- 1Department of Psychology, Middlebury College, Middlebury, VT, United States
- 2Department of Psychiatry, Massachusetts General Hospital, Boston, MA, United States
- 3Department of Oncology, Massachusetts General Hospital, Boston, MA, United States
- 4Department of Psychological Science, University of Vermont, Vermont Psychological Services, Burlington, VT, United States
Loneliness and insomnia are endemic in college students, and emotion regulation is strongly related to both. Starting with a biopsychosocial framework, the present study tested a model in which emotional repair mediated the relationship between loneliness and insomnia, with the goal of using a potential mechanism of action to address loneliness. Participants were undergraduate students (N=1,513) in the United States who completed a survey including the Trait Meta-Mood Scale, Sleep Condition Indicator, and UCLA Loneliness Scale, amongst other measures. Insomnia had a significant total negative effect on loneliness, B = −0.46, 95% CI [−0.54, −0.39]. Emotional repair partially mediated this relationship, with an indirect effect of B = 0.015, 95% CI [−0.19, −0.12]. Participants with better sleep were more able to regulate their emotions, and thus tended to experience lower levels of loneliness. Treating insomnia (e.g., CBT–I) or skills associated with emotional repair and regulation (e.g., transdiagnostic approaches to emotion regulation) could reduce overall loneliness.
1 Introduction
Over 60% of U.S. college students met the diagnostic criteria for at least one mental health disorder in 2021 (Lipson et al., 2022). College students concurrently report significant levels of insomnia (Gardani et al., 2022; Lund et al., 2010), high levels of loneliness (Demarinis, 2020; Richardson et al., 2017), and many may lack important emotion regulation skills (e.g., Moeller et al., 2020). Research on college students has modeled the relationships between these variables in pairs (e.g., Moeller and Seehuus, 2019; Zou et al., 2020), but little work has explored more complicated connections amongst insomnia, emotion regulation, and loneliness. Given the importance these factors have on overall mental health (Moeller and Seehuus, 2019), understanding the mechanisms by which they interact may help identify potential treatment targets. For example, although research on insomnia and loneliness tends to focus on loneliness as a cause of sleep disruption, this relationship appears to be bidirectional (Hom et al., 2020). Similarly, while insomnia is predictive of emotion regulation (Goldschmied, 2019), emotion regulation has inherent interpersonal and social implications and thus can interfere with effective social interaction, which may impact one's perception of loneliness (Goldschmied, 2019; Salovey and Mayer, 1990).
The present study frames the relations among insomnia, loneliness, and emotion regulation in college students using the biopsychosocial model. First proposed by Engel (1977), the biopsychosocial model posits that health outcomes are best understood in the context of the overlapping spheres of biological, psychological, and social factors. The three primary variables of interest – sleep (Adams et al., 2020; Becker et al., 2015), loneliness (Luo and Hu, 2022), and emotion regulation (Liu et al., 2023; Perry and Calkins, 2018)—fit well into this bidirectional model and have been thoroughly studied within this context, although the potential mechanisms connecting the three have not been explored.
Insomnia encompasses a multitude of conditions including difficulty falling asleep, challenges staying asleep despite otherwise adequate conditions, or sleep that is experienced as nonrestorative (Roth, 2007). Insomnia is a common challenge for college students (Jiang et al., 2015; Taylor et al., 2013; Williams et al., 2020). The bidirectional relationship between insomnia and physical and psychological health is well-established (Baglioni et al., 2016; Fang et al., 2019; Gradisar et al., 2020; LaVoy et al., 2020; Luyster et al., 2012; Morelhao et al., 2020). Higher levels of insomnia have been associated with decreased subjective well-being (Peach et al., 2016), anxiety and depression (Zou et al., 2020), and increased risk of suicide (Holdaway et al., 2018).
The relationship between sleep and mental health is particularly important to investigate in college students, as this group is at high risk for insomnia due to the dynamic experience of this period of transition. In their meta review, Wang and Bíró (2021) note insomnia was associated with social relationships, stress, caffeine use, lack of regularity in sleep habits, and low levels of physical activity. In addition, college students may not be fully aware of how impaired their sleep is (Peach et al., 2016). For example, in work by Becker et al. (2018) a validated measurement (Pittsburgh Sleep Quality Index, Buysse et al., 1989) classified 62% of their college student sample as poor sleepers, while only 27% of participants self-reported their sleep quality as “fairly bad” or “very bad.”
The feeling of loneliness is a subjective experience of social isolation, or a gap between the companionship a person desires and what they experience (Hawkley and Cacioppo, 2010; Perlman and Peplau, 1981; Russell et al., 1980). This experience of social isolation can be particularly challenging for college students, as the number and proximity of similarly aged peers in the college environment are not necessarily protective factors against loneliness (Moeller and Seehuus, 2019). For people of traditional college age in particular, the experience of loneliness is associated with stigma (Kerr and Stanley, 2021) and shame (Barreto et al., 2022). The stigma associated with loneliness may make it more difficult for college students to admit feelings of loneliness due to self- and/or others' expectations that one should easily be able to find people to socialize with in college (Bruehlman-Senecal et al., 2020).
While rates of loneliness increased for this group during the COVID-19 pandemic (Labrague et al., 2021), it is difficult to distinguish between a longer-term trend of increasing loneliness and the impact of the pandemic. A meta-analysis from Buecker et al. (2021) found that loneliness has been increasing among emerging adults over the past 43 years (1976–2019). Data from the National College Health Assessment found, of the 24,473 college students who participated in the fall 2023 assessment, ~50% screened positive for loneliness (American College Health Association, 2024).
Loneliness is linked to a variety of clinical psychopathologies in adolescents and emerging adults, including depression (Dunn and Sicouri, 2022) and suicidal ideation (Bennardi et al., 2019; Pereira and Cardoso, 2018). In their prospective study exploring the relationship between loneliness and mental health, Richardson et al. (2017) found higher levels of loneliness at baseline to be predictive of higher rates of depression, stress, and anxiety for university students a year later. Similarly, in a meta-analysis Mann et al. (2022) note that the existing literature points to loneliness as a strong predictor of negative future mental health states, particularly depression, and to a lesser extent anxiety. In light of the existing mental health challenges facing college students, loneliness is an important area of focus.
Cacioppo et al. (2002) found that greater loneliness was linked to higher levels of insomnia among college students. Griffin et al. (2020) sought to elucidate the relation between sleep and loneliness in their meta-analysis; they found that sleep and loneliness were moderately correlated across the 27 studies reviewed, with no meaningful influence of age or gender. While most of the studies included were cross-sectional in nature, the few longitudinal studies included reported mixed findings, leading the authors to conclude that the directionality of the relationship between these two variables is unclear (Griffin et al., 2020).
