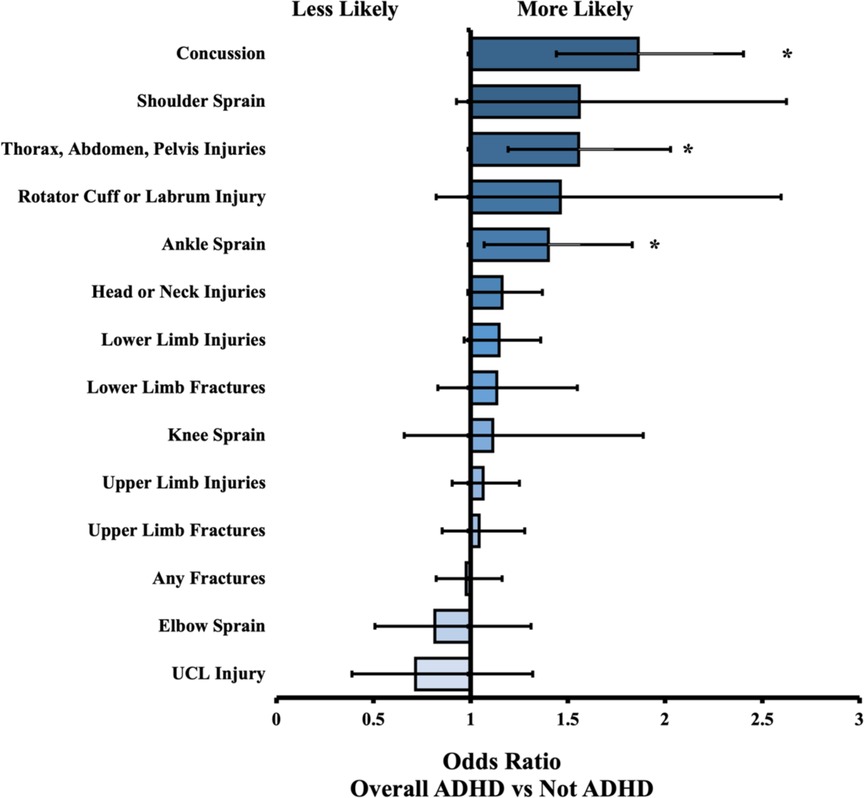
Figure 2. Odds ratio (OR) by injury type. OR < 1 indicates decreased likelihood of injury in Overall ADHD cohort compared to Not ADHD reference cohort. Confidence bars represent 95% interval. Asterisk (*) data labels indicate significant difference (P < 0.05).
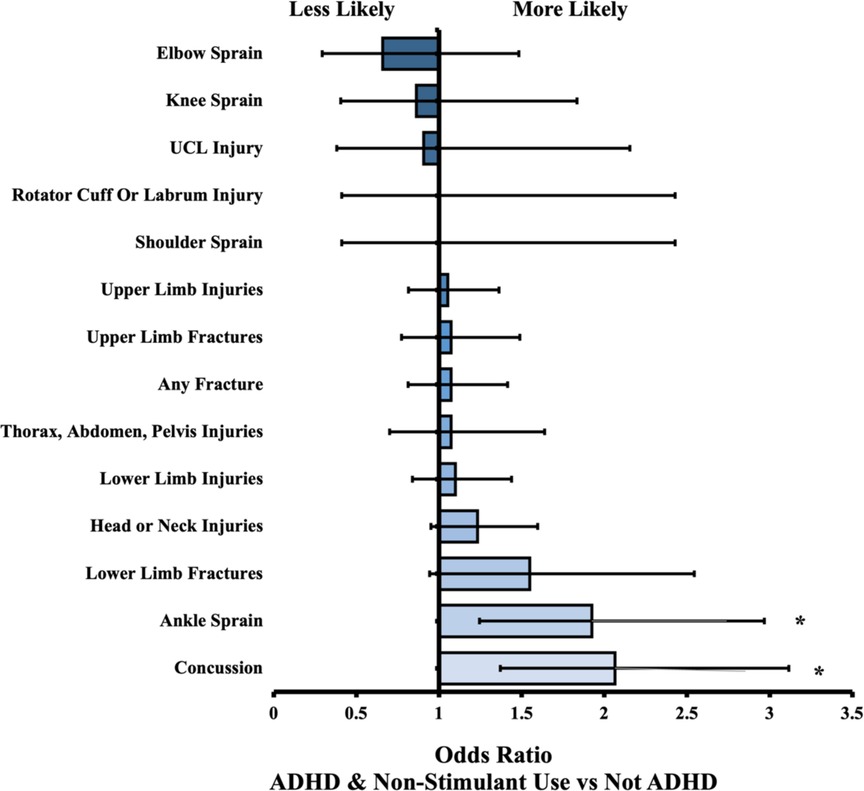
Figure 3. Odds ratio (OR) by injury type. OR < 1 indicates decreased likelihood of injury in ADHD non-stimulant cohort compared to Not ADHD reference cohort. Confidence bars represent 95% interval. Asterisk (*) data labels indicate significant difference (P < 0.05).
