- 1Department of Otolaryngology, University of Rochester, Rochester, NY, United States
- 2Physical Therapy Department, University of Rochester, Rochester, NY, United States
- 3Physical Therapy Department, University of Pittsburgh, Pittsburgh, PA, United States
- 4Department of Neuroscience, University of Rochester, Rochester, NY, United States
- 5Department of Biomedical Engineering, University of Rochester, Rochester, NY, United States
Wearing a facemask (FM) reduces the spread of COVID-19, but it also blocks a person's lower visual field. Many new public safety rules were created in response to COVID-19, including mandated FM wearing in some youth sports like youth ice hockey. We hypothesized that FM wearing in youth hockey players obstructs the lower field of view and may impact safety. Youth hockey players (n = 33) aged 12.03 (1.6) years button press when they saw an LED on the floor turn on in two conditions (wearing FM or no FM) in random order. An interleaved one-up/one-down two-alternative-forced-choice adaptive staircase design was used. Visual thresholds were calculated for each condition and participant. The visual angle threshold (VAT) was determined using standing eye height and the linear distance from the tip of the skates to the visual threshold. Paired t-tests determined whether mask wearing changed the VAT. We modeled the probability a player could see the puck on their stick in four distinct scenarios to estimate the potential impact of FM wearing during hockey play. The average unmasked VAT (11.4 degrees) was significantly closer to the skates than the masked VAT (20.3 degrees) (p < 0.001). Our model indicated a significant reduction in ability to visualize the puck using peripheral vision when more upright while wearing a FM. FM wearing compromised their lower visual field, suggesting a downward head tilt may be necessary to see the puck. Playing ice hockey while wearing a FM may lead to unsafe on-ice playing conditions due to downward head tilt to see the puck.
Introduction
While the COVID-19 pandemic is far from eradicated, there are definite signs of hope for a return to normalcy. Vaccine distribution has begun and most adults and teenagers (but not children under 12) are eligible to receive the vaccine in the US (Centers for Disease Control Prevention, 2021). Several studies have demonstrated that policies of universal masking contribute to preventing the spread of COVID-19 (Hendrix et al., 2020; Payne et al., 2020; Van Dyke et al., 2020; Wang et al., 2020), and the Centers for Disease Control and Prevention continues to recommend mask wearing for non-vaccinated individuals (Centers for Disease Control and Prevention) and many institutions continue to have mask mandates, especially for non-vaccinated individuals. With the emergence of contagious variants, considerations other than disease transmission are relevant to decisions about universal masking in youth sports. This is highly relevant as winter approaches and there is a greater emphasis on indoor sports that were largely cancelled or required athletes to wear masks during play (Dergaa et al., 2021).
Although wearing a facemask mitigates the spread of COVID-19, wearing a facemask has also been shown to block the lower visual field (El-Nimri et al., 2020; Young et al., 2020; Klatt and Anson, 2021; Weber et al., 2021). Restricting the peripheral visual field increased reaction times and has been linked to reduced overall sports performance in football and downhill skiing (Loopeker and Rowley, 2001; Ruedl et al., 2011; Miller et al., 2019). Blocking the lower visual field promotes downward head tilt, which reduces how far ahead obstacles can be detected (Timmis and Buckley, 2012). Blocking the lower visual field during walking may lead to a trip or fall. Obstruction of the lower visual field related to wearing a facemask may worsen balance for people with higher fall risk (Kal et al., 2020; Klatt and Anson, 2021). Another arena where facemask wearing may have detrimental consequences related to increased risk for injury is the sport of ice hockey. Ice hockey was designated as a “moderate or high-risk” sport related to the potential for COVID-19 spread in several US states, and rules were developed for players/coaches/officials to wear facemasks (Maine Department of Economic Comminuty Development, 2021; MinnesotaHockey, 2021). In some cases, wearing facemasks was mandated for any on-ice hockey activities at all age levels. However, not all states/countries adopted this mandate for players. Although most early evidence suggests that healthy individuals are only mildly impacted while wearing a FM during exercise (Shaw et al., 2020; Hopkins et al., 2021; Mapelli et al., 2021; Shein et al., 2021), others have reported significant reductions in respiratory capacity in healthy adults (Fikenzer et al., 2020; Lässing et al., 2020; Driver et al., 2021). To date the impact of mask wearing on aspects of exercise or sports participation, such as player safety, has received little attention.
Ice hockey players wearing a FM may have reduced lower field of view and to facilitate seeing the puck may need to tilt their head down. Tilting the head downward reduces the “look ahead” window, effectively shortening the reaction time for contact avoidance (Patla and Vickers, 2003). In fast moving contact sports like ice hockey, not being able to see your opponent soon enough because of downward head tilt may lead to more frequent body contact/checking which is the most common cause of player injury (Brust et al., 1992; Emery et al., 2011; Brenner et al., 2014; Mosenthal et al., 2017; Simmons et al., 2017). The Hockey Equipment Certification Counsel Inc. promotes an education program titled “Heads-Up, Don't Duck” to specifically create awareness of the increased risk of cervical spine injuries when looking downward (HECC). Therefore, a scenario where ice hockey players tilt their head downward to play the puck due to a restricted lower visual field (from wearing a facemask while playing), may lead to unsafe on-ice conditions.