Insomnia and loneliness have both been linked to depression and anxiety, although the mechanisms by which they are connected are not well studied (Cacioppo and Hawkley, 2003; Cacioppo et al., 2003; Griffin et al., 2020). Loneliness and depression have been shown to predict poor sleep quality and insomnia symptoms (Griffin et al., 2020), but modeling depression and anxiety as predictors of loneliness has not been formally tested, despite evidence suggesting such a relationship (Hom et al., 2017, 2020). More severe insomnia has been linked to heightened feelings of loneliness, but it is unclear the extent to which that relationship is explained by depressive symptoms (Hom et al., 2017).
Sleep also has both direct and indirect effects on social behavior, which may in turn have implications for an individual's feelings of loneliness (Dorrian et al., 2019). Sleepiness can lead to a decrease in social activity and duration of social activity (Holding et al., 2020), as well as less desire to be in the presence of others and engage in social activities (Axelsson et al., 2020). Similarly, sleep loss has been linked to social avoidance (Simon and Walker, 2018). At the same time, an individual's sleepiness may deter others from wanting to interact with them. Sleep-deprived participants and photos of such participants, respectively, were rated by independent judges as seeming more lonely (Simon and Walker, 2018; Sundelin et al., 2017). This may be especially detrimental to one's loneliness levels considering that sleepiness can increase the desire to be cared for by others (Axelsson et al., 2020). Thus, the consequences of insomnia on day-to-day functioning may lead to both increased drive for social contact and impaired ability to obtain or maintain that contact, thus increasing the gap between desired and actual social contact.
Emotional intelligence is the ability to monitor, discriminate between, and skillfully use information about one's emotions (Salovey and Mayer, 1990). It is also considered a subset of social intelligence (Salovey and Mayer, 1990). Mayer and Salovey (1997) divided emotional intelligence into four related abilities: perceiving, using, understanding, and managing emotions. Emotional intelligence thus encompasses many specific abilities involving one's own and others' emotions, including empathy, emotion recognition, emotional expression, emotion identification, and emotion regulation. The Trait Meta-Mood Scale (TMMS; Salovey et al., 1995) is a measure designed to examine various cognitive aspects of emotional intelligence, including emotional repair (Fitness and Curtis, 2005; Salovey et al., 1995). Emotional repair refers to the ability to regulate one's emotional states and, in particular, to return to baseline from a negative emotional state (Fitness and Curtis, 2005; Salovey et al., 1995).
There is evidence of a bidirectional nature between sleep and one's ability to regulate, and more specifically repair, their emotional states (Vandekerckhove and Wang, 2018). The repair of one's emotional states has a strong impact on their ability to settle themself into a state that is conducive to falling and staying asleep (Hoag et al., 2016); therefore, individuals with poor emotional repair are more likely to experience insomnia. Insomnia also lowers the impact of an individual's ability to repair their emotional states (Baglioni et al., 2010). Thus sleep and emotion regulation, in particular emotional repair, are complexly interconnected, with sleep disruption increasing the need for emotional repair while also impairing the ability to accomplish it.
Similarly, the way in which an individual experiences their emotional states and in particular their ability to modify their emotional experience is an important factor associated with loneliness (Gallardo et al., 2018) and may impact insomnia. In other words, one's ability to regulate or repair their emotions impacts how one interacts with others, which may have implications for experiences of loneliness.
For college students, emotional repair is an important aspect of emotional intelligence and has a strong impact on their mental health (Costa et al., 2013; Jeong et al., 2024), with higher levels of emotional repair associated with significantly lower levels of mental health distress. For example, being able to alter one's emotions and engage in emotional repair is associated with lower levels of depression (Aradilla-Herrero et al., 2014; Extremera and Fernández-Berrocal, 2006), and emotional repair is also associated with lower levels of anxiety (Extremera and Fernández-Berrocal, 2006; Guil et al., 2021). Other work has suggested that emotional repair may be a mediator between insomnia and depression (Salguero-Alcañiz et al., 2021).
A bidirectional relationship between emotion regulation and loneliness has been demonstrated (Wols et al., 2015; Zysberg, 2012). While some work has focused on specific emotion regulation strategies (Kearns and Creaven, 2017; Preece et al., 2021), other work has explored the connection more broadly, finding that those with chronic loneliness may be less likely to accept invitations for social inclusion and more likely to use maladaptive emotion regulation strategies (Vanhalst et al., 2017). Studies have examined the relationship between emotion regulation and loneliness using the TMMS-repair subscale (Gallardo et al., 2018; Martín-Albo et al., 2015). A study of high school students found experiences of relatedness to be a partial mediator between emotional repair and loneliness, although when relatedness was high, repair directly influenced loneliness (Martín-Albo et al., 2015). Other studies have found that high levels of emotional repair are positively associated with task-oriented coping and negatively associated with destructive and dysfunctional coping (Fitness and Curtis, 2005). High emotional repair has also been found to be associated with positive interactive behaviors and being perceived as more socially competent (Hessel et al., 2016), while low emotional repair may lead to more interpersonal challenges (Trickey et al., 2011). Similarly, Goldschmied (2019) concludes that effectively adapting one's emotional responses to a given context helps ensure appropriate behavior with others and successful integration into society. In this way, poor emotion regulation may lead to loneliness if it impedes effective interaction with others.
Considering the multiple and complex connections between sleep and emotion regulation (Fairholme and Manber, 2015; Goldschmied, 2019), and the interpersonal implications of impaired emotion regulation (Fitness and Curtis, 2005; Goldschmied, 2019), emotional repair emerges as a possible link between insomnia and loneliness. Among college students, Tavernier and Willoughby (2015) found that sleep disruption contributed to dysfunctional emotion regulation, which in turn resulted in less positive social ties.
The present study uses survey data from a cross-sequential study of mental health among college students. Our aim is to expand the currently limited understanding of the mechanisms linking insomnia to loneliness in a population for which sleep health is particularly important (Becker et al., 2015; Brand and Kirov, 2011) and loneliness is prevalent (Moeller and Seehuus, 2019; U.S. Department of Health Human Services, 2023. We propose that one's ability to repair negative emotional experiences serves as a mediator between insomnia and loneliness. Thus, we expect our proposed mediation model to find that lower levels of insomnia are associated with better emotional repair (H1) and less loneliness (H2) and better emotional repair also predicts less loneliness (H3). Furthermore, we hypothesize that emotional repair is the mechanism by which insomnia has an effect on loneliness (H4).
2 Methods
2.1 Study design
This article is based on data from a cross-sequential study examining mental health in undergraduate students from two liberal arts colleges in the northeastern United States. Data collection occurred over the span of 2 weeks in January 2022. This study was approved by the Institutional Review Board of the last author's home institution. An email was sent to all students at both colleges with a unique link to a survey, which was delivered through Qualtrics. Participants indicated their consent online before completing the survey. N = 1,815 completed the survey, for a response rate of 39.77%. Students who completed the survey were entered into a raffle to win one of many Amazon gift cards.
