- 1School of Human Sciences, Exercise and Sport Science, University of Western Australia, Perth, WA, Australia
- 2Laboratory Sport, Expertise and Performance, EA 7370, French Institute of Sport (INSEP), Paris, France
- 3Western Australian Institute of Sport (WAIS), Perth, WA, Australia
- 4Faculty of Biology and Medicine, Institute of Sport Sciences, University of Lausanne, Lausanne, Switzerland
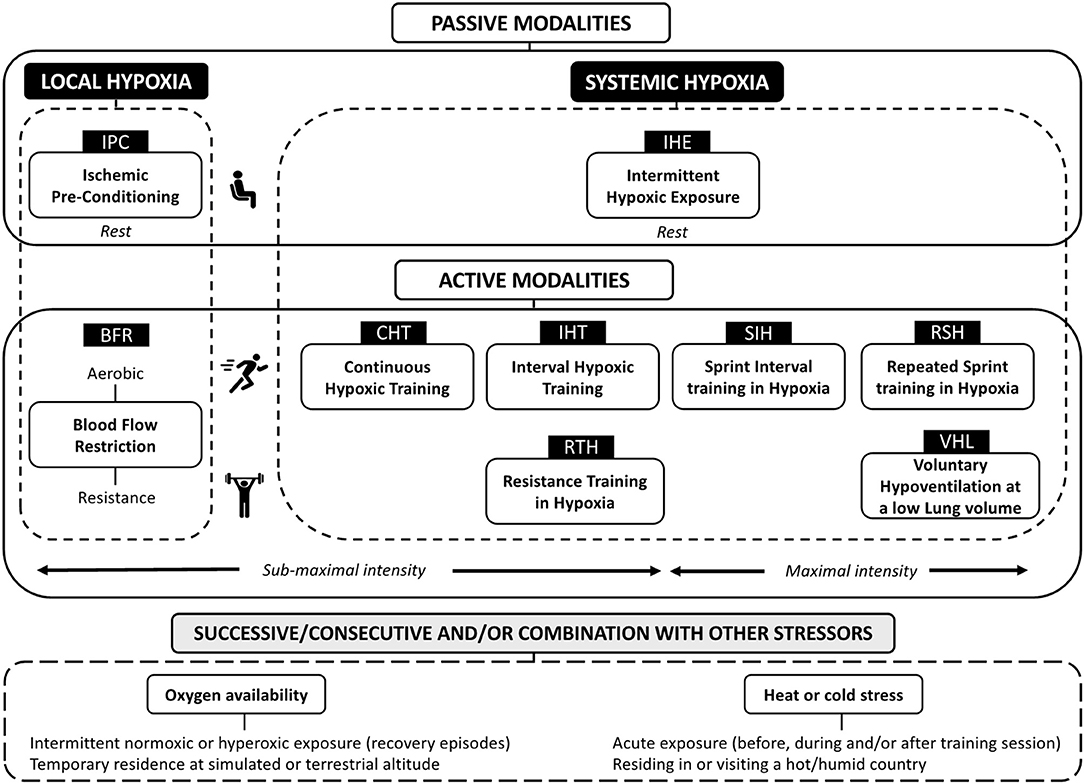
With minimal costs and travel constraints for athletes, the “living low-training high” (LLTH) approach is becoming an important intervention for modern sport. The popularity of the LLTH model of altitude training is also associated with the fact that it only causes a slight disturbance to athletes' usual daily routine, allowing them to maintain their regular lifestyle in their home environment. In this perspective article, we discuss the evolving boundaries of the LLTH paradigm and its practical applications for athletes. Passive modalities include intermittent hypoxic exposure at rest (IHE) and Ischemic preconditioning (IPC). Active modalities use either local [blood flow restricted (BFR) exercise] and/or systemic hypoxia [continuous low-intensity training in hypoxia (CHT), interval hypoxic training (IHT), repeated-sprint training in hypoxia (RSH), sprint interval training in hypoxia (SIH) and resistance training in hypoxia (RTH)]. A combination of hypoxic methods targeting different attributes also represents an attractive solution. In conclusion, a growing number of LLTH altitude training methods exists that include the application of systemic and local hypoxia stimuli, or a combination of both, for performance enhancement in many disciplines.