Although it has long been known that blocking the lower visual field impairs walking ability (Marigold et al., 2007; Marigold and Patla, 2008) and reaction times in football and alpine skiing (Ruedl et al., 2011; Miller et al., 2019), the extent to which wearing a mask blocks the lower field of view in the context of ice hockey is unknown. Here we report on whether mask wearing in youth hockey players significantly restricts their lower field of view. We hypothesized that youth ice hockey players would experience a significant reduction in the lower visual field when wearing a facemask. We additionally modeled the relationship between the FM induced reduction in the lower visual field and the ability to see a puck on their stick. We hypothesized that wearing a facemask would impair the ability of youth hockey players to use peripheral vision to see a puck on their stick.
Methods
Subjects
Thirty-three youth hockey players (5 girls, 28 boys) average age 12.03 (SD 1.6) were recruited and provided written assent (ages <18) to participate in this study approved by the institutional review board at the University of Rochester Medical Center. Written parental permission was also provided for participants under 18. All experimental participation took place at Rochester Ice Center in Fairport, NY. At the time of data collection, all persons inside the building at Rochester Ice Center were required to wear masks, except when on the ice for practice or games. Participants were tested using the FM they wore at the time of testing as this method pragmatically represented the FM type they were likely to wear when playing. No effort was made to adjust fit of the FM for any participant. Participants were compensated with a $15 gift card to a sporting goods store after completion.
Experimental Setup
Apparatus
An individually addressable light emitting diode (LED) strip (WS2812B ECO LED Strip, BTF-Lighting Technology Co., Ltd., Guangdong, China) three meters in length (180 LEDs, 60 LEDs/m) was centered on a black plastic mat, see Figure 1. Distance between each LED was 12 mm. During the experiment, individually addressed LEDs were powered for 200 ms and specified to be white light for maximum contrast with the black plastic mat. These colors were selected to better simulate the color contrast of the typical black hockey puck on a white ice surface. A wired Xbox (Microsoft, Inc., Redmond, WA) controller allowed participants to respond during the protocol by clicking either the right or left buttons with their index fingers for “yes” and “no” responses, respectively. A custom MATLAB 2018a (The MathWorks, Inc., Natick, MA) script and an Arduino Nano3 (Arduino LLC., Torino, Italy) were used to play the auditory tone and turn on/off individual LEDs as well as capture participant responses (Xbox button press). All data were analyzed offline using custom MATLAB scripts.
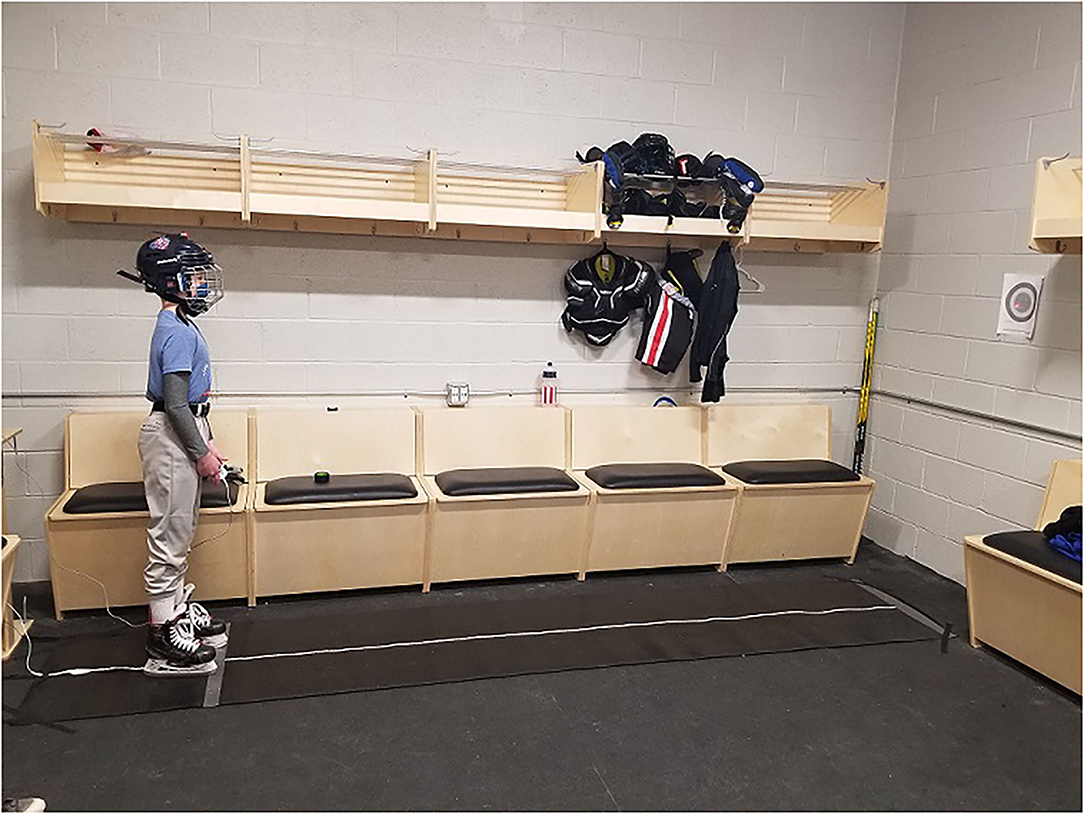
Figure 1. An exemplar demonstrating the experimental set-up. Participants were instructed to keep the helmet mounted laser pointer in the center of the bulls-eye (Radius 9.1 cm) taped to the wall at eye height 12 feet away. Subjects stood with a comfortable stance straddling the LED strip in their skates holding the Xbox controller so that it was not visible while looking straight ahead.