2.2 Sample size and power
A power analysis was run to determine if the available sample would likely be able to meaningfully address the research questions. The power analysis focused on the mediation model in which emotional repair mediates the relationship between insomnia and loneliness. We used the R package semPower (Moshagen and Bader, 2023) version 2.1.0 with an alpha value of 0.05 and a beta value of 0.10. Our a priori estimate for the a path from insomnia to emotional repair was set at a conservatively small 0.15, based on the relationships observed using different instruments to measure the same relationship (Emert et al., 2017; Killgore et al., 2022). Our value for the b path from emotional repair to loneliness was set at 0.25, based on existing research addressing a similar mediation model using different measurement instruments (Martín-Albo et al., 2015). Finally, the c' path from sleep to loneliness was estimated at 0.32 based on a meta-analysis addressing that specific question (Martín-Albo et al., 2015), using the smaller end of the confidence interval for observed relationships. Note that the c' estimate assumes no mediation, which is a more conservative approach. Given these parameters, we estimate the required number of participants to find effects of approximately the same size as those that previous studies have observed to be 463. The actual raw sample size of N = 1,815 exceeds that estimate.
2.3 Participants
Data quality checks were conducted prior to analysis. Participants were removed if they did not complete all of the measures used in this survey (n = 230), or if they completed the survey in less than the average time minus three standard deviations, or if they had more than one straight-line response pattern (an additional n = 51). Thus, the final analytic data set of N = 1,534 did not contain any relevant missing data and had passed all data quality checks. No data transformations were conducted prior to analysis. Analyses were run to determine if there were significant differences in demographic or other variables of interest between completers and non-completers, with no significant differences observed. See Table 1 for sample demographics by gender.
2.4 Measures
2.4.1 Insomnia
The Sleep Condition Indicator (SCI; Espie et al., 2014) was used to measure insomnia. The SCI is a widely-used, eight-item measure designed to detect signs of insomnia disorder, and has been validated in several languages (Palagini et al., 2015; Uygur et al., 2024). The measure captures sleep onset, maintenance, awakenings, quality, as well as daytime functioning and persistence of sleep problems (Espie et al., 2014). Items include, “Thinking about a typical night in the last month, how long does it take you to fall asleep?”; “Thinking about the past month, to what extent has poor sleep affective your mood, energy, or relationships?”; and “How long have you had a problem with your sleep?” Each item has five options: for instance, the options for the first question listed above are 0–15 min, 16–30 min, 31–45 min, 46–60 min, and ≥61 min, and the options for the second question are “Not at all,” “A little,” “Somewhat,” “Much,” and “Very much.” Responses are then summed with a possible range of 0–32 with a higher score representing better sleep quality. In the present sample, the SCI had a Cronbach's alpha of 0.86, demonstrating adequate internal reliability.
2.4.2 Emotional repair
Emotional repair was measured using the emotion repair subscale of the Trait Meta-Mood Scale (TMMS) (Salovey et al., 1995). This subscale has 12 items including “If I find myself getting mad, I try to calm myself down” and “When I am upset I realize that the ‘good things in life' are illusions,” which are measured on a five-point scale with 1 being “strongly disagree” and 5 being “strongly agree.” The repair subscale had adequate reliability in the present sample, with a Cronbach's alpha of 0.82.
2.4.3 Loneliness
Loneliness was measured with the UCLA Loneliness Scale (version 3) (Russell, 1996). This twenty-item measure is scored on a scale of 1 (“never”) to 4 (“always”), including items such as, “How often do you feel that you lack companionship?” and “How often do you feel that your relationships with others are not meaningful?” This measure demonstrated adequate internal reliability, with an observed Cronbach's alpha of 0.94.
3 Results
Normality of the three relevant variables (insomnia, emotional repair, and loneliness) was assessed by visual analysis of the Q-Q residual plots. No significant deviation from the expected pattern was observed. Correlations between the variables of interest were estimated, with significant correlations observed between loneliness and insomnia (r = −0.30, p < 0.001) and emotional repair (r = −0.46, p < 0.001), and between insomnia and emotional repair (r = 0.24, p < 0.001).
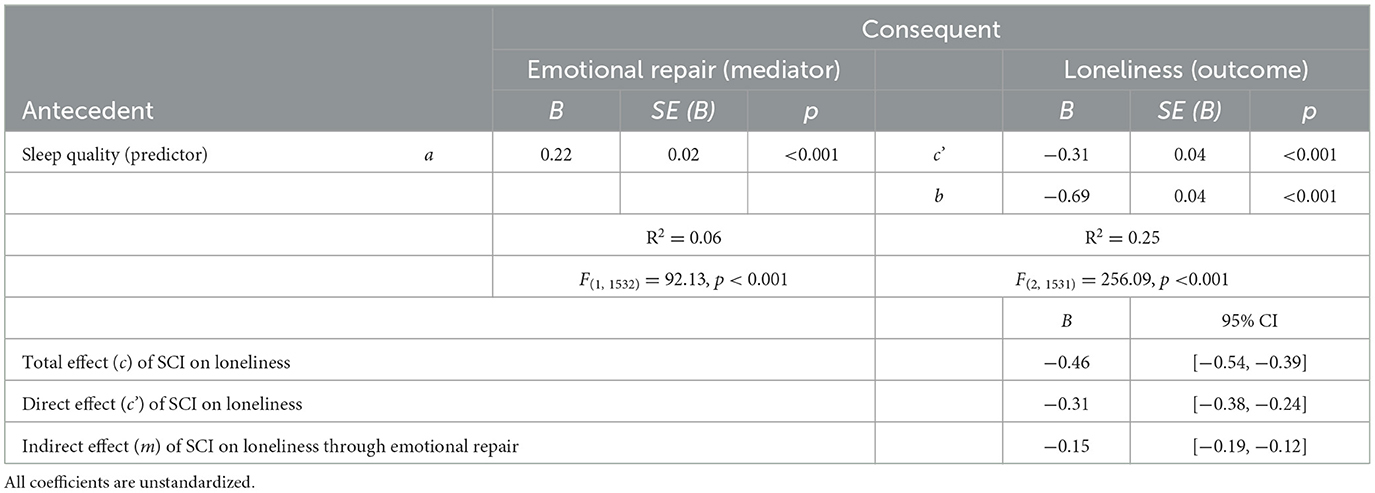
To test our hypothesis, a mediation analysis was performed in SPSS 29.0 using the PROCESS macro (Hayes, 2022), using Model 4. Regression assumptions were tested, including (a) autocorrelation, assessed via the Durbin-Watson statistic (DW = 1.99), which indicated no meaningful autocorrelation; (b) normality and homoscedasticity of residuals, assessed through both estimation of standardized residuals (M = 0.00; range = −2.83 to 3.63), which fell within acceptable limits, and visual inspection of residual plots confirming no strong deviations from normality or non-constant variance; and (c) multicollinearity, assessed via variance inflation factors (VIF < 1.10 for all predictors), indicating no concerns regarding multicollinearity. These results confirm that the data meet the necessary assumptions for regression analysis. Our results are illustrated in Figure 1 and detailed in Table 2. These results partially support our hypotheses, with the variables of interest (insomnia and emotional repair) accounting for a statistically significant (p < 0.001) and meaningful (R2 = 0.25) amount of variability in loneliness. As we hypothesized, higher scores on the SCI (representing lower levels of insomnia) are associated with better emotional repair (H1, R2 = 0.06, p < 0.001) as well as with lower levels of loneliness (H2, R2 = 0.09, p < 0.001), and better emotional repair is associated with less reported loneliness (H3, R2 =0.21, p < 0.001). Our mediation hypothesis (H4) was partially supported. The total effect of insomnia on loneliness (c) was B = −0.46, 95% CI [−0.54, −0.39], but both the direct (c', B = −0.31, 95% CI [−0.38, −0.24]) and indirect pathway (m, B = −0.15, 95% CI [−0.19, −0.12]) between insomnia and loneliness account for a meaningful portion of the variance in loneliness. That is, while emotional repair accounts for a significant and meaningful proportion of the overall effect of insomnia on loneliness, other unaccounted for factors remain.