Discussion
Our findings present an interesting mix of injury differences across baseball athletes based on ADHD status and medication management. The comparison between patients without ADHD and the overall ADHD group revealed three injuries that are more common: “thorax, abdomen, pelvis injuries,” “ankle sprain,” and “concussion.” Within the category of “thorax, abdomen, and pelvis injuries,” the most common injury type is a fracture of the lumbosacral spine and pelvis (S32.9), which most often occurs in high-energy collisions (14), but there is also a specific type of pelvic avulsion fracture almost exclusively encountered in adolescent athletes, commonly in baseball (15). Ankle sprains are also very common in baseball, due to the combination of rapid acceleration, rotational force, and sliding maneuvers employed (8). The increased rate of sprains in patients with overall ADHD and ADHD without stimulant use could be caused by a variety of ADHD factors. For example, an athlete with decreased situational awareness may decide to slide without appropriate recognition of another player's positioning, leading to collision (16).
Concussion is an important event that is increased in both overall ADHD and ADHD without stimulant use. Research into associations between concussion and athletes with ADHD has been performed at all levels of baseball, including high school, college, and professional play. In one study, more than 50% of athletes with ADHD in NCAA Division I sports reported at least one prior concussion, compared to 14% of athletes without ADHD (17). Given the substantial negative impact of concussions on neurocognitive function, preventing concussions whenever possible is an important goal (17). Our data is in line with prior research, both for overall ADHD, ADHD without stimulant use, and the comparatively lower risk for concussion in athletes receiving stimulant medications (18, 19). Our cohort with ADHD and stimulant use showed no statistical difference in concussion occurrence compared to athletes without ADHD, which is further evidence in support of stimulant use preventing concussions in this population (19). Prior research has shown fractures involving the skull are less common in patients with ADHD on stimulants and that the detrimental effect of concussions that do occur is minimized in patients on stimulants compared to ADHD patients without stimulant use (18–20).
Concussions were not the only improved outcome present in our stimulant group. Compared to baseball players without ADHD, athletes with ADHD on stimulants were less likely to have fractures of the axial skeleton, less likely to have any fractures at all, and less likely to injure the head, neck, upper limb, and lower limb. Reduced fracture rates in ADHD patients on stimulants has been reported in prior research (20), but the decreased rate of baseball specific injuries in the limbs and head or neck is a significant finding with many possible explanations as to an underlying mechanism. For example, the decreased sensation of pain associated with chronic stimulant use may result in a decrease rate of reported injuries (21), even if the true occurrence rate were identical. It is also possible that the increased situational awareness, acceleration capability, and reaction speed associated with stimulant use allows these players to avoid collisions or mistakes that would have led to injuries in neurotypical players and ADHD athletes without stimulants (22). Without specific case-by-case analysis of the mechanism of injury, it is difficult to make definitive statements on the cause behind this strong association. However, the difference in risk is substantial enough to warrant further investigation.
Stimulant use is a controversial topic within the baseball community (23). Stimulants have many beneficial effects for youths with ADHD that go beyond academic performance (24), yet there is a persistent suspicion that some baseball players may be feigning ADHD symptoms in order to gain an exemption for stimulant use (25). This perception has led to large organizations like the MLB reducing the number of exemptions allowed over time, despite an increase in the overall prevalence of ADHD (26). Given the potential financial incentives of performance enhancing drug use in baseball, it is understandable that fans may be concerned regarding a potential advantage given to some players. However, our data indicate that stimulant use is associated with fewer head and neck injuries for adolescent players with ADHD. Head and neck injuries correspond to a significant amount of healthcare costs and lost playing time (22). While it is beyond the scope of this study, this difference in injury risk associated with stimulant use should be given considerable weight in discussions around medication regulations in sports.