Introduction
Individual- or team-sport athletes are constantly looking for training innovation to gain a competitive edge. Altitude/hypoxic training is often viewed as the practice adopted by athletes who live and train for several weeks at moderate natural altitude (1,800–2,500 m) in the lead up to competition, termed “living high-training high” (LHTH) (Millet et al., 2010). Since the 1968 Olympic Games, sojourns at terrestrial altitude have become popular among endurance athletes to improve their aerobic performance, with a more recent development involving performing some training nearer to sea level, also known as “living high-training low” (LHTL) (Levine and Stray-Gundersen, 1997). In recent times, altitude training has grown in popularity with team sports (Girard et al., 2013). However, traveling to a mountain region (hypobaric hypoxia) is not always feasible (i.e., travel time, athlete engagement, expenses) for all but the really top athletes or squads. Additionally, access to altitude hotel facilities (normobaric hypoxia) for permanent residence at simulated altitude is costly and logistically difficult for large numbers of athletes.
Vision of athletes gasping for breath when undertaking training programs in oxygen (O2) controlled rooms is increasingly common. With minimal costs and travel constraints for athletes, the “living low-training high” (LLTH) approach is becoming an important intervention for modern sport. Athletes implementing LLTH methods receive discrete and relatively brief intervals of exposure to hypoxia that typically last <2 h, at rest or while training, 2–5 times per week. The popularity of the LLTH model of altitude training is also associated with the fact that it only causes a slight disturbance to athletes' usual daily routine, allowing them to maintain their regular lifestyle in their home environment (McLean et al., 2014). Moreover, sleep quality or recovery is well preserved since the athletes do not sleep in hypoxia. The anticipated benefits of LLTH may vary widely across individuals, in particular when the focus of their training also differs (preferential aerobic vs. anaerobic adaptations) (Figure 1).
Nonetheless, it is worth mentioning that the LLTH model is not new. In fact, its effects on the human body have been studied as early as the 1940s by Russian researchers. Dating back to World War II, the former Soviet Union used hypobaric chambers to condition their pilots to fly open cockpit airplanes at altitudes higher than 7,000 m (Sirotinin, 1940). The technological development of new tools that either decrease the atmospheric pressure in the room (e.g., hypobaric chambers) or reduce the fraction of O2 in the inspired air (FiO2) by diluting it with extra nitrogen or filtering out O2 (e.g., altitude tents, hypoxicator machines) has prompted renewed interest in LLTH interventions (Wilber, 2007). In this perspective article, we first discuss the evolving boundaries of the LLTH paradigm and its practical applications for athletes by providing an updated panorama of available methods (Figure 1) and finally we highlight areas for future research.
Passive Modalities
Research into the effects of hypoxia under passive conditions has involved exposing individuals intermittently to systemic [intermittent hypoxic exposure at rest (IHE)] or local [(ischemic preconditioning (IPC)] hypoxia while seated at rest.
Intermittent Hypoxic Exposure at Rest (IHE)
IHE refers to the use of “brief” periods (3–6 min) of relatively severe levels of hypoxia (FiO2 = 0.15–0.09; ~2,800–5,500 m simulated altitude) interspersed with normoxic episodes of similar duration. Intermittent applications of “chronic” hypoxic exposures lasting 30 min to 5 h have also been introduced for high altitude expeditions pre-acclimatization protocols, with the main purpose of improving well-being (i.e., reducing the acclimatization time) and performance at altitude (Serebrovskaya, 2002). A meta-analysis indicated that IHE may improve performance in sub-elite, but not elite, performers (Bonetti and Hopkins, 2009). However, the effect observed on performance and selected physiological variables is contentious, and this strategy may not improve endurance capacity any more than regular training (Bärtsch et al., 2008). Moreover, an IOC expert group pointed that the underlying mechanisms of IHE remain obscure and concluded that “the use of intermittent hypoxic exposure does not increase sea-level performance and is not recommend. Further research in this area with respect to improving endurance performance does not seem warranted” (Lundby et al., 2012).
Ischemic Preconditioning (IPC)
IPC is a procedure causing tissue ischemia via circumferential compression of limb(s) followed by reperfusion in a repeated, cyclic manner (Murry et al., 1986). Common IPC protocols include three or four cycles of 5 min circulatory occlusion and reperfusion that are usually completed 30–45 min prior to a given exercise. Despite large between-study variability, IPC benefits include a subsequent 1–5% gain in time-trial performance and aerobic capacity (Salvador et al., 2016). IPC is also effective for improving performance at altitude (Paradis-Deschênes et al., 2018). While it represents an attractive ergogenic aid, likely related to local hyperaemia inducing accelerated/greater tissue re-/oxygenation dynamics, mechanisms remain poorly resolved (Incognito et al., 2016). Additionally, rather than a one-time intervention administered in acute settings, another novel application of IPC is to use it chronically to evoke favorable vascular (i.e., larger brachial artery flow-mediated dilatation; Jones et al., 2015) and molecular (i.e., genes involved in mitochondrial oxidative metabolism; Depre et al., 2010) adaptations.