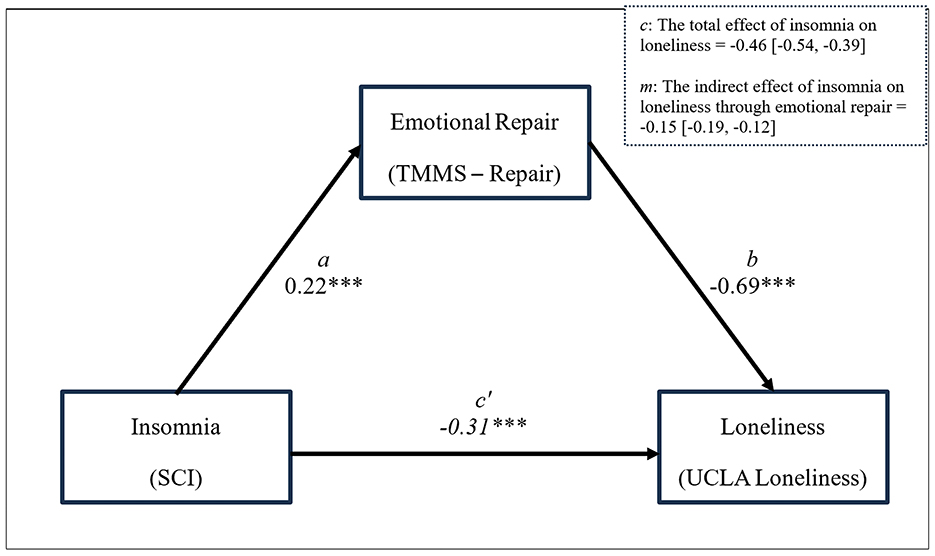
Figure 1. Emotional Repair partially mediates the relationship between sleep quality and loneliness. R2 = 0.25; F(2, 1, 531) = 256.09, p < 0.001. *p < 0.05; **p < 0.01; ***p < 0.001. All coefficients are unstandardized. a is the effect of insomnia on emotional repair; b is the effect of emotional repair on loneliness; c' is the direct effect of insomnia on loneliness, while considering the indirect effect through emotional repair.
4 Discussion
Our results partially support our hypothesized model: We observed a significant, though small, negative association between SCI scores and loneliness, indicating that lower levels of insomnia are related to decreased loneliness. In addition, emotional repair partially mediated the relationship between insomnia and loneliness. The former finding aligns with previous research that has examined the impact of insomnia on loneliness (Simon and Walker, 2018; Hom et al., 2017, 2020), and additionally provide more information about how insomnia and loneliness may be related to each other: through emotional repair. Sleep is related to our emotions in several ways, impacting our affect or mood (Baum et al., 2014; McMakin et al., 2016), empathy (Tempesta et al., 2018), emotion recognition (de Almondes et al., 2016; Tempesta et al., 2018), emotional expression (McGlinchey et al., 2011), and more. The present study brings more attention to one's ability to manage their emotions and repair a negative emotional state in the context of sleep and social interaction/isolation. Gross's (2014, 2015) models of emotion regulation suggest that emotion regulation is a complex process requiring significant cognitive resources, and sleep is an essential aspect of strong cognitive functioning; thus, we would expect better sleep quality to be related to heightened emotion regulation ability. At the same time, one's emotional stability can affect the quality of their social interactions (Fitness and Curtis, 2005; Goldschmied, 2019).
The results of this study provide additional insight into contributing factors associated with college students' experiences of loneliness. Improving emotional repair skills may be a useful target of intervention for colleges seeking to reduce students' experiences of insomnia and loneliness. It may be apt, then, to incorporate more opportunities on college campuses for students to learn how to improve their emotional repair skills as a way to buffer against loneliness.
Ellard et al. (2023) conducted a review of 22 articles addressing loneliness interventions in college students and identified four different intervention strategies: psychoeducation, increased social support, reflective exercises, and increased social interaction, the latter three exhibiting greater effectiveness than the former. Considering the interpersonal nature of emotion regulation, a social-based intervention may work particularly well in this context. As the present study suggests, however, targeting students' sleep may also be a meaningful point of intervention. There have been several examples of effective interventions among college students to improve sleep, most prominently those that are based on cognitive-behavioral therapy (Friedrich and Schlarb, 2018).
4.1 Limitations
It is important to note that our model relies on a self-report as opposed to physiological measures of sleep disruption. It is possible that our participants' self-perceptions of their sleep (as measured by the SCI) are not in agreement with what polysomnography, actigraphy, or other more objective methods would report. Furthermore, mediation implies a temporal order, which our methodology is unable to confirm due to the cross-sectional nature of our data. Even though this model is consistent with our hypotheses, we did not measure any of the variables across time, and therefore these data do not speak directly to temporal directionality. The online nature of our survey could be considered an additional limitation; however evidence suggests that findings from surveys conducted over the internet are consistent with findings from traditional survey methods (e.g., Gosling et al., 2004; Uygur et al., 2022).