Protocol
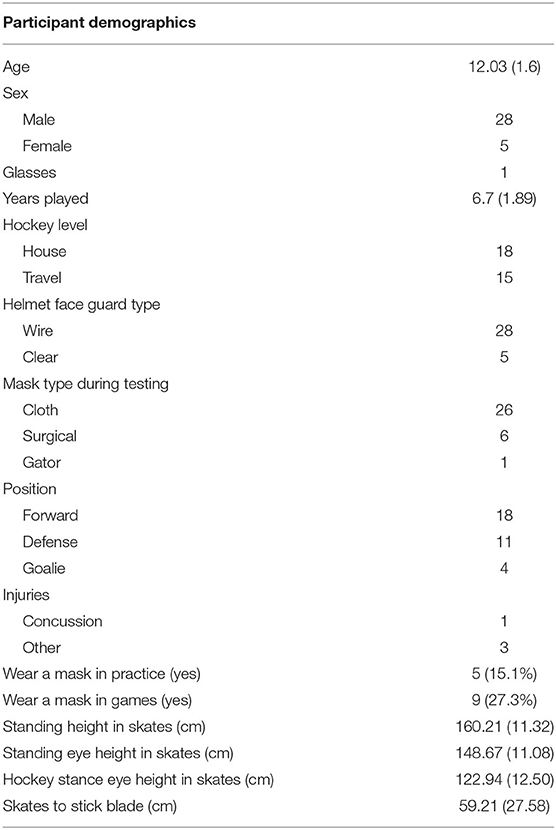
After providing assent/permission or consent to participate, each participant provided demographic data including age and sex, and sport specific information including years played, level of play (house or travel), whether they wear glasses during play, type of faceguard (wire/clear plastic), their playing position (center/wing/defense/goalie), and the type of personal facemask they wore for the experiment, see Table 1 for demographics. Participants indicated whether they had experienced a concussion or other injuries in the last 6 months during play. Participants indicated whether they wore a facemask while skating during either practice or games. If they responded “yes” to either of those questions they were asked what type of mask they wore and whether they were required to wear a mask. If required to wear a mask they indicated who provided the mask for them to use. Finally, participants who reported wearing a mask during practice or game play were asked, “Do you feel you have to look down more with the mask on to see the puck than when you do not wear a mask?” While wearing their hockey skates standing height, standing eye height, hockey stance eye height, and distance from the tip of their skates to the toe and heel of their stick were measured for all players except goalies. Hockey stance positioning includes holding the stick with both hands, resting the stick blade on the floor in front of them with their head up, back straight, and both knees slightly bent. This terminology is common in youth hockey all participants easily understood.
A laser pointer was attached to their helmet and participants were then familiarized with the two-alternative-forced-choice (2AFC) paradigm with a demonstration that included 10 auditory cues (300 ms 200 Hz tones) that served as a prompt to respond. For six auditory cues an LED turned on, and for four auditory cues no LED was turned on. During the familiarization task, participants were allowed to look directly at the LED strip to ensure visualization of the LEDs when turned on. This task familiarization ensured that the participants would click the correct response button. The familiarization task was repeated until the participant demonstrated understanding of the task. The experimental set up is shown in Figure 1.
Participants were instructed to keep the helmet mounted laser pointer “as close to the center of a bulls-eye target as possible” which was taped to the wall at their eye height (in skates) 12 feet in front of them. This distance was determined to be achievable but sufficiently challenging to require continuous visual attention in early piloting. Participants were tested in two conditions (wearing a facemask or no facemask) in random order determined by a coin flip. Each condition consisted of 60 trials (paired audio cues and responses). An interleaved 2AFC adaptive staircase design was used with 30 trials per staircase (Levitt, 1971). Each staircase included five trials with auditory cues intentionally paired with the LED remaining off to check for task attention (trials 3, 9, 17, 21, 25 for the descending staircase and 2, 10, 16, 22, 27 for the ascending staircase). The remaining 25 cues presented synchronous auditory and visual (LED) cues. The auditory cues were 300 ms 200 Hz tones from the internal speakers of the data acquisition computer at maximum volume (Dell Lattitude 7400, Dell, Inc.). The visual cues were white light LEDs turned on for a 200 ms duration. This supra-threshold stimulus duration was twice that needed for a visual discrimination task (Croker and Maratos, 2011). We opted for a brief but supra-threshold visual stimulus as the hockey puck is never invisible. The inter-trial interval varied randomly between 1.5 and 2.5 seconds.
For both staircases, the maximum LED number was 182 and the minimum LED number was one. Whether a trial was to test the up or down staircase was determined randomly, with two exceptions. The number of consecutive steps per staircase was randomly determined (integers between one and five) following each staircase reversal. The next step(s) must be for the other staircase. Additionally, if all 30 trials were completed for a particular staircase, the remaining trials must all be from the other staircase. The step sizes were predefined in order [20, 16, 14, 12, 10, 9, 7, 5, 3, 2, 1] allowing for 11 staircase reversals or consecutive changes in step sizes (Wetherill and Levitt, 1965). This method ensures more stimuli near the threshold (Roditi and Crane, 2012). If the next step size was less than the pre-set minimum step size (one LED), the step size was specified as one LED.