Active Modalities
Possible improvements in exercise capacity resulting from LLTH interventions depend on the type and intensity of the workout considered—this includes using either local [blood flow restricted (BFR) exercise] and/or systemic hypoxia [continuous low-intensity training in hypoxia (CHT), interval hypoxic training (IHT), repeated-sprint training in hypoxia (RSH), sprint interval training in hypoxia (SIH) and resistance training in hypoxia (RTH)].
Local Hypoxia
Blood Flow Restriction
BFR exercise requires the continuous or cyclical application of an inflatable cuff or elastic wraps around a limb. Limiting the blood supply to and return from the contracting muscle (i.e., proximal to the muscles to be trained) produces a local hypoxic stress (Wernbom et al., 2008). In well-trained athletes this practice can induce hypertrophy and strength gains (albeit small) during low-load dynamic exercise training, while it may not cause noticeable modifications under normal circumstances (Scott et al., 2016). Training with BFR enhances performance and K+ regulation during intense exercise, in turn improving blood flow to exercising muscles and muscle anti-oxidant function (Christiansen et al., 2019). Although the magnitude of gains varies between modalities, this effect is true for both low-load resistance (e.g., weight lifting at 20–30% of 1 repetition maximum) and aerobic (e.g., cycling at 50–70% of maximal heart rate) BFR exercises. Despite BFR exercise typically utilizing lower training loads than conventional exercise (i.e., therapeutic exercise loading for return to performance athletes; Korakakis et al., 2018), repeated “all-out” efforts can also be performed with application of moderate cuff pressures (i.e., 40–60% of maximal occlusion pressure) to restrict venous return while preserving arterial inflow (Willis et al., 2019). For evidence-based recommendations when implementing BFR exercise, the reader is referred to Patterson et al. (2019).
Systemic Hypoxia
Submaximal Exercise
Continuous hypoxic training (CHT) corresponds to continuous sub-maximal training sessions in hypoxia, usually in order to improve endurance-based performance (McLean et al., 2014). Similarly to IHE, IHT refers to using moderate hypoxic exposures (i.e., generally 2,500–3,500 m although more severe elevations up to 5,500 m can also be used; Sanchez and Borrani, 2018), but during high-intensity exercise (>70% of maximal heart rate) interspersed with similar or shorter duration recoveries, and generally performed to improve high-intensity activities (McLean et al., 2014). To date, however, the effects of CHT and IHT to further improve performance compared to sea level equivalents remain elusive (Faiss et al., 2013).
RTH involves resistance training in hypoxia in order to boost muscular strength and power production (Scott et al., 2015). Due to vastly different methodologies for implementing RTH (e.g., training programs, hypoxia severity, and participants background), improvements are not always greater than resistance training in normoxia (Ramos-Campo et al., 2018). Common features of IHT and RTH efficacy are the relatively brief inter-set recovery periods in order to provide a potent metabolic stimulus to enhance anabolic responses, beyond which is possible with matched normoxic training (Scott et al., 2015). If absolute exercise intensities are not carefully matched between hypoxic and normoxic conditions, however, determining the true effectiveness of LLTH interventions (i.e., submaximal exercise intensities) remains difficult.
Maximal Exercise
RSH is a recent training method that was introduced given some of the inherent limitations of IHT (e.g., lower hypoxia-induced training stimulus) (Faiss et al., 2013). Briefly, RSH is the repetition of short (<30 s) “all-out” sprints with incomplete recoveries (<60 s) in hypoxia, also including exercise-to-rest ratios typically lower than repeated-sprint ability tests/in-match scenarios to increase metabolic strain (Millet et al., 2019). The general consensus is that RSH leads to superior (1–5%) repeated-sprint ability (i.e., faster mean sprint times or higher power outputs often accompanied by a better fatigue resistance) in normoxic conditions (Brocherie et al., 2017).
When hypoxia is induced by voluntary hypoventilation at a low lung volume (VHL), which causes relatively similar hypoxemia than altitude exposure (Woorons et al., 2007), encouraging results have been reported. In highly trained rugby players, for instance, RSH-VHL has shown larger improvements in repeated-sprint performance (~60% more sprints on average during an exhaustive “open loop” test) than with an unrestricted breathing pattern (Fornasier-Santos et al., 2018). Using this technique, swimmers can also train in hypoxia while residing near sea level and expect an improved repeated-sprint ability through an accentuation of the glycolytic stimulus of their training (Trincat et al., 2017).