4.2 Future directions/implications
Considering the limitations of self-report sleep measures and the impracticality of polysomnography for studies of this nature, future research should consider using wearable sleep monitoring devices to track sleep directly. This multi-method approach would allow future research to speak more clearly to the mechanisms of the connections. Furthermore, our findings highlight the potential for loneliness (or more broadly, mental health) interventions that are low-cost and less stigmatizing: that is, by targeting sleep at the individual level. Sleep quality may have advantages over other mental health issues in terms of treatment because sleep dysfunction is relatively low in stigma, and it is a convenient target of intervention. College students may be more willing to participate in such a sleep intervention, due to minimal feelings of shame and/or embarrassment, providing another avenue for intervention. The present study partially explains the relationship between sleep and loneliness, suggesting that emotional repair accounts for some of that connection. These findings may also suggest that, by making more of an effort to prioritize sleep in both self-care and clinical treatment, emotional repair and loneliness may both be improved.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Middlebury College Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KO: Conceptualization, Methodology, Project administration, Writing – original draft, Writing – review & editing. OR: Writing – original draft, Writing – review & editing. RM: Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – review & editing. MS: Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under award number 1R15MH125373–01. Additional support was provided by the Middlebury College Research Leave Program.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adams, S. K., Murdock, K. K., Daly-Cano, M., and Rose, M. (2020). Sleep in the social world of college students: Bridging interpersonal stress and fear of missing out with mental health. Behav. Sci. 10, 54. doi: 10.3390/bs10020054
American College Health Association (2024). American College Health Association-National College Health Assessment III: Reference Group Executive Summary Fall 2023. Silver Spring, MD: American College Health Association. Available at: https://www.acha.org/wp-content/uploads/2024/06/NCHA-IIIb_FALL_2023_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf (accessed August 2, 2024).
Aradilla-Herrero, A., Tomás-Sábado, J., and Gómez-Benito, J. (2014). Associations between emotional intelligence, depression and suicide risk in nursing students. Nurse Educ. Today 34, 520–525. doi: 10.1016/j.nedt.2013.07.001
Axelsson, J., Ingre, M., Kecklund, G., Lekander, M., Wright, K. P. Jr, and Sundelin, T. (2020). Sleepiness as motivation: a potential mechanism for how sleep deprivation affects behavior. Sleep 43:zsz291. doi: 10.1093/sleep/zsz291
Baglioni, C., Nanovska, S., Regen, W., Spiegelhalder, K., Feige, B., Nissen, C., et al. (2016). Sleep and mental disorders: a meta-analysis of polysomnographic research. Psychol. Bull. 142, 969–990. doi: 10.1037/bul0000053
Baglioni, C., Spiegelhalder, K., Lombardo, C., and Riemann, D. (2010). Sleep and emotions: a focus on insomnia. Sleep Med. Rev. 14, 227–238. doi: 10.1016/j.smrv.2009.10.007
Barreto, M., van Breen, J., Victor, C., Hammond, C., Eccles, A., Richins, M. T., et al. (2022). Exploring the nature and variation of the stigma associated with loneliness. J. Soc. Pers. Relat. 39, 2658–2679. doi: 10.1177/02654075221087190
Baum, K. T., Desai, A., Field, J., Miller, L. E., Rausch, J., and Beebe, D. W. (2014). Sleep restriction worsens mood and emotion regulation in adolescents. J. Child Psychol. Psychiat. 55, 180–190. doi: 10.1111/jcpp.12125
Becker, S. P., Jarrett, M. A., Luebbe, A. M., Garner, A. A., Burns, G. L., and Kofler, M. J. (2018). Sleep in a large, multi-university sample of college students: sleep problem prevalence, sex differences, and mental health correlates. Sleep Health 4, 174–181. doi: 10.1016/j.sleh.2018.01.001
Becker, S. P., Langberg, J. M., and Byars, K. C. (2015). Advancing a biopsychosocial and contextual model of sleep in adolescence: a review and introduction to the special issue. J. Youth Adolesc. 44, 239–270. doi: 10.1007/s10964-014-0248-y
Bennardi, M., Caballero, F. F., Miret, M., Ayuso-Mateos, J. L., Haro, J. M., Lara, E., et al. (2019). Longitudinal relationships between positive affect, loneliness, and suicide ideation: Age-specific factors in a general population. Suicide Life-Threat. Behav. 49, 90–103. doi: 10.1111/sltb.12424
Brand, S., and Kirov, R. (2011). Sleep and its importance in adolescence and in common adolescent somatic and psychiatric conditions. Int. J. Gen. Med. 4, 425–442. doi: 10.2147/IJGM.S11557
Bruehlman-Senecal, E., Hook, C. J., Pfeifer, J. H., FitzGerald, C., Davis, B., Delucchi, K. L., et al. (2020). Smartphone app to address loneliness among college students: pilot randomized controlled trial. JMIR Mental Health 7:e21496. doi: 10.2196/21496
Buecker, S., Mund, M., Chwastek, S., Sostmann, M., and Luhmann, M. (2021). Is loneliness in emerging adults increasing over time? A preregistered cross-temporal meta-analysis and systematic review. Psychological Bulletin 147, 787. doi: 10.1037/bul0000332
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R., and Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213. doi: 10.1016/0165-1781(89)90047-4
Cacioppo, J. T., and Hawkley, L. C. (2003). Social isolation and health, with an emphasis on underlying mechanisms. Perspect. Biol. Med. 46, S39–S52. doi: 10.1353/pbm.2003.0049
Cacioppo, J. T., Hawkley, L. C., and Bernston, G. C. (2003). The anatomy of loneliness. Curr. Dir. Psychol. Sci. 12, 71–74. doi: 10.1111/1467-8721.01232
Cacioppo, J. T., Hawkley, L. C., Crawford, L. E., Ernst, J. M., Burleson, M. H., Kowalewski, R. B., et al. (2002). Loneliness and health: potential mechanisms. Psychosom. Med. 64, 407–417. doi: 10.1097/00006842-200205000-00005
Costa, H., Ripoll, P., Sánchez, M., and Carvalho, C. (2013). Emotional intelligence and self-efficacy: Effects on psychological well-being in college students. Span. J. Psychol. 16, E50. doi: 10.1017/sjp.2013.39
de Almondes, K. M., Júnior, F. W. N. H., and Alves, N. T. (2016). Sleep deprivation and implications for recognition and perception of facial emotions. Sleep Biol. Rhythms 14, 13–22. doi: 10.1007/s41105-015-0029-3
Demarinis, S. (2020). Loneliness at epidemic levels in America. Explore 16, 278–279. doi: 10.1016/j.explore.2020.06.008
Dorrian, J., Centofanti, S., Smith, A., and McDermott, K. D. (2019). Self-regulation and social behavior during sleep deprivation. Prog. Brain Res. 246, 73–110. doi: 10.1016/bs.pbr.2019.03.010
Dunn, C., and Sicouri, G. (2022). The relationship between loneliness and depressive symptoms in children and adolescents: a meta-analysis. Behav. Change 39, 134–145. doi: 10.1017/bec.2022.13
Ellard, O. B., Dennison, C., and Tuomainen, H. (2023). Review: Interventions addressing loneliness amongst university students: a systematic review. Child Adolescent Ment. Health. 28, 512–523. doi: 10.1111/camh.12614
Emert, S. E., Tutek, J., and Lichstein, K. L. (2017). Associations between sleep disturbances, personality, and trait emotional intelligence. Pers. Individ. Dif. 107, 195–200. doi: 10.1016/j.paid.2016.11.050
Engel, G. L. (1977). The need for a new medical model: a challenge for biomedicine. Science 196, 129–136. doi: 10.1126/science.847460
Espie, C. A., Kyle, S. D., Hames, P., Gardani, M., Fleming, L., and Cape, J. (2014). The Sleep Condition Indicator: a clinical screening tool to evaluate insomnia disorder. BMJ Open 4:e004183. doi: 10.1136/bmjopen-2013-004183
Extremera, N., and Fernández-Berrocal, P. (2006). Emotional intelligence as predictor of mental, social, and physical health in university students. Span. J. Psychol. 9, 45–51. doi: 10.1017/S1138741600005965
Fairholme, C. P., and Manber, R. (2015). “Chapter 3 - sleep, emotions, and emotion regulation: an overview,” in Sleep and Affect, eds. K. A. Babson and M. T. Feldner (San Diego, CA: Academic Press), 45–61.