Data Analysis
As a first pass, the ascending and descending staircases were examined for convergence based on overlapping histograms to ensure appropriate task performance. The binary data (no = 0, yes = 1) were bootstrapped with 100 replications and fit to a psychometric curve. The mean of the bootstrapped psychometric fits was calculated as the threshold (in units of LEDs) for each condition and participant and corresponded to the 50% point of subjective equality (Levitt, 1971; Roditi and Crane, 2012). The visual angle threshold was determined using standing eye height and the linear distance from the tip of the skates to the LED threshold. A paired t-test determined whether mask wearing changed the visual angle threshold. Hockey stance visual angle was determined using hockey stance eye height and the midpoint of the stick blade for all non-goalie players. To estimate the potential impact of mask wearing during hockey play, we modeled the probability a player would see the puck in several simulated conditions using Solver (Frontline Systems, Inc.). We created four normally distributed simulation models bootstrapped on the collected empirical data (mean and standard deviation). We ran 10,000 replications for each simulation. The four models used the visual angle threshold with mask and without mask as well as the calculated visual angle from eye height of the subject standing upright and in hockey stance with respect to the distance between the skates and the middle of the hockey stick. The models were run with logic, pairing conditions together to resemble four distinct possible outcomes simulating hockey playing: (1) masked paired with upright height (least ideal scenario), (2) unmasked paired with hockey stance height (most ideal scenario), (3) unmasked paired with upright height, and (4) masked paired with hockey stance height. Alpha was specified for each statistical comparison as α = 0.05 as they were considered independent questions.
Results
Four participants did not demonstrate staircase convergence (indicating incorrect task performance) and one participant had missing data due to technical problems and were not included in the statistical analyses. The participants were 84.8% male and 45.4% (n = 15) played travel hockey last season, with the remaining participants being house players. Four individuals reported an injury last season, and nine individuals reported wearing a mask during practice or game play at least for some of the season, see Table 1. Six of the nine individuals reported that they had to look down to play the puck when wearing a mask compared to when unmasked.
The average unmasked visual angle threshold [11.4 degrees (SD 5.9 degrees)] was significantly smaller (closer to the skates) than the masked visual angle threshold [20.3 degrees (SD 8.0 degrees)], [t(1, 26) = −6.2515, p < 0.0000012, Cohen's d = −1.2], as shown in Figure 2. The average hockey stance visual angle was 29.73 degrees (SD 3.79 degrees). Four of the players had visual thresholds that exceeded their hockey stance visual angle.
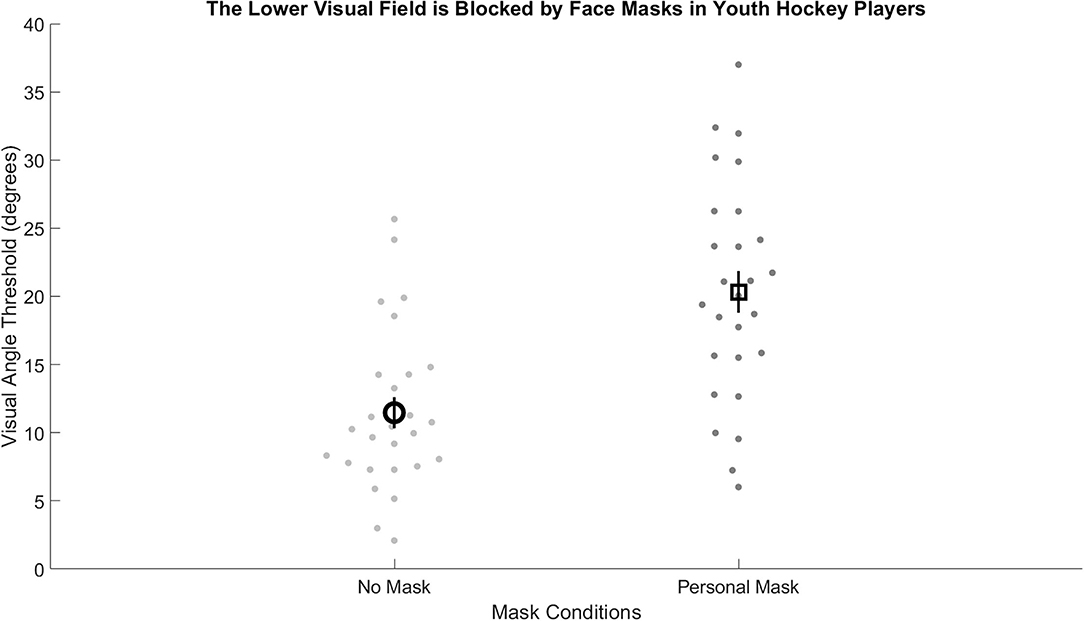
Figure 2. Visual angle thresholds for the no mask (light gray) were significantly smaller than for the masked (dark gray) condition. Group averages represented by a bolded circle (no mask) and a bolded square (masked). Error bars represent standard error.
Model Results
The results of the Solver models indicated approximately 20% reduction in the probability that a player would be able to see a puck on their stick blade using peripheral vision if wearing a facemask and standing closer to upright, see Figure 3. A further comparison of the distribution of visual angle thresholds compared to visual angles necessary to see the center of the hockey stick blade demonstrated significant overlap (overlap of 90% confidence intervals) between empirically derived masked visual angle thresholds and estimated visual angles needed in both hockey stance and upright stance conditions, see Figure 4. The model results demonstrate that players will periodically need to tip their head down to visualize the puck while skating.