Sprint interval training typically involves 20-s to 30-s “all out” efforts interspersed by 3 to 5 min of passive or low-intensity active recovery episodes. This training is often presented as a time-efficient strategy to increase cardiac output, maximal O2 uptake, and skeletal muscle mitochondrial content to a similar or even greater extent than traditional, high-volume endurance training (Gibala and Hawley, 2017). Reduced O2 delivery to the muscles with hypoxic exposure increases the stress on glycolytic flux, up-regulating this energy pathway (Puype et al., 2013). Consequently, SIH is a useful exercise stimulus to maximize exercise performance both at sea level and at altitude (Kon et al., 2015).
Combination of Various Methods
A combination of hypoxic methods targeting different attributes also represents a sounded approach (Millet et al., 2010). When implementing a “living high-training low and high” (LHTLH) intervention, for instance, athletes live high and train low except for few intense sessions in hypoxia. Reportedly, LHTL and RSH when combined can elicit concurrent aerobic and anaerobic adaptations, as manifested by a better repeated-sprint ability, in team-sport athletes (Brocherie et al., 2015). Intermittent hypoxic interval training (IHIT) is a method where hypoxia and normoxia are alternated during the same session (Millet et al., 2010). Hypoxic preconditioning (HPC), utilizing continuous or intermittent exposure to O2-deprived conditions, can also be superimposed to BFR to eventually augment the magnitude of the hemodynamic responses during realization of the subsequent exercise (Aebi et al., 2019). The combination of systemic hypoxia with vascular occlusion represents a promising mixture of hypoxic methods, for instance, BFR resistance exercise + RTH (Girard et al., 2019) or BFR aerobic exercise + RSH (Peyrard et al., 2019), for maximizing the training stimulus. Many training centers in altitude [Font-Romeu (France) or Colorado Springs (USA) at 1850 m combined with RTH and/or RSH in a climatic chamber] or at sea level [Aspetar hospital (Qatar), Western Australia Institute of Sport (Australia)] offer the possibility for such combination of hypoxic methods.
Although this is beyond the scope of this perspective article, there are various options for applying an hypoxic stimuli together with other environmental stressors—i.e., hot/humid air (heat stress; Takeno et al., 2001) or O2-enriched air (hyperoxia; Brinkmann et al., 2018)—otherwise known to independently improve physical performance (Millet et al., 2010; Gibson et al., 2019). In doing so, however, it is important to verify that absolute training quality is not blunted due to exacerbated fatigue development. For optimal implementation, the physiological stress associated with a combination of various methods or stressors can be mitigated by lower relative workload (McLean et al., 2014). Practically, this would require adjustment of duration/intensity of exercise and recovery intervals, exercise-to-rest ratio, inter-set recovery duration and/or session frequency. Whether the repetitive use of various stressors during training periods, in reference to each one alone, may also lead to further performance and physiological capacity enhancements is largely undetermined.
On the Non-Haematological Mechanisms Underlying Adaptations
With LLTH, it is doubtful that the hypoxic dose per se is sufficient to induce beneficial hematological changes in red blood cell number or total hemoglobin mass (Humberstone-Gough et al., 2013). With hypoxia exposure, the transcriptional signaling and subsequent adaptations are determined at the molecular level by HIF-1α related processes (Semenza, 2000). The many common features in the signaling initiated by exercise and hypoxia suggest that the two stressors may exert a more robust stimulus. LLTH up-regulates the activity of the transcriptional factor HIF-1α (Vogt et al., 2001; Brocherie et al., 2018) that not only govern the regulatory genes for erythropoiesis but also vasodilatory responses, glycolysis and pH regulation. Reportedly, short and intense workouts characterizing LLTH may cause larger skeletal muscle tissue adaptations through the O2 sensing pathway [capillary-to-fiber ratio, fiber cross-section area, myoglobin content and oxidative enzyme activity] than normoxic conditions (Brocherie et al., 2018). Practically, greater buffering capacity, lactic acid tolerance and/or O2 extraction in the working muscle would ultimately improve exercise tolerance.
Limitations, Challenges and Opportunities of LLTH Interventions
Despite mounting evidence of LLTH safety and efficacy, some uncertainty remains:
• While more strictly controlled and mechanistic studies are required, no single form of LLTH exists that is more effectively improving physical performance. Considering the large variability in between-subject LLTH responsiveness and the rather modest improvements in exercise capacity associated with these methods, future studies should increase their sample sizes (McLean et al., 2014). Determination of whether clamping of SpO2 would induce a more consistent hypoxic stimulus, eventually reducing variability of the LLTH responses across individuals (Hamlin et al., 2010), is required.