Fang, H., Tu, S., Sheng, J., and Shao, A. (2019). Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J. Cell. Mol. Med. 23, 2324–2332. doi: 10.1111/jcmm.14170
Fitness, J., and Curtis, M. (2005). Emotional intelligence and the trait meta-mood scale: relationships with empathy, attributional complexity, self-control, and responses to interpersonal conflict. E-J. Appl. Psychol. 1, 50–62. doi: 10.7790/ejap.v1i1.9
Friedrich, A., and Schlarb, A. A. (2018). Let's talk about sleep: a systematic review of psychological interventions to improve sleep in college students. J. Sleep Res. 27, 4–22. doi: 10.1111/jsr.12568
Gallardo, L. O., Martín-Albo, J., and Barrasa, A. (2018). What leads to loneliness? an integrative model of social, motivational, and emotional approaches in adolescents. J. Research on Adolescence 28, 839–857. doi: 10.1111/jora.12369
Gardani, M., Bradford, D. R. R., Russell, K., Allan, S., Beattie, L., Ellis, J. G., et al. (2022). A systematic review and meta-analysis of poor sleep, insomnia symptoms and stress in undergraduate students. Sleep Med. Rev. 61:101565. doi: 10.1016/j.smrv.2021.101565
Goldschmied, J. R. (2019). “How sleep shapes emotion regulation,” in Sleep, Personality, and Social Behavior, ed. Z. KriŽan (Cham: Springer International Publishing), 83–97.
Gosling, S. D., Vazire, S., Srivastava, S., and John, O. P. (2004). Should we trust web-based studies? A comparative analysis of six preconceptions about internet questionnaires. Am. Psychol. 59, 93–104. doi: 10.1037/0003-066X.59.2.93
Gradisar, M., Gregory, A. M., and Tikotzky, L. (2020). Is sleep the red flag to psychopathology's bull? J. Child Psychol. Psychiatry 61, 1055–1057. doi: 10.1111/jcpp.13331
Griffin, S. C., Williams, A. B., Ravyts, S. G., Mladen, S. N., and Rybarczyk, B. D. (2020). Loneliness and sleep: a systematic review and meta-analysis. Health Psychol. Open 7:2055102920913235. doi: 10.1177/2055102920913235
Gross, J. J. (2014). “Emotion regulation: conceptual and empirical foundations,” in Handbook of Emotion Regulation (2nd ed.). New York City: Guillford.
Gross, J. J. (2015). Emotion regulation: current status and future prospects. Psychol. Inq. 26, 1–26. doi: 10.1080/1047840X.2014.940781
Guil, R., Gómez-Molinero, R., Merchán-Clavellino, A., and Gil-Olarte, P. (2021). Lights and shadows of trait emotional intelligence: its mediating role in the relationship between negative affect and state anxiety in university students. Front. Psychol. 11:615010. doi: 10.3389/fpsyg.2020.615010
Hawkley, L. C., and Cacioppo, J. T. (2010). Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 40, 218–227. doi: 10.1007/s12160-010-9210-8
Hayes, A. F. (2022). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York City: Guilford Publications.
Hessel, E. T., Loeb, E. L., Szwedo, D. E., and Allen, J. P. (2016). Predictions from early adolescent emotional repair abilities to functioning in future relationships. J. Res. Adolesc. 26, 776–789. doi: 10.1111/jora.12229
Hoag, J. R., Tennen, H., Stevens, R. G., Coman, E., and Wu, H. (2016). Affect, emotion dysregulation, and sleep quality among low-income women. Sleep Health 2, 283–288. doi: 10.1016/j.sleh.2016.08.006
Holdaway, A. S., Luebbe, A. M., and Becker, S. P. (2018). Rumination in relation to suicide risk, ideation, and attempts: Exacerbation by poor sleep quality? J. Affect. Disord. 236, 6–13. doi: 10.1016/j.jad.2018.04.087
Holding, B. C., Sundelin, T., Schiller, H., Åkerstedt, T., Kecklund, G., and Axelsson, J. (2020). Sleepiness, sleep duration, and human social activity: an investigation into bidirectionality using longitudinal time-use data. Proc. Nat. Acad. Sci. 117, 21209–21217. doi: 10.1073/pnas.2004535117
Hom, M. A., Chu, C., Rogers, M. L., and Joiner, T. E. (2020). A meta-analysis of the relationship between sleep problems and loneliness. Clin. Psychol. Sci. 8, 799–824. doi: 10.1177/2167702620922969
Hom, M. A., Hames, J. L., Bodell, L. P., Buchman-Schmitt, J. M., Chu, C., Rogers, M. L., et al. (2017). Investigating insomnia as a cross-sectional and longitudinal predictor of loneliness: Findings from six samples. Psychiatry Res. 253, 116–128. doi: 10.1016/j.psychres.2017.03.046
Jeong, J., Shimono, M., Mallinckrodt, B., and Baldwin, D. R. (2024). Adult attachment, emotional intelligence, affect regulation, and self-reported distress in first-year college students at a predominantly White university. Profess. Psychol. 55, 107–117. doi: 10.1037/pro0000544
Jiang, X. L., Zheng, X. Y., Yang, J., Ye, C. P., Chen, Y. Y., Zhang, Z. G., et al. (2015). A systematic review of studies on the prevalence of insomnia in university students. Public Health 129, 1579–1584. doi: 10.1016/j.puhe.2015.07.030
Kearns, S. M., and Creaven, A. M. (2017). Individual differences in positive and negative emotion regulation: which strategies explain variability in loneliness?. Personal. Ment. Health 11, 64–74. doi: 10.1002/pmh.1363
Kerr, N. A., and Stanley, T. B. (2021). Revisiting the social stigma of loneliness. Pers. Individ. Dif. 171, 110482. doi: 10.1016/j.paid.2020.110482