As the average age in our study is 17.7 years old, our findings are more relevant for athletes at the high school and early collegiate level. Stimulants are the mainstay of ADHD treatment due to their highly beneficial effects on academic performance, as well as social development, emotional regulation, and overall mental health (13, 24). Stimulants are also associated with lower rates of injuries such as fractures in all patients with ADHD, not only baseball players (20). Therefore, it is crucial that individuals with ADHD do not experience undue restriction on ADHD treatment. While athletic scholarships may provide some incentive to feign ADHD symptoms to obtain stimulants, the fact remains that roughly 10% of youths in the United States have ADHD (1). Detecting and diagnosing true ADHD should be the responsibility of physicians and psychologists, and those with diagnoses should be able to continue using stimulant medications without stigmatization or undue restriction by athletic associations.
While our study avoids many potential confounders, such as age, sex, and race, there are some limitations that restrict the generalizability of our findings. The data obtained from TriNetX are deidentified and presented in aggregate form, which prevents analysis on an individual level and restricts important information such as severity of ADHD symptoms. Furthermore, electronic medical records are limited to information entered by health care providers; it is extremely likely that our findings are an underestimate of baseball injuries as we only included patients identified as playing baseball through their health record. Similarly, medications may be entered in the record but not taken. However, the large size of our study mitigates most of these limitations, and ensures our findings have some generalizability to ADHD athletes in baseball.
Given the growing population of ADHD youth, and the ongoing debate around stimulant use in athletics, our study is relevant to a wide variety of patients, providers, and the baseball community at large. Still, further research is needed to investigate potential causes behind the associations identified. As more is discovered about the link between ADHD and injuries, the use of stimulants in baseball should be continually reassessed. With collaborative effort, the rate of injuries in ADHD athletes might be reduced, allowing more players to continue enjoying the quintessential American pastime.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
EWH had full access to all the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis. EWH served as senior author, JMF served as first author, ARS served as second author, and SRB served as third author. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. Children and adolescents, 2016. J Clin Child Adolesc Psychol. (2018) 47(2):199–212. doi: 10.1080/15374416.2017.1417860
2. Faraone S V, Asherson P, Banaschewski T, Biederman J, Buitelaar J, Ramos-Quiroga J, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers. (2015) 1:1–23. doi: 10.1038/NRDP.2015.20
3. Ng QX, Ho CYX, Chan HW, Yong BZJ, Yeo WS. Managing childhood and adolescent attention-deficit/hyperactivity disorder (ADHD) with exercise: a systematic review. Complement Ther Med. (2017) 34:123–8. doi: 10.1016/J.CTIM.2017.08.018
4. O’Connor BC, Fabiano GA, Waschbusch DA, Belin PJ, Gnagy EM, Pelham WE, et al. Effects of a summer treatment program on functional sports outcomes in young children with ADHD. J Abnorm Child Psychol. (2014) 42(6):1005–17. doi: 10.1007/S10802-013-9830-0
5. State of Play 2021 — The Aspen Institute Project Play. Available at: https://www.aspenprojectplay.org/state-of-play-2021/introduction (Accessed August 28, 2022).
6. Zaremski JL, Zeppieri G, Tripp BL. Sport specialization and overuse injuries in adolescent throwing athletes: a narrative review. J Athl Train. (2019) 54(10):1030–9. doi: 10.4085/1062-6050-333-18
7. Evans SI, Hale EW, Silverman MS. Mechanisms of bodily harm in emergency department youths with ADHD. Front Child Adolesc Psychiatry. (2022) 0:5. doi: 10.3389/FRCHA.2022.1033822
8. Lucasti CJ, Dworkin M, Warrender WJ, Winters B, Cohen S, Ciccotti M, et al. Ankle and lower leg injuries in professional baseball players. Am J Sports Med. (2020) 48(4):908–15. doi: 10.1177/0363546520902135
9. Walsh CJ, Rosenberg SL, Hale EW. Obstetric complications in mothers with ADHD. Front Reprod Health. (2022) 1AD(0):90. doi: 10.3389/FRPH.2022.1040824
10. Hale EW, Murphy MO, Thompson KP. H is for hypersexual: sexuality in youths with ADHD. Front Child Adolesc Psychiatry. (2022) 1AD(0):7. doi: 10.3389/FRCHA.2022.1048732
11. Yoon Y, Kennis M, Hale EW. Post-Operative complications and ADHD. Front Child Adolesc Psychiatry. (2022) 0:4. doi: 10.3389/FRCHA.2022.1032559
12. TriNetX. Available at: https://trinetx.com/real-world-resources/publications/trinetx-publication-guidelines/ (Accessed July 11, 2022).