• Beyond the LLTH method considered, selection of an appropriate “hypoxic dose” (i.e., hypoxia severity, duration of a single exposure, and the number of aggregate exposures) and effective management of the training load likely influence attainment of peak physical performance (Chapman et al., 2014). Hypoxia is a stressor that may do more harm than good if it is too intense. In other words, it cannot be assumed that “more is better” regarding the LLTH dosage (Goods et al., 2014). Consequently, if the total training load (i.e., exercise-to-rest ratio, recovery times) is not adjusted accordingly, the amplified training impulse can swiftly lead to overreaching or overtraining.
• Identifying the optimal period of a competitive season to implement each LLTH method and the decay of adaptations during several days or weeks post-intervention deserve future attention. It also remains to be determined whether each LLTH method is best used as a strategy for pre-acclimatization, improved training responsiveness following an altitude training camp, accelerating musculoskeletal rehabilitation and/or preventing detraining during immobilization in injured athletes. The value of LLTH as a “performance recovery” strategy, for example, to limit the extent of muscle damage (Arriel et al., 2018), is promising.
• Aside from hypobaric chambers, normobaric reduced O2 rooms or terrestrial altitude, recent technological boosts open doors for military and clinical applications of LLTH methods with the widespread development of portable mask-system hypoxicator machines (Lopata and Serebrovskaya, 2012). Mobile inflatable simulated hypoxic equipment now allows swimmers or team-sport players to train in hypoxia, for example by performing swim intervals, repeated running sprints or small-side games directly in their naturally-occurring environments (Girard et al., 2013).
• Direct comparisons of the effects of VHL with other LLTH methods are required. In doing, there is also a need to better understand mechanisms at play and the potential for combination with other LLTH modalities.
• In many populations, musculoskeletal disorders such as knee osteoarthritis (e.g., older adults and/or obese individuals) or painful locomotion (e.g., injured populations awaiting surgical procedures) may outweigh possible benefits of physical activity or lead to temporary loss of fitness due to reduced mobility. The combination of slower walking/running speeds (i.e., decreased external load) and hypoxia exposure (i.e., increased internal load) is a novel intervention that in theory is metabolically similar to exercising near sea level (normoxia), yet it is associated with a reduced exercise-induced pain (Girard et al., 2017). Clinical validation of hypoxic conditioning as an innovative LLTH strategy improving therapeutic outcome beyond what is obtained today is necessary.
Conclusion
A growing number of LLTH altitude training methods exists that include the application of systemic and local hypoxia stimuli, or a combination of both, for performance enhancement in many disciplines (Figure 1). Moving forward, elite athletes and their support team will continue to strive for refinement of best practice and the individualization of the altitude dose to ultimately reduce inter-individual variability. Translation of these innovative LLTH interventions to the clinical field is also promising.
Author Contributions
OG drafted the manuscript and prepared Figure 1. All authors listed have edited, critically revised, and approved the final version for submission.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Aebi, M. R., Willis, S. J., Girard, O., Borrani, F., and Millet, G. P. (2019). Active preconditioning with blood flow restriction or/and systemic hypoxic exposure does not improve repeated sprint cycling performance. Front. Physiol. 10:1393. doi: 10.1152/ajpregu.00104.2002
Arriel, R. A., de Souza, H. L. R., da Mota, G. R., and Marocolo, M. (2018). Declines in exercise performance are prevented 24 hours after postexercise ischemic conditioning in amateur cyclists. PLoS ONE 13:e0207053. doi: 10.1371/journal.pone.0207053
Bärtsch, P., Dehnert, C., Friedmann-Bette, B., and Tadibi, V. (2008). Intermittent hypoxia at rest for improvement of athletic performance. Scand. J. Med. Sci. Sports 18, 50–56. doi: 10.1111/j.1600-0838.2008.00832.x