Killgore, W. D. S., Vanuk, J. R., Persich, M. R., Cloonan, S. A., Grandner, M. A., and Dailey, N. S. (2022). Sleep quality and duration are associated with greater trait emotional intelligence. Sleep Health 8, 230–233. doi: 10.1016/j.sleh.2021.06.003
Labrague, L. J., De Los Santos, J. A. A., and Falguera, C. C. (2021). Social and emotional loneliness among college students during the COVID-19 pandemic: The predictive role of coping behaviors, social support, and personal resilience. Perspect. Psychiatr. Care 57, 1578–1584. doi: 10.1111/ppc.12721
LaVoy, E. C., Palmer, C. A., So, C., and Alfano, C. A. (2020). Bidirectional relationships between sleep and biomarkers of stress and immunity in youth. Int. J. Psychophysiol. 158, 331–339. doi: 10.1016/j.ijpsycho.2020.10.010
Lipson, S. K., Zhou, S., Abelson, S., Heinze, J., Jirsa, M., Morigney, J., et al. (2022). Trends in college student mental health and help-seeking by race/ethnicity: findings from the national healthy minds study, 2013–2021. J. Affect. Disord. 306, 138–147. doi: 10.1016/j.jad.2022.03.038
Liu, P., Mo, B., Yang, P., Li, D., Liu, S., and Cai, D. (2023). Values mediated emotional adjustment by emotion regulation: a longitudinal study among adolescents in China. Front. Psychol. 14, 1093072. doi: 10.3389/fpsyg.2023.1093072
Lund, H. G., Reider, B. D., Whiting, A. B., and Prichard, J. R. (2010). Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health 46, 124–132. doi: 10.1016/j.jadohealth.2009.06.016
Luo, X., and Hu, C. (2022). Loneliness and sleep disturbance among first-year college students: the sequential mediating effect of attachment anxiety and mobile social media dependence. Psychol. Sch. 59, 1776–1789. doi: 10.1002/pits.22721
Luyster, F. S., Strollo, P. J., Zee, P. C., and Walsh, J. K. (2012). Sleep: a health imperative. Sleep 35, 727–734. doi: 10.5665/sleep.1846
Mann, F., Wang, J., Pearce, E., Ma, R., Schlief, M., Lloyd-Evans, B., et al. (2022). Loneliness and the onset of new mental health problems in the general population. Soc. Psychiat. Psychiatr. Epidemiol. 57, 2161–2178. doi: 10.1007/s00127-022-02261-7
Martín-Albo, J., Lombas, A. S., Jiménez, T. I., Valdivia-Salas, S., Núñez, J. L., and León, J. (2015). The mediating role of relatedness between repair and loneliness: a preliminary model in high school students. J. Happiness Stud. 16, 1131–1148. doi: 10.1007/s10902-014-9550-3
Mayer, J. D., and Salovey, P. (1997). “What is emotional intelligence?,” in Emotional Development and Emotional Intelligence: Educational Implications (New York City: Basic Books), 3–34.
McGlinchey, E. L., Talbot, L. S., Chang, K. H., Kaplan, K. A., Dahl, R. E., and Harvey, A. G. (2011). The effect of sleep deprivation on vocal expression of emotion in adolescents and adults. Sleep 34, 1233–1241. doi: 10.5665/SLEEP.1246
McMakin, D. L., Dahl, R. E., Buysse, D. J., Cousins, J. C., Forbes, E. E., Silk, J. S., et al. (2016). The impact of experimental sleep restriction on affective functioning in social and nonsocial contexts among adolescents. J. Child Psychol. Psychiat. 57, 1027–1037. doi: 10.1111/jcpp.12568
Moeller, R. W., and Seehuus, M. (2019). Loneliness as a mediator for college students' social skills and experiences of depression and anxiety. J. Adolesc. 73, 1–13. doi: 10.1016/j.adolescence.2019.03.006
Moeller, R. W., Seehuus, M., and Peisch, V. (2020). Emotional intelligence, belongingness, and mental health in college students. Front. Psychol. 11:93. doi: 10.3389/fpsyg.2020.00093
Morelhao, P. K., Pinto, R. Z., Tufik, S., and Andersen, M. L. (2020). Sleep disturbance and low back pain in older adults: a bidirectional relationship? Pain Med. 21, 1303–1304. doi: 10.1093/pm/pnz240
Moshagen, M., and Bader, M. (2023). semPower: Power Analyses for Sem. (version 2.1.0). Available at: https://CRAN.R-project.org/package=semPower (accessed August 2, 2024).
Palagini, L., Ragno, G., Caccavale, L., Gronchi, A., Terzaghi, M., Mauri, M., et al. (2015). Italian validation of the Sleep Condition Indicator: a clinical screening tool to evaluate Insomnia Disorder according to DSM-5 criteria. Int. J. Psychophysiol. 98, 435–440. doi: 10.1016/j.ijpsycho.2015.08.008
Peach, H., Gaultney, J. F., and Gray, D. D. (2016). Sleep hygiene and sleep quality as predictors of positive and negative dimensions of mental health in college students. Cogent Psychol. 3, 1168768. doi: 10.1080/23311908.2016.1168768
Pereira, A. A. G., and Cardoso, F. M. (2018). Searching for psychological predictors of suicidal ideation in university students. Psicologia: Teoria e Pesquisa 33:e33420. doi: 10.1590/0102.3772e33420
Perlman, D., and Peplau, L. A. (1981). “Toward a social psychology of loneliness,” in Personal Relationships: 3. Relationships in Disorder, eds. R. Gilmour, and S. Duck (San Diego, CA: Academic Press), 31–56.
Perry, N. B., and Calkins, S. D. (2018). “A biopsychosocial perspective on the development of emotion regulation across childhood,” in Emotion Regulation (London: Routledge), 3–30.