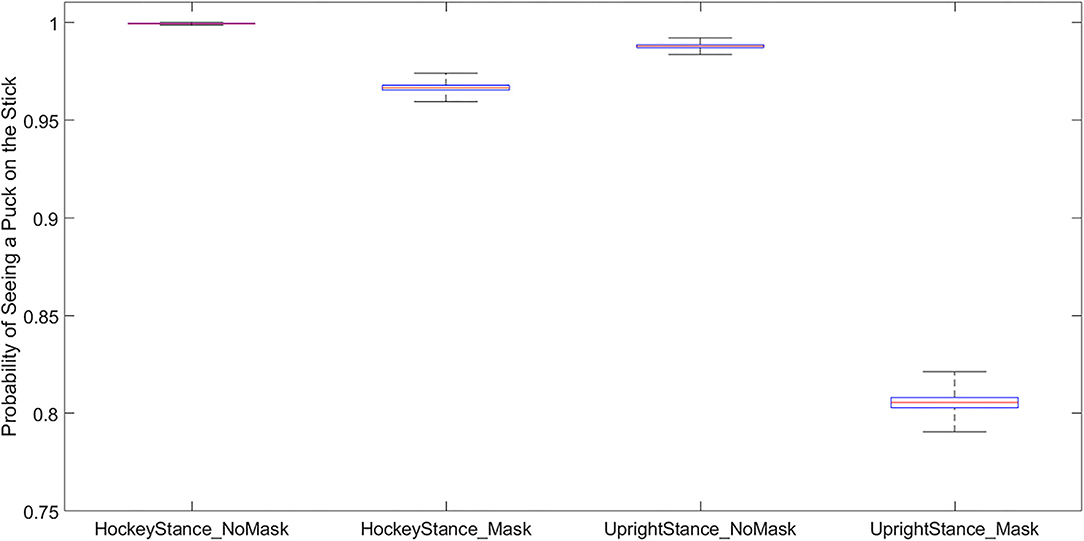
Figure 3. A box plot depicting the cross model results. This plot shows the percent chance the player could see the center of the stick blade compared across various conditions. The y-axis is the probability that the puck will be seen (yes = 1), note the significant drop in puck on stick visibility (~20%) when masked players are more upright.
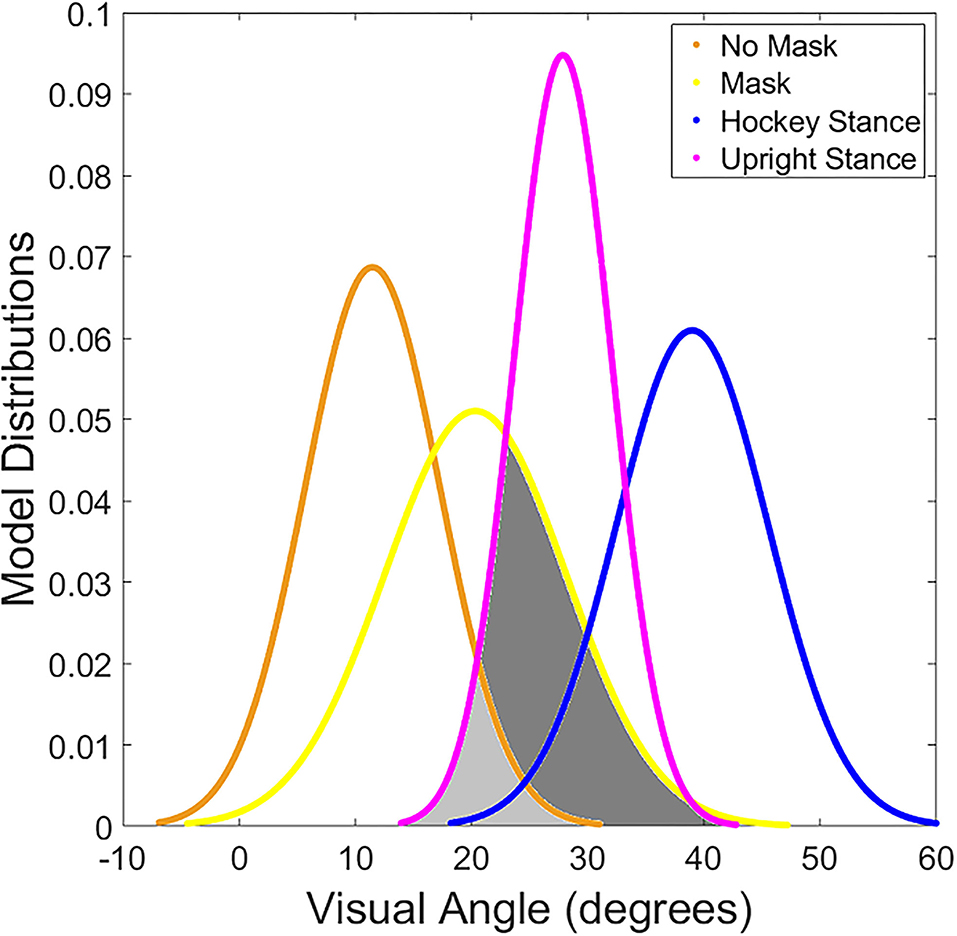
Figure 4. Depicts the distribution of visual thresholds determined for each model. The yellow (FM condition) and orange (No mask) lines illustrate the range of visual angles based on the empirical visual angle threshold data. The purple (upright stance) and blue (hockey stance) lines show the range of visual angles for the cohort across the height conditions. Where the orange or yellow line overlaps the blue or purple line (shaded in light and dark gray for emphasis) represents circumstances where the puck on the stick would not be visible without tilting the head down.