Bonetti, D. L., and Hopkins, W. G. (2009). Sea-level exercise performance following adaptation to hypoxia: a meta-analysis. Sports Med. 39, 107–127. doi: 10.2165/00007256-200939020-00002
Brinkmann, C., Bloch, W., and Brixius, K. (2018). Exercise during short-term exposure to hypoxia or hyperoxia - novel treatment strategies for type 2 diabetic patients?! Scand. J. Med. Sci. Sports. 28, 549–564. doi: 10.1111/sms.12937
Brocherie, F., Girard, O., Faiss, R., and Millet, G. P. (2017). Effects of repeated-sprint Training in hypoxia on sea-level performance: a meta-analysis. Sports Med. 47, 1651–1660. doi: 10.1007/s40279-017-0685-3
Brocherie, F., Millet, G. P., D'Hulst, G., Van Thienen, R., Deldicque, L., and Girard, O. (2018). Repeated maximal-intensity hypoxic exercise superimposed to hypoxic residence boosts skeletal muscle transcriptional responses in elite team-sport athletes. Acta Physiol (Oxf). 222. doi: 10.1111/apha.12851 Available online at: https://onlinelibrary.wiley.com/doi/full/10.1111/apha.12851
Brocherie, F., Millet, G. P., Hauser, A., Steiner, T., Rysman, J., Wehrlin, J. P., et al. (2015). “Live High-Train Low and High” hypoxic training improves team-sport performance. Med. Sci. Sports Exerc. 47, 2140–2149. doi: 10.1249/MSS.0000000000000630
Chapman, R. F., Karlsen, T., Resaland, G. K., Ge, R. L., Harber, M. P., Witkowski, S., et al. (2014). Defining the “dose” of altitude training: how high to live for optimal sea level performance enhancement. J. Appl. Physiol. 116, 595–603. doi: 10.1152/japplphysiol.00634.2013
Christiansen, D., Eibye, K. H., Rasmussen, V., Voldbye, H. M., Thomassen, M., Nyberg, M., et al. (2019). Cycling with blood flow restriction improves performance and muscle K+ regulation and alters the effect of anti-oxidant infusion in humans. J. Physiol. 597, 2421–2444. doi: 10.1113/JP277657
Depre, C., Park, J. Y., Shen, Y. T., Zhao, X., Qiu, H., Yan, L., et al. (2010). Molecular mechanisms mediating preconditioning following chronic ischemia differ from those in classical second window. Am. J. Physiol. Heart Circ. Physiol. 299, H752–H762. doi: 10.1152/ajpheart.00147.2010
Faiss, R., Girard, O., and Millet, G. P. (2013). Advancing hypoxic training in team sports: from intermittent hypoxic training to repeated sprint training in hypoxia. Br. J. Sports Med. 47, 45–50. doi: 10.1136/bjsports-2013-092741
Fornasier-Santos, C., Millet, G. P., and Woorons, X. (2018). Repeated-sprint training in hypoxia induced by voluntary hypoventilation improves running repeated-sprint ability in rugby players. Eur. J. Sport Sci. 18, 504–512. doi: 10.1080/17461391.2018.1431312
Gibala, M. J., and Hawley, J. A. (2017). Sprinting toward fitness. Cell Metab. 25, 988–990. doi: 10.1016/j.cmet.2017.04.030
Gibson, O. R., James, C. A., Mee, J. A., Willmott, A. G. B., Turner, G., Hayes, M., et al. (2019): Heat alleviation strategies for athletic performance: a review practitioner guidelines. Temperature7, 3–36. doi: 10.1080/23328940.2019.1666624
Girard, O., Amann, M., Aughey, R., Billaut, F., Bishop, D. J., Bourdon, P., et al. (2013). Position statement - altitude training for improving team-sport players' performance: current knowledge and unresolved issues. Br. J. Sports Med. 47, i8–i16. doi: 10.1136/bjsports-2013-093109
Girard, O., Malatesta, D., and Millet, G. P. (2017). Walking in hypoxia: an efficient treatment to lessen mechanical constraints and improve health in obese individuals? Front. Physiol. 8:73. doi: 10.3389/fphys.2017.00073
Girard, O., Willis, S. J., Purnelle, M., Scott, B. R., and Millet, G. P. (2019). Separate and combined effects of local and systemic hypoxia in resistance exercise. Eur. J. Appl. Physiol. 119, 2313–2325. doi: 10.1007/s00421-019-04217-3
Goods, P. S. R., Dawson, B. T., Landers, G. J., Gore, C. J., and Peeling, P. (2014). Effect of different simulated altitudes on repeat-sprint performance in team-sport athletes. Int. J. Sports Physiol. Perform. 9, 857–862. doi: 10.1123/ijspp.2013-0423
Hamlin, M. J., Marshall, H. C., Hellemans, J., and Ainslie, P. N. (2010). Effect of intermittent hypoxia on muscle and cerebral oxygenation during a 20-km time trial in elite athletes: a preliminary report. Appl. Physiol. Nutr. Metab. 35, 548–559. doi: 10.1139/H10-044
Humberstone-Gough, C. E., Saunders, P. U., Bonetti, D. L., Stephens, S., Bullock, N., Anson, J. M., et al. (2013). Comparison of live high: train low altitude and intermittent hypoxic exposure. J. Sports Sci. Med. 12, 394–401.