13. Groom MJ, Cortese S. Current pharmacological treatments for ADHD. Curr Top Behav Neurosci. (2022) 57:19–50. doi: 10.1007/7854_2022_330
14. Aghakhani K, Kordrostami R, Memarian A, Asl ND, Zavareh FN. The association between type of spine fracture and the mechanism of trauma: a useful tool for identifying mechanism of trauma on legal medicine field. J Forensic Leg Med. (2018) 56:80–2. doi: 10.1016/J.JFLM.2018.01.004
15. Lambert MJ, Fligner DJ. Avulsion of the iliac crest apophysis: a rare fracture in adolescent athletes. Ann Emerg Med. (1993) 22(7):1218–20. doi: 10.1016/S0196-0644(05)80994-1
16. Farooqi AS, Lee A, Abreu E, Talwar D, Maguire KJ. Epidemiology of pediatric baseball and softball player injuries. Orthop J Sports Med. (2021) 9(12):1–8. doi: 10.1177/23259671211052585
17. Alosco ML, Fedor AF, Gunstad J. Attention deficit hyperactivity disorder as a risk factor for concussions in NCAA division-I athletes. Brain Inj. (2014) 28(4):472–4. doi: 10.3109/02699052.2014.887145
18. Iaccarino MA, Fitzgerald M, Pulli A, Woodworth KY, Spencer TJ, Zafonte R, et al. Sport concussion and attention deficit hyperactivity disorder in student athletes: a cohort study. Neurol Clin Pract. (2018) 8(5):403–11. doi: 10.1212/CPJ.0000000000000525
19. Ali M, Dreher N, Hannah T, Li A, Asghar N, Spiera Z, et al. Concussion incidence and recovery among youth athletes with ADHD taking stimulant-based therapy. Orthop J Sports Med. (2021) 9(10):1–6. doi: 10.1177/23259671211032564
20. Zhang SW, Shen D, Yan YT. ADHD, stimulant medication use, and the risk of fracture: a systematic review and meta-analysis. Arch Osteoporos. (2021) 16(1):81. doi: 10.1007/s11657-021-00960-3
21. Lei BH, Chen JH, Yin HS. Repeated amphetamine treatment alters spinal magnetic resonance signals and pain sensitivity in mice. Neurosci Lett. (2014) 583:70–5. doi: 10.1016/J.NEULET.2014.09.031
22. van der Meere JJ, Shalev RS, Borger N, Wiersema JR. Methylphenidate, interstimulus interval, and reaction time performance of children with attention deficit/hyperactivity disorder: a pilot study. Child Neuropsychol. (2009) 15(6):554–66. doi: 10.1080/09297040902758803
23. How ADHD Treatment Changed the Game for Pitcher Scott Eyre. Available at: https://www.additudemag.com/a-giant-accomplishment/ (Accessed August 28, 2022).
24. Coghill D. The benefits and limitations of stimulants in treating ADHD. Curr Top Behav Neurosci. (2022) 57:51–77. doi: 10.1007/7854_2022_331
25. Number of Baseball Players Given Drug Exemptions Grows Slightly—The New York Times. Available at: https://www.nytimes.com/2009/12/02/sports/baseball/02baseball.html?_r=2 (Accessed August 28, 2022).
26. Exemptions for ADHD drugs in MLB drop to lowest in decade | AP News. Available at: https://apnews.com/article/d284e3f57cdf4b258b579c99e154b38d (Accessed August 28, 2022).
Keywords: ADHD, baseball, stimulants, controversy, sports
Citation: Feldkamp JM, Stevens AR, Blaakman SR and Hale EW (2023) Baseball injuries in adolescent athletes with ADHD. Front. Sports Act. Living 4:1032558. doi: 10.3389/fspor.2022.1032558
Received: 31 August 2022; Accepted: 29 November 2022;
Published: 9 January 2023.
Edited by:
Elizabeth Elder, University of Alabama, United StatesReviewed by:
Jennifer Hogg, University of Tennessee at Chattanooga, United StatesWilliam Magilione, Independent Researcher, Switzerland
© 2023 Feldkamp, Stevens, Blaakman and Hale. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elijah W. Hale ZWxpamFoLmhhbGVAY3VhbnNjaHV0ei5lZHU=
Specialty Section: This article was submitted to Elite Sports and Performance Enhancement, a section of the journal Frontiers in Sports and Active Living
 John M. Feldkamp1
John M. Feldkamp1 Elijah W. Hale
Elijah W. Hale