Discussion
The primary result from this novel investigation indicates that wearing a facemask significantly restricts the lower field of view in youth hockey players. Although not surprising, to our knowledge this has not previously been demonstrated in youth hockey players. These thresholds suggest that in a “heads-up” hockey stance, the lower visual field angular thresholds would allow most if not all tested players to visualize their stick blade only when not wearing a mask. When wearing a facemask, the fraction of time that the puck would be visible in the peripheral field of view is significantly reduced. Four of the non-goalie participants had a masked visual angle threshold larger than the visual angle from the eyes to the middle of the stick blade while in a hockey stance. Those four individuals would not be able to use peripheral vision to see the puck on the stick blade while skating with a mask on. Thus, to visualize the puck on the stick players must tilt their head down rather than relying on peripheral vision.
We further examined the potential for on ice change in head tilt behavior by relating the masked visual angle threshold to the calculated visual angles in both a hockey stance and an upright stance. It is unlikely that players maintain the exact hockey position height while in play on the ice. Our model conservatively accounts for this by examining the frequency the puck would not be visible given masking and stance criteria while holding the stick placement relative to the skates constant. While masked we expect the players to be able to see the puck using peripheral vision roughly 96% while in their hockey stance. The probability of seeing the puck when more upright is reduced to about 80%. Often during game play players skate in a more upright position than the hockey stance which is more analogous to the non-skating face off position. An important caveat to the interpretation of these models is that if the stick is not perfectly straight out in front of a masked player, the masked player may have to look down more often as the visual angle will shift closer to the visual threshold. Similarly, if the puck was held to the player's side the distance between puck and player would be shortened, further reducing visibility. Although we employed a conservative model to more closely link the visual angle thresholds to skating performance, additional studies are needed to examine on ice performance including both maintaining puck possession and avoiding body contact while masked.
Overall, the combined visual threshold results and modeling suggest that youth hockey players wearing facemasks would need to adopt head-down behaviors more frequently to see the puck. Head-down positioning increases the chance for player-to-player collision which is the primary cause of on-ice injury (Brenner et al., 2014; Black et al., 2016; Simmons et al., 2017). Restricted peripheral vision has been shown to reduce reaction times for visual targets detection (Miller et al., 2019). Hockey players with only slightly obstructed visual fields from protective equipment (face cages and face shields) also demonstrate slower reaction times to visual targets (Ing et al., 2002; Dowler et al., 2009). Increased oculomotor variability for target tracking and gaze shifting was associated with more frequent high acceleration collision impacts in youth ice hockey (Kiefer et al., 2018). The current results suggest that the on-ice use of FM in youth hockey may increase the risk for on-ice injury. The current results do not address potential for disease transmission during play, but highlight a previously unknown risk to player safety that has relevance to universal masking during participation in youth ice hockey. Ice hockey players appear to be special case population such that facemask wearing during participation may have unintentional effects that increase risk for injury.
Limitations
The main limitation to this study is the off-ice, non-play oriented determination of a lower visual field threshold. The LEDs represent a stationary target, and thus a player's ability to intercept a moving puck cannot be determined. However, skating while possessing the puck may require at least periodic visual updating. We employed a conservative model to account for the static nature of the testing environment. Despite being well representative of the participants in this study, variations in facemask styles may not represent those used by players not participating in this study. Older youth hockey players or adults may have different results. This study did not address the impact of mask wearing during ice hockey play on disease transmission or respiration. The small sample size prevented within group comparisons to determine effects from position or type of face shield.
Conclusion
Facemask wearing restricted the lower visual field in youth hockey players. Puck on stick visibility was compromised suggesting an increase in downward head tilt would be necessary to see the puck on the stick while playing ice hockey while wearing a FM. The current results suggest that the on-ice use of FM in youth hockey may be associated with increased use of head-down positioning that might lead to greater injury incidence during play. However, the association between FM use and an increase in injury risk should be evaluated directly.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by University of Rochester, Research Subjects Review Board. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author Contributions
EA and BK conceived and designed the study. EA, KC, and VD collected study data. EA, KC, and BC performed data analysis. EA drafted the initial version of the manuscript. EA, VD, KC, BK, and BC critically edited the manuscript. All authors contributed to the article and approved the submitted version.
Funding
EA was supported in part by the National Institutes of Health (NIDCD K23 DC018303).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
Thank you to all the youth hockey players and parents who participated in this study. Thank you to the Rochester Junior Americans and Rochester Ice Center for supporting this study and providing us the space to conduct the study. Paul Allen for thoughtful advice and modeling suggestions.
References
Black, A. M., Macpherson, A. K., Hagel, B. E., Romiti, M. A., Palacios-Derflingher, L., Kang, J., et al. (2016). Policy change eliminating body checking in non-elite ice hockey leads to a threefold reduction in injury and concussion risk in 11- and 12-year-old players. Br. J. Sports Med. 50, 55–61. doi: 10.1136/bjsports-2015-095103
Brenner, J. S., Brooks, A., Demorest, R. A., Halstead, M. E., Weiss Kelly, A. K., Koutures, C. G., et al. (2014). Reducing injury risk from body checking in boys' youth ice hockey. Pediatrics 133, 1151–1157. doi: 10.1542/peds.2014-0692
Brust, J. D., Leonard, B. J., Pheley, A., and Roberts, W. O. (1992). Children's ice hockey injuries. Am. J. Dis. Child. 146, 741–747. doi: 10.1001/archpedi.1992.02160180101026
Centers for Disease Control Prevention (2021). Key Things to Know About COVID-19 Vaccines. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/keythingstoknow.html?s_cid=10493:isthecovidvaccineout:sem.ga:p:RG:GM:gen:PTN:FY21
Centers for Disease Control Prevention. National Center for Injury Prevention Control. COVID-19: Considerations for Wearing Masks. CDC. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cloth-face-cover-guidance.html (accessed August 3 2021).