Preece, D., Goldenberg, A., Becerra, R., Boyes, M., Hasking, P., and Gross, J. (2021). Loneliness and emotion regulation. Pers. Individ. Dif. 180:110974. doi: 10.1016/j.paid.2021.110974
Richardson, J. C., Maeda, Y., Lv, J., and Caskurlu, S. (2017). Social presence in relation to students' satisfaction and learning in the online environment: a meta-analysis. Comput. Human Behav. 71, 402–417. doi: 10.1016/j.chb.2017.02.001
Roth, T. (2007). Insomnia: definition, prevalence, etiology, and consequences. J. Clini. Sleep Med. 3, S7–S10. doi: 10.5664/jcsm.26929
Russell, D., Peplau, L. A., and Cutrona, C. E. (1980). The revised UCLA loneliness scale: concurrent and discriminant validity evidence. J. Pers. Soc. Psychol. 39, 472–480. doi: 10.1037/0022-3514.39.3.472
Russell, D. W. (1996). UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J. Pers. Assess. 66, 20–40. doi: 10.1207/s15327752jpa6601_2
Salguero-Alcañiz, M. P., Merchán-Clavellino, A., and Alameda-Bailén, J. R. (2021). Emotional intelligence as a mediator between subjective sleep quality and depression during the confinement due to COVID-19. Int. J. Environ. Res. Public Health 18:8837. doi: 10.3390/ijerph18168837
Salovey, P., and Mayer, J. D. (1990). Emotional intelligence. Imagin. Cogn. Pers. 9, 185–211. doi: 10.2190/DUGG-P24E-52WK-6CDG
Salovey, P., Mayer, J. D., Goldman, S. L., Turvey, C., and Palfai, T. P. (1995). “Emotional attention, clarity, and repair: exploring emotional intelligence using the Trait Meta-Mood Scale,” in Emotion, Disclosure, & Health (Washington, D.C.: American Psychological Association), 125–154.
Simon, E. B., and Walker, M. P. (2018). Sleep loss causes social withdrawal and loneliness. Nat. Commun. 9:1. doi: 10.1038/s41467-018-05377-0
Sundelin, T., Lekander, M., Sorjonen, K., and Axelsson, J. (2017). Negative effects of restricted sleep on facial appearance and social appeal. R. Soc. Open Sci. 4:160918. doi: 10.1098/rsos.160918
Tavernier, R., and Willoughby, T. (2015). A longitudinal examination of the bidirectional association between sleep problems and social ties at university: the mediating role of emotion regulation. J. Youth Adolesc. 44, 317–330. doi: 10.1007/s10964-014-0107-x
Taylor, D. J., Bramoweth, A. D., Grieser, E. A., Tatum, J. I., and Roane, B. M. (2013). Epidemiology of insomnia in college students: relationship with mental health, quality of life, and substance use difficulties. Behav. Ther. 44, 339–348. doi: 10.1016/j.beth.2012.12.001
Tempesta, D., Socci, V., De Gennaro, L., and Ferrara, M. (2018). Sleep and emotional processing. Sleep Med. Rev. 40, 183–195. doi: 10.1016/j.smrv.2017.12.005
Trickey, M. L., Farhall, J., Wertheim, E. H., Hinch, C., and Ong, B. (2011). An examination of the relationships among emotion management, interpersonal hassles, and depressive symptomatology. Aust. J. Psychol. 63, 100–106. doi: 10.1111/j.1742-9536.2011.00016.x
U.S. Department of Health and Human Services (2023). Our Epidemic of Loneliness and Isolation: The U.S. Surgeon General's Advisory on the Healing Effects of Social Connection and Community. Washington, D.C.: U.S. Department of Health and Human Services. Available online at: https://www.hhs.gov/surgeongeneral/reports-and-publications/loneliness/index.html
Uygur, H., Ahmed, O., Uygur, O. F., Miller, C. B., Hursitoglu, O., Bahar, A., et al. (2024). Validity and reliability of the Turkish Version of the sleep condition indicator: a clinical screening instrument based on the DSM-5 criteria for insomnia. Nat. Sci. Sleep 16, 63–74. doi: 10.2147/NSS.S433656
Uygur, O. F., Uygur, H., Chung, S., Ahmed, O., Demiroz, D., Aydin, E. F., et al. (2022). Validity and reliability of the Turkish version of the Glasgow sleep effort scale. Sleep Med. 98, 144–151. doi: 10.1016/j.sleep.2022.06.022
Vandekerckhove, M., and Wang, Y. L. (2018). Emotion, emotion regulation and sleep: an intimate relationship. AIMS Neurosci. 5:1. doi: 10.3934/Neuroscience.2018.5.1
Vanhalst, J., Luyckx, K., Van Petegem, S., and Soenens, B. (2017). The detrimental effects of adolescents' chronic loneliness on motivation and emotion regulation in social situations. J. Youth Adolesc. 47, 162–176. doi: 10.1007/s10964-017-0686-4
Wang, F., and Bíró, É. (2021). Determinants of sleep quality in college students: A literature review. Explore 17, 170–177. doi: 10.1016/j.explore.2020.11.003
Williams, A. B., Dzierzewski, J. M., Griffin, S. C., Lind, M. J., Dick, D., and Rybarczyk, B. D. (2020). Insomnia disorder and behaviorally induced insufficient sleep syndrome: prevalence and relationship to depression in college students. Behav. Sleep Med. 18, 275–286. doi: 10.1080/15402002.2019.1578772
Wols, A., Scholte, R. H. J., and Qualter, P. (2015). Prospective associations between loneliness and emotional intelligence. J. Adolesc. 39, 40–48. doi: 10.1016/j.adolescence.2014.12.007
Zou, P., Wang, X., Sun, L., Liu, K., Hou, G., Yang, W., et al. (2020). Poorer sleep quality correlated with mental health problems in college students: a longitudinal observational study among 686 males. J. Psychosom. Res. 136:110177. doi: 10.1016/j.jpsychores.2020.110177
Keywords: sleep, insomnia, loneliness, emotion regulation, emotional repair, college students
Citation: Ostrow KD, Rieur O, Moeller RW and Seehuus M (2025) From sleeplessness to solitude: emotional repair as a buffer between insomnia and loneliness in university students. Front. Sleep 4:1516094. doi: 10.3389/frsle.2025.1516094
Received: 23 October 2024; Accepted: 17 February 2025;
Published: 07 March 2025.
Edited by:
Li Yang, National Institutes of Health (NIH), United StatesReviewed by:
Alun Thomas Lloyd Hughes, Liverpool John Moores University, United KingdomDevon Hansen, Washington State University, United States
Ömer Faruk Uygur, Atatürk University, Türkiye
Copyright © 2025 Ostrow, Rieur, Moeller and Seehuus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Robert W. Moeller, cm1vZWxsZXJAbWlkZGxlYnVyeS5lZHU=
 Katherine Domar Ostrow
Katherine Domar Ostrow Olivia Rieur
Olivia Rieur Robert W. Moeller
Robert W. Moeller Martin Seehuus
Martin Seehuus