Incognito, A. V., Burr, J. F., and Millar, P. J. (2016). The effects of ischemic preconditioning on human exercise performance. Sports Med. 46, 531–544. doi: 10.1007/s40279-015-0433-5
Jones, H., Nyakayiru, J., Bailey, T. G., Green, D. J., Cable, N. T., Sprung, V. S., et al. (2015). Impact of eight weeks of repeated ischaemic preconditioning on brachial artery and cutaneous micro-circulatory function in healthy males. Eur. J. Prev. Cardiol. 22, 1083–1087. doi: 10.1177/2047487314547657
Kon, M., Nakagaki, K., Ebi, Y., Nishiyama, T., and Russell, A. P. (2015). Hormonal and metabolic responses to repeated cycling sprints under different hypoxic conditions. Growth Horm. IGF Res. 25, 121–126. doi: 10.1016/j.ghir.2015.03.002
Korakakis, V., Whiteley, R., and Epameinontidis, K. (2018). Blood flow restriction induces hypoalgesia in recreationally active adult male anterior knee pain patients allowing therapeutic exercise loading. Phys. Ther. Sport. 32, 235–243. doi: 10.1016/j.ptsp.2018.05.021
Levine, B. D., and Stray-Gundersen, J. (1997). “Living high-training low”: effect of moderate-altitude acclimatization with low-altitude training on performance. J. Appl. Physiol. 83, 102–112. doi: 10.1152/jappl.1997.83.1.102
Lopata, V. A., and Serebrovskaya, T. V. (2012). “Hypoxicators: review of the operating principles and constructions,” in Intermittent Hypoxia and Human Diseases, eds L. Xi and T. V. Serebrovskaya (London: Springer), 291–302. doi: 10.1007/978-1-4471-2906-6_24
Lundby, C., Millet, G. P., Calbet, J. A., Bartsch, P., and Subudhi, A. W. (2012). Does ‘altitude training’ increase exercise performance in elite athletes? Br. J. Sports Med. 46, 792–795. doi: 10.1136/bjsports-2012-091231
McLean, B. D., Gore, C. J., and Kemp, J. (2014). Application of 'live low-train high' for enhancing normoxic exercise performance in team sport athletes. Sports Med. 44, 1275–1287. doi: 10.1007/s40279-014-0204-8
Millet, G. P., Girard, O., Beard, A., and Brocherie, F. (2019). Repeated sprint training in hypoxia – an innovative method. Dtsch. Z. Sportmed. 70, 115–122. doi: 10.5960/dzsm.2019.374
Millet, G. P., Roels, B., Schmitt, L., Woorons, X., and Richalet, J. P. (2010). Combining hypoxic methods for peak performance. Sports Med. 40, 1–25. doi: 10.2165/11317920-000000000-00000
Murry, C. E., Jennings, R. B., and Reimer, K. A. (1986). Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 74, 1124–1136. doi: 10.1161/01.cir.74.5.1124
Paradis-Deschênes, P., Joanisse, D. R., and Billaut, F. (2018). Ischemic preconditioning improves time trial performance at moderate altitude. Med. Sci. Sports Exerc. 50, 533–541. doi: 10.1249/MSS.0000000000001473
Patterson, S. D., Hughes, L., Warmington, S., Burr, J., Scott, B. R., Owens, J., et al. (2019). Blood flow restriction exercise position stand: considerations of methodology, application, and safety. Front. Physiol. 10:533. doi: 10.3389/fphys.2019.00533
Peyrard, A., Willis, S. J., Place, N., Millet, G. P., Borrani, F., and Rupp, T. (2019). Neuromuscular evaluation of arm-cycling repeated sprints under hypoxia and/or blood flow restriction. Eur. J. Appl. Physiol. 119, 1533–1545. doi: 10.1007/s00421-019-04143-4
Puype, J., Van Proeyen, K., Raymackers, J. M., Deldicque, L., and Hespel, P. (2013). Sprint interval training in hypoxia stimulates glycolytic enzyme activity. Med. Sci. Sports Exerc. 45, 2166–2174. doi: 10.1249/MSS.0b013e31829734ae
Ramos-Campo, D. J., Scott, B. R., Alcaraz, P. E., and Rubio-Arias, J. A. (2018). The efficacy of resistance training in hypoxia to enhance strength and muscle growth: a systematic review and meta-analysis. Eur. J. Sport Sci. 18, 92–103. doi: 10.1080/17461391.2017.1388850