Croker, S., and Maratos, F. A. (2011). Visual processing speeds in children. Child. Dev. Res. 2011, 1–6. doi: 10.1155/2011/450178
Dergaa, I., Abdelrahman, H., Varma, A., Yousfi, N., Souissi, A., Ghram, A., et al. (2021). COVID-19 vaccination, herd immunity and the transition toward normalcy: challenges with the upcoming sports events. Ann. Appl. Sport Sci. 1:10. doi: 10.52547/aassjournal.1032
Dowler, P. M., Pearsall, D. J., and Stapley, P. J. (2009). Effects of ice hockey facial protectors on the response time and kinematics in goal-directed tasks. Proc. Inst. Mech. Eng. Part P J. Sport. Eng. Technol. 223, 99–108. doi: 10.1243/17543371JSET29
Driver, S., Reynolds, M., Brown, K., Vingren, J. L., Hill, D. W., Bennett, M., et al. (2021). Effects of wearing a cloth face mask on performance, physiological and perceptual responses during a graded treadmill running exercise test. Br. J. Sports Med. doi: 10.1136/bjsports-2020-103758. [Epub ahead of print].
El-Nimri, N. W., Moghimi, S., Fingeret, M., and Weinreb, R. N. (2020). Visual field artifacts in glaucoma with face mask use during the COVID-19 pandemic. J. Glaucoma 29, 1184–1188. doi: 10.1097/IJG.0000000000001706
Emery, C., Kang, J., Shrier, I., Goulet, C., Hagel, B., Benson, B., et al. (2011). Risk of injury associated with bodychecking experience among youth hockey players. CMAJ 183, 1249–1256. doi: 10.1503/cmaj.101540
Fikenzer, S., Uhe, T., Lavall, D., Rudolph, U., Falz, R., Busse, M., et al. (2020). Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin. Res. Cardiol. 109, 1522–1530. doi: 10.1007/s00392-020-01704-y
HECC. HECC.org > Safety Guidelines - Heads Up Don't Duck! A Program to Decrease the Risk for Spinal Cord Injuries. Available online at: http://hecc.org/headsup.html (accessed August 3 2021).
Hendrix, M. J., Walde, C., Findley, K., and Trotman, R. (2020). Absence of apparent transmission of SARS-CoV-2 from two stylists after exposure at a hair salon with a universal face covering policy — Springfield, Missouri, May 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 930–932. doi: 10.15585/mmwr.mm6928e2
Hopkins, S. R., Dominelli, P. B., Davis, C. K., Guenette, J. A., Luks, A. M., Molgat-Seon, Y., et al. (2021). Face masks and the cardiorespiratory response to physical activity in health and disease. Ann. Am. Thorac. Soc. 18, 399–407. doi: 10.1513/AnnalsATS.202008-990CME
Ing, E., Ing, T., and Ing, S. (2002). The effect of a hockey visor and sports goggles on visual function. Can. J. Ophthalmol. 37, 161–167. doi: 10.1016/S0008-4182(02)80058-8
Kal, E. C., Young, W. R., and Ellmers, T. J. (2020). Face masks, vision, and risk of falls. BMJ 1:2. doi: 10.1136/bmj.m4133
Kiefer, A. W., DiCesare, C., Nalepka, P., Foss, K. B., Thomas, S., and Myer, G. D. (2018). Less efficient oculomotor performance is associated with increased incidence of head impacts in high school ice hockey. J. Sci. Med. Sport. 21, 4–9. doi: 10.1016/j.jsams.2017.06.016
Klatt, B. N., and Anson, E. R. (2021). Navigating through a covid-19 world: avoiding obstacles. J. Neurol. Phys. Ther. 45, 36–40. doi: 10.1097/NPT.0000000000000338
Lässing, J., Falz, R., Pökel, C., Fikenzer, S., Laufs, U., Schulze, A., et al. (2020). Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Sci. Rep. 10:22363. doi: 10.1038/s41598-020-78643-1
Levitt, H.. (1971). Transformed up-down methods in psychoacoustics. J. Acoust. Soc. Am. 49:467. doi: 10.1121/1.1912375
Loopeker, K., and Rowley, B. (2001). The Effects of Ski Goggles' Induced Field and Tint on Stability. Pacific University. Available online at: https://commons.pacificu.edu/opt/1379
Maine Department of Economic Comminuty Development (2021). Community Sports | Department of Economic and Community Development. Available online at: https://www.maine.gov/decd/checklists/community-sports
Mapelli, M., Salvioni, E., De Martino, F., Mattavelli, I., Gugliandolo, P., Vignati, C., et al. (2021). “You can leave your mask on”: effects on cardiopulmonary parameters of different airway protection masks at rest and during maximal exercise. Eur. Respir. J. 3:2004473. doi: 10.1183/13993003.04473-2020
Marigold, D. S., and Patla, A. E. (2008). Visual information from the lower visual field is important for walking across multi-surface terrain. Exp. Brain Res. 188, 23–31. doi: 10.1007/s00221-008-1335-7
Marigold, D. S., Weerdesteyn, V., Patla, A. E., and Duysens, J. (2007). Keep looking ahead? Re-direction of visual fixation does not always occur during an unpredictable obstacle avoidance task. Exp. Brain Res. 176, 32–42. doi: 10.1007/s00221-006-0598-0