Salvador, A. F., De Aguiar, R. A., Lisbôa, F. D., Pereira, K. L., Cruz, R. S., and Caputo, F. (2016). Ischemic preconditioning and exercise performance: a systematic review and meta-analysis. Int. J. Sports Physiol. Perform. 11, 4–14. doi: 10.1123/ijspp.2015-0204
Sanchez, A. M., and Borrani, F. (2018). Effects of intermittent hypoxic training performed at high hypoxia level on exercise performance in highly trained runners. J. Sports Sci. 36, 2045–2052. doi: 10.1080/02640414.2018.1434747
Scott, B. R., Loenneke, J. P., Slattery, K. M., and Dascombe, B. J. (2016). Blood flow restricted exercise for athletes: a review of available evidence. J. Sci. Med. Sport. 19, 360–367. doi: 10.1016/j.jsams.2015.04.014
Scott, B. R., Slattery, K. M., and Dascombe, B. J. (2015). Intermittent hypoxic resistance training: is metabolic stress the key moderator? Med. Hypotheses. 84, 145–149. doi: 10.1016/j.mehy.2014.12.001
Semenza, G. L. (2000). HIF-1: mediator of physiological and pathophysiological responses to hypoxia. J. Appl. Physiol. 88, 1474–1480. doi: 10.1152/jappl.2000.88.4.1474
Serebrovskaya, T. V. (2002). Intermittent hypoxia research in the former Soviet Union and the commonwealth of independent states: history and review of the concept and selected applications. High Alt. Med. Biol. 3, 205–221. doi: 10.1089/15270290260131939
Sirotinin, N. N. (1940). Effect of acclimatization to high mountain climates on adaptation to decreased atmospheric pressure in decompression chambers. Arkh. Pat. Anat. Pat. Physiol. 6, 35–42.
Takeno, Y., Yoshi-Ichiro, K., and Hiroshi, N. (2001). Thermoregulatory and aerobic changes after endurance training in a hypobaric hypoxic and warm environment. J. Appl. Physiol. 91, 1520–1528. doi: 10.1152/jappl.2001.91.4.1520
Trincat, L., Woorons, X., and Millet, G. P. (2017). Repeated-sprint training in hypoxia induced by voluntary hypoventilation in swimming. Int. J. Sports Physiol. Perform. 12, 329–335. doi: 10.1123/ijspp.2015-0674
Vogt, M., Puntschart, A., Geiser, J., Zuleger, C., Billeter, R., and Hoppeler, H. (2001). Molecular adaptations in human skeletal muscle to endurance training under simulated hypoxic conditions. J. Appl. Physiol. 91,173–182. doi: 10.1152/jappl.2001.91.1.173
Wernbom, M., Augustsson, J., and Raastad, T. (2008). Ischemic strength training: a low-load alternative to heavy resistance exercise? Scand. J. Med. Sci. Sports. 18, 401–416. doi: 10.1111/j.1600-0838.2008.00788.x
Wilber, R. L. (2007). Application of altitude/hypoxic training by elite athletes. Med. Sci. Sports Exerc. 39, 1610–1624. doi: 10.1249/mss.0b013e3180de49e6
Willis, S. J., Borrani, F., and Millet, G. P. (2019). Leg- vs arm-cycling repeated sprints with blood flow restriction and systemic hypoxia. Eur. J. Appl. Physiol. 119, 1819–1828. doi: 10.1007/s00421-019-04171-0
Keywords: live low train high, altitude training, simulated altitude, systemic hypoxia, local hypoxia
Citation: Girard O, Brocherie F, Goods PSR and Millet GP (2020) An Updated Panorama of “Living Low-Training High” Altitude/Hypoxic Methods. Front. Sports Act. Living 2:26. doi: 10.3389/fspor.2020.00026
Received: 26 January 2020; Accepted: 06 March 2020;
Published: 31 March 2020.
Edited by:
George P. Nassis, University of Southern Denmark, DenmarkReviewed by:
François Billaut, Laval University, CanadaGeoffrey M. Minett, Queensland University of Technology, Australia
Copyright © 2020 Girard, Brocherie, Goods and Millet. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Olivier Girard, b2xpdi5naXJhcmRAZ21haWwuY29t
 Olivier Girard
Olivier Girard Franck Brocherie
Franck Brocherie Paul S. R. Goods1,3
Paul S. R. Goods1,3 Gregoire P. Millet
Gregoire P. Millet