Miller, R. A., Rogers, R. R., Williams, T. D., Marshall, M. R., Moody, J. R., Hensarling, R. W., et al. (2019). Effects of protective American Football Headgear on peripheral vision reaction time and visual target detection in division I NCAA Football Players. Sport 7:213. doi: 10.3390/sports7090213
MinnesotaHockey (2021). Minnesota Hockey Return to Play Rules & Guidelines. Available online at: https://cdn3.sportngin.com/attachments/document/7e5e-2367056/Minnesota_Hockey_Return_to_Play_Phase_6_FINAL.pdf#_ga=2.28744891.628826342.1615234491-557158269.1615234490
Mosenthal, W., Kim, M., Holzshu, R., Hanypsiak, B., and Athiviraham, A. (2017). Common ice hockey injuries and treatment: a current concepts review. Curr. Sports Med. Rep. 16, 357–362. doi: 10.1249/JSR.0000000000000402
Patla, A. E., and Vickers, J. N. (2003). How far ahead do we look when required to step on specific locations in the travel path during locomotion? Exp. Brain Res. 148, 133–138. doi: 10.1007/s00221-002-1246-y
Payne, D. C., Smith-Jeffcoat, S. E., Nowak, G., Chukwuma, U., Geibe, J. R., Hawkins, R. J., et al. (2020). SARS-CoV-2 infections and serologic responses from a sample of U.S. Navy Service Members — USS Theodore Roosevelt, April 2020. MMWR Morb. Mortal Wkly Rep. 69, 714–721. doi: 10.15585/mmwr.mm6923e4
Roditi, R. E., and Crane, B. T. (2012). Suprathreshold asymmetries in human motion perception. Exp. Brain Res. 219, 369–379. doi: 10.1007/s00221-012-3099-3
Ruedl, G., Herzog, S., Schöpf, S., Anewanter, P., Geiger, A., Burtscher, M., et al. (2011). Do ski helmets affect reaction time to peripheral stimuli? Wilderness Environ. Med. 22, 148–150. doi: 10.1016/j.wem.2010.12.010
Shaw, K., Butcher, S., Ko, J., Zello, G. A., and Chilibeck, P. D. (2020). Wearing of cloth or disposable surgical face masks has no effect on vigorous exercise performance in healthy individuals. Int. J. Environ. Res. Public Health 17, 1–9. doi: 10.3390/ijerph17218110
Shein, S. L., Whitticar, S., Mascho, K. K., Pace, E., Speicher, R., and Deakins, K. (2021). The effects of wearing facemasks on oxygenation and ventilation at rest and during physical activity. PLoS ONE 16:e0247414. doi: 10.1371/journal.pone.0247414
Simmons, M. M., Swedler, D. I., and Kerr, Z. Y. (2017). Injury surveillance of head, neck, and facial injuries in collegiate ice hockey players, 2009-2010 through 2013-2014 academic years. J. Athl. Train. 52, 776–784. doi: 10.4085/1062-6050-52.4.03
Timmis, M. A., and Buckley, J. G. (2012). Obstacle crossing during locomotion: visual exproprioceptive information is used in an online mode to update foot placement before the obstacle but not swing trajectory over it. Gait Posture. 36, 160–162. doi: 10.1016/j.gaitpost.2012.02.008
Van Dyke, M. E., Rogers, T. M., Pevzner, E., Satterwhite, C. L., Shah, H. B., Beckman, W. J., et al. (2020). Trends in county-level COVID-19 incidence in counties with and without a mask mandate — Kansas, June 1–August 23, 2020. MMWR Morb. Mortal. Wkly. Rep. 69, 1777–1781. doi: 10.15585/mmwr.mm6947e2
Wang, Y., Tian, H., Zhang, L., Zhang, M., Guo, D., Wu, W., et al. (2020). Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China. BMJ Glob Heal. 5:e002794. doi: 10.1136/bmjgh-2020-002794
Weber, A., Hohberger, B., and Bergua, A. (2021). Mouth-nose masks impair the visual field of healthy eyes. PLoS ONE 6:e0251201. doi: 10.1371/journal.pone.0251201
Wetherill, G. B., and Levitt, H. (1965). Sequential estimation of points on a psychometric function. Br. J. Math. Stat. Psychol. 18, 1–10. doi: 10.1111/j.2044-8317.1965.tb00689.x
Keywords: facemask, ice hockey, safety, COVID-19, visual fields
Citation: Critelli K, Demiris V, Klatt BN, Crane B and Anson ER (2021) Facemasks Block Lower Visual Field in Youth Ice Hockey. Front. Sports Act. Living 3:787182. doi: 10.3389/fspor.2021.787182
Received: 30 September 2021; Accepted: 11 November 2021;
Published: 06 December 2021.
Edited by:
Marc Norcross, Oregon State University, United StatesReviewed by:
Martin Kopp, University of Innsbruck, AustriaMorteza Taheri, Imam Khomeini International University, Iran
Copyright © 2021 Critelli, Demiris, Klatt, Crane and Anson. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eric R. Anson, ZXJpY19hbnNvbkB1cm1jLnJvY2hlc3Rlci5lZHU=
 Kyle Critelli1
Kyle Critelli1 Brooke N. Klatt
Brooke N. Klatt Eric R. Anson
Eric R. Anson